Operative vaginal delivery US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Operative vaginal delivery. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Operative vaginal delivery US Medical PG Question 1: A 26-year-old primigravid woman at 39 weeks' gestation is admitted to the hospital in active labor. Pregnancy was complicated by mild oligohydramnios detected a week ago, which was managed with hydration. Her pulse is 92/min, respirations are 18/min, and blood pressure is 134/76 mm Hg. Pelvic examination shows 100% cervical effacement and 10 cm cervical dilation; the vertex is at 0 station. Cardiotocography is shown. Which of the following is the most appropriate next step in management?
- A. Maternal repositioning and oxygen administration (Correct Answer)
- B. Emergent cesarean section
- C. Elevation of the fetal head
- D. Reassurance
- E. Rapid amnioinfusion
Operative vaginal delivery Explanation: ***Maternal repositioning and oxygen administration***
- The cardiotocography shows **variable decelerations**, which are characterized by an abrupt decrease in fetal heart rate, often U, V, or W shaped, and not consistently related to contractions.
- Initial management for variable decelerations, common in cases of **oligohydramnios**, involves conservative measures like **maternal repositioning** (e.g., left lateral, right lateral, hands and knees) to relieve umbilical cord compression and administering **oxygen** to improve fetal oxygenation.
*Emergent cesarean section*
- While severe, unremitting variable decelerations unresponsive to conservative measures may warrant a cesarean section, the current tracing does not indicate an **immediate obstetric emergency** requiring such an invasive procedure as the first step.
- An emergent cesarean section is reserved for situations of **persistent non-reassuring fetal status** despite intervention.
*Elevation of the fetal head*
- Elevating the fetal head is typically done to **relieve umbilical cord prolapse** during a vaginal examination, a condition that might present with sudden, profound decelerations or bradycardia, which is not clearly depicted as the primary issue here.
- This maneuver is an intervention for a specific obstetric emergency and does not address the underlying pathophysiology of variable decelerations due to cord compression.
*Reassurance*
- The presence of **variable decelerations** indicates **umbilical cord compression** and potential fetal compromise, requiring active intervention rather than passive reassurance.
- Reassurance alone is insufficient and inappropriate when there are signs of **fetal distress** on the cardiotocograph.
*Rapid amnioinfusion*
- **Amnioinfusion** can be considered for **recurrent variable decelerations** due to oligohydramnios that are unresponsive to maternal repositioning and oxygen.
- It is generally not the *first* step, as less invasive measures should be attempted first. Moreover, rapid amnioinfusion carries its own risks and should be carefully considered.
Operative vaginal delivery US Medical PG Question 2: A 34-year-old pregnant woman with unknown medical history is admitted to the hospital at her 36th week of gestation with painful contractions. She received no proper prenatal care during the current pregnancy. On presentation, her vital signs are as follows: blood pressure is 110/60 mm Hg, heart rate is 102/min, respiratory rate is 23/min, and temperature is 37.0℃ (98.6℉). Fetal heart rate is 179/min. Pelvic examination shows a closed non-effaced cervix. During the examination, the patient experiences a strong contraction accompanied by a high-intensity pain after which contractions disappear. The fetal heart rate becomes 85/min and continues to decrease. The fetal head is now floating. Which of the following factors would most likely be present in the patient’s history?
- A. Fundal cesarean delivery (Correct Answer)
- B. Adenomyosis
- C. Intrauterine synechiae
- D. Multiple vaginal births
- E. Postabortion metroendometritis
Operative vaginal delivery Explanation: ***Fundal cesarean delivery***
- The sudden onset of intense pain followed by cessation of contractions, fetal bradycardia, and a floating fetal head in a woman with a prior Cesarean section scar is highly suggestive of **uterine rupture**.
- A previous **classical or fundal Cesarean section** scar carries the highest risk of rupture in subsequent pregnancies due to the incision extending into the contractile upper uterine segment.
*Adenomyosis*
- **Adenomyosis** involves the presence of endometrial tissue within the myometrium, which can cause heavy, painful periods and chronic pelvic pain, but it doesn't directly predispose to uterine rupture during labor.
- While it can complicate pregnancy with an increased risk of preterm birth or miscarriage, it is not associated with the acute presentation described.
*Intrauterine synechiae*
- **Intrauterine synechiae**, or Asherman's syndrome, are adhesions within the uterine cavity, often resulting from endometrial trauma.
- They primarily cause infertility, recurrent pregnancy loss, or abnormal placentation (like placenta accreta), but not uterine rupture.
*Multiple vaginal births*
- A history of **multiple vaginal births** generally *reduces* the risk of uterine rupture in subsequent pregnancies as the cervix and lower uterine segment are often more compliant.
- While prolonged labor or instrumental delivery can rarely increase rupture risk, it's not a primary risk factor like a prior classical Cesarean.
*Postabortion metroendometritis*
- **Postabortion metroendometritis** is an infection of the uterus after an abortion.
- While it can lead to complications such as Asherman's syndrome or infertility, it does not typically increase the risk of uterine rupture in a subsequent pregnancy in the manner described.
Operative vaginal delivery US Medical PG Question 3: A 36-year-old woman, gravida 3, para 2, at 37 weeks' gestation comes to the emergency department because of sparse vaginal bleeding for 3 hours. She also noticed the bleeding 3 days ago. She has had no prenatal care. Both of her previous children were delivered by lower segment transverse cesarean section. Her temperature is 37.1°C (98.8°F), pulse is 90/min, respirations are 16/min, and blood pressure is 110/80 mm Hg. The abdomen is nontender, and no contractions are felt. Examination shows that the fetus is in a vertex presentation. The fetal heart rate is 160/min and shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Perform cesarean delivery
- B. Perform transvaginal sonography (Correct Answer)
- C. Perform Kleihauer-Betke test
- D. Perform pelvic examination
- E. Conduct contraction stress test
Operative vaginal delivery Explanation: ***Perform transvaginal sonography***
- The history of **previous cesarean sections** and **painless vaginal bleeding** raises suspicion for **placenta previa**.
- **Transvaginal sonography** is the gold standard for diagnosing placenta previa, as it accurately visualizes the relationship between the placenta and the cervical os without increasing bleeding risk.
*Perform cesarean delivery*
- While a cesarean delivery may eventually be necessary if **placenta previa** is confirmed, it is premature to proceed without a definitive diagnosis.
- An immediate cesarean delivery is indicated only in cases of **heavy, uncontrolled bleeding** or fetal distress, neither of which is present here.
*Perform Kleihauer-Betke test*
- The **Kleihauer-Betke test** measures the amount of fetal hemoglobin transferred into the maternal bloodstream for quantifying **fetomaternal hemorrhage**, which is typically performed after a potential placental abruption or trauma.
- This test is not primarily used for diagnosing the **cause of vaginal bleeding** in this context and would not identify placenta previa.
*Perform pelvic examination*
- A **digital pelvic examination** is **contraindicated** in cases of suspected placenta previa due to the risk of exacerbating bleeding and potentially causing **massive hemorrhage**.
- Even a speculum examination should generally be deferred until a sonogram has ruled out placenta previa to avoid disturbing the placenta.
*Conduct contraction stress test*
- A **contraction stress test** assesses **fetal well-being** in response to uterine contractions and is used to evaluate uteroplacental insufficiency.
- It does not help in diagnosing the cause of **vaginal bleeding** and is not the appropriate first step in a patient with suspected placenta previa.
Operative vaginal delivery US Medical PG Question 4: Three hours after the onset of labor, a 39-year-old woman, gravida 2, para 1, at 40 weeks' gestation has sudden worsening of abdominal pain and vaginal bleeding. 18 months ago her first child was delivered by a lower segment transverse cesarean section because of cephalopelvic disproportion. Her temperature is 37.5°C (99.5°F), pulse is 120/min, respirations are 20/min, and blood pressure is 90/50 mm Hg. Examination shows abdominal tenderness and the absence of uterine contractions. The cervix is 100% effaced and 10 cm dilated; the vertex is at -3 station. An hour before, the vertex was at 0 station. Cardiotocography shows fetal bradycardia, late decelerations, and decreased amplitude of uterine contractions. Which of the following is the most specific feature of this patient's condition?
- A. Loss of fetal station (Correct Answer)
- B. Fetal distress
- C. Abdominal tenderness
- D. Absent uterine contractions
- E. Hemodynamic instability
Operative vaginal delivery Explanation: ***Loss of fetal station***
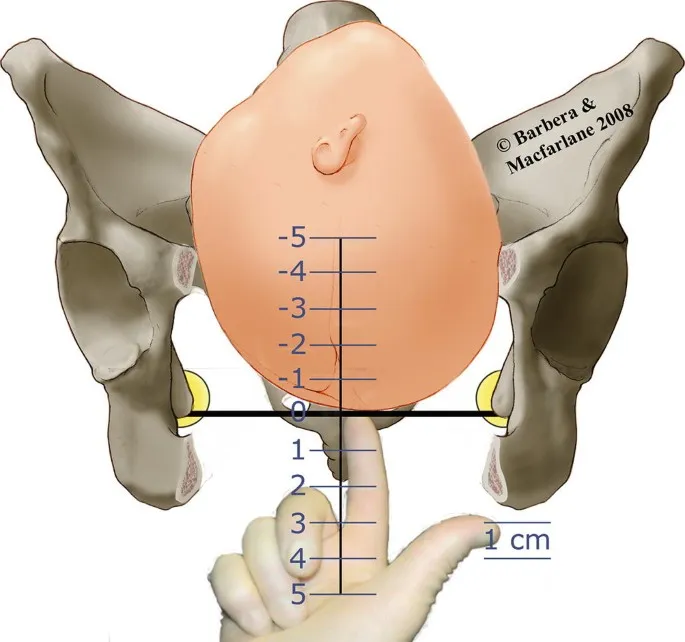
- The sudden **retraction of the presenting part** (vertex moving from 0 to -3 station) after a period of labor progression is a classical and highly specific sign of **uterine rupture**.
- This occurs because the uterus tears, allowing the fetus to partially or wholly slip out of the birth canal into the abdominal cavity.
*Fetal distress*
- While fetal bradycardia and late decelerations indicate **fetal distress**, this is a common finding in many obstetric emergencies, including placental abruption and cord prolapse, and is not specific to uterine rupture.
- Fetal distress reflects the immediate impact on the fetus but doesn't pinpoint the exact maternal pathology.
*Abdominal tenderness*
- **Abdominal tenderness** is a general symptom that can be present in various conditions such as placental abruption, chorioamnionitis, or even normal labor with strong contractions, making it non-specific for uterine rupture.
- The type of tenderness and its severity can vary, but by itself, it does not confirm a uterine rupture.
*Absent uterine contractions*
- The cessation of uterine contractions is a significant finding in uterine rupture, as the uterus can no longer effectively contract to expel the fetus.
- However, contractions can also decrease or become absent in cases of maternal exhaustion, failed induction, or excessive analgesia, thus not being entirely specific to rupture.
*Hemodynamic instability*
- The patient's **hypotension** (90/50 mm Hg) and **tachycardia** (120/min) indicate significant blood loss and **hypovolemic shock**, which commonly occur with uterine rupture.
- However, hemodynamic instability can also be seen in other severe obstetric hemorrhages like placental abruption or postpartum hemorrhage from other causes, making it a sensitive but non-specific indicator.
Operative vaginal delivery US Medical PG Question 5: A 4430-g (9-lb 10-oz) male newborn is delivered at term to a 27-year-old woman, gravida 2, para 1. The second stage of labor was prolonged and required vacuum-assisted vaginal delivery. Apgar scores are 9 and 10 at 1 and 5 minutes, respectively. Examination of the neonate 2 hours later shows a soft, nonpulsatile swelling over the left parietal bone that does not cross suture lines. Vital signs are within normal limits. The pupils are equal and reactive to light. The lungs are clear to auscultation. Heart sounds are normal. The spine is normal. Which of the following is the most likely diagnosis?
- A. Subgaleal hemorrhage
- B. Epidermoid cyst
- C. Lipoma
- D. Cephalohematoma (Correct Answer)
- E. Encephalocele
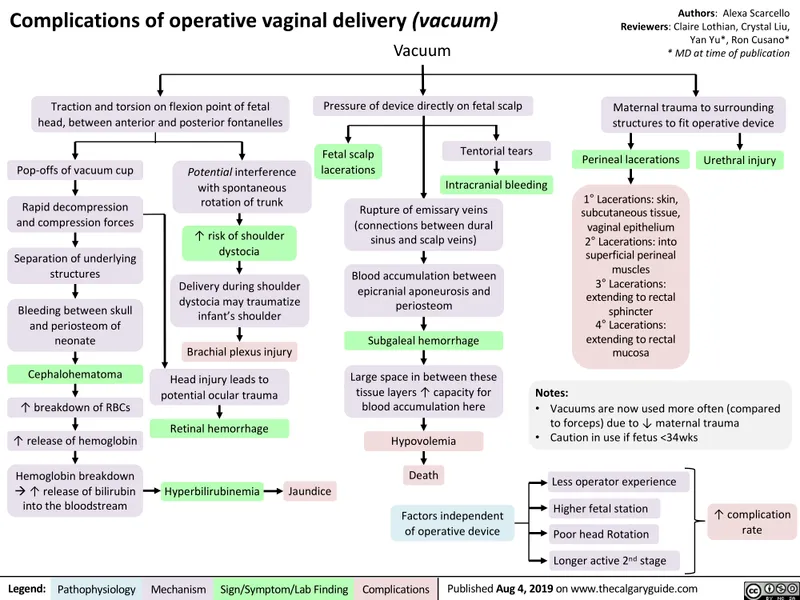
Operative vaginal delivery Explanation: ***Cephalohematoma***
- This is characterized by a **subperiosteal hemorrhage** that is typically contained by the fetal skull sutures, explaining why the swelling does not cross suture lines.
- It often results from **capillary damage** during prolonged or assisted deliveries, such as the vacuum-assisted delivery in this case, and frequently presents hours after birth.
*Subgaleal hemorrhage*
- A **subgaleal hemorrhage** involves bleeding into the potential space between the **galea aponeurotica** and the periosteum, which is not limited by suture lines and can spread across the entire scalp.
- This type of hemorrhage would present with a more diffuse, fluctuant swelling that **crosses suture lines** and can lead to significant blood loss and hypovolemic shock.
*Epidermoid cyst*
- An **epidermoid cyst** is a benign, congenital lesion that results from the sequestration of epidermal cells during neural tube closure.
- These cysts are typically present at birth or early infancy as a **fixed, firm nodule** and do not involve acute bleeding or arise due to birth trauma.
*Lipoma*
- A **lipoma** is a benign tumor composed of mature adipose (fat) tissue.
- It would present as a **soft, movable mass** that is usually present from birth or develops over time, and would not be an acute consequence of birth trauma or a prolonged second stage of labor.
*Encephalocele*
- An **encephalocele** is a neural tube defect characterized by the protrusion of brain tissue and/or meninges through a defect in the skull.
- This condition is typically present at birth as a **pulsatile, soft, reducible mass**, and often involves neurological deficits, which are not described in this otherwise healthy neonate.
Operative vaginal delivery US Medical PG Question 6: Immediately following prolonged delivery of the placenta at 40 weeks gestation, a 32-year-old multiparous woman develops vaginal bleeding. Other than mild asthma, the patient’s pregnancy has been uncomplicated. She has attended many prenatal appointments and followed the physician's advice about screening for diseases, laboratory testing, diet, and exercise. Previous pregnancies were uncomplicated. She has no history of a serious illness. She is currently on intravenous infusion of oxytocin. Her temperature is 37.2°C (99.0°F), blood pressure is 108/60 mm Hg, pulse is 88/min, and respirations are 17/min. Uterine palpation reveals a soft enlarged fundus that extends above the umbilicus. Based on the assessment of the birth canal and placenta, which of the following options is the most appropriate initial step in patient management?
- A. Intramuscular carboprost
- B. Manual exploration of the uterus
- C. Discontinuing oxytocin
- D. Intravenous methylergonovine
- E. Uterine fundal massage (Correct Answer)
Operative vaginal delivery Explanation: ***Uterine fundal massage***
- The patient presents with **postpartum hemorrhage** indicated by vaginal bleeding and a **soft, enlarged fundus** after placental delivery, suggesting **uterine atony**.
- **Uterine fundal massage** is the **first-line intervention** to encourage uterine contraction and reduce bleeding by expelling clots and compressing vessels.
*Intramuscular carboprost*
- **Carboprost** is a **prostaglandin F2 alpha analog** used to treat **uterine atony** when initial measures like uterine massage and oxytocin are insufficient.
- It is contraindicated in patients with **asthma** due to its bronchoconstrictive effects, which this patient has.
*Manual exploration of the uterus*
- **Manual exploration of the uterus** is indicated when there is suspicion of **retained placental fragments** or **uterine rupture**.
- While these can cause postpartum hemorrhage, the primary finding of a soft, boggy uterus points more strongly to atony, making massage the immediate priority.
*Discontinuing oxytocin*
- The patient is already on an **intravenous oxytocin infusion**, which is a uterotonic agent used to prevent and treat uterine atony.
- Discontinuing it would worsen **uterine atony** and increase blood loss, directly contradicting the goal of management.
*Intravenous methylergonovine*
- **Methylergonovine** is an **ergot alkaloid** used to treat **uterine atony**, but it is contraindicated in patients with **hypertension**, which is not explicitly present here, but it is a potent vasoconstrictor and second-line.
- It is often used as a **second-line agent** if oxytocin and massage are ineffective and there are no contraindications.
Operative vaginal delivery US Medical PG Question 7: A 30-year-old woman, gravida 2 para 1, at 39 weeks gestation presents to the hospital with painful contractions and a rupture of membranes. She reports that the contractions started a couple hours ago and are now occurring every 4 minutes. She is accompanied by her husband who states, “her water broke an hour ago before we left for the hospital." The patient denies vaginal bleeding, and fetal movements are normal. The patient has attended all her pre-natal visits without pregnancy complications. She has no chronic medical conditions and takes only pre-natal vitamins. Her blood pressure is 110/75 mm Hg and pulse is 82/min. A fetal heart rate tracing shows a pulse of 140/min with moderate variability and no decelerations. Cervical examination reveals a cervix that is 7 cm dilated and 100% effaced with the fetal head at -1 station. The patient forgoes epidural anesthesia. During which of the following scenarios should a cesarean delivery be considered for this patient?
- A. Cervix is 7 cm dilated and fetal head is at 0 station after 4 hours, with contractions every 2 minutes (Correct Answer)
- B. Cervix is 7 cm dilated and fetal head is at -1 station after 2 hours with contractions every 7 minutes
- C. Cervix is 9 cm dilated and fetal head is at -1 station after 3 hours, with contractions every 3 minutes
- D. Cervix is 10 cm dilated and fetal head is at +1 station after 2 hours, with contractions every 2 minutes
- E. Cervix is 7 cm dilated and fetal head is at 0 station after 1 hour, with contractions every 5 minutes
Operative vaginal delivery Explanation: ***Cervix is 7 cm dilated and fetal head is at 0 station after 4 hours, with contractions every 2 minutes***
- This scenario describes **arrest of active phase of labor** in a **multiparous woman**, defined as no cervical change for at least 4 hours with adequate contractions (every 2-3 minutes) or at least 6 hours with inadequate contractions.
- The patient started at 7 cm dilation and, after 4 hours of strong contractions, has shown no further cervical change, indicating failed labor progression and warranting C-section.
*Cervix is 7 cm dilated and fetal head is at -1 station after 2 hours with contractions every 7 minutes*
- This still represents the **active phase of labor** (from 6 cm dilation onwards), but the contractions are **inadequate** (every 7 minutes) and the duration of observation is too short to diagnose an arrest (2 hours vs. 4 hours for multiparous).
- The appropriate step would be to **augment labor** (e.g., with oxytocin) rather than proceed directly to C-section.
*Cervix is 9 cm dilated and fetal head is at -1 station after 3 hours, with contractions every 3 minutes*
- The patient has progressed from 7 cm to 9 cm, indicating **cervical change**, and contractions are adequate.
- This is not an arrest of labor; she is nearing full dilation and likely progressing appropriately.
*Cervix is 10 cm dilated and fetal head is at +1 station after 2 hours, with contractions every 2 minutes*
- This scenario describes the **second stage of labor** (complete cervical dilation), where the focus shifts to fetal descent. The fetal head has already descended to +1 station and contractions are adequate.
- While prolonged second stage can lead to C-section, the general threshold for intervention in a multiparous woman with epidural is 3 hours, and without epidural, it's 2 hours. This patient is at 2 hours and progressing, so a C-section is not immediately indicated.
*Cervix is 7 cm dilated and fetal head is at 0 station after 1 hour, with contractions every 5 minutes*
- This is still the **active phase of labor**, but the observation period (1 hour) is too short to diagnose an arrest of labor, even with inadequate contractions (every 5 minutes).
- The first step would be to ensure **adequate uterine activity** and observe for a longer period before considering a C-section.
Operative vaginal delivery US Medical PG Question 8: A 63-year-old woman with a past medical history significant for hypertension presents to the outpatient clinic for evaluation of vaginal dryness, loss of libido, and hot flashes. These symptoms have been progressively worsening over the past 3 months. Her vital signs are: blood pressure 131/81 mm Hg, pulse 68/min, and respiratory rate 16/min. She is afebrile. On further review of systems, she endorses having irregular periods for almost a year, and asks if she has begun menopause. Which of the following parameters is required to formally diagnosis menopause in this patient?
- A. Increased serum follicle-stimulating hormone (FSH)
- B. Increased serum luteinizing hormone (LH)
- C. Cessation of menses for at least 12 months (Correct Answer)
- D. Pelvic ultrasound demonstrating decreased follicular activity
- E. Increased total cholesterol
Operative vaginal delivery Explanation: ***Cessation of menses for at least 12 months***
- The formal diagnosis of **menopause** is clinical, defined as 12 consecutive months of **amenorrhea** in the absence of other physiological or pathological causes.
- This criterion indicates the **cessation of ovarian function** without requiring lab tests, especially in women over 40.
*Increased serum follicle-stimulating hormone (FSH)*
- While an **elevated FSH level** is a biochemical indicator of declining ovarian function, it is not strictly required for a clinical diagnosis of menopause, particularly in older women with typical symptoms and amenorrhea.
- FSH levels can fluctuate during the **perimenopausal period**, making a single measurement less definitive than the clinical criterion of 12 months without menses.
*Increased serum luteinizing hormone (LH)*
- Similar to FSH, **LH levels** typically rise during menopause due to reduced estrogen feedback, but an elevated LH is not part of the formal clinical diagnostic criteria for menopause.
- The **FSH-to-LH ratio** can also be used, but the 12-month amenorrhea rule remains the primary diagnostic standard.
*Pelvic ultrasound demonstrating decreased follicular activity*
- A pelvic ultrasound can show **decreased ovarian volume** and a lack of developing follicles, indicating reduced ovarian activity, but this is not a required diagnostic parameter for menopause.
- Clinical history and the 12-month cessation of menses are sufficient for diagnosis, making **imaging studies** generally unnecessary unless there are other concerns.
*Increased total cholesterol*
- While **elevated cholesterol levels** can be associated with menopause due to changes in estrogen, it is a metabolic consequence or associated risk factor, not a diagnostic criterion for menopause itself.
- Menopause can lead to an increased risk of **cardiovascular disease**, which includes dyslipidemia, but this is a secondary effect, not a primary diagnostic marker.
Operative vaginal delivery US Medical PG Question 9: A 37-year-old woman, gravida 2, para 1, at 35 weeks' gestation is brought to the emergency department for the evaluation of continuous, dark, vaginal bleeding and abdominal pain for one hour. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. The patient has a history of hypertension and has been noncompliant with her hypertensive regimen. Her medications include methyldopa, folic acid, and a multivitamin. Her pulse is 90/min, respirations are 16/min, and blood pressure is 145/90 mm Hg. The abdomen is tender, and hypertonic contractions can be felt. There is blood on the vulva, the introitus, and on the medial aspect of both thighs. The fetus is in a breech presentation. The fetal heart rate is 180/min with recurrent decelerations. Which of the following is the cause of fetal compromise?
- A. Rupture of the uterus
- B. Placental tissue covering the cervical os
- C. Rupture of aberrant fetal vessels
- D. Abnormal position of the fetus
- E. Detachment of the placenta (Correct Answer)
Operative vaginal delivery Explanation: ***Detachment of the placenta***
- The presentation of **continuous, dark vaginal bleeding**, **abdominal pain**, and **hypertonic contractions** in a pregnant woman with hypertension strongly indicates **placental abruption**.
- **Fetal compromise**, evidenced by a fetal heart rate of 180/min with recurrent decelerations, results from the compromised oxygen and nutrient exchange due to placental detachment.
*Rupture of the uterus*
- Uterine rupture typically presents with **sudden sharp abdominal pain**, **vaginal bleeding**, and often **cessation of uterine contractions**, which is contradicted by hypertonic contractions.
- A previous C-section scar is a risk factor, but the clinical picture with continuous dark bleeding and hypertonic contractions points more strongly to abruption.
*Placental tissue covering the cervical os*
- This describes **placenta previa**, which typically causes **painless, bright red vaginal bleeding** and usually does not present with abdominal pain or hypertonic contractions.
- The characteristics of pain and dark bleeding make placenta previa less likely.
*Rupture of aberrant fetal vessels*
- This condition, known as **vasa previa**, involves the rupture of fetal blood vessels, leading to **fetal blood loss** and rapid fetal compromise.
- However, the presenting symptoms usually include **sudden onset of bleeding with concurrent fetal bradycardia** or distress, and the vaginal bleeding is typically bright red fetal blood, not dark maternal blood as described.
*Abnormal position of the fetus*
- An abnormal fetal position, such as **breech presentation**, can complicate delivery but does not directly cause dark vaginal bleeding, abdominal pain, or hypertonic uterine contractions.
- While the fetus is breech, this finding does not explain the acute maternal symptoms or the signs of placental compromise.
Operative vaginal delivery US Medical PG Question 10: A 57-year-old, multiparous, woman comes to the physician because of urinary leakage for the past 6 months. She involuntarily loses a small amount of urine after experiencing a sudden, painful sensation in the bladder. She has difficulty making it to the bathroom in time, and feels nervous when there is no bathroom nearby. She also started having to urinate at night. She does not have hematuria, abdominal pain, or pelvic pain. She has insulin-dependent diabetes mellitus type 2, and underwent surgical treatment for symptomatic pelvic organ prolapse 3 years ago. Menopause was 6 years ago, and she is not on hormone replacement therapy. She works as an administrative manager, and drinks 3–4 cups of coffee daily at work. On physical examination, there is no suprapubic tenderness. Pelvic examination shows no abnormalities and Q-tip test was negative. Ultrasound of the bladder shows a normal post-void residual urine. Which of the following is the primary underlying etiology for this patient's urinary incontinence?
- A. Increased urine bladder volumes
- B. Increased detrusor muscle activity (Correct Answer)
- C. Recurrent pelvic organ prolapse
- D. Trauma to urinary tract
- E. Decreased pelvic floor muscle tone
Operative vaginal delivery Explanation: ***Increased detrusor muscle activity***
- The patient's symptoms of **sudden, painful sensation in the bladder**, involuntary urine loss, difficulty making it to the bathroom ("** बाथरूम-hopping**"), and **nocturia** are classic for **urge incontinence**.
- **Urge incontinence** is primarily caused by **uninhibited contractions of the detrusor muscle**, often due to **detrusor overactivity**. Her caffeine intake and history of diabetes can exacerbate this condition.
*Increased urine bladder volumes*
- While increased urine volume can exacerbate incontinence, it's typically associated with **overflow incontinence** (constant dribbling due to an overfilled bladder) or **polyuria** (excessive urine production), neither of which are suggested as the primary cause of her specific symptoms.
- The post-void residual urine is normal, ruling out significant retention that would lead to chronically increased bladder volumes from incomplete emptying.
*Recurrent pelvic organ prolapse*
- Pelvic organ prolapse can contribute to **stress incontinence** or **obstructive symptoms**, but her current pelvic exam shows no abnormalities, and she recently underwent surgery for this, making it less likely to be the primary cause of her current symptoms.
- Her symptoms of **urgency and nocturia** are not typical presentations of prolapse-related incontinence.
*Trauma to urinary tract*
- Trauma to the urinary tract would typically present with symptoms such as **hematuria**, **pain**, or difficulty voiding, none of which are reported in this case.
- There is no history of recent trauma or procedures that would directly lead to her current symptoms of urge incontinence.
*Decreased pelvic floor muscle tone*
- **Decreased pelvic floor muscle tone** is the primary cause of **stress incontinence**, characterized by urine leakage with increased intra-abdominal pressure (e.g., coughing, sneezing).
- Her symptoms are of **urgency and involuntary loss of urine** after a sudden sensation, which is distinct from stress incontinence, and her negative Q-tip test suggests good urethral support.
More Operative vaginal delivery US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.