Aneurysms and dissections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Aneurysms and dissections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Aneurysms and dissections US Medical PG Question 1: A 58-year-old man is brought to the emergency department by his family because of severe upper back pain, which he describes as ripping. The pain started suddenly 1 hour ago while he was watching television. He has hypertension for 13 years, but he is not compliant with his medications. He denies the use of nicotine, alcohol or illicit drugs. His temperature is 36.5°C (97.7°F), the heart rate is 110/min and the blood pressure is 182/81 mm Hg in the right arm and 155/71 mm Hg in the left arm. CT scan of the chest shows an intimal flap limited to the descending aorta. Intravenous opioid analgesia is started. Which of the following is the best next step in the management of this patient condition?
- A. Intravascular ultrasound
- B. Emergency surgical intervention
- C. Sublingual nitroglycerin
- D. Intravenous esmolol (Correct Answer)
- E. Oral metoprolol and/or enalapril
Aneurysms and dissections Explanation: ***Intravenous esmolol***
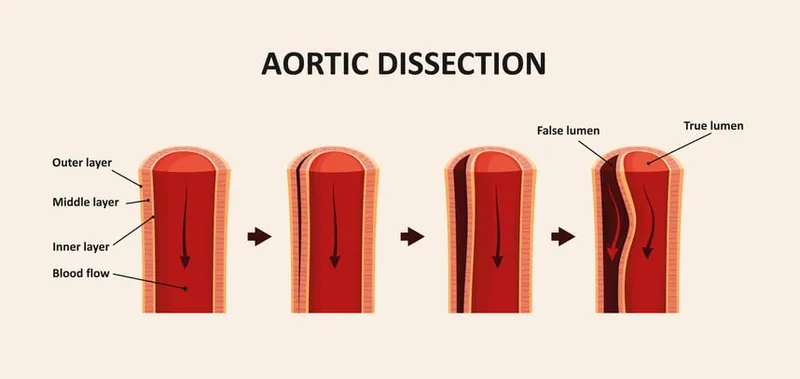
- This patient presents with an **acute aortic dissection** (descending aorta, Type B), characterized by sudden severe ripping back pain and a significant blood pressure difference between the arms [1]. The immediate priority is to reduce **heart rate** and **blood pressure** to decrease shear stress on the aortic wall and prevent progression of the dissection.
- **Intravenous beta-blockers** like esmolol are the first-line medical treatment for uncomplicated Type B aortic dissections, as they rapidly decrease heart rate and blood pressure, which helps to mitigate further aortic injury.
*Intravascular ultrasound*
- While intravascular ultrasound can provide detailed imaging of the aorta, it is an **invasive procedure** and not the immediate next step in managing an acute, hemodynamically unstable condition like aortic dissection where rapid blood pressure control is paramount.
- The patient already has a diagnostic CT scan confirming the intimal flap; thus, additional imaging during the acute stabilization phase is not typically the first priority over medical management [2].
*Emergency surgical intervention*
- **Emergency surgical intervention** is primarily indicated for **Type A aortic dissections** (involving the ascending aorta) or for complicated Type B dissections (e.g., malperfusion, rupture, rapid expansion) [1].
- This patient has an **uncomplicated Type B dissection** (limited to the descending aorta) that is initially managed medically with aggressive heart rate and blood pressure control.
*Sublingual nitroglycerin*
- **Nitroglycerin** primarily causes **vasodilation**, which can lower blood pressure but also induces reflex tachycardia, potentially increasing shear stress on the dissected aorta.
- It is **contraindicated** in acute aortic dissection as the increase in heart rate can worsen the dissection.
*Oral metoprolol and/or enalapril*
- **Oral medications** like metoprolol and enalapril are not suitable for the **initial acute management** of aortic dissection because their onset of action is too slow to achieve rapid and precise control of heart rate and blood pressure.
- **Intravenous agents** are required for immediate and titratable blood pressure and heart rate reduction in this emergency setting.
Aneurysms and dissections US Medical PG Question 2: A 68-year-old man presents for a screening ultrasound scan. He has been feeling well and is in his usual state of good health. His medical history is notable for mild hypertension and a 100-pack-year tobacco history. He has a blood pressure of 128/86 and heart rate of 62/min. Physical examination is clear lung sounds and regular heart sounds. On ultrasound, an infrarenal aortic aneurysm of 4 cm in diameter is identified. Which of the following is the best initial step for this patient?
- A. Reassurance
- B. Beta-blockers
- C. Urgent repair
- D. Surveillance (Correct Answer)
- E. Elective repair
Aneurysms and dissections Explanation: **Surveillance**
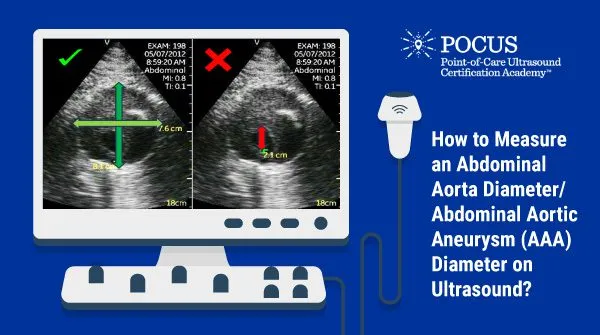
- An **infrarenal aortic aneurysm** of 4 cm in diameter in an asymptomatic patient is typically managed with **regular surveillance** to monitor for growth.
- Surgical intervention is generally reserved for aneurysms larger than 5.5 cm or those that are rapidly expanding or symptomatic.
*Reassurance*
- While it's important to provide reassurance, simply doing so without a concrete plan for follow-up would be inappropriate given the potential for **aneurysm expansion** and rupture.
- The patient's **tobacco history** is a significant risk factor for aneurysm progression and warrants monitoring.
*Beta-blockers*
- Beta-blockers may be part of the medical management for **hypertension** and could theoretically slow aneurysm growth by reducing pulsatile stress.
- However, they are not the primary **initial step** for an asymptomatic aneurysm of this size and do not replace the need for surveillance.
*Urgent repair*
- **Urgent repair** is indicated for symptomatic aneurysms, those that are rapidly expanding, or those showing signs of rupture or impending rupture, none of which are present here.
- A 4 cm aneurysm in an asymptomatic patient does not meet the criteria for **urgent intervention**.
*Elective repair*
- **Elective repair** is typically considered for aneurysms exceeding 5.5 cm in diameter or those that are symptomatic or rapidly growing.
- A 4 cm aneurysm is below the threshold for **elective repair** in an asymptomatic patient without other high-risk features.
Aneurysms and dissections US Medical PG Question 3: A 75-year-old Caucasian man presents to the emergency department with abdominal pain. The patient states he was at home eating dinner when he began to experience severe abdominal pain. The patient has a past medical history of diabetes, hypertension, and atherosclerosis. He lives at home alone, smokes cigarettes, and drinks 1 to 2 alcoholic drinks per day. The patient is given IV morphine and an ultrasound is obtained demonstrating a dilated abdominal aorta. The patient states that his father died of a similar finding and is concerned about his prognosis. Which of the following is the greatest risk factor for this patient's presentation?
- A. Male gender and age
- B. Caucasian race
- C. Cigarette smoking (Correct Answer)
- D. Family history
- E. Atherosclerosis
Aneurysms and dissections Explanation: ***Cigarette smoking***
- **Cigarette smoking** is the most significant modifiable risk factor for the development and expansion of **abdominal aortic aneurysms (AAAs)**, directly contributing to vascular inflammation and degradation.
- The patient's history of smoking suggests a strong causal link to his current presentation of a dilated aorta, which is highly indicative of an AAA.
*Male gender and age*
- While **male gender** and **advanced age (over 65)** are significant demographic risk factors for AAA, they are considered non-modifiable and less impactful than smoking in terms of risk magnitude.
- These factors increase predisposition but do not exert the same direct, damaging effect on the arterial wall as chronic smoking.
*Caucasian race*
- **Caucasian race** is a known demographic risk factor for AAA, with higher prevalence rates compared to other ethnic groups.
- However, this is a non-modifiable genetic predisposition and contributes less to the overall risk than modifiable lifestyle factors like smoking.
*Family history*
- A **family history** of AAA, as suggested by the patient's father having a similar condition, increases an individual's susceptibility.
- This is a significant non-modifiable risk factor, indicating genetic predisposition, but its overall impact on aneurysm formation and progression is typically less than that of active smoking.
*Atherosclerosis*
- **Atherosclerosis** is a strong associated condition with AAA, as both share common risk factors and pathology related to arterial wall degeneration.
- While atherosclerosis contributes to the overall vascular compromise, smoking specifically has a more direct and potent effect on promoting aneurysm formation and rupture independently.
Aneurysms and dissections US Medical PG Question 4: A 72-year-old man comes to the physician because of a 6-month history of intermittent dull abdominal pain that radiates to the back. He has smoked one pack of cigarettes daily for 50 years. His blood pressure is 145/80 mm Hg. Abdominal examination shows generalized tenderness and a pulsatile mass in the periumbilical region on deep palpation. Further evaluation of the affected blood vessel is most likely to show which of the following?
- A. Obliterative inflammation of the vasa vasorum
- B. Formation of giant cells in the tunica media
- C. Necrotizing inflammation of the entire vessel wall
- D. Fragmentation of elastic tissue in the tunica media (Correct Answer)
- E. Accumulation of foam cells in the tunica intima
Aneurysms and dissections Explanation: ***Fragmentation of elastic tissue in the tunica media***
- This patient's presentation with **intermittent dull abdominal pain radiating to the back**, a **pulsatile periumbilical mass**, and a history of **heavy smoking** is highly suggestive of an **abdominal aortic aneurysm (AAA)**.
- The pathological hallmark of AAA is **degradation and fragmentation of elastic tissue in the tunica media**, caused by chronic inflammation and increased activity of **matrix metalloproteinases (MMPs)**.
- This medial degeneration leads to **weakening of the vessel wall** and progressive **dilation**, ultimately forming an aneurysm.
- While atherosclerosis initiates the process, the actual aneurysm formation is characterized by this elastic tissue destruction in the media.
*Accumulation of foam cells in the tunica intima*
- This describes the **early lesion of atherosclerosis**, which is a **risk factor** for AAA development.
- However, when examining an **established AAA**, the predominant finding is not intimal foam cells but rather **medial degeneration** with elastic tissue fragmentation.
- Atherosclerosis is the underlying cause, but the question asks about findings in the affected vessel (the aneurysm itself).
*Obliterative inflammation of the vasa vasorum*
- This is characteristic of **syphilitic aortitis** (tertiary syphilis), which typically affects the **ascending thoracic aorta**.
- While syphilis can cause aneurysms, the patient's presentation and demographics are more consistent with atherosclerotic AAA.
*Formation of giant cells in the tunica media*
- This finding is associated with **giant cell arteritis** (temporal arteritis), which affects large and medium-sized arteries, particularly the temporal and ophthalmic arteries.
- It presents with headache, jaw claudication, and visual disturbances—features absent in this case.
*Necrotizing inflammation of the entire vessel wall*
- This describes **necrotizing vasculitis** such as **polyarteritis nodosa**, which affects medium-sized muscular arteries.
- While vasculitis can cause aneurysms, the clinical picture of AAA in an elderly smoker with atherosclerotic risk factors points to atherosclerotic pathogenesis, not primary vasculitis.
Aneurysms and dissections US Medical PG Question 5: A 71-year-old man with hypertension is taken to the emergency department after the sudden onset of stabbing abdominal pain that radiates to the back. He has smoked 1 pack of cigarettes daily for 20 years. His pulse is 120/min and thready, respirations are 18/min, and blood pressure is 82/54 mm Hg. Physical examination shows a periumbilical, pulsatile mass and abdominal bruit. There is epigastric tenderness. Which of the following is the most likely underlying mechanism of this patient's current condition?
- A. Mesenteric atherosclerosis
- B. Gastric mucosal ulceration
- C. Portal vein stasis
- D. Abdominal wall defect
- E. Aortic wall stress (Correct Answer)
Aneurysms and dissections Explanation: ***Aortic wall stress***
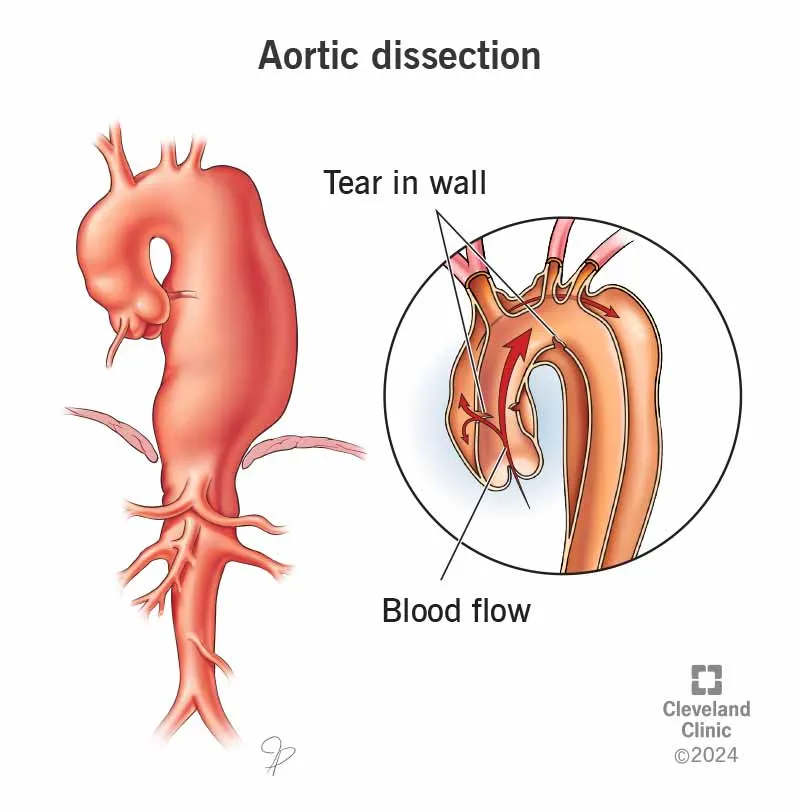
- The patient's presentation with **sudden onset of stabbing abdominal pain radiating to the back**, **hypotension** (BP 82/54 mm Hg), **tachycardia** (pulse 120/min), and a **pulsatile periumbilical mass** with an **abdominal bruit** is highly suggestive of a ruptured **abdominal aortic aneurysm (AAA)**.
- **Aortic wall stress**, often exacerbated by **hypertension** and **smoking**, leads to the progressive weakening and dilation of the aortic wall, eventually resulting in rupture.
*Mesenteric atherosclerosis*
- This condition typically causes **chronic abdominal pain** that is worse after eating (**postprandial angina**) due to inadequate blood supply to the intestines.
- It does not usually present with an acute, catastrophic event like **shock** and a **pulsatile mass**.
*Gastric mucosal ulceration*
- Ulceration can cause **epigastric pain**, but a ruptured ulcer would typically present with signs of **peritonitis** (rigidity, rebound tenderness) and potentially **hematemesis** or **melena**, which are not described.
- It would not cause a **pulsatile periumbilical mass** or the characteristic back pain of an AAA.
*Portal vein stasis*
- **Portal vein stasis** or **thrombosis** often leads to **portal hypertension**, **ascites**, and **gastrointestinal bleeding** from varices.
- It does not explain the acute onset of severe abdominal pain, hypotension, a pulsatile mass, or an abdominal bruit.
*Abdominal wall defect*
- An **abdominal wall defect**, such as a hernia, can cause localized pain and sometimes bowel obstruction.
- However, it does not account for the **hypotension**, **tachycardia**, **radiating pain to the back**, or the **pulsatile mass**, all of which point to a major vascular emergency.
Aneurysms and dissections US Medical PG Question 6: An 88-year-old woman with no significant medical history is brought to the emergency room by her daughter after a fall, where the woman lightly hit her head against a wall. The patient is lucid and complains of a mild headache. The daughter indicates that her mother did not lose consciousness after the fall. On exam, there are no focal neurological deficits, but you decide to perform a CT scan to be sure there is no intracranial bleeding. The CT scan is within normal limits and head MRI is performed (shown). Which of the following conditions has the most similar risk factor to this patient's condition?
- A. Pulmonary embolism
- B. Raynaud's phenomenon
- C. Prinzmetal's angina
- D. Abdominal aortic aneurysm
- E. Thoracic aortic aneurysm (Correct Answer)
Aneurysms and dissections Explanation: ***Thoracic aortic aneurysm***
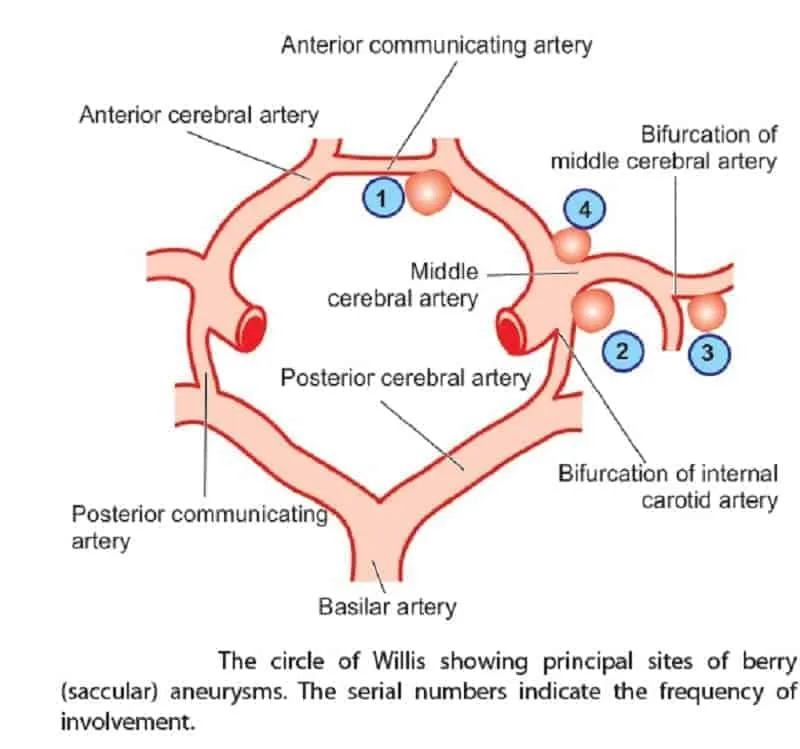
- The MRI images show numerous **microhemorrhages** (dark spots on the GRE/SWI sequences), indicative of **cerebral amyloid angiopathy (CAA)**, a common cause of lobar intracerebral hemorrhage in the elderly.
- CAA is most strongly associated with **advanced age** (the primary risk factor), and both CAA and **thoracic aortic aneurysm (TAA)** can be associated with **underlying connective tissue abnormalities** and vascular wall weakening processes.
- While the exact pathophysiology differs, both conditions involve progressive vascular wall degeneration that increases with age.
*Abdominal aortic aneurysm*
- While AAA is strongly associated with **advanced age**, **hypertension**, and **smoking**, it is primarily driven by **atherosclerotic degeneration** rather than the amyloid deposition seen in CAA.
- AAA has a particularly strong association with smoking (the most important modifiable risk factor), which is not characteristic of CAA.
*Pulmonary embolism*
- Primarily caused by **venous thromboembolism** (VTE) due to factors like immobility, surgery, cancer, and hypercoagulable states, which are distinct from CAA risk factors.
- While age is a risk factor for PE, the underlying mechanisms (thrombosis vs. vascular wall amyloid deposition) differ fundamentally.
*Raynaud's phenomenon*
- Characterized by **vasospasm** of small arteries and arterioles, typically triggered by cold or stress, and is often associated with connective tissue diseases.
- Its pathophysiology is unrelated to the progressive vascular wall degeneration and amyloid deposition seen in CAA.
*Prinzmetal's angina*
- Caused by **coronary artery spasm**, leading to transient myocardial ischemia, often occurring at rest and typically not associated with age-related vascular degeneration.
- The mechanism is localized vascular spasm rather than widespread degenerative arterial disease or amyloid deposition.
Aneurysms and dissections US Medical PG Question 7: A 55-year-old man presents to the emergency department for chest pain. He states that the pain started last night and has persisted until this morning. He describes the pain as in his chest and radiating into his back between his scapulae. The patient has a past medical history of alcohol abuse and cocaine abuse. He recently returned from vacation on a transatlantic flight. The patient has smoked 1 pack of cigarettes per day for the past 20 years. His temperature is 99.5°F (37.5°C), blood pressure is 167/118 mmHg, pulse is 120/min, and respirations are 22/min. Physical exam reveals tachycardia and clear air movement bilaterally on cardiopulmonary exam. Which of the following is also likely to be found in this patient?
- A. Pulmonary artery thrombus
- B. Coronary artery thrombus
- C. Elevated lipase
- D. Asymmetric blood pressures in the upper extremities (Correct Answer)
- E. Coronary artery vasospasm
Aneurysms and dissections Explanation: ***Asymmetric blood pressures in the upper extremities***
- The patient's presentation with **sudden-onset, severe, tearing chest pain radiating to the back**, combined with **hypertension** and **tachycardia**, is highly suggestive of an **aortic dissection**. Asymmetric blood pressures are a classic sign.
- Aortic dissection involves a tear in the intima of the aorta, leading to a false lumen that can compress branch arteries, causing **pulse deficits** or **limb ischemia**, resulting in pressure differences.
*Pulmonary artery thrombus*
- While a **transatlantic flight** is a risk factor for **pulmonary embolism (PE)**, the described chest pain is typically pleuritic and not usually severe or radiating to the back in this manner.
- PE often presents with **dyspnea** and **hypoxia**, which are not prominent features described here.
*Coronary artery thrombus*
- **Cocaine abuse**, **smoking**, and **hypertension** are risk factors for **myocardial infarction (MI)** due to **coronary artery thrombosis**. However, MI pain is typically crushing or constricting, and radiation to the back between the scapulae is less common than in dissection.
- The description of **tearing pain** is more characteristic of aortic dissection than MI.
*Elevated lipase*
- The patient's history of **alcohol abuse** and **cocaine abuse** are risk factors for **pancreatitis**, which presents with elevated lipase. However, pancreatitis pain is typically **epigastric** and radiates to the back, but it's usually steady, severe, and often associated with nausea/vomiting, not the tearing quality described.
- The acute, severe, radiating chest pain pattern is not typical for an initial presentation of pancreatitis.
*Coronary artery vasospasm*
- **Cocaine abuse** is a known trigger for **coronary artery vasospasm**, leading to angina or MI, and can cause chest pain.
- However, the pain from vasospasm is usually anginal in quality, often responsive to nitrates, and less likely to present with the severe, tearing, interscapular back pain and hemodynamic instability suggestive of aortic dissection.
Aneurysms and dissections US Medical PG Question 8: A 47-year-old man presents as a new patient at an outpatient clinic. He has never seen a physician before, but was motivated by his 40-year-old brother's recent heart attack and seeks to optimize his health. In particular, he read that uncontrolled atherosclerosis can lead to a heart attack. Which molecule is downregulated in response to the advent of atherosclerosis?
- A. Tumor necrosis factor
- B. Serotonin
- C. Nitric oxide (Correct Answer)
- D. Interleukin 1
- E. Thromboxane A2
Aneurysms and dissections Explanation: ***Nitric oxide***
- **Nitric oxide (NO)** is a potent **vasodilator** and **anti-inflammatory** molecule produced by endothelial cells. In atherosclerosis, endothelial dysfunction leads to reduced NO bioavailability.
- Decreased NO production contributes to vasoconstriction, increased platelet aggregation, and enhanced smooth muscle cell proliferation, all of which promote **atherosclerotic plaque formation** and progression.
*Tumor necrosis factor*
- **Tumor necrosis factor-alpha (TNF-α)** is a **pro-inflammatory cytokine** that plays a significant role in the pathogenesis of atherosclerosis.
- It is **upregulated** in response to atherosclerotic plaque formation, contributing to endothelial activation, leukocyte recruitment, and smooth muscle cell proliferation.
*Serotonin*
- **Serotonin (5-hydroxytryptamine)** is primarily known for its role as a neurotransmitter but also acts as a **vasoconstrictor** and promotes platelet aggregation.
- While it can be released from activated platelets in the context of vascular injury, it is not consistently **downregulated** in atherosclerosis; rather, its effects can contribute to disease progression.
*Interleukin 1*
- **Interleukin-1 (IL-1)**, particularly IL-1β, is a major **pro-inflammatory cytokine** critically involved in the immune response in atherosclerosis.
- It is **upregulated** in atherosclerotic plaques, contributing to systemic inflammation, endothelial dysfunction, and vascular smooth muscle cell activation.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is a potent **vasoconstrictor** and **platelet aggregator** produced by activated platelets.
- Its levels are **increased** in atherosclerosis, contributing to hypercoagulability and increased risk of thrombotic events like myocardial infarction.
Aneurysms and dissections US Medical PG Question 9: A 42-year-old man with systolic heart failure secondary to amyloidosis undergoes heart transplantation. The donor heart is obtained from a 17-year-old boy who died in a motor vehicle collision. Examination of the donor heart during the procedure shows a flat, yellow-white discoloration with an irregular border on the luminal surface of the aorta. A biopsy of this lesion is most likely to show which of the following?
- A. Apoptotic smooth muscle cells
- B. Necrotic cell debris
- C. Proteoglycan accumulation
- D. Collagen deposition
- E. Lipoprotein-laden macrophages (Correct Answer)
Aneurysms and dissections Explanation: ***Lipoprotein-laden macrophages***
- The description of a flat, yellow-white discolored lesion with an irregular border on the luminal surface of the aorta in a 17-year-old is classic for a **fatty streak**, the earliest lesion of **atherosclerosis**.
- Fatty streaks are histologically characterized by the accumulation of **macrophages that have ingested oxidized lipoproteins**, appearing as foam cells within the intima.
*Apoptotic smooth muscle cells*
- While apoptosis of various cell types, including smooth muscle cells, can occur in advanced atherosclerotic lesions, it is not the primary or defining feature of an early **fatty streak**.
- **Apoptosis** contributes to the necrotic core formation in later stages of plaque development, not the initial yellow-white discoloration of a fatty streak.
*Necrotic cell debris*
- **Necrotic cell debris** is a prominent feature of more advanced, **complicated atherosclerotic plaques**, forming the necrotic core.
- In a **fatty streak**, the cells are primarily viable foam cells, and significant necrosis is not yet present.
*Proteoglycan accumulation*
- **Proteoglycan accumulation** occurs in the arterial intima and is involved in the retention of lipoproteins, contributing to the development of atherosclerosis.
- However, the immediate and most characteristic histological finding of the **yellow-white discoloration** in a fatty streak is the lipid-laden macrophage.
*Collagen deposition*
- **Collagen deposition** is a key feature of the fibrous cap in **advanced atherosclerotic plaques**, laid down by migrating smooth muscle cells.
- It is not the primary histological characteristic of an early, flat, yellow-white **fatty streak**.
Aneurysms and dissections US Medical PG Question 10: A 73-year-old man with coronary artery disease and hypertension is brought to the emergency department by ambulance 90 minutes after the acute onset of substernal chest pain and dyspnea. He has smoked 2 packs of cigarettes daily for 52 years. Shortly after arriving at the hospital, he loses consciousness and is pulseless. Despite attempts at cardiopulmonary resuscitation, he dies. Examination of the heart at autopsy shows complete occlusion of the left anterior descending artery with a red thrombus overlying a necrotic plaque. Which of the following pathophysiologic mechanisms is most likely responsible for this patient's acute coronary condition?
- A. Influx of lipids into the endothelium
- B. Secretion of matrix metalloproteinases (Correct Answer)
- C. Release of platelet-derived growth factor
- D. Type III collagen deposition
- E. Proliferation of smooth muscle cells
Aneurysms and dissections Explanation: ***Secretion of matrix metalloproteinases***
- **Matrix metalloproteinases (MMPs)** degrade the **extracellular matrix** within the fibrous cap of an atherosclerotic plaque, leading to its **destabilization and rupture**.
- Plaque rupture then exposes the highly thrombogenic lipid core, initiating thrombus formation and acute coronary events like the **red thrombus** seen in the **left anterior descending artery (LAD)**.
*Influx of lipids into the endothelium*
- This process is characteristic of the **initial stages of atherosclerosis**, leading to **fatty streak formation**, not the acute plaque rupture and thrombosis described.
- While essential for plaque development, lipid influx alone does not directly explain aggressive plaque rupture and acute thrombus formation.
*Release of platelet-derived growth factor*
- **Platelet-derived growth factor (PDGF)** is primarily involved in **smooth muscle cell proliferation** and migration, contributing to plaque growth and thickening.
- Its role is more chronic and proliferative, not immediate plaque destabilization and rupture leading to acute thrombosis.
*Type III collagen deposition*
- **Type III collagen** is characteristic of early, developing atherosclerotic plaques and granulation tissue, contributing to plaque stability.
- Plaque vulnerability associated with rupture involves a **thin fibrous cap** with reduced **collagen content**, often due to increased collagen degradation.
*Proliferation of smooth muscle cells*
- **Smooth muscle cell proliferation** occurs during chronic atherosclerosis, contributing to the **fibrous cap formation** and overall plaque stability.
- In the context of acute plaque rupture, it is the *erosion* of the fibrous cap, often due to degradation, rather than proliferation, that is the immediate cause.
More Aneurysms and dissections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.