Pain management in labor US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pain management in labor. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pain management in labor US Medical PG Question 1: A 32-year-old homeless woman is brought to the emergency department by ambulance 30 minutes after the police found her on the sidewalk. On arrival, she is unresponsive. Her pulse is 76/min, respirations are 6/min, and blood pressure is 110/78 mm Hg. Examination shows cool, dry skin. The pupils are pinpoint and react sluggishly to light. Intravenous administration of a drug is initiated. Two minutes after treatment is started, the patient regains consciousness and her respirations increase to 12/min. The drug that was administered has the strongest effect on which of the following receptors?
- A. Ryanodine receptor
- B. 5-HT2A receptor
- C. M1 receptor
- D. GABAA receptor
- E. μ-receptor (Correct Answer)
Pain management in labor Explanation: ***μ-receptor***
- The patient's presentation with **unresponsiveness, pinpoint pupils, and respiratory depression** is classic for an **opioid overdose**.
- The rapid reversal of symptoms after drug administration indicates that the drug was an **opioid antagonist** like **naloxone**, which primarily acts on **μ-opioid receptors**.
*Ryanodine receptor*
- These receptors are primarily involved in **calcium release** from the sarcoplasmic reticulum in muscle cells, crucial for muscle contraction.
- They are targeted by drugs used in conditions like **malignant hyperthermia**, which is not indicated here.
*5-HT2A receptor*
- This receptor is a subtype of **serotonin receptors** and is a target for **antipsychotics** and some **hallucinogens**.
- While serotonin syndrome can cause altered mental status, it typically presents with **hyperthermia, myoclonus, and hypertension**, which are not seen in this patient.
*M1 receptor*
- These are **muscarinic acetylcholine receptors** found in the central nervous system and autonomic ganglia.
- Drugs acting on M1 receptors are involved in conditions like **Alzheimer's disease** (cholinesterase inhibitors) or **motion sickness** (anticholinergics), and are not relevant to opioid overdose.
*GABAA receptor*
- This receptor is the primary target for **benzodiazepines** and **barbiturates**, which cause central nervous system depression.
- While these drugs can cause respiratory depression and unresponsiveness, they typically do not cause **pinpoint pupils**, a hallmark of opioid overdose.
Pain management in labor US Medical PG Question 2: A 24-year-old woman, gravida 1, at 35 weeks gestation is admitted to the hospital with regular contractions and pelvic pressure for the last 5 hours. Her pregnancy has been uncomplicated and she has attended many prenatal appointments and followed the physician's advice about screening for diseases, laboratory testing, diet, and exercise. She has had no history of fluid leakage or bleeding. At the hospital, her temperature is 37.2°C (99.0°F), blood pressure is 108/60 mm Hg, pulse is 88/min, and respirations are 16/min. Cervical examination shows 60% effacement and 5 cm dilation with intact membranes. Cardiotocography shows a contraction amplitude of 220 MVU in 10 minutes. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Magnesium sulfate
- B. No pharmacotherapy at this time (Correct Answer)
- C. Dexamethasone
- D. Oxytocin
- E. Terbutaline
Pain management in labor Explanation: ***No pharmacotherapy at this time***
- The patient is at **35 weeks gestation** and in **active labor** (5 cm dilated, 60% effacement, regular contractions with adequate Montevideo units). At this gestational age, labor is typically allowed to progress without intervention unless there are complications.
- Pharmacotherapy to stop labor (tocolysis) or induce fetal lung maturity (corticosteroids) is generally not indicated at or beyond 34 weeks gestation in uncomplicated cases.
*Magnesium sulfate*
- This is primarily used for **fetal neuroprotection** in anticipated preterm birth before 32 weeks gestation, or as a **tocolytic** to inhibit contractions, neither of which is indicated here.
- The patient is 35 weeks, beyond the typical window for neuroprotection, and stopping labor is not appropriate given her advanced dilation and gestational age.
*Dexamethasone*
- **Corticosteroids** like dexamethasone are administered to accelerate **fetal lung maturity** in cases of anticipated preterm birth, typically between 24 and 34 weeks gestation.
- At 35 weeks, the benefits of corticosteroids for lung maturity are minimal and generally not recommended.
*Oxytocin*
- **Oxytocin** is used to **induce or augment labor** if contractions are inadequate or to prevent **postpartum hemorrhage**.
- This patient is already in active, effective labor with adequate contractions (220 MVU in 10 minutes), so oxytocin for augmentation is not needed.
*Terbutaline*
- **Terbutaline** is a **beta-agonist tocolytic** used to relax the uterus and stop preterm labor.
- Given the patient's gestational age of 35 weeks and the progression of her labor (5 cm dilated), stopping contractions is not the appropriate management.
Pain management in labor US Medical PG Question 3: Five minutes after initiating a change of position and oxygen inhalation, the oxytocin infusion is discontinued. A repeat CTG that is done 10 minutes later shows recurrent variable decelerations and a total of 3 uterine contractions in 10 minutes. Which of the following is the most appropriate next step in management?
- A. Restart oxytocin infusion
- B. Emergent Cesarean section
- C. Administer terbutaline
- D. Monitor without intervention
- E. Amnioinfusion (Correct Answer)
Pain management in labor Explanation: ***Amnioinfusion***
- **Recurrent variable decelerations** persisting after discontinuing oxytocin and changing maternal position often indicate **cord compression**, which can be relieved by amnioinfusion.
- Adding fluid to the amniotic cavity **cushions the umbilical cord**, reducing compression during uterine contractions.
*Restart oxytocin infusion*
- Reinitiating oxytocin would likely **worsen the recurrent variable decelerations** by increasing uterine contraction frequency and intensity, thereby exacerbating cord compression.
- The goal is to alleviate fetal distress, not to intensify uterine activity that is already causing issues.
*Emergent Cesarean section*
- While an emergent Cesarean section is indicated for **unresolved fetal distress**, it's usually considered after less invasive measures, such as amnioinfusion, have failed.
- There is still an opportunity for a simpler intervention to resolve the issue before resorting to surgery.
*Administer terbutaline*
- Terbutaline is a **tocolytic agent** used to reduce uterine contractions, which can be helpful in cases of tachysystole or hyperstimulation.
- In this scenario, the contraction frequency is low (3 in 10 minutes), so reducing contractions is not the primary aim; rather, the focus is on resolving the cord compression causing decelerations.
*Monitor without intervention*
- **Recurrent variable decelerations** are an concerning sign of **fetal distress** and require intervention to prevent potential harm to the fetus.
- Simply monitoring without intervention would be inappropriate and could lead to worsening fetal hypoxemia and acidosis.
Pain management in labor US Medical PG Question 4: A 33-year-old woman, gravida 2, para 1, at 26 weeks' gestation comes to the emergency department because of frequent contractions. The contractions are 40 seconds each, occurring every 2 minutes, and increasing in intensity. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her current medications include folic acid and a multivitamin. Her temperature is 36.9°C (98.4°F), heart rate is 88/min, and blood pressure is 126/76 mm Hg. Contractions are felt on the abdomen. There is clear fluid in the vulva and the introitus. The cervix is dilated to 5 cm, 70% effaced, and station of the head is -2. A fetal ultrasound shows polyhydramnios, a median cleft lip, and fused thalami. The corpus callosum, 3rd ventricle, and lateral ventricles are absent. The spine shows no abnormalities and there is a four chamber heart. Which of the following is the most appropriate next step in management?
- A. Initiate misoprostol therapy
- B. Allow vaginal delivery (Correct Answer)
- C. Perform dilation and evacuation
- D. Initiate nifedipine therapy
- E. Perform cesarean delivery
Pain management in labor Explanation: ***Allow vaginal delivery***
- The presence of severe fetal anomalies, including **holoprosencephaly** (median cleft lip, fused thalami, absent corpus callosum, 3rd and lateral ventricles), indicates that the fetus is **incompatible with life**.
- Given the prognosis, the most appropriate and safest approach for the mother is to **allow vaginal delivery**, as there is no benefit to delaying delivery or attempting a surgical intervention that might pose more risks to the mother.
*Initiate misoprostol therapy*
- **Misoprostol** is a prostaglandin analog used to induce labor or abortion, particularly in cases of uterine atony or to ripen the cervix.
- While it aids in cervical ripening and uterine contractions, the cervix is already 5 cm dilated and 70% effaced, indicating a **rapidly progressing labor** not requiring additional induction.
*Perform dilation and evacuation*
- **Dilation and evacuation (D&E)** is typically performed in the second trimester for fetal demise or termination of pregnancy, usually before 24 weeks' gestation.
- At 26 weeks' gestation with advanced labor and significant cervical dilation, D&E is a **high-risk procedure** for the mother and less appropriate than vaginal delivery.
*Initiate nifedipine therapy*
- **Nifedipine is a tocolytic** used to suppress preterm labor by relaxing the uterine muscles.
- Given the **lethal fetal anomalies** and the advanced stage of labor (5 cm dilated, 70% effaced, intense contractions), stopping labor would only prolong a non-viable pregnancy and increase maternal risk.
*Perform cesarean delivery*
- **Cesarean delivery** would expose the mother to surgical risks (e.g., infection, hemorrhage, future pregnancy complications) without any benefit to the fetus, who has anomalies **incompatible with survival**.
- A previous cesarean section does not preclude a vaginal delivery in this context, especially when **fetal viability is not a concern**.
Pain management in labor US Medical PG Question 5: A 24-year-old woman at 36 weeks pregnant presents to the emergency department with a headache and abdominal pain. The woman has no known past medical history and has inconsistently followed up with an obstetrician for prenatal care. Her temperature is 98.5°F (36.9°C), blood pressure is 163/101 mmHg, pulse is 90/min, respirations are 16/min, and oxygen saturation is 97% on room air. Prior to performing the physical exam, the patient experiences a seizure, which resolves after 60 seconds. Which of the following is the best management for this patient?
- A. Diazepam, magnesium, and continuous monitoring
- B. Magnesium and continuous monitoring
- C. Nifedipine and cesarean section
- D. Magnesium and cesarean section (Correct Answer)
- E. Magnesium and labetalol
Pain management in labor Explanation: **Magnesium and cesarean section**
- The patient's presentation with **headache**, **abdominal pain**, and **hypertension** followed by a **seizure** is classic for **eclampsia**, a severe complication of pre-eclampsia.
- **Magnesium sulfate** is the first-line treatment for seizure control and prevention in eclampsia, while **delivery (cesarean section)** is the definitive treatment since it removes the source of the disease (the placenta).
*Diazepam, magnesium, and continuous monitoring*
- While **magnesium** is correct for seizure management, **diazepam** is typically reserved as a second-line agent if magnesium is ineffective or contraindicated.
- The definitive management of eclampsia is delivery; continuous monitoring alone is insufficient without plans for delivery.
*Magnesium and continuous monitoring*
- **Magnesium** is indeed the critical first step for seizure management in eclampsia.
- However, continuous monitoring without addressing the underlying cause via **delivery** is not sufficient definitive management for eclampsia.
*Nifedipine and cesarean section*
- **Nifedipine** is an antihypertensive and can be used to manage severe hypertension in pregnancy, but it is not the primary treatment for active seizures or seizure prevention in eclampsia.
- While a **cesarean section** is appropriate for delivery, **magnesium** is crucial for immediate seizure control.
*Magnesium and labetalol*
- **Magnesium** is appropriate for seizure management.
- **Labetalol** is an antihypertensive agent used for severe hypertension in pregnancy, but it does not treat the seizure or the underlying eclampsia definitively; delivery is still required.
Pain management in labor US Medical PG Question 6: A 30-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the hospital for regular, painful contractions that have been increasing in frequency. Her pregnancy has been complicated by gestational diabetes treated with insulin. Pelvic examination shows the cervix is 50% effaced and 4 cm dilated; the vertex is at -1 station. Ultrasonography shows no abnormalities. A tocometer and Doppler fetal heart monitor are placed on the patient's abdomen. The fetal heart rate monitoring strip shows a baseline heart rate of 145/min with a variability of ≥ 15/min. Within a 20-minute recording, there are 7 uterine contractions, 4 accelerations, and 3 decelerations that have a nadir occurring within half a minute. The decelerations occur at differing intervals relative to the contractions. Which of the following is the most appropriate next step in the management of this patient?
- A. Vibroacoustic stimulation
- B. Routine monitoring (Correct Answer)
- C. Administer tocolytics
- D. Emergent cesarean delivery
- E. Placement of fetal scalp electrode
Pain management in labor Explanation: ***Routine monitoring***
- The presented FHR tracing exhibits a **normal baseline rate** (145/min), **moderate variability** (≥15/min), and the presence of **accelerations**, indicating a reassuring fetal status.
- The described decelerations are **variable decelerations** due to their sudden onset, nadir within 30 seconds, and variable relationship to contractions, which are generally benign unless prolonged, deep, or repetitive. Given the otherwise reassuring status, continued routine monitoring is appropriate.
*Vibroacoustic stimulation*
- This intervention is used to elicit **fetal accelerations** or movement during non-stress tests (NSTs) when the fetus is quiet or shows a non-reactive pattern.
- In this case, the fetus is already showing **accelerations** and moderate variability, so stimulation is not needed to assess fetal well-being.
*Administer tocolytics*
- **Tocolytics** are used to stop or slow down labor, typically in cases of preterm labor or uterine tachysystole causing fetal distress.
- This patient is at **38 weeks' gestation** and in active labor, and there are no signs of fetal distress warranting the cessation of contractions.
*Emergent cesarean delivery*
- **Emergent cesarean delivery** is indicated for acute fetal distress, such as prolonged decelerations, significant bradycardia, or absent variability in conjunction with other concerning FHR patterns.
- The FHR tracing described is largely reassuring with moderate variability and accelerations, and the variable decelerations are not indicative of immediate threat, making emergent delivery unnecessary.
*Placement of fetal scalp electrode*
- A **fetal scalp electrode** provides a more accurate and continuous measure of the FHR, often used when external monitoring is difficult or when there are concerns about the reliability of the tracing.
- While it can be useful in some situations, the current tracing is **interpretable as reassuring**, making invasive monitoring currently unnecessary.
Pain management in labor US Medical PG Question 7: A 37-year-old woman presents with an inability to void in the hours after giving birth to her first child via vaginal delivery. Her delivery involved the use of epidural anesthesia as well as pelvic trauma from the use of forceps. She is currently experiencing urinary leakage and complains of increased lower abdominal pressure. Which of the following is the most appropriate treatment for this patient’s condition?
- A. Pessary insertion
- B. Pelvic floor muscle strengthening
- C. Antimuscarinic drugs
- D. Midurethral sling
- E. Urethral catheterization (Correct Answer)
Pain management in labor Explanation: ***Urethral catheterization***
- The patient is experiencing **postpartum urinary retention** (inability to void) and **overflow incontinence** (urinary leakage due to bladder overdistension), alongside increased lower abdominal pressure, all indicative of an overfilled bladder.
- **Urethral catheterization** is the most appropriate immediate treatment to relieve bladder distension, prevent kidney damage, and allow bladder recovery.
*Pessary insertion*
- **Pessaries** are used for pelvic organ prolapse or stress urinary incontinence, not for acute postpartum urinary retention.
- They provide structural support but do not address the inability to void in an overdistended bladder.
*Pelvic floor muscle strengthening*
- **Pelvic floor exercises** are beneficial for stress incontinence or mild degrees of prolapse.
- They are contraindicated in acute urinary retention as they may worsen the inability to void if the issue is a failure of bladder contractility or urethral relaxation.
*Antimuscarinic drugs*
- **Antimuscarinics** relax the detrusor muscle and are used to treat overactive bladder symptoms (e.g., urgency, frequency).
- They would worsen bladder emptying in a patient with urinary retention.
*Midurethral sling*
- A **midurethral sling** is a surgical procedure for stress urinary incontinence.
- It is an invasive treatment for a chronic condition and is not appropriate for acute postpartum urinary retention.
Pain management in labor US Medical PG Question 8: A 27-year old primigravid woman at 37 weeks' gestation comes to the emergency department because of frequent contractions for 4 hours. Her pregnancy has been complicated by hyperemesis gravidarum which subsided in the second trimester. The contractions occur every 10–15 minutes and have been increasing in intensity and duration since onset. Her temperature is 37.1°C (98.8°F), pulse is 110/min, and blood pressure is 140/85 mm Hg. Uterine contractions are felt on palpation. Pelvic examination shows clear fluid in the vagina. The cervix is 50% effaced and 3 cm dilated. After 4 hours the cervix is 80% effaced and 6 cm dilated. Pelvic examination is inconclusive for the position of the fetal head. The fetal heart rate is reassuring. Which of the following is the most appropriate next step?
- A. Administer oxytocin
- B. Perform external cephalic version
- C. Administer misoprostol
- D. Perform Mauriceau-Smellie-Veit maneuver
- E. Perform ultrasonography (Correct Answer)
Pain management in labor Explanation: ***Perform ultrasonography***
- The examination notes that the **pelvic examination is inconclusive for the position of the fetal head**, which is a critical piece of information needed for safe delivery. **Ultrasonography** is the most appropriate next step to ascertain the fetal presentation and position, especially given the dilated cervix.
- Determining fetal position is essential to rule out **malpresentation**, such as **breech** or **transverse lie**, which would significantly impact the delivery plan and potentially necessitate a **cesarean section**.
*Administer oxytocin*
- **Oxytocin** is used to induce or augment labor when contractions are insufficient or labor is prolonged, but in this case, the cervix is progressing well (from 3 cm to 6 cm dilation in 4 hours), indicating **active labor**.
- Without knowing the fetal presentation, administering oxytocin could exacerbate issues if there's a **malpresentation**, potentially leading to **fetal distress** or **uterine rupture**.
*Perform external cephalic version*
- **External cephalic version (ECV)** is performed to change a **breech presentation** to a **cephalic presentation** by external manipulation, typically done before labor onset or early in labor at term.
- This patient is already in **active labor** with significant cervical dilation (6 cm), making ECV less likely to be successful and potentially increasing risks like **placental abruption** or **umbilical cord compression**.
*Administer misoprostol*
- **Misoprostol** is a prostaglandin analog used for **cervical ripening** and **labor induction** in cases where the cervix is unfavorable or labor needs to be initiated.
- This patient is already in **active labor** with progressive cervical dilation, making misoprostol unnecessary and potentially harmful due to the risk of **uterine hyperstimulation**.
*Perform Mauriceau-Smellie-Veit maneuver*
- The **Mauriceau-Smellie-Veit maneuver** is a technique used during a **vaginal breech delivery** to deliver the fetal head, specifically in cases of **frank or complete breech** that are being delivered vaginally.
- This maneuver is only performed *during* delivery of a breech baby, and the fetal position is currently unknown. It would be premature and inappropriate to consider this maneuver without first confirming a **breech presentation** and the decision for vaginal delivery.
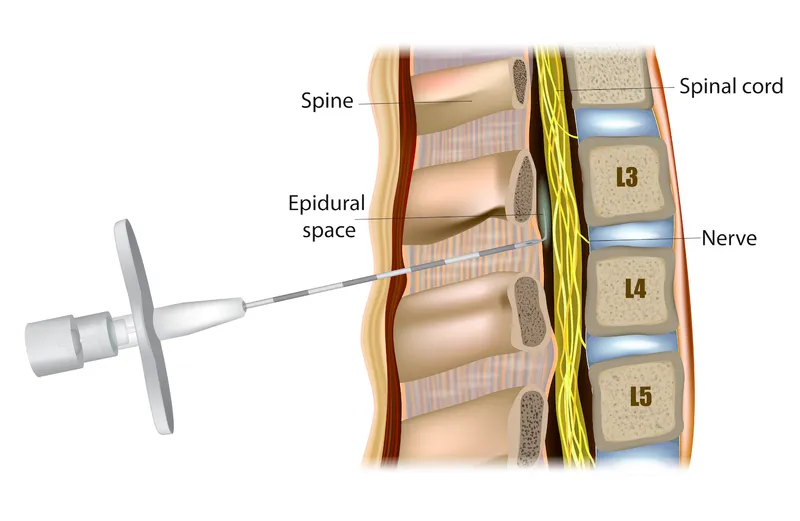
Pain management in labor US Medical PG Question 9: A 22-year-old primigravid woman at 41 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been uncomplicated. She has asthma treated with theophylline and inhaled corticosteroids. She has had 2 surgeries in the past to repair multiple lower limb and pelvis fractures that were the result of a car accident. She is otherwise healthy. Her temperature is 37.2°C (99°F) and blood pressure is 108/70 mm Hg. Examination shows the cervix is 100% effaced and 10 cm dilated; the vertex is at -4 station, with the occiput in the anterior position. Uterine activity is measured at 275 MVUs. Maternal pushing occurs during the contractions. Fetal heart tracing is 166/min and reactive with no decelerations. Epidural anesthesia is initiated for pain relief. After 4 hours of pushing, the vertex is found to be at -4 station, with increasing strength and rate of uterine contractions; fetal heart tracing shows late decelerations. Which of the following is the most likely cause of this patient's prolonged labor?
- A. Deep transverse arrest
- B. Insufficient uterine contraction
- C. Epidural anesthesia
- D. Cephalopelvic disproportion (Correct Answer)
- E. Inefficient maternal pushing
Pain management in labor Explanation: ***Cephalopelvic disproportion***
- The history of **multiple lower limb and pelvis fractures** from a car accident suggests a high likelihood of a **contracted or abnormally shaped pelvis**. This can lead to **cephalopelvic disproportion (CPD)**, where the fetal head cannot fit through the maternal pelvis despite adequate uterine contractions (275 MVUs).
- The combination of **prolonged labor** (4 hours of pushing with no descent), **vertex at -4 station** even after full dilation, increasing contraction strength, and new **late decelerations** (indicating fetal distress due to impaired oxygenation from prolonged compression) points towards an obstruction.
*Deep transverse arrest*
- This occurs when the fetal head rotates into the transverse diameter of the pelvis and fails to rotate anteriorly. While it causes **arrest of descent and dilation**, the primary issue is **malposition**, not a fundamental size mismatch.
- The occiput is described as in the **anterior position**, which does not immediately suggest deep transverse arrest.
*Insufficient uterine contraction*
- The uterine activity is measured at **275 MVUs**, which indicates **adequate contraction strength**. Insufficient contractions would typically be below 200 MVUs.
- While weak contractions can cause prolonged labor, the current uterine activity suggests this is not the primary problem.
*Epidural anesthesia*
- Epidural anesthesia can sometimes prolong the second stage of labor by reducing the urge to push or temporarily decreasing the effectiveness of pushing efforts. However, the patient's **strong uterine activity (275 MVUs)** and previous **pelvic fractures** make a mechanical obstruction (CPD) a more specific and likely cause of arrest in this scenario.
- Furthermore, the vertex remaining at -4 station for 4 hours despite strong contractions points to a physical barrier rather than just altered pushing dynamics.
*Inefficient maternal pushing*
- While inefficient maternal pushing can contribute to prolonged labor, the fetus remaining at -4 station for 4 hours with **strong uterine contractions (275 MVUs)** indicates that the issue is likely beyond just inadequate pushing efforts.
- The historical detail of **pelvic fractures** points more strongly to an anatomical obstruction rather than simply ineffective maternal exertion.
Pain management in labor US Medical PG Question 10: A 24-year-old primigravida at 28 weeks gestation presents to the office stating that she “can’t feel her baby kicking anymore.” She also noticed mild-to-moderate vaginal bleeding. A prenatal visit a few days ago confirmed the fetal cardiac activity by Doppler. The medical history is significant for GERD, hypertension, and SLE. The temperature is 36.78°C (98.2°F), the blood pressure is 125/80 mm Hg, the pulse is 70/min, and the respiratory rate is 14/min. Which of the following is the next best step in evaluation?
- A. Confirmation of cardiac activity by Doppler (Correct Answer)
- B. Order platelet count, fibrinogen, PT and PTT levels
- C. Abdominal delivery
- D. Speculum examination
- E. Misoprostol
Pain management in labor Explanation: ***Confirmation of cardiac activity by Doppler***
- The patient presents with **decreased fetal movement** and **vaginal bleeding** at 28 weeks, which are concerning signs for complications like **placental abruption** or **fetal demise**.
- The immediate priority is to assess **fetal viability** by confirming the presence of a **fetal heartbeat**, with **Doppler ultrasonography** being the quickest and most accessible method.
*Order platelet count, fibrinogen, PT and PTT levels*
- While **coagulation studies** are important in cases of significant vaginal bleeding, especially if **placental abruption** is suspected, they are not the *next best step*.
- Assessing **fetal well-being** takes precedence, as the presence or absence of a **fetal heart rate** will guide subsequent emergency management.
*Abdominal delivery*
- **Abdominal delivery (C-section)** is a definitive intervention and should only be considered *after* an immediate assessment of **fetal status** and maternal stability.
- Delivery at 28 weeks gestation would be considered **preterm**, and careful evaluation is needed before making such a critical decision.
*Speculum examination*
- A **speculum examination** is used to investigate the source of vaginal bleeding, assess the cervix, and rule out causes such as **cervical lesions** or **cervical dilation**.
- However, given the *decreased fetal movement* and the potential for severe obstetrical emergencies, **fetal viability** must be confirmed first.
*Misoprostol*
- **Misoprostol** is a **prostaglandin analog** used to induce cervical ripening and uterine contractions, primarily for **labor induction** or **abortion**.
- It is not indicated as an initial diagnostic or therapeutic step in a patient with *decreased fetal movement* and *vaginal bleeding* without a clear diagnosis or indication for delivery.
More Pain management in labor US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.