First stage of labor US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for First stage of labor. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
First stage of labor US Medical PG Question 1: A 36-year-old primigravid woman at 26 weeks' gestation comes to the physician complaining of absent fetal movements for the last 2 days. Pregnancy was confirmed by ultrasonography 14 weeks earlier. She has no vaginal bleeding or discharge. She has a history of type 1 diabetes mellitus controlled with insulin. Vital signs are all within the normal limits. Pelvic examination shows a soft, 2-cm long cervix in the midline with a cervical os measuring 3 cm and a uterus consistent in size with 24 weeks' gestation. Transvaginal ultrasonography shows a fetus with no cardiac activity. Which of the following is the most appropriate next step in management?
- A. Plan for oxytocin administration (Correct Answer)
- B. Perform weekly pelvic ultrasound
- C. Perform dilation and curettage
- D. Perform cesarean delivery
- E. Administer magnesium sulfate
First stage of labor Explanation: ***Plan for oxytocin administration***
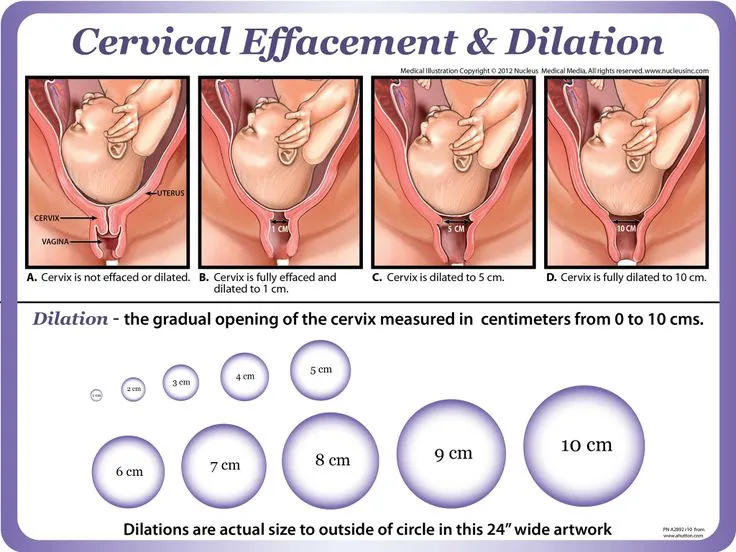
- The patient is at 26 weeks' gestation with confirmed fetal demise and an effaced, dilated cervix (2 cm long, 3 cm dilated). This indicates the cervix is already preparing for delivery.
- **Oxytocin** is the most appropriate next step to induce labor and facilitate vaginal delivery in cases of **intrauterine fetal demise** (IUFD) after the first trimester, especially when cervical changes have begun.
*Perform weekly pelvic ultrasound*
- The ultrasound has already confirmed **absent fetal cardiac activity**, making repeated ultrasounds unnecessary as the diagnosis of IUFD is already established.
- This option would delay necessary management and exposure to the deceased fetus in utero could increase risks such as **coagulopathy** if prolonged.
*Perform dilation and curettage*
- **Dilation and curettage (D&C)** is generally reserved for termination of pregnancy or management of miscarriage up to **16-18 weeks' gestation**.
- At **26 weeks' gestation**, the size of the fetus and uterus makes D&C a less safe and less effective procedure compared to labor induction.
*Perform cesarean delivery*
- **Cesarean delivery** for IUFD is typically reserved for cases with maternal indications (e.g., prior classical C-section scar, placenta previa obstructing the birth canal) or when labor induction fails.
- There are no maternal or fetal contraindications to vaginal delivery in this scenario, and a C-section would primarily increase maternal morbidity without fetal benefit.
*Administer magnesium sulfate*
- **Magnesium sulfate** is used for **neuroprotection** in preterm deliveries (usually before 32 weeks) and seizure prophylaxis in **preeclampsia/eclampsia**.
- As the fetus is deceased, neuroprotection is not applicable, and there are no signs of preeclampsia, making this intervention inappropriate.
First stage of labor US Medical PG Question 2: A 34-year-old pregnant woman with unknown medical history is admitted to the hospital at her 36th week of gestation with painful contractions. She received no proper prenatal care during the current pregnancy. On presentation, her vital signs are as follows: blood pressure is 110/60 mm Hg, heart rate is 102/min, respiratory rate is 23/min, and temperature is 37.0℃ (98.6℉). Fetal heart rate is 179/min. Pelvic examination shows a closed non-effaced cervix. During the examination, the patient experiences a strong contraction accompanied by a high-intensity pain after which contractions disappear. The fetal heart rate becomes 85/min and continues to decrease. The fetal head is now floating. Which of the following factors would most likely be present in the patient’s history?
- A. Fundal cesarean delivery (Correct Answer)
- B. Adenomyosis
- C. Intrauterine synechiae
- D. Multiple vaginal births
- E. Postabortion metroendometritis
First stage of labor Explanation: ***Fundal cesarean delivery***
- The sudden onset of intense pain followed by cessation of contractions, fetal bradycardia, and a floating fetal head in a woman with a prior Cesarean section scar is highly suggestive of **uterine rupture**.
- A previous **classical or fundal Cesarean section** scar carries the highest risk of rupture in subsequent pregnancies due to the incision extending into the contractile upper uterine segment.
*Adenomyosis*
- **Adenomyosis** involves the presence of endometrial tissue within the myometrium, which can cause heavy, painful periods and chronic pelvic pain, but it doesn't directly predispose to uterine rupture during labor.
- While it can complicate pregnancy with an increased risk of preterm birth or miscarriage, it is not associated with the acute presentation described.
*Intrauterine synechiae*
- **Intrauterine synechiae**, or Asherman's syndrome, are adhesions within the uterine cavity, often resulting from endometrial trauma.
- They primarily cause infertility, recurrent pregnancy loss, or abnormal placentation (like placenta accreta), but not uterine rupture.
*Multiple vaginal births*
- A history of **multiple vaginal births** generally *reduces* the risk of uterine rupture in subsequent pregnancies as the cervix and lower uterine segment are often more compliant.
- While prolonged labor or instrumental delivery can rarely increase rupture risk, it's not a primary risk factor like a prior classical Cesarean.
*Postabortion metroendometritis*
- **Postabortion metroendometritis** is an infection of the uterus after an abortion.
- While it can lead to complications such as Asherman's syndrome or infertility, it does not typically increase the risk of uterine rupture in a subsequent pregnancy in the manner described.
First stage of labor US Medical PG Question 3: A 39-year-old woman, gravida 5, para 4, at 41 weeks' gestation is brought to the hospital because of regular uterine contractions that started 2 hours ago. Pregnancy has been complicated by iron deficiency anemia treated with iron supplements. Pelvic examination shows the cervix is 90% effaced and 7-cm dilated; the vertex is at -1 station. Fetal heart tracing is shown. The patient is repositioned, O2 therapy is initiated, and amnioinfusion is done. A repeat assessment after 20 minutes shows a similar cervical status, and no changes in the fetal heart tracing, and less than 5 contractions in a period of 10 minutes.What is the most appropriate next step in management?
- A. Emergent cesarean delivery (Correct Answer)
- B. Monitor without intervention
- C. Begin active pushing
- D. Retry maternal repositioning
- E. Administer tocolytics
First stage of labor Explanation: ***Emergent cesarean delivery***
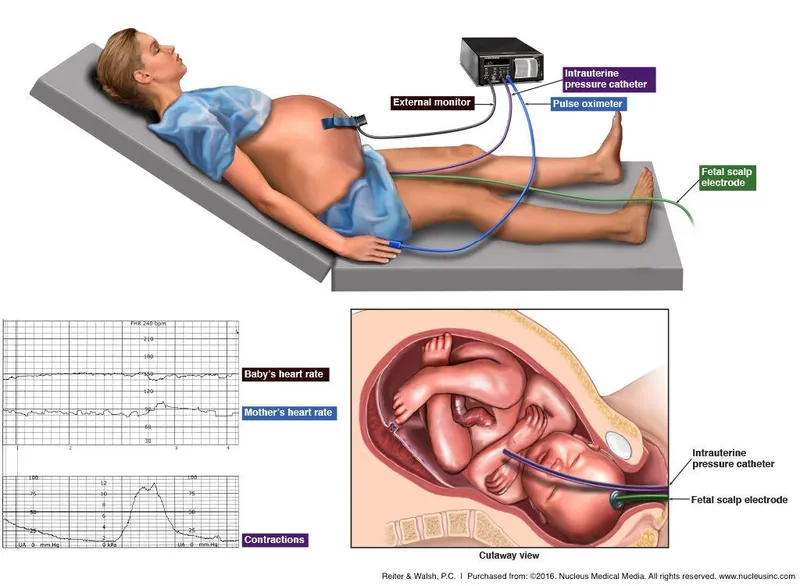
- The fetal heart tracing shows **recurrent late decelerations** unresponsive to **intrauterine resuscitation** (repositioning, O2, amnioinfusion), indicating fetal distress and uteroplacental insufficiency.
- Given the fetal distress and persistent late decelerations despite interventions, **expedited delivery** via cesarean section is indicated to prevent further fetal compromise.
*Monitor without intervention*
- This approach is inappropriate as the fetal heart tracing indicates **fetal distress** with recurrent **late decelerations** that have not resolved with initial interventions.
- Continued monitoring without action would place the fetus at risk for **hypoxia** and acidosis.
*Begin active pushing*
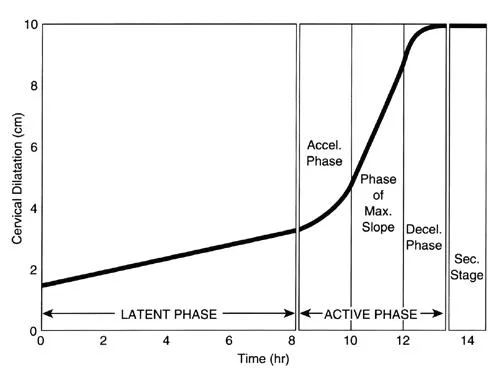
- The cervix is 7-cm dilated, meaning the patient is still in the **active phase of labor** and has not reached **complete cervical dilation** (10 cm) necessary for effective pushing.
- Pushing at this stage is unlikely to resolve the fetal distress and can potentially worsen **fetal acidosis** and maternal exhaustion.
*Retry maternal repositioning*
- The patient has already been repositioned and received other intrauterine resuscitation measures (O2 therapy, amnioinfusion) without improvement in the fetal heart tracing.
- Repeated repositioning alone is unlikely to resolve the underlying cause of the **late decelerations** in this context.
*Administer tocolytics*
- Tocolytics are used to **reduce uterine contractions** and manage conditions like **uterine tachysystole** or arrested labor, which are not explicitly present as the primary problem here (less than 5 contractions in 10 minutes).
- While they can temporarily improve uterine blood flow, they do not address the persistent **fetal distress** indicated by the recurrent late decelerations unresponsive to other interventions.
First stage of labor US Medical PG Question 4: A 24-year-old woman, gravida 1, at 35 weeks gestation is admitted to the hospital with regular contractions and pelvic pressure for the last 5 hours. Her pregnancy has been uncomplicated and she has attended many prenatal appointments and followed the physician's advice about screening for diseases, laboratory testing, diet, and exercise. She has had no history of fluid leakage or bleeding. At the hospital, her temperature is 37.2°C (99.0°F), blood pressure is 108/60 mm Hg, pulse is 88/min, and respirations are 16/min. Cervical examination shows 60% effacement and 5 cm dilation with intact membranes. Cardiotocography shows a contraction amplitude of 220 MVU in 10 minutes. Which of the following is the most appropriate pharmacotherapy at this time?
- A. Magnesium sulfate
- B. No pharmacotherapy at this time (Correct Answer)
- C. Dexamethasone
- D. Oxytocin
- E. Terbutaline
First stage of labor Explanation: ***No pharmacotherapy at this time***
- The patient is at **35 weeks gestation** and in **active labor** (5 cm dilated, 60% effacement, regular contractions with adequate Montevideo units). At this gestational age, labor is typically allowed to progress without intervention unless there are complications.
- Pharmacotherapy to stop labor (tocolysis) or induce fetal lung maturity (corticosteroids) is generally not indicated at or beyond 34 weeks gestation in uncomplicated cases.
*Magnesium sulfate*
- This is primarily used for **fetal neuroprotection** in anticipated preterm birth before 32 weeks gestation, or as a **tocolytic** to inhibit contractions, neither of which is indicated here.
- The patient is 35 weeks, beyond the typical window for neuroprotection, and stopping labor is not appropriate given her advanced dilation and gestational age.
*Dexamethasone*
- **Corticosteroids** like dexamethasone are administered to accelerate **fetal lung maturity** in cases of anticipated preterm birth, typically between 24 and 34 weeks gestation.
- At 35 weeks, the benefits of corticosteroids for lung maturity are minimal and generally not recommended.
*Oxytocin*
- **Oxytocin** is used to **induce or augment labor** if contractions are inadequate or to prevent **postpartum hemorrhage**.
- This patient is already in active, effective labor with adequate contractions (220 MVU in 10 minutes), so oxytocin for augmentation is not needed.
*Terbutaline*
- **Terbutaline** is a **beta-agonist tocolytic** used to relax the uterus and stop preterm labor.
- Given the patient's gestational age of 35 weeks and the progression of her labor (5 cm dilated), stopping contractions is not the appropriate management.
First stage of labor US Medical PG Question 5: A 30-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the hospital for regular, painful contractions that have been increasing in frequency. Her pregnancy has been complicated by gestational diabetes treated with insulin. Pelvic examination shows the cervix is 50% effaced and 4 cm dilated; the vertex is at -1 station. Ultrasonography shows no abnormalities. A tocometer and Doppler fetal heart monitor are placed on the patient's abdomen. The fetal heart rate monitoring strip shows a baseline heart rate of 145/min with a variability of ≥ 15/min. Within a 20-minute recording, there are 7 uterine contractions, 4 accelerations, and 3 decelerations that have a nadir occurring within half a minute. The decelerations occur at differing intervals relative to the contractions. Which of the following is the most appropriate next step in the management of this patient?
- A. Vibroacoustic stimulation
- B. Routine monitoring (Correct Answer)
- C. Administer tocolytics
- D. Emergent cesarean delivery
- E. Placement of fetal scalp electrode
First stage of labor Explanation: ***Routine monitoring***
- The presented FHR tracing exhibits a **normal baseline rate** (145/min), **moderate variability** (≥15/min), and the presence of **accelerations**, indicating a reassuring fetal status.
- The described decelerations are **variable decelerations** due to their sudden onset, nadir within 30 seconds, and variable relationship to contractions, which are generally benign unless prolonged, deep, or repetitive. Given the otherwise reassuring status, continued routine monitoring is appropriate.
*Vibroacoustic stimulation*
- This intervention is used to elicit **fetal accelerations** or movement during non-stress tests (NSTs) when the fetus is quiet or shows a non-reactive pattern.
- In this case, the fetus is already showing **accelerations** and moderate variability, so stimulation is not needed to assess fetal well-being.
*Administer tocolytics*
- **Tocolytics** are used to stop or slow down labor, typically in cases of preterm labor or uterine tachysystole causing fetal distress.
- This patient is at **38 weeks' gestation** and in active labor, and there are no signs of fetal distress warranting the cessation of contractions.
*Emergent cesarean delivery*
- **Emergent cesarean delivery** is indicated for acute fetal distress, such as prolonged decelerations, significant bradycardia, or absent variability in conjunction with other concerning FHR patterns.
- The FHR tracing described is largely reassuring with moderate variability and accelerations, and the variable decelerations are not indicative of immediate threat, making emergent delivery unnecessary.
*Placement of fetal scalp electrode*
- A **fetal scalp electrode** provides a more accurate and continuous measure of the FHR, often used when external monitoring is difficult or when there are concerns about the reliability of the tracing.
- While it can be useful in some situations, the current tracing is **interpretable as reassuring**, making invasive monitoring currently unnecessary.
First stage of labor US Medical PG Question 6: A 26-year-old gravida 1 at 36 weeks gestation is brought to the emergency department by her husband complaining of contractions lasting up to 2 minutes. The contractions are mostly in the front of her abdomen and do not radiate. The frequency and intensity of contractions have not changed since the onset. The patient worries that she is in labor. The blood pressure is 125/80 mm Hg, the heart rate is 96/min, the respiratory rate is 15/min, and the temperature 36.8°C (98.2℉). The physical examination is unremarkable. The estimated fetal weight is 3200 g (6.6 lb). The fetal heart rate is 146/min. The cervix is not dilated. The vertex is at the -4 station. Which of the following would be proper short-term management of this woman?
- A. Reassurance, hydration, and ambulation (Correct Answer)
- B. Admit to the Obstetrics Department for observation
- C. Manage with terbutaline
- D. Admit to the Obstetrics Department in preparation for labor induction
- E. Perform an ultrasound examination
First stage of labor Explanation: ***Reassurance, hydration, and ambulation***
- This patient is experiencing **Braxton-Hicks contractions**, which are irregular, do not cause cervical change, and often resolve with hydration and rest or light activity.
- Given her stable vital signs, normal fetal heart rate, and undilated cervix, these interventions are appropriate to differentiate from true labor and provide comfort.
*Admit to the Obstetrics Department for observation*
- Admission for observation is unnecessary as there are no signs of **true labor** (cervical dilation or effacement) or fetal distress.
- The contractions are described as not changing in frequency or intensity and are localized to the anterior abdomen, consistent with **false labor**.
*Manage with terbutaline*
- **Terbutaline** is a tocolytic used to stop or prevent premature labor, but this patient is at 36 weeks gestation, which is near term, and not in true labor.
- Using a tocolytic for **Braxton-Hicks contractions** is not indicated and can have adverse effects.
*Admit to the Obstetrics Department in preparation for labor induction*
- There is no indication for **labor induction** as the patient is not in active labor and has not reached her due date.
- Labor induction is reserved for medical or obstetric indications, which are not present here.
*Perform an ultrasound examination*
- An ultrasound has already provided an estimated fetal weight and the fetal heart rate is normal, suggesting no immediate need for further **ultrasound evaluation**.
- There are no clinical signs to suggest fetal distress or other complications that would warrant an **urgent ultrasound**.
First stage of labor US Medical PG Question 7: A 28-year-old woman, gravida 2, para 1, at 14 weeks' gestation, comes to the physician with a 3-day history of abnormal vaginal discharge. She has not had fever, chills, or abdominal pain. One week ago, her 2-year-old daughter had a urinary tract infection that quickly resolved after antibiotic therapy. The patient reports that she is sexually active with one male partner and they do not use condoms. Vital signs are within normal limits. Pelvic examination shows an inflamed and friable cervix. There is mucopurulent, foul-smelling discharge from the cervical os. There is no uterine or cervical motion tenderness. Vaginal pH measurement shows a pH of 3.5. Which of the following is the most appropriate initial step in management?
- A. Wet mount preparation
- B. Nucleic acid amplification test (Correct Answer)
- C. Amine test
- D. Urine analysis and culture
- E. Potassium hydroxide preparation
First stage of labor Explanation: ***Nucleic acid amplification test***
- The patient's symptoms of **inflamed, friable cervix** and **mucopurulent discharge**, along with a normal vaginal pH (3.5), are highly suggestive of **cervicitis**, commonly caused by *Chlamydia trachomatis* or *Neisseria gonorrhoeae*.
- **NAATs** are the most sensitive and specific tests for detecting these organisms, which is crucial for prompt diagnosis and treatment, especially in pregnancy, to prevent adverse outcomes.
*Wet mount preparation*
- A **wet mount** would be useful for identifying *Trichomonas vaginalis* or *Candida* species and diagnosing **bacterial vaginosis**, but the patient's normal vaginal pH makes these diagnoses less likely.
- While it can help rule out other common causes of vaginal discharge, it is **not sensitive enough** to reliably detect *Chlamydia* or *Gonorrhea*.
*Amine test*
- The **amine test** (or whiff test) is used to detect the release of amines in the presence of **bacterial vaginosis**, typically indicated by a **vaginal pH >4.5**.
- The patient's vaginal pH of 3.5 makes **bacterial vaginosis highly unlikely**, so an amine test would not be beneficial in this scenario.
*Urine analysis and culture*
- While the patient's daughter recently had a **urinary tract infection (UTI)**, the patient's symptoms are localized to the cervix (cervicitis) with **no fever, chills, or abdominal pain** indicative of a UTI.
- A urine analysis and culture would be appropriate if bladder symptoms were present, but it **will not diagnose cervicitis** or the specific sexually transmitted infections causing it.
*Potassium hydroxide preparation*
- A **KOH preparation** is primarily used to identify **fungal elements (hyphae and spores)**, indicating a *Candida* infection, which typically presents with thick, white, "cottage cheese" discharge and itching.
- This test is **not useful for diagnosing cervicitis** or bacterial causes of vaginal discharge, and the patient's symptoms are not consistent with candidiasis.
First stage of labor US Medical PG Question 8: A 54-year-old male comes to the clinic to initiate care with a new physician. He has no complaints at this time. When taking his history, the patient says his medical history is notable for diabetes and hypertension both of which are well managed on his medications. His medications are metformin and lisinopril. A review of systems is negative. While taking the social history, the patient hesitates when asked about alcohol consumption. Further gentle questioning by the physician leads the patient to admit that he drinks 5-6 beers per night and up to 10-12 drinks per day over the weekend. He says that he has been drinking like this for “years.” He becomes emotional and says that his alcohol is negatively affecting his relationship with his wife and children; however, when asked about efforts to decrease his consumption, the patient says he has not tried in the past and doesn’t think he has “the strength to stop”. Which of the following stages of change most accurately describes this patient’s behavior?
- A. Contemplation (Correct Answer)
- B. Maintenance
- C. Preparation
- D. Precontemplation
- E. Action
First stage of labor Explanation: ***Contemplation***
- The patient acknowledges his problem behavior (alcohol consumption) and its negative impact on his family, indicating an awareness of the issue.
- He expresses a desire for change ("strength to stop") but has not yet committed to taking action or made concrete plans, which is characteristic of the contemplation stage.
*Maintenance*
- This stage involves actively sustaining new behaviors and preventing relapse over a long period (typically 6 months or more).
- The patient admits he has not tried to decrease his consumption, ruling out any active behavior change or sustainability.
*Preparation*
- In this stage, individuals are ready to take action within the next month and have often developed a plan for change.
- The patient explicitly states he hasn't tried to reduce his alcohol intake and doesn't feel he has "the strength to stop," indicating a lack of readiness for immediate action or planning.
*Precontemplation*
- Individuals in this stage are unaware or unwilling to acknowledge that a problem exists and have no intention of changing their behavior in the foreseeable future.
- The patient clearly recognizes his drinking as a problem affecting his family, which distinguishes him from someone in precontemplation.
*Action*
- This stage involves actively modifying one's behavior, environment, or experiences to overcome problems.
- The patient has not made any efforts to decrease his alcohol consumption, meaning he has not yet entered the action phase.
First stage of labor US Medical PG Question 9: A 17-year-old teenager presents to the clinic with her parents complaining of headaches and loss of vision which began insidiously 3 months ago. She describes her headaches as throbbing, mostly on her forehead, and severe enough to affect her daily activities. She has not experienced menarche. Past medical history is noncontributory. She takes no medication. Both of her parents are alive and well. Today, her blood pressure is 110/70 mm Hg, the heart rate is 90/min, the respiratory rate is 17/min, and the temperature is 37.0°C (98.6°F). Breasts and pubic hair development are in Tanner stage I. Blood work is collected and an MRI is performed (the result is shown). Decreased production of which of the following hormones is the most likely explanation for the patient's signs and symptoms?
- A. Antidiuretic hormone
- B. Adrenocorticotropic hormone
- C. Prolactin
- D. Gonadotropins (Correct Answer)
- E. Thyroid-stimulating hormone
First stage of labor Explanation: **Gonadotropins**
- The MRI image shows a **pituitary mass** (indicated by the red arrow) in a 17-year-old girl with **amenorrhea** (has not experienced menarche) and **Tanner stage I breast and pubic hair development**.
- This clinical picture, coupled with the mass effect, suggests **hypogonadotropic hypogonadism** due to compression of the pituitary gland, leading to insufficient production of **gonadotropins** (LH and FSH), which are essential for pubertal development and menstrual cycles.
*Antidiuretic hormone*
- Deficiency of ADH primarily causes **diabetes insipidus**, characterized by **polyuria** and **polydipsia**, which are not mentioned in this patient's symptoms.
- While a pituitary mass can affect ADH production, the primary clinical presentation here is related to pubertal delay.
*Adrenocorticotropic hormone*
- ACTH deficiency would lead to **adrenal insufficiency**, presenting with symptoms such as **fatigue, weakness, weight loss, hypotension, and electrolyte disturbances**. These symptoms are not described in the patient.
- Her vital signs (e.g., blood pressure) are within normal limits.
*Prolactin*
- Elevated prolactin (hyperprolactinemia) can cause **amenorrhea** and **galactorrhea** (if the patient has reached puberty), but it is usually due to a **prolactinoma** or stalk compression.
- While a pituitary mass could potentially affect prolactin, the lack of pubertal development (Tanner stage I) points more directly to a general gonadotropin deficiency rather than isolated prolactinopathy.
*Thyroid-stimulating hormone*
- TSH deficiency would result in **hypothyroidism**, characterized by symptoms like **fatigue, weight gain, cold intolerance, and bradycardia**.
- The patient's vital signs are normal, and symptoms of hypothyroidism are not described.
First stage of labor US Medical PG Question 10: A 3-year-old girl is brought to the physician by her mother two days after the sudden onset of a rash. The mother says that the rash developed an hour after she bathed the child in hot water. Two weeks ago, the patient was diagnosed with a skin infection and was treated with penicillin V. She has been otherwise healthy but has missed several well-child examinations. She lives with her single mother, who recently lost her job and is now dependent on social assistance. The patient's mother has major depressive disorder and her maternal aunt has systemic lupus erythematosus. The girl's temperature is 36.8°C (98.2°F), pulse is 112/min, and blood pressure is 108/62 mm Hg. She has poor eye contact. Physical examination shows sharply delineated erythema on the lower extremities up to the umbilicus with sparing of the knees and flexor surfaces. Further evaluation is most likely to reveal which of the following?
- A. Dermatographism
- B. Multiple injuries in different stages of healing (Correct Answer)
- C. Ulcers of the oral mucosa
- D. Malar rash with sparing of the nasolabial folds
- E. Positive Nikolsky's sign
First stage of labor Explanation: ***Multiple injuries in different stages of healing***
- This scenario strongly suggests **child abuse**. The "rash" described is suspicious; it is a **sharply delineated erythema** on the lower extremities up to the umbilicus with sparing of the knees and flexor surfaces, appearing after a hot bath. This pattern is classic for a **scald injury**, which would be considered abuse if inflicted by hot water.
- The mother's claim of a sudden rash occurring an hour after a hot bath makes a thermal injury more likely, especially given her recent job loss, dependence on social assistance, and major depressive disorder, all of which are **risk factors for child abuse**. The child's poor eye contact also raises concerns.
*Dermatographism*
- **Dermatographism** is a form of urticaria where strokes or pressure on the skin cause raised, red lines.
- This condition presents as transient wheals and would not align with the described **sharply delineated erythema** in a specific distribution, nor would it be triggered only by a hot bath in this manner.
*Ulcers of the oral mucosa*
- **Oral ulcers** are common in various systemic conditions (e.g., aphthous stomatitis, viral infections, lupus) but are not directly suggested by a sudden onset of skin erythema after a hot bath.
- While some forms of abuse might involve oral injury, the described skin rash is not a typical presentation or associated finding that would lead one to specifically look for oral ulcers.
*Malar rash with sparing of the nasolabial folds*
- A **malar rash** (butterfly rash) is characteristic of **systemic lupus erythematosus (SLE)**, which the patient's maternal aunt has. However, this rash typically affects the cheeks and bridge of the nose.
- The patient's rash is described as **sharply delineated erythema** on the lower extremities up to the umbilicus, with sparing of specific areas, which is inconsistent with the distribution and appearance of a malar rash.
*Positive Nikolsky's sign*
- **Nikolsky's sign** involves the epidermal detachment upon light friction, indicative of blistering disorders like **pemphigus vulgaris** or **staphylococcal scalded skin syndrome (SSSS)**.
- While SSSS can cause widespread erythema and skin peeling, the description of **sharply delineated erythema** on specific body parts after a hot bath is more consistent with a thermal injury than the diffuse blistering and epidermal sloughing seen in SSSS.
More First stage of labor US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.