Atherosclerosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Atherosclerosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Atherosclerosis US Medical PG Question 1: A 60-year-old man seeks evaluation at a medical office due to leg pain while walking. He says the pain starts in his buttocks and extends to his thighs and down to his calves. Previously, the pain resolved with rest, but the pain now persists in his feet, even during rest. His past medical history is significant for diabetes mellitus, hypertension, and cigarette smoking. The vital signs are within normal limits. The physical examination shows an atrophied leg with bilateral loss of hair. Which of the following is the most likely cause of this patient’s condition?
- A. Thrombus formation
- B. Weakening of vessel wall
- C. Narrowing and calcification of vessels (Correct Answer)
- D. Decreased permeability of endothelium
- E. Peripheral emboli formation
Atherosclerosis Explanation: ***Narrowing and calcification of vessels***
- This describes **atherosclerosis**, the most common cause of **peripheral artery disease (PAD)**, which presents with **intermittent claudication** (leg pain with walking, improving with rest) progressing to **rest pain**, especially in the feet.
- The patient's risk factors (**diabetes, hypertension, smoking**) and physical findings (**atrophied leg, hair loss**) are highly consistent with chronic ischemia due to atherosclerosis.
*Thrombus formation*
- While thrombus formation can cause acute limb ischemia, the patient's symptoms are chronic and progressive, evolving over time from claudication to rest pain, which is more characteristic of gradual **atherosclerotic narrowing**.
- Acute thrombosis typically leads to a sudden onset of severe pain, pallor, pulselessness, paresthesias, and paralysis, which are not described here.
*Weakening of vessel wall*
- Weakening of the vessel wall is associated with conditions like **aneurysms** or dissections, which typically present with different symptoms (e.g., pulsatile masses, sudden severe chest/back pain).
- It does not directly explain the progressive ischemic symptoms described, such as claudication and rest pain from inadequate blood flow.
*Decreased permeability of endothelium*
- Decreased permeability of the endothelium generally implies difficulty in substances passing through the vessel wall, which is not directly linked to the pathophysiology of ischemic pain and tissue atrophy observed in this patient.
- Conditions affecting endothelial permeability often relate to inflammation, edema, or microvascular dysfunction, but not the macrovascular obstruction causing PAD.
*Peripheral emboli formation*
- Emboli can cause acute peripheral artery occlusion, leading to sudden onset severe limb pain and signs of ischemia.
- However, the patient's symptoms have progressed chronically over time, starting with intermittent claudication and worsening to rest pain, which is more indicative of a gradual atherosclerotic process rather than an acute embolic event.
Atherosclerosis US Medical PG Question 2: One day after undergoing a left carotid endarterectomy, a 63-year-old man has a severe headache. He describes it as 9 out of 10 in intensity. He has nausea. He had 80% stenosis in the left carotid artery and received heparin prior to the surgery. He has a history of 2 transient ischemic attacks, 2 and 4 months ago. He has hypertension, type 2 diabetes mellitus, and hypercholesterolemia. He has smoked one pack of cigarettes daily for 40 years. He drinks 1–2 beers on weekends. Current medications include lisinopril, metformin, sitagliptin, and aspirin. His temperature is 37.3°C (99.1°F), pulse is 111/min, and blood pressure is 180/110 mm Hg. He is confused and oriented only to person. Examination shows pupils that react sluggishly to light. There is a right facial droop. Muscle strength is decreased in the right upper and lower extremities. Deep tendon reflexes are 3+ on the right. There is a left cervical surgical incision that shows no erythema or discharge. Cardiac examination shows no abnormalities. A complete blood count and serum concentrations of creatinine, electrolytes, and glucose are within the reference range. A CT scan of the head is shown. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Smoking
- B. Hypertension (Correct Answer)
- C. Perioperative heparin
- D. Degree of carotid stenosis
- E. Aspirin therapy
Atherosclerosis Explanation: ***Hypertension***
- Uncontrolled **hypertension** is the strongest predisposing factor for **cerebral hyperperfusion syndrome (CHS)**, especially in patients undergoing carotid endarterectomy.
- The patient's blood pressure of **180/110 mm Hg** post-surgery, combined with symptoms like severe headache, confusion, and focal neurological deficits, is highly indicative of CHS, which is exacerbated by poor blood pressure control.
*Smoking*
- While **smoking** is a significant risk factor for **atherosclerosis** and stroke, it is not the primary predisposing factor for **cerebral hyperperfusion syndrome (CHS)** specifically.
- The immediate postoperative presentation of headache, confusion, and focal deficits points more directly to issues related to cerebral blood flow regulation rather than generalized atherosclerotic disease.
*Perioperative heparin*
- **Heparin** administration increases the risk of **hemorrhage**, which could manifest as an intracranial bleed.
- However, the clinical presentation and the typical CT findings of CHS (edema, hemorrhage in severe cases) are more strongly associated with the sudden increase in cerebral blood flow rather than just anticoagulation.
*Degree of carotid stenosis*
- A high degree of **carotid stenosis** (e.g., 80% in this case) is an indication for endarterectomy to reduce stroke risk.
- While it sets the stage for potential **cerebral hyperperfusion syndrome (CHS)** by suddenly restoring flow to a chronically ischemic brain, the degree of stenosis itself is not the predisposing factor; rather, the subsequent deregulation of cerebral autoregulation in the context of other risk factors (like hypertension) is key.
*Aspirin therapy*
- **Aspirin** is an antiplatelet agent used for secondary stroke prevention and could increase the risk of minor bleeding.
- However, it is not a direct predisposing factor for **cerebral hyperperfusion syndrome (CHS)**, nor does it typically cause the acute neurological deterioration seen in this patient in the absence of a major hemorrhagic event.
Atherosclerosis US Medical PG Question 3: A 70-year-old woman presents with substernal chest pain. She says that the symptoms began 2 hours ago and have not improved. She describes the pain as severe, episodic, and worse with exertion. She reports that she has had multiple similar episodes that have worsened and increased in frequency over the previous 4 months. Past medical history is significant for diabetes and hypertension, both managed medically. The vital signs include temperature 37.0°C (98.6°F), blood pressure 150/100 mm Hg, pulse 80/min, and respiratory rate 15/min. Her serum total cholesterol is 280 mg/dL and high-density lipoprotein (HDL) is 30 mg/dL. The electrocardiogram (ECG) shows ST-segment depression on multiple chest leads. Coronary angiography reveals 75% narrowing of her left main coronary artery. In which of the following anatomical locations is a mural thrombus most likely to form in this patient?
- A. Left ventricle (Correct Answer)
- B. Left atrium
- C. Aorta
- D. Right atrium
- E. Right ventricle
Atherosclerosis Explanation: ***Left ventricle***
- The patient presents with symptoms and ECG findings consistent with **unstable angina** or **non-ST elevation myocardial infarction (NSTEMI)**, indicating myocardial ischemia.
- With **75% left main coronary artery stenosis**, there is high risk of progression to **transmural myocardial infarction (STEMI)**, particularly affecting the anterior wall and septum.
- Mural thrombi in the left ventricle typically form **3-7 days post-infarction** in areas of **dyskinetic or akinetic myocardium** due to blood stasis, endocardial injury, and hypercoagulability (Virchow's triad).
- Left main disease affecting such a large territory makes the **left ventricle the most likely site** for mural thrombus formation.
*Left atrium*
- Mural thrombi in the left atrium are most commonly associated with **atrial fibrillation** due to blood stasis in the **left atrial appendage**.
- This patient's symptoms are characteristic of coronary artery disease affecting the left ventricle, not an atrial arrhythmia.
*Aorta*
- While thrombi can form in the aorta (e.g., in the setting of **atherosclerosis** or **aneurysms**), they are typically mural thrombi associated with specific vascular pathologies.
- The symptoms of **chest pain, ST depression**, and **coronary artery narrowing** point toward a myocardial event, making the left ventricle the most likely site for mural thrombus in this clinical context.
*Right atrium*
- Thrombi in the right atrium are usually associated with conditions leading to **venous stasis, such as deep vein thrombosis**, **central venous catheters**, or **right-sided heart failure**.
- The patient's presentation with exertional chest pain and left main coronary artery narrowing is unrelated to right atrial thrombosis.
*Right ventricle*
- The right ventricle is **much less commonly** affected by ischemic events leading to mural thrombi compared to the left ventricle, due to its **lower oxygen demand** and **different blood supply** (right coronary artery).
- While right ventricular infarction can occur (usually with inferior MI), the **left main coronary artery** supplies the left ventricle, making it the primary concern for mural thrombus formation in this patient.
Atherosclerosis US Medical PG Question 4: A 61-year-old man with hypertension and hyperlipidemia comes to the physician for a 4-month history of recurrent episodes of retrosternal chest pain, shortness of breath, dizziness, and nausea. The episodes usually start after physical activity and subside within minutes of resting. He has smoked one pack of cigarettes daily for 40 years. He is 176 cm (5 ft 9 in) tall and weighs 95 kg (209 lb); BMI is 30 kg/m2. His blood pressure is 160/100 mm Hg. Coronary angiography shows an atherosclerotic lesion with stenosis of the left anterior descending artery. Compared to normal healthy coronary arteries, increased levels of platelet-derived growth factor (PDGF) are found in this lesion. Which of the following is the most likely effect of this factor?
- A. Calcification of the atherosclerotic plaque core
- B. Invasion of T-cells through the disrupted endothelium
- C. Increased expression of vascular cell-adhesion molecules
- D. Ingestion of cholesterol by mature monocytes
- E. Intimal migration of smooth muscle cells (Correct Answer)
Atherosclerosis Explanation: ***Intimal migration of smooth muscle cells***
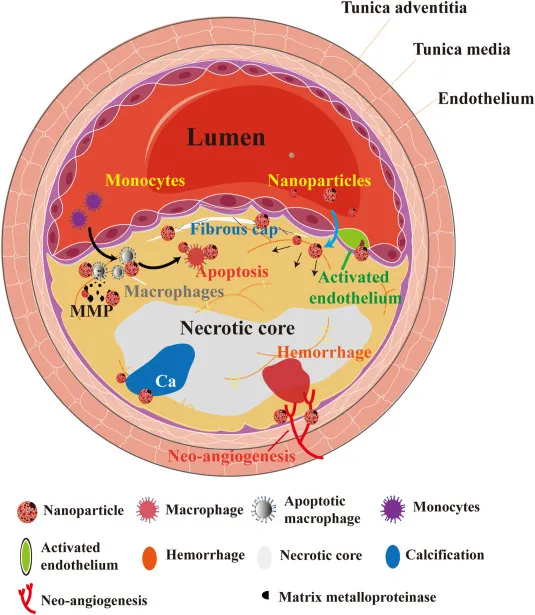
- **PDGF** is a potent **mitogen** and **chemotactic factor** for smooth muscle cells, promoting their migration from the tunica media into the intima during atherogenesis.
- This migration is a crucial step in the formation of the **fibrous cap**, contributing to plaque growth and stability.
*Calcification of the atherosclerotic plaque core*
- While calcification does occur in advanced atherosclerotic plaques, it is primarily driven by mechanisms involving **osteoblast-like differentiation** of vascular cells and deposition of **calcium phosphate**, not directly by PDGF.
- PDGF's primary role is in **cellular proliferation** and **migration**, particularly of smooth muscle cells.
*Invasion of T-cells through the disrupted endothelium*
- **T-cell invasion** into the arterial wall is an important inflammatory process in atherosclerosis, but it is primarily mediated by **chemokines** like MCP-1 and adhesion molecules, not directly by PDGF.
- PDGF typically acts on mesenchymal cells (like smooth muscle cells and fibroblasts) rather than immune cells in this context.
*Increased expression of vascular cell-adhesion molecules*
- **Expression of adhesion molecules** (e.g., VCAM-1, ICAM-1) is crucial for the recruitment of inflammatory cells, but this process is mainly driven by **pro-inflammatory cytokines** like TNF-α and IL-1, not PDGF.
- While there might be indirect effects, PDGF's direct role is not primarily in promoting adhesion molecule expression.
*Ingestion of cholesterol by mature monocytes*
- **Ingestion of cholesterol** by **macrophages** (which mature from monocytes) leads to the formation of **foam cells**, a hallmark of early atherosclerosis.
- This process is largely driven by oxidized LDL uptake, often facilitated by scavenger receptors, rather than directly by PDGF.
Atherosclerosis US Medical PG Question 5: A 47-year-old man presents as a new patient at an outpatient clinic. He has never seen a physician before, but was motivated by his 40-year-old brother's recent heart attack and seeks to optimize his health. In particular, he read that uncontrolled atherosclerosis can lead to a heart attack. Which molecule is downregulated in response to the advent of atherosclerosis?
- A. Tumor necrosis factor
- B. Serotonin
- C. Nitric oxide (Correct Answer)
- D. Interleukin 1
- E. Thromboxane A2
Atherosclerosis Explanation: ***Nitric oxide***
- **Nitric oxide (NO)** is a potent **vasodilator** and **anti-inflammatory** molecule produced by endothelial cells. In atherosclerosis, endothelial dysfunction leads to reduced NO bioavailability.
- Decreased NO production contributes to vasoconstriction, increased platelet aggregation, and enhanced smooth muscle cell proliferation, all of which promote **atherosclerotic plaque formation** and progression.
*Tumor necrosis factor*
- **Tumor necrosis factor-alpha (TNF-α)** is a **pro-inflammatory cytokine** that plays a significant role in the pathogenesis of atherosclerosis.
- It is **upregulated** in response to atherosclerotic plaque formation, contributing to endothelial activation, leukocyte recruitment, and smooth muscle cell proliferation.
*Serotonin*
- **Serotonin (5-hydroxytryptamine)** is primarily known for its role as a neurotransmitter but also acts as a **vasoconstrictor** and promotes platelet aggregation.
- While it can be released from activated platelets in the context of vascular injury, it is not consistently **downregulated** in atherosclerosis; rather, its effects can contribute to disease progression.
*Interleukin 1*
- **Interleukin-1 (IL-1)**, particularly IL-1β, is a major **pro-inflammatory cytokine** critically involved in the immune response in atherosclerosis.
- It is **upregulated** in atherosclerotic plaques, contributing to systemic inflammation, endothelial dysfunction, and vascular smooth muscle cell activation.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is a potent **vasoconstrictor** and **platelet aggregator** produced by activated platelets.
- Its levels are **increased** in atherosclerosis, contributing to hypercoagulability and increased risk of thrombotic events like myocardial infarction.
Atherosclerosis US Medical PG Question 6: A 42-year-old man with systolic heart failure secondary to amyloidosis undergoes heart transplantation. The donor heart is obtained from a 17-year-old boy who died in a motor vehicle collision. Examination of the donor heart during the procedure shows a flat, yellow-white discoloration with an irregular border on the luminal surface of the aorta. A biopsy of this lesion is most likely to show which of the following?
- A. Apoptotic smooth muscle cells
- B. Necrotic cell debris
- C. Proteoglycan accumulation
- D. Collagen deposition
- E. Lipoprotein-laden macrophages (Correct Answer)
Atherosclerosis Explanation: ***Lipoprotein-laden macrophages***
- The description of a flat, yellow-white discolored lesion with an irregular border on the luminal surface of the aorta in a 17-year-old is classic for a **fatty streak**, the earliest lesion of **atherosclerosis**.
- Fatty streaks are histologically characterized by the accumulation of **macrophages that have ingested oxidized lipoproteins**, appearing as foam cells within the intima.
*Apoptotic smooth muscle cells*
- While apoptosis of various cell types, including smooth muscle cells, can occur in advanced atherosclerotic lesions, it is not the primary or defining feature of an early **fatty streak**.
- **Apoptosis** contributes to the necrotic core formation in later stages of plaque development, not the initial yellow-white discoloration of a fatty streak.
*Necrotic cell debris*
- **Necrotic cell debris** is a prominent feature of more advanced, **complicated atherosclerotic plaques**, forming the necrotic core.
- In a **fatty streak**, the cells are primarily viable foam cells, and significant necrosis is not yet present.
*Proteoglycan accumulation*
- **Proteoglycan accumulation** occurs in the arterial intima and is involved in the retention of lipoproteins, contributing to the development of atherosclerosis.
- However, the immediate and most characteristic histological finding of the **yellow-white discoloration** in a fatty streak is the lipid-laden macrophage.
*Collagen deposition*
- **Collagen deposition** is a key feature of the fibrous cap in **advanced atherosclerotic plaques**, laid down by migrating smooth muscle cells.
- It is not the primary histological characteristic of an early, flat, yellow-white **fatty streak**.
Atherosclerosis US Medical PG Question 7: A prospective cohort study was conducted to assess the relationship between LDL and the incidence of heart disease. The patients were selected at random. Results showed a 10-year relative risk of 2.3 for people with elevated LDL levels compared to individuals with normal LDL levels. The 95% confidence interval was 1.05-3.50. This study is most likely to have which of the following p values?
- A. 0.20
- B. 0.06
- C. 0.08
- D. 0.04 (Correct Answer)
- E. 0.10
Atherosclerosis Explanation: ***0.04***
- A 95% confidence interval that **does not include 1 (one)** suggests a **statistically significant** association, meaning the p-value is likely to be **less than 0.05**.
- The given CI of 1.05-3.50 for the relative risk (RR) is entirely above 1, indicating a significant positive association, and therefore, a p-value less than 0.05.
*0.20*
- A p-value of 0.20 is **greater than 0.05**, which would imply the finding is **not statistically significant**.
- If the p-value were 0.20, the 95% confidence interval would likely **include 1**, suggesting no significant difference in risk.
*0.06*
- A p-value of 0.06 is **greater than 0.05**, indicating that the association is **not statistically significant at the conventional alpha level**.
- If the p-value were 0.06, the 95% confidence interval would likely **include 1**, or be very close to including it, contradicting the given CI of 1.05-3.50.
*0.08*
- A p-value of 0.08 is **greater than 0.05**, indicating that the finding is **not statistically significant**.
- If the p-value were 0.08, the 95% confidence interval would almost certainly **include 1**, which is inconsistent with the provided interval.
*0.10*
- A p-value of 0.10 is **greater than 0.05**, which signifies that the finding is **not statistically significant**.
- If the p-value were 0.10, the 95% confidence interval for the relative risk would typically **include 1**, contradicting the given confidence interval.
Atherosclerosis US Medical PG Question 8: A 72-year-old man comes to the physician because of a 6-month history of intermittent dull abdominal pain that radiates to the back. He has smoked one pack of cigarettes daily for 50 years. His blood pressure is 145/80 mm Hg. Abdominal examination shows generalized tenderness and a pulsatile mass in the periumbilical region on deep palpation. Further evaluation of the affected blood vessel is most likely to show which of the following?
- A. Obliterative inflammation of the vasa vasorum
- B. Formation of giant cells in the tunica media
- C. Necrotizing inflammation of the entire vessel wall
- D. Fragmentation of elastic tissue in the tunica media (Correct Answer)
- E. Accumulation of foam cells in the tunica intima
Atherosclerosis Explanation: ***Fragmentation of elastic tissue in the tunica media***
- This patient's presentation with **intermittent dull abdominal pain radiating to the back**, a **pulsatile periumbilical mass**, and a history of **heavy smoking** is highly suggestive of an **abdominal aortic aneurysm (AAA)**.
- The pathological hallmark of AAA is **degradation and fragmentation of elastic tissue in the tunica media**, caused by chronic inflammation and increased activity of **matrix metalloproteinases (MMPs)**.
- This medial degeneration leads to **weakening of the vessel wall** and progressive **dilation**, ultimately forming an aneurysm.
- While atherosclerosis initiates the process, the actual aneurysm formation is characterized by this elastic tissue destruction in the media.
*Accumulation of foam cells in the tunica intima*
- This describes the **early lesion of atherosclerosis**, which is a **risk factor** for AAA development.
- However, when examining an **established AAA**, the predominant finding is not intimal foam cells but rather **medial degeneration** with elastic tissue fragmentation.
- Atherosclerosis is the underlying cause, but the question asks about findings in the affected vessel (the aneurysm itself).
*Obliterative inflammation of the vasa vasorum*
- This is characteristic of **syphilitic aortitis** (tertiary syphilis), which typically affects the **ascending thoracic aorta**.
- While syphilis can cause aneurysms, the patient's presentation and demographics are more consistent with atherosclerotic AAA.
*Formation of giant cells in the tunica media*
- This finding is associated with **giant cell arteritis** (temporal arteritis), which affects large and medium-sized arteries, particularly the temporal and ophthalmic arteries.
- It presents with headache, jaw claudication, and visual disturbances—features absent in this case.
*Necrotizing inflammation of the entire vessel wall*
- This describes **necrotizing vasculitis** such as **polyarteritis nodosa**, which affects medium-sized muscular arteries.
- While vasculitis can cause aneurysms, the clinical picture of AAA in an elderly smoker with atherosclerotic risk factors points to atherosclerotic pathogenesis, not primary vasculitis.
Atherosclerosis US Medical PG Question 9: A 51-year-old African American man presents to his primary care physician’s office for an annual visit. He has no major concerns and says that he has been healthy for the last year. His past medical history is significant for diabetes as well as long standing hypertension that has developed gradually since his 30's; however, he has refused to take any medications. Physical exam shows no abnormal findings. Routine laboratory testing reveals the following:
Serum creatinine concentration: 1.5 mg/dL
Blood urea nitrogen: 31 mg/dL
Based on these results, urine studies are conducted that reveal mild proteinuria of less than 1 g/day and no casts.
Which of the following is most likely associated with the cause of this patient's elevated creatinine?
- A. String of beads on angiography
- B. Kimmelstiel-Wilson lesions (Correct Answer)
- C. Apple-green birefringent lesions
- D. Renal cortex necrosis
- E. Flea-bitten kidney
Atherosclerosis Explanation: **Kimmelstiel-Wilson lesions**
- The patient has a history of long-standing diabetes and hypertension, which are the primary risk factors for **diabetic nephropathy**.
- **Kimmelstiel-Wilson lesions** are nodular glomerulosclerosis pathognomonic for **diabetic nephropathy**, characterized by hyaline nodules in the mesangium.
- This is the most likely cause given the combination of diabetes, mild proteinuria (<1 g/day), and chronic renal insufficiency.
*String of beads on angiography*
- This finding is characteristic of **fibromuscular dysplasia**, a non-inflammatory vascular disease that can cause **renal artery stenosis**.
- While renal artery stenosis can cause hypertension and renal impairment, the patient's long-standing diabetes and gradual progression make diabetic nephropathy a more probable cause.
*Apple-green birefringent lesions*
- This describes the characteristic staining of **amyloid deposits** with **Congo red stain** under polarized light.
- While amyloidosis can cause renal failure with proteinuria, it is less common than diabetic nephropathy in a patient with long-standing diabetes and the typical presentation described.
*Renal cortex necrosis*
- This is a rare and severe form of **acute kidney injury** often associated with conditions like severe sepsis, obstetric complications, or disseminated intravascular coagulation.
- The patient's history of gradual onset hypertension and diabetes, along with mild proteinuria and elevated creatinine, points to a chronic rather than acute process.
*Flea-bitten kidney*
- This describes the gross appearance of kidneys in **malignant hypertension**, showing petechial hemorrhages on the renal surface.
- While the patient has long-standing hypertension, the presentation suggests chronic kidney disease from diabetic nephropathy rather than acute malignant hypertension, which would present with markedly elevated blood pressure and acute kidney injury.
Atherosclerosis US Medical PG Question 10: A 73-year-old man with coronary artery disease and hypertension is brought to the emergency department by ambulance 90 minutes after the acute onset of substernal chest pain and dyspnea. He has smoked 2 packs of cigarettes daily for 52 years. Shortly after arriving at the hospital, he loses consciousness and is pulseless. Despite attempts at cardiopulmonary resuscitation, he dies. Examination of the heart at autopsy shows complete occlusion of the left anterior descending artery with a red thrombus overlying a necrotic plaque. Which of the following pathophysiologic mechanisms is most likely responsible for this patient's acute coronary condition?
- A. Influx of lipids into the endothelium
- B. Secretion of matrix metalloproteinases (Correct Answer)
- C. Release of platelet-derived growth factor
- D. Type III collagen deposition
- E. Proliferation of smooth muscle cells
Atherosclerosis Explanation: ***Secretion of matrix metalloproteinases***
- **Matrix metalloproteinases (MMPs)** degrade the **extracellular matrix** within the fibrous cap of an atherosclerotic plaque, leading to its **destabilization and rupture**.
- Plaque rupture then exposes the highly thrombogenic lipid core, initiating thrombus formation and acute coronary events like the **red thrombus** seen in the **left anterior descending artery (LAD)**.
*Influx of lipids into the endothelium*
- This process is characteristic of the **initial stages of atherosclerosis**, leading to **fatty streak formation**, not the acute plaque rupture and thrombosis described.
- While essential for plaque development, lipid influx alone does not directly explain aggressive plaque rupture and acute thrombus formation.
*Release of platelet-derived growth factor*
- **Platelet-derived growth factor (PDGF)** is primarily involved in **smooth muscle cell proliferation** and migration, contributing to plaque growth and thickening.
- Its role is more chronic and proliferative, not immediate plaque destabilization and rupture leading to acute thrombosis.
*Type III collagen deposition*
- **Type III collagen** is characteristic of early, developing atherosclerotic plaques and granulation tissue, contributing to plaque stability.
- Plaque vulnerability associated with rupture involves a **thin fibrous cap** with reduced **collagen content**, often due to increased collagen degradation.
*Proliferation of smooth muscle cells*
- **Smooth muscle cell proliferation** occurs during chronic atherosclerosis, contributing to the **fibrous cap formation** and overall plaque stability.
- In the context of acute plaque rupture, it is the *erosion* of the fibrous cap, often due to degradation, rather than proliferation, that is the immediate cause.
More Atherosclerosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.