Labor curve and Friedman curve US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Labor curve and Friedman curve. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Labor curve and Friedman curve US Medical PG Question 1: You have been entrusted with the task of finding the causes of low birth weight in infants born in the health jurisdiction for which you are responsible. In 2017, there were 1,500 live births and, upon further inspection of the birth certificates, 108 of these children had a low birth weight (i.e. lower than 2,500 g), while 237 had mothers who smoked continuously during pregnancy. Further calculations have shown that the risk of low birth weight in smokers was 14% and in non-smokers, it was 7%, while the relative risk of low birth weight linked to cigarette smoking during pregnancy was 2%. In other words, women who smoked during pregnancy were twice as likely as those who did not smoke to deliver a low-weight infant. Using this data, you are also asked to calculate how much of the excess risk for low birth weight, in percentage terms, can be attributed to smoking. What is the attributable risk percentage for smoking leading to low birth weight?
- A. 40%
- B. 30%
- C. 20%
- D. 10%
- E. 50% (Correct Answer)
Labor curve and Friedman curve Explanation: ***50%***
- This value is calculated using the formula for **attributable risk percent (ARP)** in the exposed group: ARP = ((Risk in exposed - Risk in unexposed) / Risk in exposed) × 100.
- Given that the risk of low birth weight in smokers (exposed) is 14% and in non-smokers (unexposed) is 7%, the calculation is ((0.14 - 0.07) / 0.14) × 100 = (0.07 / 0.14) × 100 = **0.50 × 100 = 50%**.
*40%*
- This percentage does not align with the provided risk values for low birth weight in smokers (14%) and non-smokers (7%).
- A calculation of ((0.14 - 0.07) / 0.14) * 100 does not yield 40%.
*30%*
- This value is incorrect, as it would suggest a smaller difference in risk between the exposed and unexposed groups relative to the risk in the exposed group than what is presented in the problem.
- The calculated attributable risk percent is higher than 30%.
*20%*
- This option is significantly lower than the true attributable risk percent derived from the given risk figures.
- It would imply a much weaker association between smoking and low birth weight in terms of excess risk than what is calculated.
*10%*
- This value is substantially different from the correct calculation and would suggest a very minor attributable risk.
- The attributable risk percent for smoking leading to low birth weight is much higher than 10% based on the provided data.
Labor curve and Friedman curve US Medical PG Question 2: A 39-year-old woman, gravida 5, para 4, at 41 weeks' gestation is brought to the hospital because of regular uterine contractions that started 2 hours ago. Pregnancy has been complicated by iron deficiency anemia treated with iron supplements. Pelvic examination shows the cervix is 90% effaced and 7-cm dilated; the vertex is at -1 station. Fetal heart tracing is shown. The patient is repositioned, O2 therapy is initiated, and amnioinfusion is done. A repeat assessment after 20 minutes shows a similar cervical status, and no changes in the fetal heart tracing, and less than 5 contractions in a period of 10 minutes.What is the most appropriate next step in management?
- A. Emergent cesarean delivery (Correct Answer)
- B. Monitor without intervention
- C. Begin active pushing
- D. Retry maternal repositioning
- E. Administer tocolytics
Labor curve and Friedman curve Explanation: ***Emergent cesarean delivery***
- The fetal heart tracing shows **recurrent late decelerations** unresponsive to **intrauterine resuscitation** (repositioning, O2, amnioinfusion), indicating fetal distress and uteroplacental insufficiency.
- Given the fetal distress and persistent late decelerations despite interventions, **expedited delivery** via cesarean section is indicated to prevent further fetal compromise.
*Monitor without intervention*
- This approach is inappropriate as the fetal heart tracing indicates **fetal distress** with recurrent **late decelerations** that have not resolved with initial interventions.
- Continued monitoring without action would place the fetus at risk for **hypoxia** and acidosis.
*Begin active pushing*
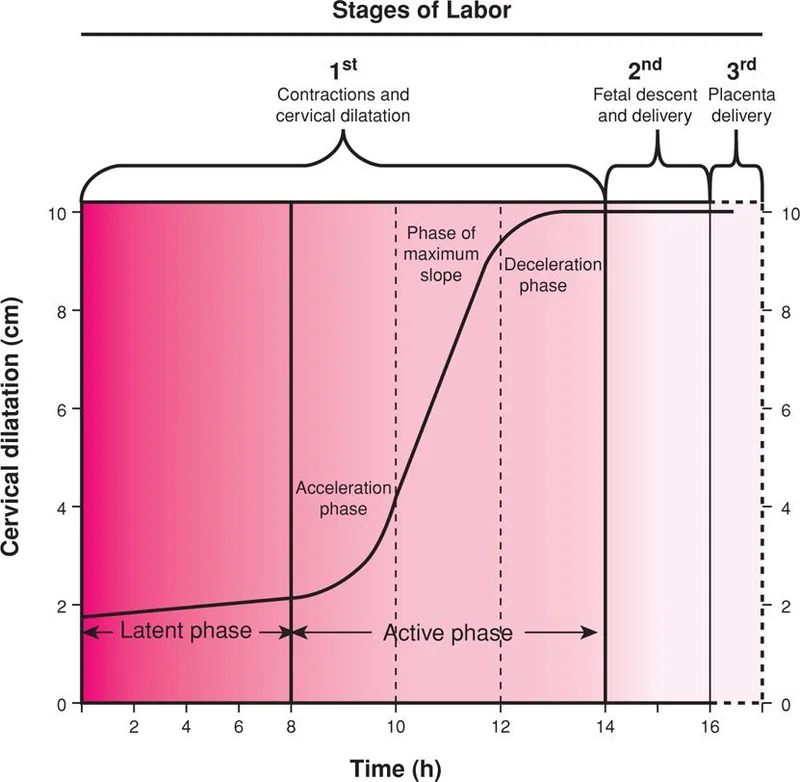
- The cervix is 7-cm dilated, meaning the patient is still in the **active phase of labor** and has not reached **complete cervical dilation** (10 cm) necessary for effective pushing.
- Pushing at this stage is unlikely to resolve the fetal distress and can potentially worsen **fetal acidosis** and maternal exhaustion.
*Retry maternal repositioning*
- The patient has already been repositioned and received other intrauterine resuscitation measures (O2 therapy, amnioinfusion) without improvement in the fetal heart tracing.
- Repeated repositioning alone is unlikely to resolve the underlying cause of the **late decelerations** in this context.
*Administer tocolytics*
- Tocolytics are used to **reduce uterine contractions** and manage conditions like **uterine tachysystole** or arrested labor, which are not explicitly present as the primary problem here (less than 5 contractions in 10 minutes).
- While they can temporarily improve uterine blood flow, they do not address the persistent **fetal distress** indicated by the recurrent late decelerations unresponsive to other interventions.
Labor curve and Friedman curve US Medical PG Question 3: A 30-year-old G3P0 woman who is 28 weeks pregnant presents for a prenatal care visit. She reports occasionally feeling her baby move but has not kept count over the past couple weeks. She denies any bleeding, loss of fluid, or contractions. Her previous pregnancies resulted in spontaneous abortions at 12 and 14 weeks. She works as a business executive, has been in excellent health, and has had no surgeries. She states that she hired a nutritionist and pregnancy coach to ensure good prospects for this pregnancy. On physical exam, fetal heart tones are not detected. Abdominal ultrasound shows a 24-week fetal demise. The patient requests an autopsy on the fetus and wishes for the fetus to pass "as naturally as possible." What is the best next step in management?
- A. Induction of labor now (Correct Answer)
- B. Dilation and evacuation
- C. Dilation and curettage
- D. Induction of labor at term
- E. Caesarean delivery
Labor curve and Friedman curve Explanation: ***Induction of labor now***
- With a confirmed **fetal demise at 28 weeks**, induction of labor is the most appropriate and respectful approach, allowing the patient's request to pass "as naturally as possible" to be honored and initiating the grieving process.
- Delaying labor induction can lead to increased risks of **coagulopathy** (disseminated intravascular coagulation) due to retained fetal tissue, and also prolonged emotional distress for the patient.
*Dilation and evacuation*
- While D&E is a common method for second-trimester termination or fetal demise, it is typically performed earlier in pregnancy (up to 24 weeks) and may not align with the patient's wish for the fetus to pass "as naturally as possible" for a 28-week demise.
- Given the patient's strong emotional investment in this pregnancy and desire for an autopsy, a D&E might be perceived as less respectful or less natural than labor induction.
*Dilation and curettage*
- **Dilation and curettage (D&C)** is primarily used for first-trimester miscarriages or early second-trimester procedures and is not suitable for a 28-week fetal demise due to the size of the fetus.
- Performing a D&C at this gestational age would be technically difficult and carry a higher risk of complications, including uterine perforation.
*Induction of labor at term*
- Waiting until term for a known fetal demise at 28 weeks is medically inappropriate and dangerous due to the significant risk of **disseminated intravascular coagulation (DIC)** developing from retained fetal tissue.
- Prolonged retention of a deceased fetus also significantly increases the emotional and psychological burden on the patient.
*Caesarean delivery*
- **Caesarean delivery** is generally reserved for live births where there is a medical indication for surgical delivery or in cases of an intact dilation and extraction procedure which is not typically first line for fetal demise at this gestation.
- Performing a C-section for a fetal demise offers no benefit to the fetus and carries unnecessary surgical risks for the mother, including infection, hemorrhage, and complications in future pregnancies.
Labor curve and Friedman curve US Medical PG Question 4: A 38-year-old woman, gravida 4, para 3, at 20 weeks' gestation comes to the physician for a prenatal care visit. She used fertility enhancing treatment for her current pregnancy. Her other children were born before 37 weeks' gestation. She is 170 cm (5 ft 7 in) tall and weighs 82 kg (180 lb); BMI is 28.4 kg/m2. Her vital signs are within normal limits. The abdomen is nontender, and no contractions are felt. Ultrasonography shows a cervical length of 22 mm and a fetal heart rate of 140/min. Which of the following is the most likely diagnosis?
- A. Placental insufficiency
- B. Bicornuate uterus
- C. Diethylstilbestrol exposure
- D. Cephalopelvic disproportion
- E. Cervical insufficiency (Correct Answer)
Labor curve and Friedman curve Explanation: ***Cervical insufficiency***
- A **short cervical length** (22 mm at 20 weeks) in a woman with a history of **multiple preterm births (G4P3 before 37 weeks)** is highly indicative of cervical insufficiency, where the cervix prematurely shortens and dilates.
- **Fertility-enhancing treatments** are an additional risk factor, as they often involve manipulations that can weaken the cervix or lead to multiple gestations, further stressing the cervix.
*Placental insufficiency*
- This condition is characterized by **fetal growth restriction** or **fetal distress** due to inadequate nutrient and oxygen supply from the placenta.
- The presented information primarily points to cervical changes, not direct evidence of placental dysfunction affecting fetal growth or well-being (e.g., normal fetal heart rate, no mention of FGR).
*Bicornuate uterus*
- A **bicornuate uterus** is a congenital uterine anomaly that can increase the risk of preterm birth due to a smaller uterine cavity or abnormal uterine contractions.
- However, while it can cause preterm labor, the primary finding here is a very short cervix, suggesting a cervical rather than uterine structural issue as the immediate diagnosis.
*Diethylstilbestrol exposure*
- **Diethylstilbestrol (DES) exposure** *in utero* can lead to reproductive tract abnormalities, including an increased risk of cervical incompetence and preterm birth.
- This diagnosis would require a history of maternal DES exposure during her own *in utero* development, which is not mentioned in the patient's history.
*Cephalopelvic disproportion*
- **Cephalopelvic disproportion (CPD)** is a mismatch between the size of the fetal head and the maternal pelvis, making vaginal delivery difficult or impossible.
- This condition is typically diagnosed later in pregnancy or during labor and is not related to cervical shortening at 20 weeks' gestation or a history of preterm births.
Labor curve and Friedman curve US Medical PG Question 5: A 30-year-old woman, gravida 2 para 1, at 39 weeks gestation presents to the hospital with painful contractions and a rupture of membranes. She reports that the contractions started a couple hours ago and are now occurring every 4 minutes. She is accompanied by her husband who states, “her water broke an hour ago before we left for the hospital." The patient denies vaginal bleeding, and fetal movements are normal. The patient has attended all her pre-natal visits without pregnancy complications. She has no chronic medical conditions and takes only pre-natal vitamins. Her blood pressure is 110/75 mm Hg and pulse is 82/min. A fetal heart rate tracing shows a pulse of 140/min with moderate variability and no decelerations. Cervical examination reveals a cervix that is 7 cm dilated and 100% effaced with the fetal head at -1 station. The patient forgoes epidural anesthesia. During which of the following scenarios should a cesarean delivery be considered for this patient?
- A. Cervix is 7 cm dilated and fetal head is at 0 station after 4 hours, with contractions every 2 minutes (Correct Answer)
- B. Cervix is 7 cm dilated and fetal head is at -1 station after 2 hours with contractions every 7 minutes
- C. Cervix is 9 cm dilated and fetal head is at -1 station after 3 hours, with contractions every 3 minutes
- D. Cervix is 10 cm dilated and fetal head is at +1 station after 2 hours, with contractions every 2 minutes
- E. Cervix is 7 cm dilated and fetal head is at 0 station after 1 hour, with contractions every 5 minutes
Labor curve and Friedman curve Explanation: ***Cervix is 7 cm dilated and fetal head is at 0 station after 4 hours, with contractions every 2 minutes***
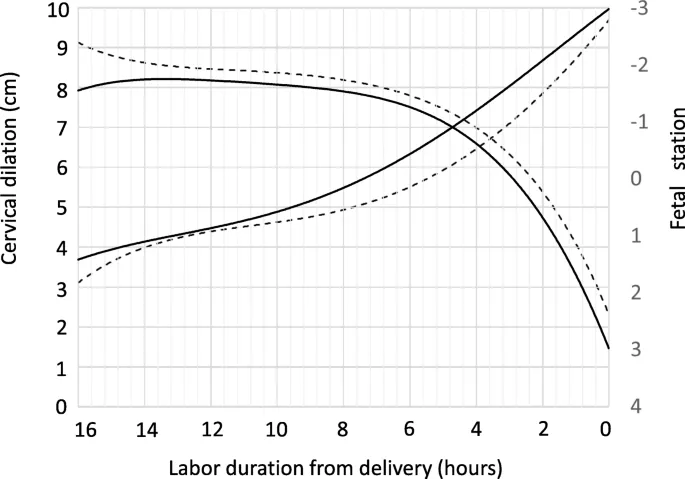
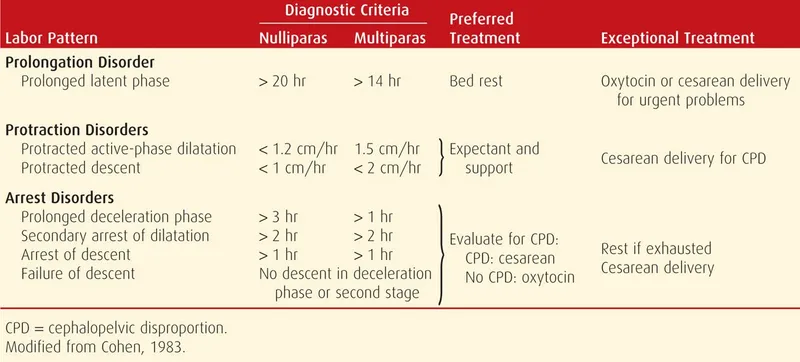
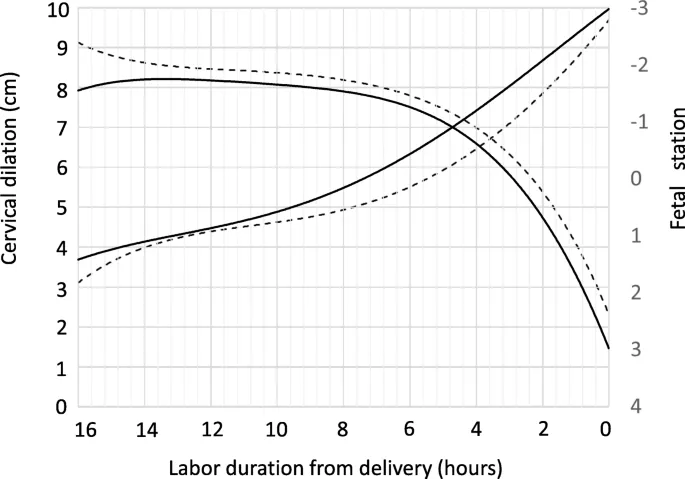
- This scenario describes **arrest of active phase of labor** in a **multiparous woman**, defined as no cervical change for at least 4 hours with adequate contractions (every 2-3 minutes) or at least 6 hours with inadequate contractions.
- The patient started at 7 cm dilation and, after 4 hours of strong contractions, has shown no further cervical change, indicating failed labor progression and warranting C-section.
*Cervix is 7 cm dilated and fetal head is at -1 station after 2 hours with contractions every 7 minutes*
- This still represents the **active phase of labor** (from 6 cm dilation onwards), but the contractions are **inadequate** (every 7 minutes) and the duration of observation is too short to diagnose an arrest (2 hours vs. 4 hours for multiparous).
- The appropriate step would be to **augment labor** (e.g., with oxytocin) rather than proceed directly to C-section.
*Cervix is 9 cm dilated and fetal head is at -1 station after 3 hours, with contractions every 3 minutes*
- The patient has progressed from 7 cm to 9 cm, indicating **cervical change**, and contractions are adequate.
- This is not an arrest of labor; she is nearing full dilation and likely progressing appropriately.
*Cervix is 10 cm dilated and fetal head is at +1 station after 2 hours, with contractions every 2 minutes*
- This scenario describes the **second stage of labor** (complete cervical dilation), where the focus shifts to fetal descent. The fetal head has already descended to +1 station and contractions are adequate.
- While prolonged second stage can lead to C-section, the general threshold for intervention in a multiparous woman with epidural is 3 hours, and without epidural, it's 2 hours. This patient is at 2 hours and progressing, so a C-section is not immediately indicated.
*Cervix is 7 cm dilated and fetal head is at 0 station after 1 hour, with contractions every 5 minutes*
- This is still the **active phase of labor**, but the observation period (1 hour) is too short to diagnose an arrest of labor, even with inadequate contractions (every 5 minutes).
- The first step would be to ensure **adequate uterine activity** and observe for a longer period before considering a C-section.
Labor curve and Friedman curve US Medical PG Question 6: A 28-year-old primigravid woman at 36 weeks' gestation comes to the emergency department for 2 hours of contractions. Her pregnancy has been uncomplicated. The contractions occur once every 20–30 minutes, last less than 30 seconds, and have been consistent in intensity and duration since onset. During that time there has been an increase in fetal movements. Her temperature is 37.1°C (98.8°F), pulse is 98/min, and blood pressure is 104/76 mm Hg. Pelvic examination shows clear cervical mucus and a firm uterus consistent in size with a 36-week gestation. The cervix is 0% effaced and undilated; the vertex is at -3 station. The fetal heart rate is reassuring. After an hour of monitoring in the emergency department, the character of the contractions and pelvic examination findings remain unchanged. Which of the following is the most appropriate next step?
- A. Admit for continuous monitoring
- B. Reassurance and discharge (Correct Answer)
- C. Administer tocolytics
- D. Perform cesarean delivery
- E. Offer local or regional anesthesia
Labor curve and Friedman curve Explanation: ***Reassurance and discharge***
- The patient's symptoms (contractions every 20-30 minutes, lasting less than 30 seconds, consistent in intensity and duration, **no cervical changes**) are consistent with **Braxton Hicks contractions** rather than true labor.
- Given the reassuring fetal movements, normal vital signs, and unchanged cervical examination after an hour of monitoring, **reassurance and discharge** with instructions to return for signs of true labor are appropriate.
*Admit for continuous monitoring*
- Admission for continuous monitoring is indicated for **true labor**, suspected fetal distress, or complications requiring close observation.
- This patient's findings, including lack of cervical change and stable contraction pattern, do not meet criteria for admission.
*Administer tocolytics*
- **Tocolytics** are used to stop or slow down premature labor.
- This patient is at **36 weeks' gestation** (near term) and is not in true labor, making tocolytic administration inappropriate and unnecessary.
*Perform cesarean delivery*
- **Cesarean delivery** is indicated for obstetric emergencies, fetal distress, or failed vaginal delivery.
- There are no indications for an operative delivery at this time; the patient is not in active labor and both mother and fetus are stable.
*Offer local or regional anesthesia*
- **Local or regional anesthesia** (e.g., epidural) is typically offered for pain management during active labor.
- Since the patient is not in active labor, pain management for labor is not necessary.
Labor curve and Friedman curve US Medical PG Question 7: A 22-year-old primigravid woman at 41 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been uncomplicated. She has asthma treated with theophylline and inhaled corticosteroids. She has had 2 surgeries in the past to repair multiple lower limb and pelvis fractures that were the result of a car accident. She is otherwise healthy. Her temperature is 37.2°C (99°F) and blood pressure is 108/70 mm Hg. Examination shows the cervix is 100% effaced and 10 cm dilated; the vertex is at -4 station, with the occiput in the anterior position. Uterine activity is measured at 275 MVUs. Maternal pushing occurs during the contractions. Fetal heart tracing is 166/min and reactive with no decelerations. Epidural anesthesia is initiated for pain relief. After 4 hours of pushing, the vertex is found to be at -4 station, with increasing strength and rate of uterine contractions; fetal heart tracing shows late decelerations. Which of the following is the most likely cause of this patient's prolonged labor?
- A. Deep transverse arrest
- B. Insufficient uterine contraction
- C. Epidural anesthesia
- D. Cephalopelvic disproportion (Correct Answer)
- E. Inefficient maternal pushing
Labor curve and Friedman curve Explanation: ***Cephalopelvic disproportion***
- The history of **multiple lower limb and pelvis fractures** from a car accident suggests a high likelihood of a **contracted or abnormally shaped pelvis**. This can lead to **cephalopelvic disproportion (CPD)**, where the fetal head cannot fit through the maternal pelvis despite adequate uterine contractions (275 MVUs).
- The combination of **prolonged labor** (4 hours of pushing with no descent), **vertex at -4 station** even after full dilation, increasing contraction strength, and new **late decelerations** (indicating fetal distress due to impaired oxygenation from prolonged compression) points towards an obstruction.
*Deep transverse arrest*
- This occurs when the fetal head rotates into the transverse diameter of the pelvis and fails to rotate anteriorly. While it causes **arrest of descent and dilation**, the primary issue is **malposition**, not a fundamental size mismatch.
- The occiput is described as in the **anterior position**, which does not immediately suggest deep transverse arrest.
*Insufficient uterine contraction*
- The uterine activity is measured at **275 MVUs**, which indicates **adequate contraction strength**. Insufficient contractions would typically be below 200 MVUs.
- While weak contractions can cause prolonged labor, the current uterine activity suggests this is not the primary problem.
*Epidural anesthesia*
- Epidural anesthesia can sometimes prolong the second stage of labor by reducing the urge to push or temporarily decreasing the effectiveness of pushing efforts. However, the patient's **strong uterine activity (275 MVUs)** and previous **pelvic fractures** make a mechanical obstruction (CPD) a more specific and likely cause of arrest in this scenario.
- Furthermore, the vertex remaining at -4 station for 4 hours despite strong contractions points to a physical barrier rather than just altered pushing dynamics.
*Inefficient maternal pushing*
- While inefficient maternal pushing can contribute to prolonged labor, the fetus remaining at -4 station for 4 hours with **strong uterine contractions (275 MVUs)** indicates that the issue is likely beyond just inadequate pushing efforts.
- The historical detail of **pelvic fractures** points more strongly to an anatomical obstruction rather than simply ineffective maternal exertion.
Labor curve and Friedman curve US Medical PG Question 8: A 62-year-old woman makes an appointment with her primary care physician because she recently started experiencing post-menopausal bleeding. She states that she suffered from anorexia as a young adult and has been thin throughout her life. She says that this nutritional deficit is likely what caused her to not experience menarche until age 15. She used oral contraceptive pills for many years, has never been pregnant, and experienced menopause at age 50. A biopsy of tissue inside the uterus reveals foci of both benign and malignant glandular cells. Which of the following was a risk factor for the development of the most likely cause of her symptoms?
- A. Menopause at age 50
- B. Never becoming pregnant (Correct Answer)
- C. Using oral contraceptive pills
- D. Menarche at age 15
- E. Being underweight
Labor curve and Friedman curve Explanation: ***Never becoming pregnant***
- **Nulliparity** is a significant risk factor for **endometrial cancer** as it implies longer exposure to unopposed estrogen, which stimulates endometrial proliferation.
- The diagnosis of malignant glandular cells in the context of post-menopausal bleeding strongly suggests **endometrial carcinoma**, where nulliparity contributes to increased estrogen exposure over time.
*Menopause at age 50*
- **Later age of menopause** (e.g., after 52) is a risk factor for endometrial cancer, as it prolongs the duration of estrogen exposure.
- Menopause at age 50 is considered within the **average range**, thus not typically an independent risk factor for endometrial cancer.
*Using oral contraceptive pills*
- **Combined oral contraceptive pills** (estrogen and progestin) actually **reduce the risk** of endometrial cancer.
- The progestin component in OCPs counteracts the proliferative effects of estrogen on the endometrium, offering protection.
*Menarche at age 15*
- **Early menarche** (before age 12) is a risk factor for endometrial cancer due to a longer lifetime exposure to estrogen.
- Menarche at age 15 is considered **later than average**, which would typically be a protective factor against endometrial cancer, as it shortens the duration of estrogen exposure.
*Being underweight*
- **Obesity** is a major risk factor for endometrial cancer because adipose tissue converts androgens to estrogens, leading to higher levels of circulating estrogen.
- Being underweight or having a history of anorexia does not increase the risk of endometrial cancer; in fact, it may be associated with **lower estrogen levels**, which could be protective.
Labor curve and Friedman curve US Medical PG Question 9: A 27-year old primigravid woman at 37 weeks' gestation comes to the emergency department because of frequent contractions for 4 hours. Her pregnancy has been complicated by hyperemesis gravidarum which subsided in the second trimester. The contractions occur every 10–15 minutes and have been increasing in intensity and duration since onset. Her temperature is 37.1°C (98.8°F), pulse is 110/min, and blood pressure is 140/85 mm Hg. Uterine contractions are felt on palpation. Pelvic examination shows clear fluid in the vagina. The cervix is 50% effaced and 3 cm dilated. After 4 hours the cervix is 80% effaced and 6 cm dilated. Pelvic examination is inconclusive for the position of the fetal head. The fetal heart rate is reassuring. Which of the following is the most appropriate next step?
- A. Administer oxytocin
- B. Perform external cephalic version
- C. Administer misoprostol
- D. Perform Mauriceau-Smellie-Veit maneuver
- E. Perform ultrasonography (Correct Answer)
Labor curve and Friedman curve Explanation: ***Perform ultrasonography***
- The examination notes that the **pelvic examination is inconclusive for the position of the fetal head**, which is a critical piece of information needed for safe delivery. **Ultrasonography** is the most appropriate next step to ascertain the fetal presentation and position, especially given the dilated cervix.
- Determining fetal position is essential to rule out **malpresentation**, such as **breech** or **transverse lie**, which would significantly impact the delivery plan and potentially necessitate a **cesarean section**.
*Administer oxytocin*
- **Oxytocin** is used to induce or augment labor when contractions are insufficient or labor is prolonged, but in this case, the cervix is progressing well (from 3 cm to 6 cm dilation in 4 hours), indicating **active labor**.
- Without knowing the fetal presentation, administering oxytocin could exacerbate issues if there's a **malpresentation**, potentially leading to **fetal distress** or **uterine rupture**.
*Perform external cephalic version*
- **External cephalic version (ECV)** is performed to change a **breech presentation** to a **cephalic presentation** by external manipulation, typically done before labor onset or early in labor at term.
- This patient is already in **active labor** with significant cervical dilation (6 cm), making ECV less likely to be successful and potentially increasing risks like **placental abruption** or **umbilical cord compression**.
*Administer misoprostol*
- **Misoprostol** is a prostaglandin analog used for **cervical ripening** and **labor induction** in cases where the cervix is unfavorable or labor needs to be initiated.
- This patient is already in **active labor** with progressive cervical dilation, making misoprostol unnecessary and potentially harmful due to the risk of **uterine hyperstimulation**.
*Perform Mauriceau-Smellie-Veit maneuver*
- The **Mauriceau-Smellie-Veit maneuver** is a technique used during a **vaginal breech delivery** to deliver the fetal head, specifically in cases of **frank or complete breech** that are being delivered vaginally.
- This maneuver is only performed *during* delivery of a breech baby, and the fetal position is currently unknown. It would be premature and inappropriate to consider this maneuver without first confirming a **breech presentation** and the decision for vaginal delivery.
Labor curve and Friedman curve US Medical PG Question 10: A 33-year-old woman, gravida 2, para 1, at 26 weeks' gestation comes to the emergency department because of frequent contractions. The contractions are 40 seconds each, occurring every 2 minutes, and increasing in intensity. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her current medications include folic acid and a multivitamin. Her temperature is 36.9°C (98.4°F), heart rate is 88/min, and blood pressure is 126/76 mm Hg. Contractions are felt on the abdomen. There is clear fluid in the vulva and the introitus. The cervix is dilated to 5 cm, 70% effaced, and station of the head is -2. A fetal ultrasound shows polyhydramnios, a median cleft lip, and fused thalami. The corpus callosum, 3rd ventricle, and lateral ventricles are absent. The spine shows no abnormalities and there is a four chamber heart. Which of the following is the most appropriate next step in management?
- A. Initiate misoprostol therapy
- B. Allow vaginal delivery (Correct Answer)
- C. Perform dilation and evacuation
- D. Initiate nifedipine therapy
- E. Perform cesarean delivery
Labor curve and Friedman curve Explanation: ***Allow vaginal delivery***
- The presence of severe fetal anomalies, including **holoprosencephaly** (median cleft lip, fused thalami, absent corpus callosum, 3rd and lateral ventricles), indicates that the fetus is **incompatible with life**.
- Given the prognosis, the most appropriate and safest approach for the mother is to **allow vaginal delivery**, as there is no benefit to delaying delivery or attempting a surgical intervention that might pose more risks to the mother.
*Initiate misoprostol therapy*
- **Misoprostol** is a prostaglandin analog used to induce labor or abortion, particularly in cases of uterine atony or to ripen the cervix.
- While it aids in cervical ripening and uterine contractions, the cervix is already 5 cm dilated and 70% effaced, indicating a **rapidly progressing labor** not requiring additional induction.
*Perform dilation and evacuation*
- **Dilation and evacuation (D&E)** is typically performed in the second trimester for fetal demise or termination of pregnancy, usually before 24 weeks' gestation.
- At 26 weeks' gestation with advanced labor and significant cervical dilation, D&E is a **high-risk procedure** for the mother and less appropriate than vaginal delivery.
*Initiate nifedipine therapy*
- **Nifedipine is a tocolytic** used to suppress preterm labor by relaxing the uterine muscles.
- Given the **lethal fetal anomalies** and the advanced stage of labor (5 cm dilated, 70% effaced, intense contractions), stopping labor would only prolong a non-viable pregnancy and increase maternal risk.
*Perform cesarean delivery*
- **Cesarean delivery** would expose the mother to surgical risks (e.g., infection, hemorrhage, future pregnancy complications) without any benefit to the fetus, who has anomalies **incompatible with survival**.
- A previous cesarean section does not preclude a vaginal delivery in this context, especially when **fetal viability is not a concern**.
More Labor curve and Friedman curve US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.