Cardiac tumors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiac tumors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
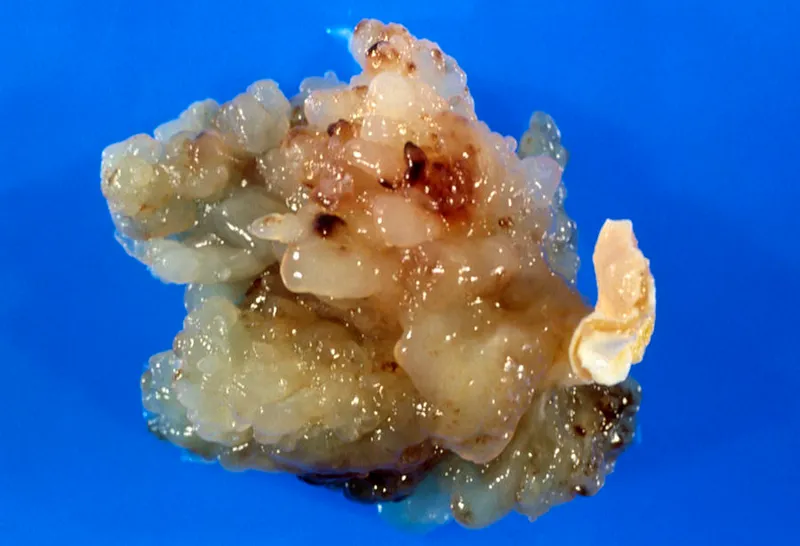
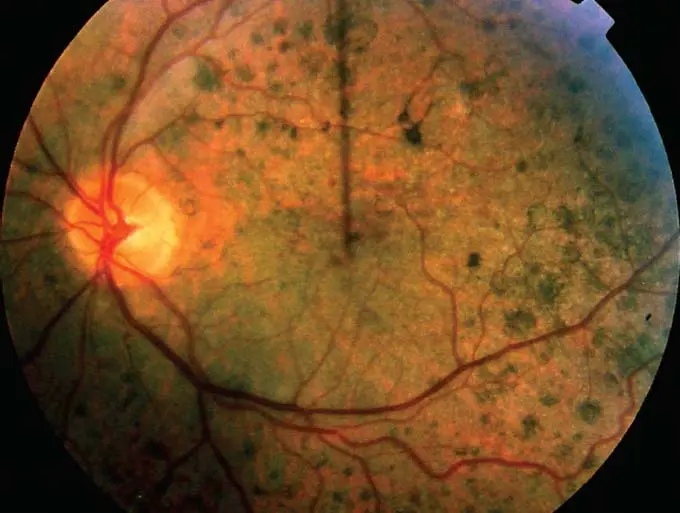
Cardiac tumors US Medical PG Question 1: A male neonate is being examined by a pediatrician. His mother informs the doctor that she had a mild fever with rash, muscle pain, and swollen and tender lymph nodes during the second month of gestation. The boy was born at 39 weeks gestation via spontaneous vaginal delivery with no prenatal care. On physical examination, the neonate has normal vital signs. Retinal examination reveals the findings shown in the image. Which of the following congenital heart defects is most likely to be present in this neonate?
- A. Double outlet right ventricle
- B. Atrial septal defect
- C. Patent ductus arteriosus (Correct Answer)
- D. Ventricular septal defect
- E. Tetralogy of Fallot
Cardiac tumors Explanation: ***Patent ductus arteriosus***
- This neonate has **congenital rubella syndrome (CRS)** based on maternal symptoms during the first trimester (fever, rash, lymphadenopathy) and the characteristic **"salt and pepper" retinopathy** shown on retinal examination
- **PDA is the most common cardiac defect** associated with CRS, occurring in approximately 50-85% of affected infants
- Other cardiac manifestations of CRS include peripheral pulmonary artery stenosis, but PDA predominates
- The classic triad of CRS includes cardiac defects, ocular abnormalities (cataracts, glaucoma, retinopathy), and sensorineural deafness
*Double outlet right ventricle*
- This is a **conotruncal anomaly** typically presenting with cyanosis in the neonatal period
- Not associated with maternal rubella infection or congenital rubella syndrome
- Would present with abnormal ventricular anatomy and significant hemodynamic compromise
*Atrial septal defect*
- While ASD is a common congenital heart defect, it is **not characteristically associated with CRS**
- Much less frequently linked to maternal viral infections compared to PDA
- Often asymptomatic in the neonatal period and detected later in childhood
*Ventricular septal defect*
- VSD is less commonly associated with **congenital rubella syndrome** compared to PDA
- When present, typically manifests with a holosystolic murmur at the left lower sternal border
- Can occur with maternal infections but is not the predominant cardiac finding in CRS
*Tetralogy of Fallot*
- Consists of four anatomic abnormalities: VSD, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy
- Presents with **cyanosis** ("tet spells") and is not specifically linked to maternal rubella infection
- Not part of the congenital rubella syndrome spectrum
Cardiac tumors US Medical PG Question 2: A 48-year-old woman comes to the physician because of progressively worsening dyspnea on exertion and fatigue for the past 2 months. She had Hodgkin lymphoma as an adolescent, which was treated successfully with chemotherapy and radiation. Her father died from complications related to amyloidosis. She does not smoke or drink alcohol. Her temperature is 36.7°C (98°F), pulse is 124/min, respirations are 20/min, and blood pressure is 98/60 mm Hg. Cardiac examination shows no murmurs. Coarse crackles are heard at the lung bases bilaterally. An ECG shows an irregularly irregular rhythm with absent P waves. An x-ray of the chest shows globular enlargement of the cardiac shadow with prominent hila and bilateral fluffy infiltrates. Transthoracic echocardiography shows a dilated left ventricle with an ejection fraction of 40%. Which of the following is the most likely cause of this patient's condition?
- A. Postradiation fibrosis
- B. Coronary artery occlusion
- C. Amyloid deposition
- D. Acute psychological stress
- E. Chronic tachycardia (Correct Answer)
Cardiac tumors Explanation: ***Chronic tachycardia***
- The **irregularly irregular rhythm with absent P waves** on ECG is characteristic of **atrial fibrillation**, which can lead to **tachycardia-induced cardiomyopathy** if sustained. The pulse of 124/min supports this.
- A sustained elevated heart rate like 124/min, especially in the context of atrial fibrillation, can cause **ventricular dilation** and reduced ejection fraction, leading to symptoms like dyspnea and fatigue observed in the patient.
*Postradiation fibrosis*
- While the patient has a history of radiation therapy for Hodgkin lymphoma, **radiation-induced cardiac damage** typically manifests as perivascular **fibrosis**, leading to **restrictive cardiomyopathy** or pericardial disease, not primarily dilated cardiomyopathy with an irregularly irregular rhythm.
- This condition is often associated with a **reduced diastolic filling** and **normal systolic function** initially, which contradicts the dilated left ventricle and reduced ejection fraction described.
*Amyloid deposition*
- The family history of amyloidosis is a red herring in this clinical picture. While **cardiac amyloidosis** can cause heart failure, it typically presents as **restrictive cardiomyopathy** with **thickened ventricular walls** and normal or reduced ventricular cavity size, not a dilated left ventricle.
- ECG findings in amyloidosis often include **low voltage QRS complexes** despite thickened walls, which is not described.
*Coronary artery occlusion*
- **Coronary artery occlusion** (e.g., myocardial infarction) can lead to dilated cardiomyopathy and reduced ejection fraction, but it usually presents with chest pain or specific ECG changes (e.g., ST elevation/depression, Q waves) that are not mentioned.
- The **irregularly irregular rhythm** (atrial fibrillation) and absence of murmurs make a primary ischemic event less likely as the sole explanation for the global cardiac changes.
*Acute psychological stress*
- **Acute psychological stress** can trigger **takotsubo cardiomyopathy** (stress-induced cardiomyopathy), which presents with left ventricular dysfunction and apical ballooning.
- However, this is typically an acute event with different ECG patterns (often ST elevation) and would not explain the chronic, sustained tachycardia and atrial fibrillation leading to dilated cardiomyopathy.
Cardiac tumors US Medical PG Question 3: A 62-year-old woman presents to the emergency department with a 2-hour history of sharp chest pain. She says that the pain is worse when she inhales and is relieved by sitting up and leaning forward. Her past medical history is significant for rheumatoid arthritis, myocardial infarction status post coronary artery bypass graft, and radiation for breast cancer 20 years ago. Physical exam reveals a rubbing sound upon cardiac auscultation as well as increased jugular venous distention on inspiration. Pericardiocentesis is performed revealing grossly bloody fluid. Which of the following is most specifically associated with this patient's presentation?
- A. Myocardial infarction
- B. Malignancy (Correct Answer)
- C. Uremia
- D. Rheumatoid arthritis
- E. Viral illness
Cardiac tumors Explanation: ***Malignancy***
- The presence of **grossly bloody (hemorrhagic) pericardial fluid** is the key finding that most specifically points to **malignancy** as the underlying cause.
- **Hemorrhagic pericardial effusion** is most commonly associated with: (1) malignancy, (2) tuberculosis, or (3) trauma. Given the patient's **history of radiation therapy for breast cancer 20 years ago**, malignancy (either metastatic breast cancer or radiation-induced secondary malignancy) is the most likely cause.
- Clinical features like **chest pain** worse on inspiration and relieved by leaning forward, a **pericardial friction rub**, and **increased jugular venous distention on inspiration (Kussmaul sign)** indicate pericarditis with possible cardiac tamponade.
*Myocardial infarction*
- While myocardial infarction can lead to pericarditis (acute post-MI pericarditis or delayed Dressler's syndrome), the pericardial fluid is typically **serous or serosanguinous, not grossly bloody**.
- The patient's history of prior MI and CABG makes this less likely to be the cause of this acute presentation with hemorrhagic effusion.
- Post-MI pericarditis usually occurs within days to weeks after the MI event.
*Uremia*
- **Uremic pericarditis** occurs in patients with severe kidney failure (uremia) and typically presents with **serofibrinous exudate**, not grossly bloody effusion.
- There is no clinical indication of renal failure or uremia in this patient's presentation.
*Rheumatoid arthritis*
- **Rheumatoid pericarditis** can occur in patients with RA, but the pericardial effusion is usually **sterile and serofibrinous**, rarely resulting in frankly hemorrhagic fluid.
- While this patient has RA, the **grossly bloody fluid** and **history of breast cancer radiation** make malignancy a much more specific and likely diagnosis.
*Viral illness*
- **Viral pericarditis** is a common cause of acute pericarditis and typically presents with chest pain and a pericardial friction rub.
- However, viral pericarditis usually produces **serous or serofibrinous effusions, not grossly bloody fluid**.
- There is no mention of prodromal viral symptoms, and the hemorrhagic nature of the fluid strongly argues against a viral etiology.
Cardiac tumors US Medical PG Question 4: A 29-year-old homeless man visits his local walk-in-clinic complaining of shortness of breath, fatigability, malaise, and fever for the past month. His personal history is significant for multiple inpatient psychiatric hospitalizations for a constellation of symptoms that included agitation, diarrhea, dilated pupils, and restless legs. On physical examination, his blood pressure is 126/72 mm Hg, heart rate is 117/min, body temperature is 38.5°C (101.3°F), and saturating 86% on room air. Auscultation reveals a holosystolic murmur that is best heard at the left sternal border and noticeably enhanced during inspiration. What is the underlying pathophysiological mechanism in this patient’s heart condition?
- A. Failed delamination
- B. Chemical endothelial damage (Correct Answer)
- C. Verrucous lesions
- D. Myxomatous degeneration
- E. Fibrillin 1 (FBN1) mutations
Cardiac tumors Explanation: ***Chemical endothelial damage***
- The patient's history of recurrent psychiatric hospitalizations with symptoms of agitation, diarrhea, dilated pupils, and restless legs points to **substance abuse**, particularly consistent with IV drug use, a common issue in homeless individuals. This, in conjunction with the signs of infection (fever, malaise, elevated heart rate) and a heart murmur, strongly suggests **infective endocarditis** in an IV drug user.
- **Intravenous drug use** introduces foreign substances and bacteria directly into the bloodstream, causing **chemical endothelial damage** to the heart valves. This damage, particularly to the **tricuspid valve** (indicated by the holosystolic murmur at the left sternal border enhanced by inspiration), provides a nidus for bacterial adherence and vegetation formation, leading to infective endocarditis.
*Failed delamination*
- **Failed delamination** is a developmental anomaly typically associated with **Ebstein's anomaly**, where the tricuspid valve leaflets are displaced into the right ventricle.
- This condition is congenital and usually diagnosed earlier in life, contrasting with the patient's acquired symptoms of infection and drug use.
*Verrucous lesions*
- **Verrucous lesions** on heart valves are characteristic of **nonbacterial thrombotic endocarditis (NBTE)**, also known as marantic endocarditis.
- While NBTE can occur in debilitated patients, it is typically associated with hypercoagulable states or advanced malignancy and does not usually present with the overt signs of infection (fever, malaise) seen in this patient.
*Myxomatous degeneration*
- **Myxomatous degeneration** is the primary pathophysiology behind **mitral valve prolapse**, a common cause of mitral regurgitation.
- While it can cause a murmur, it does not typically lead to the inflammatory and infectious presentation described, nor is it usually associated with IV drug use.
*Fibrillin 1 (FBN1) mutations*
- **Fibrillin 1 (FBN1) mutations** are the genetic basis of **Marfan syndrome**, a connective tissue disorder.
- Marfan syndrome can cause cardiovascular abnormalities, particularly **aortic root dilation** and **mitral valve prolapse**, but it does not directly explain the acute infectious presentation or the association with IV drug use.
Cardiac tumors US Medical PG Question 5: A 36-year-old man comes to the clinic for "bumps under his nipples." He is anxious that this could be breast cancer as his sister was just recently diagnosed. Past medical history is unremarkable except for an appendectomy at age 13. He currently works as a personal trainer and reports a diet that consists mainly of lean meat. The patient reports drinking 1-2 beers over the weekends. Physical examination demonstrates a muscular physique with mobile smooth masses below the areola bilaterally with no discharge. What other physical exam finding is most likely to be seen in this individual?
- A. Palmar erythema
- B. Testicular atrophy (Correct Answer)
- C. Bitemporal hemianopsia
- D. Fluid wave
- E. Spider angiomas
Cardiac tumors Explanation: ***Testicular atrophy***
- The bilateral subareolar masses suggest **gynecomastia**, which can be caused by an **imbalance of estrogens and androgens**.
- **Androgen abuse** (e.g., anabolic steroids for muscle building as a personal trainer) can suppress endogenous testosterone production, leading to secondary hypogonadism and consequently, **testicular atrophy**.
*Palmar erythema*
- **Palmar erythema** is typically associated with **chronic liver disease**, which is not indicated by the patient's history or presenting symptoms.
- While liver disease can cause gynecomastia due to impaired estrogen metabolism, there are no other signs pointing to liver dysfunction.
*Bitemporal hemianopsia*
- **Bitemporal hemianopsia** is a visual field defect caused by compression of the **optic chiasm**, commonly by a **pituitary adenoma**.
- While some pituitary adenomas can secrete prolactin (leading to hypogonadism and sometimes gynecomastia), bitemporal hemianopsia is not the most likely finding associated with the probable cause of gynecomastia in this patient.
*Fluid wave*
- A **fluid wave** is a physical exam sign of **ascites**, which indicates significant fluid accumulation in the peritoneal cavity, usually due to **severe liver disease** or heart failure.
- There are no clinical signs or symptoms in the patient's presentation to suggest ascites or these underlying conditions.
*Spider angiomas*
- **Spider angiomas** (or spider nevi) are small, arteriolar lesions commonly found on the trunk, neck, and face. They are classically associated with **chronic liver disease** or conditions with high estrogen levels (like pregnancy).
- Similar to palmar erythema, there is no evidence of liver disease in this patient, making spider angiomas an unlikely finding.
Cardiac tumors US Medical PG Question 6: A 69-year-old smoker presents to physician after noticing that his face seems to be more swollen than usual. Upon further questioning, he reports increasing shortness of breath and cough over the past 6 months. On exam, his physician notices venous distention in his neck and distended veins in the upper chest and arms. Chest radiograph shows a right upper lobe mass. What is the embryologic origin of the vessel being compressed by this patient's tumor?
- A. Cardinal veins (Correct Answer)
- B. Primitive ventricle
- C. Left horn of sinus venosus
- D. Truncus arteriosus
- E. Bulbus cordis
Cardiac tumors Explanation: ***Cardinal veins***
- The symptoms of facial swelling, neck vein distention, and upper chest/arm vein distention, especially with a right upper lobe mass, are classic for **superior vena cava (SVC) syndrome**.
- The **SVC** is formed from the fusion of the anterior **cardinal veins**, which drain the upper body during embryonic development.
*Primitive ventricle*
- The **primitive ventricle** develops into parts of the left and right **ventricles** of the heart.
- It is not directly involved in the formation of major systemic veins like the SVC.
*Left horn of sinus venosus*
- The **left horn of the sinus venosus** mostly regresses and contributes to structures like the **coronary sinus** and the oblique vein of the left atrium.
- It does not form the SVC, which drains the upper body.
*Truncus arteriosus*
- The **truncus arteriosus** is an embryonic structure that separates to form the **aorta** and the **pulmonary artery**.
- It is an arterial structure, not a venous structure that would be compressed in SVC syndrome.
*Bulbus cordis*
- The **bulbus cordis** develops into the **conus arteriosus** (infundibulum) of the right ventricle and the **aortic vestibule** of the left ventricle.
- Like the truncus arteriosus, it is involved in arterial outflow tracts and not the formation of the SVC.
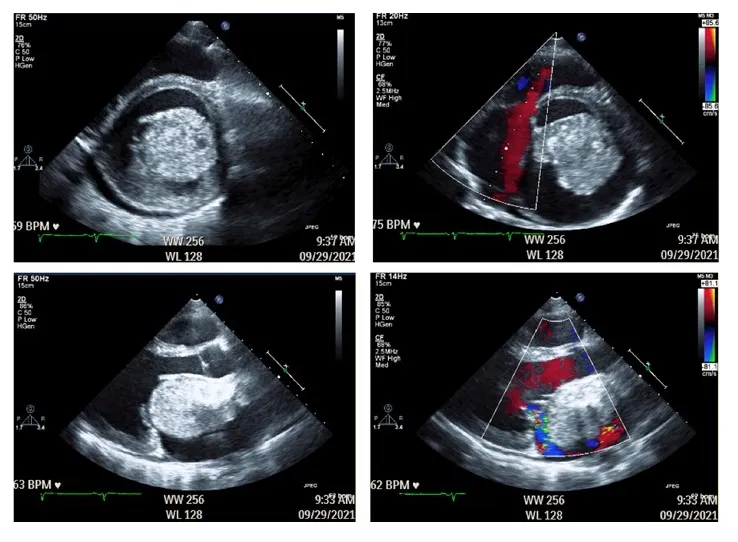
Cardiac tumors US Medical PG Question 7: A 38-year-old woman is referred to a cardiologist for evaluation of syncope. Over the past year she has experienced 2 syncopal events. The first event occurred while she was standing, and the second when she laid down on her side. She denies bowel or bladder incontinence during the episodes or palpitations. However, she reports the presence of a low-grade fever over the past 3 months and a recent visit to the emergency department for a transient ischemic attack. She has a history of intravenous drug use but reports not having used in over 5 years. Temperature is 100.0°F (37.8°C), blood pressure is 115/72 mmHg, pulse is 90/min, and respirations are 20/min and regular. A detailed neurologic examination reveals no focal deficits. Cardiac auscultation demonstrates a diastolic "plop" at the cardiac apex. Which of the following findings will most likely be demonstrated on transthoracic echocardiography?
- A. Flail mitral valve leaflet
- B. Left ventricular mass
- C. Decreased left ventricular ejection fraction
- D. Left atrial pedunculated mass (Correct Answer)
- E. Patent foramen ovale
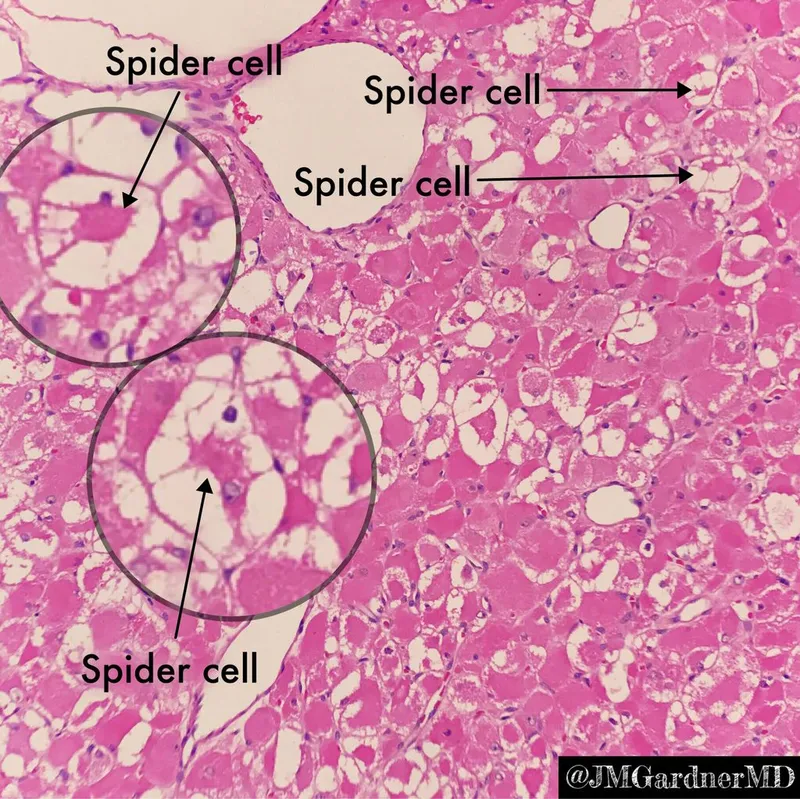
Cardiac tumors Explanation: ***Left atrial pedunculated mass***
- The patient's presentation with **syncope** in varying positions (standing and lying down), a **low-grade fever**, history of **transient ischemic attack (TIA)**, and a **diastolic "plop"** strongly suggests a **left atrial myxoma**.
- A left atrial myxoma is a **pedunculated tumor** that can intermittently obstruct mitral valve flow, leading to syncope, and can embolize, causing TIAs.
*Flail mitral valve leaflet*
- A flail mitral valve leaflet typically causes severe **mitral regurgitation**, characterized by a **systolic murmur**.
- While it can lead to syncope due to reduced cardiac output, it would not typically present with a "diastolic plop" or TIA in this manner.
*Decreased left ventricular ejection fraction*
- A decreased left ventricular ejection fraction would cause syncope due to **heart failure** or **arrhythmias**, but it does not explain the "diastolic plop" or the TIA, especially with a history of fever.
- The "plop" sound is highly specific for an **intracardiac mass** obstructing flow.
*Left ventricular mass*
- A left ventricular mass, such as a thrombus or tumor, could cause syncope and embolization (TIA).
- However, it is unlikely to produce a **diastolic "plop"** sound, which is characteristic of a mass prolapsing into the mitral orifice during diastole.
*Patent foramen ovale*
- A patent foramen ovale (PFO) can cause **paradoxical emboli** leading to TIA, especially in the context of intravenous drug use history.
- However, a PFO does not explain the recurrent syncope in various positions, the **low-grade fever**, or the specific **diastolic "plop"** on auscultation.
Cardiac tumors US Medical PG Question 8: A 32-year-old man comes to the physician because of a 3-week history of recurrent thumb pain that worsens with exposure to cold temperatures. Examination shows a 6-mm, blue-red papule under the left thumbnail. The overlying area is extremely tender to palpation. The thumbnail is slightly pitted and cracked. This lesion most likely developed from which of the following types of cells?
- A. Dysplastic melanocytes
- B. Injured nerve cells
- C. Modified smooth muscle cells (Correct Answer)
- D. Basal epidermal cells
- E. Hyperpigmented fibroblasts
Cardiac tumors Explanation: ***Modified smooth muscle cells***
- The symptoms of **recurrent thumb pain**, worsening with **cold exposure**, and a **tender, blue-red papule** under the nail are classic for a **glomus tumor**.
- **Glomus tumors** originate from the **glomus body**, which is a specialized **neuromyoarterial structure** composed of modified **smooth muscle cells** (glomus cells).
- The **glomus body** is a specialized arteriovenous anastomosis involved in thermoregulation, explaining the **cold sensitivity** and **extreme tenderness** characteristic of these lesions.
*Dysplastic melanocytes*
- **Dysplastic melanocytes** are associated with **dysplastic nevi** or **melanoma** development, which typically present as irregularly shaped pigmented lesions, not pain-sensitive masses.
- While melanoma can occur under the nail (subungual melanoma), it usually causes **melanonychia striata** (a dark streak under the nail) and typically doesn't exhibit the extreme **cold sensitivity** and **tenderness** described.
*Injured nerve cells*
- While nerve compression or injury can cause pain, a **discrete mass** with **cold sensitivity** under the nail is not characteristic of an injured nerve cell lesion.
- Neuromas, which are benign nerve tumors, usually result from trauma and are tender but often lack the **blue-red discoloration** and **cold sensitivity** seen in this case.
*Basal epidermal cells*
- Lesions originating from **basal epidermal cells** include **basal cell carcinoma**, which is a common skin cancer.
- Basal cell carcinomas typically appear as **pearly nodules** with **telangiectasias** and are usually not associated with **cold sensitivity** or the specific pain pattern described.
*Hyperpigmented fibroblasts*
- **Hyperpigmented fibroblasts** can be found in various benign skin lesions, such as **dermatofibromas**, which are firm, solitary nodules.
- However, they do not typically cause the **cold-sensitive pain** or appear as highly vascular, **blue-red papules** under the nail that are characteristic of this presentation.
Cardiac tumors US Medical PG Question 9: A 65-year-old man presents with painless swelling of the neck over the past week. He also has noted severe night sweats, which require a change of clothes and bed linens the next day. His medical history is significant for long-standing hypertension. He received a kidney transplant 6 years ago. His current medications include amlodipine, metoprolol, furosemide, aspirin, tacrolimus, and mycophenolate. His family history is significant for his sister, who died last year from lymphoma. A review of systems is positive for a 6-kg (13.2-lb) unintentional weight loss over the past 2 months. His vital signs include: temperature 37.8°C (100.0°F) and blood pressure 120/75 mm Hg. On physical examination, there are multiple painless lymph nodes, averaging 2 cm in diameter, palpable in the anterior and posterior triangles of the neck bilaterally. Axillary and inguinal lymphadenopathy is palpated on the right side. Abdominal examination is significant for a spleen of 16 cm below the costal margin on percussion. Laboratory studies are significant for the following:
Hemoglobin 9 g/dL
Mean corpuscular volume 88 μm3
Leukocyte count 12,000/mm3
Platelet count 130,000/mm3
Creatinine 1.1 mg/dL
Lactate dehydrogenase (LDH) 1,000 U/L
A peripheral blood smear is unremarkable. Which of the following is the most likely diagnosis in this patient?
- A. Multiple myeloma
- B. Non-Hodgkin’s lymphoma (NHL) (Correct Answer)
- C. Drug-induced lymphadenopathy
- D. Chronic lymphocytic leukemia (CLL)
- E. Cytomegalovirus infection
Cardiac tumors Explanation: ***Non-Hodgkin’s lymphoma (NHL)***
- This patient presents with **B symptoms** (**unintentional weight loss**, **night sweats**, fever), diffuse **lymphadenopathy**, and **splenomegaly**, which are classic signs of lymphoma. Elevated **LDH** and a history of kidney transplant requiring immunosuppression (tacrolimus, mycophenolate) significantly increase the risk of **post-transplant lymphoproliferative disorder (PTLD)**, a type of NHL.
- The **anemia**, **thrombocytopenia**, and **leukocytosis** (with an otherwise unremarkable peripheral smear) are consistent with bone marrow involvement or chronic disease in lymphoma.
*Multiple myeloma*
- Multiple myeloma is a plasma cell dyscrasia characterized by **bone pain**, **renal failure**, **hypercalcemia**, and **anemia**. While anemia and potential renal impairment are present, the widespread lymphadenopathy and splenomegaly are not typical features.
- The elevated LDH and presence of B symptoms are more indicative of lymphoma than multiple myeloma.
*Drug-induced lymphadenopathy*
- While some medications can cause lymphadenopathy, it is typically less severe, often without systemic B symptoms, and usually resolves upon discontinuation of the causative drug.
- The combination of severe B symptoms, impressive splenomegaly, and significantly elevated LDH points to a more aggressive underlying malignancy rather than a drug reaction.
*Chronic lymphocytic leukemia (CLL)*
- CLL is characterized by a persistent **lymphocytosis** (often >5,000 mature lymphocytes/µL) on peripheral smear, which is not described here ("unremarkable").
- While CLL can cause lymphadenopathy and splenomegaly, the rapid onset of severe B symptoms and the extremely high LDH are more suggestive of an aggressive lymphoma rather than indolent CLL.
*Cytomegalovirus infection*
- CMV infection can cause lymphadenopathy, fever, and fatigue, particularly in immunocompromised patients. However, the degree of **weight loss**, **splenomegaly**, and elevated **LDH** seen here are uncharacteristic of CMV infection and point towards a more serious underlying malignancy.
- CMV typically presents with a more acute, mononucleosis-like illness and often lymphocytosis with atypical lymphocytes on peripheral smear.
Cardiac tumors US Medical PG Question 10: A 38-year-old woman comes to the physician for a 3-month history of bloody discharge from the right nipple. Her mother died of breast cancer at the age of 69 years. Mammography 6 months ago did not show any abnormalities. Examination of the breast shows expression of a small amount of serosanguinous fluid from the right nipple; there are no palpable breast masses or axillary lymphadenopathy. Ultrasonography of the right breast shows a single dilated duct. Which of the following is the most likely diagnosis?
- A. Invasive ductal carcinoma
- B. Paget disease of the breast
- C. Phyllodes tumor
- D. Breast lipoma
- E. Intraductal papilloma (Correct Answer)
Cardiac tumors Explanation: ***Intraductal papilloma***
- This lesion typically presents with **bloody or serosanguinous nipple discharge** from a single duct, as described in the patient.
- It is a **benign proliferative lesion** that grows within a major lactiferous duct, often leading to ductal dilatation on ultrasound, without a palpable mass or suspicious mammographic findings.
*Invasive ductal carcinoma*
- While it can cause bloody nipple discharge, it is more commonly associated with a **palpable mass**, skin changes, or abnormal findings on mammography.
- The absence of a palpable mass, normal mammogram 6 months prior, and isolated ductal dilatation on ultrasound make it less likely in this scenario.
*Paget disease of the breast*
- This condition presents as an **eczematous lesion of the nipple and areola**, often with itching, scaling, and ulceration.
- While it can be associated with an underlying invasive or in situ carcinoma, the primary presenting symptom is skin changes, not solely nipple discharge in a seemingly normal breast.
*Phyllodes tumor*
- These are **biphasic fibroepithelial tumors** that typically present as a rapidly growing, palpable breast mass.
- They do not characteristically present with isolated nipple discharge, especially without any palpable mass.
*Breast lipoma*
- A breast lipoma is a **benign fatty tumor** that presents as a soft, mobile, non-tender lump.
- It does not cause nipple discharge and is usually easily identifiable on imaging as a fatty lesion.
More Cardiac tumors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.