Ultrasound markers and anomaly screening US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ultrasound markers and anomaly screening. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ultrasound markers and anomaly screening US Medical PG Question 1: A 39-year-old pregnant woman at 16 weeks gestation recently underwent a quad-screen which revealed elevated beta-hCG, elevated inhibin A, decreased alpha-fetoprotein, and decreased estradiol. An ultrasound was performed which found increased nuchal translucency. Which of the following is recommended for diagnosis?
- A. Biopsy and pathologic examination of fetus
- B. Confirmatory amniocentesis and chromosomal analysis of the fetal cells (Correct Answer)
- C. Fetus is normal, continue with pregnancy as expected
- D. Maternal karyotype
- E. Cell-free fetal DNA analysis
Ultrasound markers and anomaly screening Explanation: ***Confirmatory amniocentesis and chromosomal analysis of the fetal cells***
- The combination of **quad-screen results** (elevated 𝛽-hCG, elevated inhibin A, decreased AFP, decreased estradiol) and **increased nuchal translucency** strongly suggests an aneuploidy, particularly **Down Syndrome (Trisomy 21)**.
- **Amniocentesis** is a **diagnostic procedure** that provides fetal cells for definitive chromosomal analysis (karyotyping), confirming or ruling out aneuploidy with high accuracy.
*Biopsy and pathologic examination of fetus*
- A **fetal biopsy** is generally not a standard diagnostic test for aneuploidy and carries higher risks than amniocentesis or chorionic villus sampling (CVS).
- This procedure would typically be considered for specific fetal anomalies requiring tissue diagnosis, not for confirming chromosomal disorders.
*Fetus is normal, continue with pregnancy as expected*
- The abnormal **quad-screen results** and **increased nuchal translucency** are significant indicators of potential chromosomal abnormalities, making it unlikely that the fetus is normal.
- Ignoring these findings could lead to the birth of a child with an undiagnosed genetic condition.
*Maternal karyotype*
- A **maternal karyotype** evaluates the mother's chromosomes to identify balanced translocations or other inherited chromosomal abnormalities that could increase the risk in offspring.
- While helpful for identifying a parental genetic cause, it does not directly diagnose the fetal condition; a fetal sample is still needed for that.
*Cell-free fetal DNA analysis*
- **Cell-free fetal DNA (cfDNA) analysis** is a **screening test** with high sensitivity and specificity for common aneuploidies, but it is not a diagnostic test.
- While it can guide further investigation, a positive cfDNA result still requires a **confirmatory diagnostic procedure** like amniocentesis or CVS before making definitive clinical decisions.
Ultrasound markers and anomaly screening US Medical PG Question 2: A 27-year-old female in her 20th week of pregnancy presents for a routine fetal ultrasound screening. An abnormality of the right fetal kidney is detected. It is determined that the right ureteropelvic junction has failed to recanalize. Which of the following findings is most likely to be seen on fetal ultrasound:
- A. Renal cysts
- B. Duplicated ureter
- C. Bilateral renal agenesis
- D. Pelvic kidney
- E. Unilateral hydronephrosis (Correct Answer)
Ultrasound markers and anomaly screening Explanation: ***Unilateral hydronephrosis***
- Failure of the **ureteropelvic junction (UPJ)** to recanalize leads to an obstruction of urine flow from the **renal pelvis** into the ureter.
- This obstruction causes a buildup of urine in the renal pelvis and calyces, a condition known as **hydronephrosis**, which will be unilateral as only the right kidney is affected.
*Renal cysts*
- **Renal cysts** are typically associated with conditions like polycystic kidney disease or multicystic dysplastic kidney, which involve abnormal development of renal parenchyma, not specifically a UPJ obstruction.
- While hydronephrosis can sometimes lead to cystic changes if severe and prolonged, in the initial stages of a UPJ obstruction detected on fetal ultrasound, **hydronephrosis** itself is the primary and most likely finding.
*Duplicated ureter*
- A **duplicated ureter** is a distinct congenital anomaly involving the formation of two ureters draining a single kidney or separate renal moieties.
- It does not directly result from the failure of **ureteropelvic junction recanalization**.
*Bilateral renal agenesis*
- **Bilateral renal agenesis** means both kidneys failed to develop, which would lead to severe oligohydramnios and is incompatible with sustained fetal life.
- The question describes an abnormality only in the **right kidney**, making bilateral agenesis incorrect.
*Pelvic kidney*
- A **pelvic kidney** (renal ectopia) occurs when the kidney fails to ascend from the pelvis to its normal lumbar position.
- This is a positional anomaly and is not directly caused by a failure of **ureteropelvic junction recanalization**.
Ultrasound markers and anomaly screening US Medical PG Question 3: A 37-year-old woman comes for a follow-up prenatal visit at 18 weeks' gestation. At 12 weeks' gestation, ultrasonography showed increased nuchal translucency and pregnancy-associated plasma protein A (PAPP-A) was decreased by 2 standard deviations. Chorionic villus sampling showed a 47, XX, +21 karyotype. During this visit, ultrasonography shows a hypoplastic nasal bone, shortened femur length, shortened middle phalanges of the fifth digits with clinodactyly. A quadruple marker test would most likely show which of the following sets of findings?
$$$ α-Fetoprotein (AFP) %%% Estriol %%% β-Human chorionic gonadotropin (HCG) %%% Inhibin A $$$
- A. ↓ ↓ ↓ ↓
- B. ↑ normal normal normal
- C. ↓ ↓ ↑ ↑ (Correct Answer)
- D. Normal normal normal normal
- E. ↓ ↓ ↓ normal
Ultrasound markers and anomaly screening Explanation: ***↓ ↓ ↑ ↑***
- This pattern (low **AFP**, low **estriol**, high **hCG**, high **inhibin A**) is characteristic of **Down syndrome (Trisomy 21)** in a quadruple marker screen.
- The patient's history, including **increased nuchal translucency**, low **PAPP-A**, and a **47, XX, +21 karyotype**, strongly confirms the diagnosis of Down syndrome, making this a consistent finding.
*↓ ↓ ↓ ↓*
- This pattern of uniformly low markers is not typical for **Down syndrome** and would more commonly suggest other chromosomal abnormalities or a different fetal condition altogether.
- While some markers are low in Down syndrome, the elevation of **hCG** and **inhibin A** is a key differentiator.
*↑ normal normal normal*
- An isolated elevated **AFP** is commonly associated with neural tube defects or ventral wall defects, which are not suggested by the patient's presentation.
- Down syndrome invariably affects multiple markers in a specific pattern, not just one.
*Normal normal normal normal*
- Normal quadruple markers would indicate a low risk for **chromosomal aneuploidies**, which contradicts the patient's confirmed diagnosis of **Down syndrome (47, XX, +21)**.
- This option is inconsistent with the presented clinical and previous genetic findings.
*↓ ↓ ↓ normal*
- This pattern does not align with the typical profile for **Down syndrome**, which characteristically shows elevated **hCG** and **inhibin A**.
- While **AFP** and **estriol** are decreased in Down syndrome, the normal inhibin A makes this option incorrect.
Ultrasound markers and anomaly screening US Medical PG Question 4: A 34-year-old gravida 2 para 1 woman at 16 weeks gestation presents for prenatal care. Her prenatal course has been uncomplicated. She takes no medications besides her prenatal vitamin which she takes every day, and she has been compliant with routine prenatal care. She has a 7-year-old daughter who is healthy. The results of her recent quadruple screen are listed below:
AFP: Low
hCG: Low
Estriol: Low
Inhibin-A: Normal
Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Chorionic villus sampling
- B. Amniocentesis (Correct Answer)
- C. Ultrasound for nuchal translucency
- D. Folic acid supplementation
- E. Return to clinic in 4 weeks
Ultrasound markers and anomaly screening Explanation: ***Amniocentesis***
- The presented quad screen results (low AFP, low hCG, low estriol, normal Inhibin-A) are highly suggestive of **trisomy 18 (Edwards syndrome)**. Amniocentesis is a **definitive diagnostic test** that can confirm aneuploidy by providing a fetal karyotype.
- While typically performed between **15 and 20 weeks gestation**, it can differentiate between trisomy 18 and trisomy 21 (Down syndrome), which usually presents with high hCG and high Inhibin-A.
*Chorionic villus sampling (CVS)*
- **CVS** is typically performed earlier in pregnancy, between **10 and 13 weeks gestation**, meaning it is too late to perform at 16 weeks gestation.
- While it can provide a fetal karyotype for genetic diagnosis, the gestational age presented in the vignette makes this option currently inappropriate.
*Ultrasound for nuchal translucency*
- **Nuchal translucency (NT)** is part of the first-trimester screening, usually measured between **11 and 14 weeks gestation**.
- At 16 weeks gestation, measuring NT would be **outside the appropriate timeframe**, and the second-trimester quad screen has already been completed, making further screening rather than diagnosis less useful.
*Folic acid supplementation*
- **Folic acid supplementation** is crucial before and during early pregnancy to prevent neural tube defects, which would be associated with high AFP.
- The patient is already taking prenatal vitamins (which contain folic acid), and her quad screen results are not indicative of a neural tube defect but rather a chromosomal abnormality.
*Return to clinic in 4 weeks*
- The abnormal quad screen results indicate a **high risk for aneuploidy**, specifically trisomy 18, which requires immediate follow-up and definitive diagnosis.
- Delaying further assessment for 4 weeks would be clinically inappropriate and could increase patient anxiety and potentially reduce options for further management.
Ultrasound markers and anomaly screening US Medical PG Question 5: A 28-year-old G2P1 female is concerned that she may give birth to another child with Down syndrome. She states that she may not be able to take care of another child with this disorder. Which of the following tests can confirm the diagnosis of Down syndrome in utero?
- A. Ultrasound
- B. Triple marker test
- C. Integrated test
- D. Quadruple marker test
- E. Amniocentesis (Correct Answer)
Ultrasound markers and anomaly screening Explanation: ***Amniocentesis***
- **Amniocentesis** is a **diagnostic procedure** that involves collecting amniotic fluid to obtain fetal cells for **karyotyping**, which can definitively confirm the presence of an extra chromosome 21, the cause of Down syndrome.
- This test is typically performed between **15 and 20 weeks of gestation** and carries a small risk of complication but offers conclusive results.
*Ultrasound*
- **Ultrasound** is a **screening tool** that can detect anatomical features suggestive of Down syndrome, such as **nuchal translucency** or heart defects, but it cannot definitively diagnose the condition.
- It identifies **markers** that increase the suspicion of Down syndrome, prompting further diagnostic testing, but does not provide genetic confirmation.
*Triple marker test*
- The **triple marker test** is a **screening test** that measures levels of **alpha-fetoprotein (AFP)**, **unconjugated estriol (uE3)**, and **human chorionic gonadotropin (hCG)** in maternal blood.
- While it can estimate the risk of Down syndrome, it is not a diagnostic test and only provides a **risk assessment**, not a definitive diagnosis.
*Integrated test*
- The **integrated test** combines results from first-trimester screening (nuchal translucency and PAPP-A) and second-trimester screening (quadruple marker test) to provide a **single risk assessment**.
- Like other screening tests, it calculates a **risk probability** for Down syndrome but does not offer a definitive diagnosis.
*Quadruple marker test*
- The **quadruple marker test** measures AFP, uE3, hCG, and **inhibin A** in maternal blood during the second trimester.
- It is a **screening test** used to assess the risk of Down syndrome and open neural tube defects, but it is not a diagnostic tool.
Ultrasound markers and anomaly screening US Medical PG Question 6: A 19-year-old woman presents for a sports physical. She says she feels healthy and has no concerns. Past medical history is significant for depression and seasonal allergies. Current medications are fluoxetine and oral estrogen/progesterone contraceptive pills. Family history is significant for a sister with polycystic ovarian syndrome (PCOS). The patient denies current or past use of alcohol, recreational drugs, or smoking. She reports that she has been on oral birth control pills since age 14 and uses condoms inconsistently. No history of STDs. She is sexually active with her current boyfriend, who was treated for chlamydia 2 years ago. She received and completed the HPV vaccination series starting at age 11. Her vital signs include: temperature 36.8°C (98.2°F), pulse 97/min, respiratory rate 16/min, blood pressure 120/75 mm Hg. Physical examination is unremarkable. Which of the following are the recommended guidelines for cervical cancer screening for this patient at this time?
- A. Cytology (pap smear) and HPV DNA co-testing every 3 years
- B. Cytology (pap smear) every 3 years
- C. Cytology (pap smear) annually
- D. Cytology (pap smear) and HPV DNA co-testing every 5 years
- E. No cervical cancer screening is indicated at this time (Correct Answer)
Ultrasound markers and anomaly screening Explanation: ***No cervical cancer screening is indicated at this time***
- Current guidelines recommend initiating **cervical cancer screening** at age 21, regardless of sexual activity initiation.
- The patient is 19 years old, therefore, screening is not yet indicated per standard recommendations.
*Cytology (pap smear) and HPV DNA co-testing every 3 years*
- This option is incorrect because **co-testing** with cytology and HPV DNA is generally recommended for women aged 30-65 years, not for women under 21.
- While cytology every 3 years is a recommendation for women 21-29, co-testing is not the primary recommendation in this age group, and the patient is below the screening age.
*Cytology (pap smear) every 3 years*
- This screening interval is recommended for women aged 21-29 years, but the patient is currently 19 years old.
- Initiating screening earlier than 21 years is not recommended due to the high incidence of **transient HPV infections** and low risk of cervical cancer in younger individuals.
*Cytology (pap smear) annually*
- **Annual Pap smears** are no longer recommended for routine screening; guidelines have shifted to longer intervals due to the slow progression of cervical cancer and high rates of HPV clearance.
- Even if screening were indicated, annual cytology is not the current recommendation for any age group, especially not for a 19-year-old.
*Cytology (pap smear) and HPV DNA co-testing every 5 years*
- This screening strategy (**co-testing every 5 years**) is recommended for women aged 30-65 years.
- This patient is only 19 years old, making this recommendation inappropriate for her age.
Ultrasound markers and anomaly screening US Medical PG Question 7: A 45-year-old woman presents with a history of cervical erosion and spotting for the past 2 months. What is the next best step?
- A. LBC + HPV (Correct Answer)
- B. Pap smear + HSV
- C. Pap smear + HBV
- D. LBC + HSV
Ultrasound markers and anomaly screening Explanation: ***LBC + HPV***
- Cervical erosion and spotting are concerning for **cervical intraepithelial neoplasia (CIN)** or **cervical cancer**, making **Liquid-Based Cytology (LBC)** the appropriate screening method.
- **Human Papillomavirus (HPV) testing** is crucial as persistent high-risk HPV infection is the primary cause of cervical cancer and helps in risk stratification and management.
*Pap smear + HSV*
- A **routine Pap smear** (conventional cytology) is less sensitive than LBC for detecting abnormal cervical cells and is generally being phased out by LBC.
- **Herpes Simplex Virus (HSV)** causes genital herpes and is not directly associated with cervical cancer, thus testing for it in this context is not the most appropriate immediate next step.
*Pap smear + HBV*
- As mentioned, a **routine Pap smear** is not the preferred method for cervical cancer screening compared to LBC.
- **Hepatitis B Virus (HBV)** causes liver disease and is entirely unrelated to cervical pathology; therefore, testing for it would be irrelevant to the patient's symptoms.
*LBC + HSV*
- While **LBC** is the correct advanced cytology method, adding **HSV testing** is not indicated as HSV does not cause cervical cancer or intraepithelial lesions that present with cervical erosion and spotting.
- Focus should be on identifying potential malignancy or pre-malignant changes with HPV co-testing, not sexually transmitted infections unrelated to cancer risk.
Ultrasound markers and anomaly screening US Medical PG Question 8: The following set of instruments are used for which procedure?
- A. Biopsy
- B. Dilatation and curettage
- C. Pap smear (Correct Answer)
- D. Hysteroscopy
Ultrasound markers and anomaly screening Explanation: ***Pap smear***
- The image displays a complete set of instruments used for a **Pap smear**, including **glass slides** for sample collection, a **cervical brush**, a **spatula** (cytobrush and Ayre spatula), and a **speculum** to visualize the cervix.
- These tools are specifically designed for collecting cervical cells to screen for **cervical cancer** and **precancerous changes**.
*Biopsy*
- A biopsy typically involves specialized instruments like **punch biopsy tools**, **forceps**, or needles to extract tissue samples, which are not depicted here.
- While glass slides might be used for processing biopsy samples, the primary collection tools are absent.
*Dilatation and curettage*
- This procedure requires instruments such as **dilators** to open the cervix and **curetters** to scrape the uterine lining, which are not shown in the image.
- The instruments shown are for surface cell collection, not for uterine cavity procedures.
*Hysteroscopy*
- Hysteroscopy uses a **hysteroscope**—a thin, lighted tube with a camera—to visualize the inside of the uterus.
- The instruments in the image are for external examination and cervical cell collection, not for direct visualization of the uterine cavity.
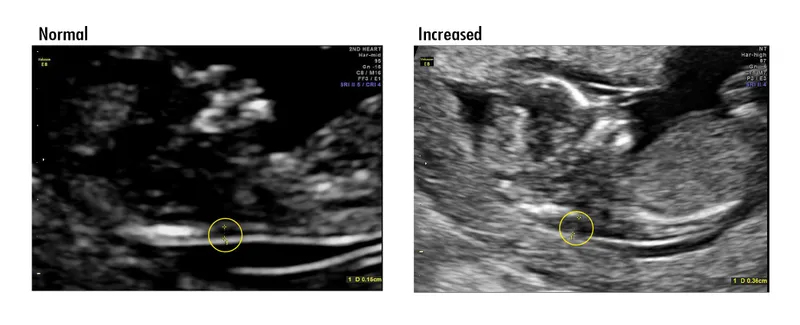
Ultrasound markers and anomaly screening US Medical PG Question 9: A 25-year-old pregnant woman, at 18 weeks of gestation, undergoes a routine ultrasound scan. The ultrasound images provided show below. Based on the imaging findings, what is the most likely diagnosis?
- A. Spina bifida (Correct Answer)
- B. Anencephaly
- C. Encephalocele
- D. Holoprosencephaly
- E. Iniencephaly
Ultrasound markers and anomaly screening Explanation: ***Spina bifida***
- The ultrasound image shows a **defect in the posterior elements of the fetal spine**, with characteristic splaying or widening of the vertebral arches.
- This is a **neural tube defect** resulting from incomplete closure of the spinal column during embryonic development.
- Associated findings on prenatal ultrasound may include the **"lemon sign"** (scalloping of frontal bones) and **"banana sign"** (abnormal cerebellar shape).
- Spina bifida is typically detected on **second-trimester anatomy scan** (18-20 weeks).
*Anencephaly*
- This condition involves the **absence of a major portion of the brain, skull, and scalp** due to failure of anterior neural tube closure.
- On ultrasound, anencephaly presents with **absent calvarium above the orbits** and absent cerebral hemispheres, which is distinctly different from a spinal defect.
- This would be a **cranial abnormality**, not a spinal column defect.
*Encephalocele*
- An **encephalocele** is a protrusion of brain tissue and meninges through a defect in the skull, most commonly at the **occipital region**.
- On ultrasound, this appears as a **cranial mass** extending beyond the skull contour, not a spinal defect.
*Holoprosencephaly*
- This condition results from **failure of forebrain (prosencephalon) to divide properly** into two hemispheres.
- Ultrasound findings include **single ventricle**, fused thalami, and absent midline structures, often with associated **facial anomalies**.
- The imaging would show **brain abnormalities**, not spinal column defects.
*Iniencephaly*
- This is a rare **neural tube defect** characterized by extreme retroflexion of the head with severe spinal defects in the cervical and thoracic regions.
- On ultrasound, iniencephaly shows the fetal head in extreme **hyperextension** with the face looking upward, creating a characteristic "stargazing" appearance.
- This differs from the typical spinal defect pattern seen in spina bifida.
Ultrasound markers and anomaly screening US Medical PG Question 10: A home drug screening test kit is currently being developed. The cut-off level is initially set at 4 mg/uL, which is associated with a sensitivity of 92% and a specificity of 97%. How might the sensitivity and specificity of the test change if the cut-off level is changed to 2 mg/uL?
- A. Sensitivity = 92%, specificity = 97%
- B. Sensitivity = 95%, specificity = 98%
- C. Sensitivity = 100%, specificity = 97%
- D. Sensitivity = 90%, specificity = 99%
- E. Sensitivity = 97%, specificity = 96% (Correct Answer)
Ultrasound markers and anomaly screening Explanation: ***Sensitivity = 97%, specificity = 96%***
- Lowering the cut-off from 4 mg/uL to 2 mg/uL means that more individuals will be classified as **positive** (anyone with drug levels ≥2 mg/uL instead of ≥4 mg/uL). This change will **increase the sensitivity** (capturing more true positives, fewer false negatives) but **decrease the specificity** (more false positives among those without the condition).
- Therefore, sensitivity will increase (e.g., to 97%), and specificity will decrease (e.g., to 96%), reflecting the fundamental trade-off between these metrics.
*Sensitivity = 92%, specificity = 97%*
- This option reflects the **original values** at the 4 mg/uL cut-off and does not account for the change in the threshold.
- A change in the cut-off level will inherently alter the test's performance characteristics.
*Sensitivity = 95%, specificity = 98%*
- This option suggests an increase in **both sensitivity and specificity**, which is generally not possible by simply changing the cut-off level in the same direction.
- There is typically an **inverse relationship** between sensitivity and specificity when adjusting the cut-off threshold.
*Sensitivity = 100%, specificity = 97%*
- Reaching **100% sensitivity** while maintaining a high specificity is highly unlikely with a simple cut-off adjustment.
- While sensitivity would increase with a lower cut-off, achieving perfect sensitivity is unrealistic in clinical practice.
*Sensitivity = 90%, specificity = 99%*
- This option suggests a **decrease in sensitivity** and an **increase in specificity**.
- A lower cut-off would lead to more positive results, thus increasing sensitivity and reducing specificity, which contradicts the proposed values.
More Ultrasound markers and anomaly screening US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.