Screening for preeclampsia risk factors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Screening for preeclampsia risk factors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Screening for preeclampsia risk factors US Medical PG Question 1: A 29-year-old G2P1 in her 22nd week of pregnancy presents with a primary complaint of peripheral edema. Her first pregnancy was without any major complications. Evaluation reveals a blood pressure of 160/90 and urinalysis demonstrates elevated levels of protein; both of these values were within normal limits at the patient's last well check-up 1 year ago. Further progression of this patient’s condition would immediately place her at greatest risk for developing which of the following?
- A. Myocardial infarction
- B. Crohn's Disease
- C. Diabetes mellitus
- D. Tubulointerstitial nephritis
- E. Seizures (Correct Answer)
Screening for preeclampsia risk factors Explanation: ***Seizures***
- The patient presents with **new-onset hypertension** (160/90 mmHg) and **proteinuria** after 20 weeks of gestation, along with peripheral edema, which is diagnostic of **preeclampsia**.
- Progression of preeclampsia to include generalized tonic-clonic seizures is known as **eclampsia**, which is an immediate and severe risk.
*Myocardial infarction*
- While preeclampsia increases the long-term risk of cardiovascular disease, **acute myocardial infarction** is not typically the immediate complication of worsening preeclampsia in a 29-year-old.
- Myocardial infarction in this context would be rare, usually associated with pre-existing cardiac conditions or more severe manifestations of disease.
*Crohn's Disease*
- **Crohn's disease** is an inflammatory bowel disease and has no direct causative or immediate progressive link to preeclampsia.
- The symptoms described (hypertension, proteinuria, edema) are not indicative of an inflammatory bowel process.
*Diabetes mellitus*
- **Gestational diabetes** is a common pregnancy complication but is characterized by hyperglycemia, not hypertension and proteinuria.
- While some cases of preeclampsia can complicate diabetic pregnancies, the immediate progression of preeclampsia itself is not to new-onset diabetes.
*Tubulointerstitial nephritis*
- **Tubulointerstitial nephritis** is an inflammatory kidney condition, but it is not typically an immediate complication directly resulting from the progression of preeclampsia.
- Preeclampsia primarily causes glomerular and endothelial dysfunction, not directly tubulointerstitial inflammation as the next immediate severe step.
Screening for preeclampsia risk factors US Medical PG Question 2: A 26-year-old woman, gravida 2, para 1, at 28 weeks' gestation comes to the physician for a prenatal visit. She feels well. Pregnancy and delivery of her first child were uncomplicated. Her temperature is 37.2°C (99°F) and blood pressure is 163/105 mm Hg. Her blood pressure 10 weeks ago was 128/84 mm Hg. At her last visit two weeks ago, her blood pressure was 142/92 mm Hg. Pelvic examination shows a uterus consistent in size with a 28-week gestation. A complete blood count and serum concentrations of electrolytes, creatinine, and hepatic transaminases are within the reference range. A urinalysis is within normal limits. Which of the following is the most appropriate next step in management?
- A. Oral labetalol therapy (Correct Answer)
- B. Lisinopril therapy
- C. Magnesium sulfate therapy
- D. Complete bed rest
- E. Dietary salt restriction
Screening for preeclampsia risk factors Explanation: **Oral labetalol therapy**
- The patient has developed **gestational hypertension** (blood pressure ≥140/90 mmHg on two occasions at least 4 hours apart after 20 weeks gestation, without proteinuria or other signs of preeclampsia), with her current BP of 163/105 mmHg confirming **severe range hypertension** (systolic ≥160 mmHg or diastolic ≥110 mmHg).
- **Labetalol** is a first-line agent for managing hypertension in pregnancy due to its established safety profile and efficacy in lowering blood pressure.
*Lisinopril therapy*
- **Angiotensin-converting enzyme (ACE) inhibitors** like lisinopril are **contraindicated in pregnancy** as they can cause fetal renal dysfunction, oligohydramnios, and neonatal hypotension.
- This medication choice would be harmful to the fetus.
*Magnesium sulfate therapy*
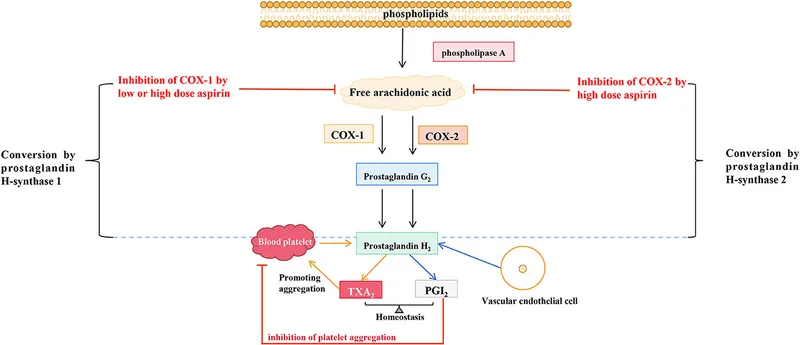
- **Magnesium sulfate** is indicated for the **prevention and treatment of seizures in preeclampsia/eclampsia**, not for blood pressure control itself.
- While the patient has hypertension, there are no signs of preeclampsia (e.g., proteinuria, signs of end-organ damage), making magnesium sulfate inappropriate at this stage.
*Complete bed rest*
- **Complete bed rest** is no longer recommended for the management of gestational hypertension or preeclampsia, as studies have shown it does not improve maternal or fetal outcomes and can increase the risk of **thromboembolism**.
- It can also negatively impact a patient's quality of life without providing therapeutic benefit.
*Dietary salt restriction*
- While generally recommended for hypertension outside of pregnancy, **severe salt restriction** in pregnancy is **not typically recommended** for gestational hypertension or preeclampsia, as it has not been shown to improve outcomes and could potentially worsen maternal fluid balance.
- The primary management for severe range gestational hypertension involves antihypertensive medications.
Screening for preeclampsia risk factors US Medical PG Question 3: A 25-year-old G1P0 woman at an estimated gestational age of 9 weeks presents for her first prenatal visit following a positive home pregnancy test. She says she missed 2 periods but assumed it was due to stress at work. She has decided to continue with the pregnancy. Her past medical history is significant for migraine headaches, seizures, and asthma. She takes multiple medications for her condition. Physical examination is unremarkable. An ultrasound confirms a 9-week-old intrauterine pregnancy. Which of the following medications poses the greatest risk to the fetus?
- A. Valproic acid (Correct Answer)
- B. Budesonide
- C. Acetaminophen
- D. Sumatriptan
- E. Albuterol
Screening for preeclampsia risk factors Explanation: ***Valproic acid***
- **Valproic acid** is a known **teratogen** strongly associated with a high incidence of **neural tube defects** (e.g., spina bifida, anencephaly) when used during the first trimester of pregnancy.
- It can also lead to other malformations, including cardiac defects and facial dysmorphism, as part of **fetal valproate syndrome**.
*Budesonide*
- **Budesonide** is an inhaled corticosteroid commonly used for asthma, considered a relatively **safe medication** during pregnancy (FDA pregnancy category B).
- Studies have shown no increased risk of major congenital malformations with its use.
*Acetaminophen*
- **Acetaminophen** is a widely used analgesic and antipyretic considered **safe** for use throughout pregnancy at recommended doses.
- There is no strong evidence linking acetaminophen to an increased risk of birth defects.
*Sumatriptan*
- **Sumatriptan** is a serotonin receptor agonist used for migraine headaches. It is generally considered to be of **low risk** during pregnancy (FDA pregnancy category C).
- While some studies have suggested a minimal risk of certain birth defects, overall data supports its use when necessary.
*Albuterol*
- **Albuterol** is a short-acting beta-agonist used to treat asthma symptoms and is considered **safe** for use during pregnancy (FDA pregnancy category C).
- There is no evidence of teratogenicity, and the benefits of controlling asthma outweigh the potential risks.
Screening for preeclampsia risk factors US Medical PG Question 4: A 36-year-old primigravid woman comes to the physician for a prenatal visit at 14 weeks' gestation. She has had episodic headaches over the past month. At home, blood pressure measurements have ranged from 134/82 mm Hg to 148/94 mm Hg. Today, her blood pressure is 146/91 mm Hg. Pelvic examination shows a uterus consistent in size with a 13-week gestation. Serum creatinine is 0.8 mg/dL, serum ALT is 17 U/L, and platelet count is 320,000/mm3. Urinalysis shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Eclampsia
- B. Preeclampsia
- C. Gestational hypertension
- D. Isolated systolic hypertension
- E. Chronic hypertension (Correct Answer)
Screening for preeclampsia risk factors Explanation: ***Chronic hypertension***
- The patient's elevated blood pressure (146/91 mm Hg) is present **before 20 weeks' gestation**, which is the defining characteristic of chronic hypertension in pregnancy.
- Her home blood pressure readings ranging from 134/82 mm Hg to 148/94 mm Hg over the past month further support a pre-existing hypertensive state.
*Eclampsia*
- Eclampsia is characterized by **new-onset grand mal seizures** in a woman with preeclampsia, which is not present in this case.
- It typically occurs **after 20 weeks' gestation** and also involves specific lab abnormalities, which are absent here.
*Preeclampsia*
- Preeclampsia involves **new-onset hypertension** (systolic ≥140 or diastolic ≥90) occurring **after 20 weeks' gestation**, often accompanied by proteinuria or other signs of end-organ damage.
- The patient's elevated blood pressure at **14 weeks' gestation** rules out preeclampsia as the initial diagnosis.
*Gestational hypertension*
- Gestational hypertension is characterized by **new-onset hypertension** (systolic ≥140 or diastolic ≥90) occurring for the **first time after 20 weeks' gestation** without proteinuria or features of preeclampsia.
- The patient's 14-week gestation and episodic headaches prior to this visit indicate that the hypertension likely predates the 20-week mark.
*Isolated systolic hypertension*
- Isolated systolic hypertension is defined as a **systolic blood pressure of 140 mm Hg or higher** and a **diastolic blood pressure less than 90 mm Hg**.
- The patient's diastolic blood pressure of 91 mm Hg (and 94 mm Hg at home) falls within the hypertensive range, ruling out isolated systolic hypertension.
Screening for preeclampsia risk factors US Medical PG Question 5: A 39-year-old G3P0 woman presents for preconception counseling and evaluation. The patient’s past medical history reveals hypertension and type 1 diabetes. She is currently on an insulin pump and medications for hypertension including labetalol. Her blood pressure is 130/85 mm Hg; pulse, 76/min; and BMI, 26 kg/m2. Her most recent HbA1c is 6.5%. Her previous pregnancies ended in spontaneous abortion during the 1st trimester despite adequate prenatal care. The patient intends to have a healthy pregnancy and desires to learn more about the risk factors that potentially trigger miscarriage. Which of the following maternal risk factors is most likely associated with early pregnancy loss?
- A. Infection
- B. Hypercoagulable state
- C. Diabetes
- D. Chronic hypertension
- E. Age (Correct Answer)
Screening for preeclampsia risk factors Explanation: ***Age***
- **Maternal age** is a significant risk factor for aneuploidy, which is the leading cause of early pregnancy loss.
- As women age, the quality of their oocytes declines, increasing the risk of chromosomal abnormalities.
*Infection*
- While certain **infections** (e.g., toxoplasmosis, rubella, cytomegalovirus, herpes simplex) can cause miscarriage, they are less common causes of recurrent early pregnancy loss than chromosomal abnormalities.
- Infections would typically present with other systemic symptoms or specific laboratory findings, which are not mentioned here.
*Hypercoagulable state*
- **Hypercoagulable states** (e.g., antiphospholipid syndrome) are known causes of recurrent pregnancy loss, particularly in the second and third trimesters, but also in early pregnancy.
- However, for general early pregnancy loss, advanced maternal age leading to aneuploidy is a more common and direct risk factor.
*Diabetes*
- Poorly controlled **diabetes** (especially with HbA1c >8%) is a significant risk factor for miscarriage and congenital anomalies.
- This patient's HbA1c of 6.5% indicates reasonably good control, reducing the likelihood of diabetes being the primary sole cause for her recurrent losses.
*Chronic hypertension*
- **Chronic hypertension** is associated with an increased risk of preeclampsia, fetal growth restriction, and stillbirth, especially in later trimesters.
- While it can contribute to adverse pregnancy outcomes, it is not the most common direct cause of **early pregnancy loss,** particularly in the first trimester.
Screening for preeclampsia risk factors US Medical PG Question 6: A 36-year-old primigravida woman visits her gynecologist during the 28th week of her pregnancy. Physical examination reveals pitting edema around her ankles and elevated systolic blood pressure. 24-hour urine collection yields 4 grams of protein. If left untreated, the patient is most at increased risk for which of the following:
- A. Thrombocytosis
- B. Gestational diabetes
- C. Hemolysis (Correct Answer)
- D. Placenta accreta
- E. Eclampsia
Screening for preeclampsia risk factors Explanation: **Hemolysis**
- The patient's presentation with **new-onset hypertension** (elevated systolic blood pressure), **proteinuria** (>300 mg/24 hours or 4 grams in this case), and **edema** strongly suggests **preeclampsia**.
- If left untreated, preeclampsia can progress to **HELLP syndrome** (**H**emolysis, **E**levated **L**iver enzymes, **L**ow **P**latelets), where **hemolysis** is a primary component.
*Thrombocytosis*
- **Preeclampsia** and its severe forms, like HELLP syndrome, are associated with **thrombocytopenia** (low platelets), not thrombocytosis (elevated platelets).
- **Thrombocytosis** is generally not a complication of severe preeclampsia or eclampsia.
*Gestational diabetes*
- While **gestational diabetes** is a common pregnancy complication, it is characterized by **glucose intolerance** and is not directly linked to the patient's symptoms of hypertension and proteinuria.
- The primary risk from gestational diabetes is for macrosomia, neonatal hypoglycemia, and increased future risk of type 2 diabetes, not the direct complications of severe preeclampsia.
*Placenta accreta*
- **Placenta accreta** is a condition where the placenta abnormally adheres to the uterine wall, typically presenting with **heavy bleeding during delivery**.
- It is not a direct complication of untreated preeclampsia, although both can increase maternal morbidity.
*Eclampsia*
- **Eclampsia** is defined by the occurrence of **new-onset grand mal seizures** in a woman with preeclampsia, without a history of epilepsy.
- While eclampsia is a severe complication of untreated preeclampsia, **hemolysis** (as part of HELLP syndrome) is also a critical and direct potential consequence that can occur with severe preeclampsia, even before seizures manifest.
Screening for preeclampsia risk factors US Medical PG Question 7: A 62-year-old woman makes an appointment with her primary care physician because she recently started experiencing post-menopausal bleeding. She states that she suffered from anorexia as a young adult and has been thin throughout her life. She says that this nutritional deficit is likely what caused her to not experience menarche until age 15. She used oral contraceptive pills for many years, has never been pregnant, and experienced menopause at age 50. A biopsy of tissue inside the uterus reveals foci of both benign and malignant glandular cells. Which of the following was a risk factor for the development of the most likely cause of her symptoms?
- A. Menopause at age 50
- B. Never becoming pregnant (Correct Answer)
- C. Using oral contraceptive pills
- D. Menarche at age 15
- E. Being underweight
Screening for preeclampsia risk factors Explanation: ***Never becoming pregnant***
- **Nulliparity** is a significant risk factor for **endometrial cancer** as it implies longer exposure to unopposed estrogen, which stimulates endometrial proliferation.
- The diagnosis of malignant glandular cells in the context of post-menopausal bleeding strongly suggests **endometrial carcinoma**, where nulliparity contributes to increased estrogen exposure over time.
*Menopause at age 50*
- **Later age of menopause** (e.g., after 52) is a risk factor for endometrial cancer, as it prolongs the duration of estrogen exposure.
- Menopause at age 50 is considered within the **average range**, thus not typically an independent risk factor for endometrial cancer.
*Using oral contraceptive pills*
- **Combined oral contraceptive pills** (estrogen and progestin) actually **reduce the risk** of endometrial cancer.
- The progestin component in OCPs counteracts the proliferative effects of estrogen on the endometrium, offering protection.
*Menarche at age 15*
- **Early menarche** (before age 12) is a risk factor for endometrial cancer due to a longer lifetime exposure to estrogen.
- Menarche at age 15 is considered **later than average**, which would typically be a protective factor against endometrial cancer, as it shortens the duration of estrogen exposure.
*Being underweight*
- **Obesity** is a major risk factor for endometrial cancer because adipose tissue converts androgens to estrogens, leading to higher levels of circulating estrogen.
- Being underweight or having a history of anorexia does not increase the risk of endometrial cancer; in fact, it may be associated with **lower estrogen levels**, which could be protective.
Screening for preeclampsia risk factors US Medical PG Question 8: A 36-year-old primigravid woman at 34 weeks' gestation comes to the physician because of a 1-week history of upper abdominal discomfort, nausea, and malaise. She had a mild upper respiratory tract infection a week ago. She has a 10-year history of polycystic ovarian syndrome and a 3-year history of hypertension. Her medications include metformin, labetalol, folic acid, and a multivitamin. Her pulse is 92/min, respirations are 18/min, and blood pressure is 147/84 mm Hg. Examination shows a nontender uterus consistent in size with a 34-week gestation. There is mild tenderness of the right upper quadrant of the abdomen. The fetal heart rate is reactive with no decelerations. Which of the following is the most appropriate next step in management?
- A. Reassurance and follow-up
- B. Serum transaminase levels and platelet count (Correct Answer)
- C. Serum bile acid levels
- D. HBsAg and IgM anti-HBc serology
- E. Stool antigen assay for H. pylori
Screening for preeclampsia risk factors Explanation: ***Serum transaminase levels and platelet count***
- The patient presents with symptoms such as **upper abdominal discomfort**, nausea, malaise, and **mild right upper quadrant tenderness**, along with a history of **hypertension** in pregnancy, raising concern for **preeclampsia with severe features** or **HELLP syndrome**.
- **Elevated liver transaminases** and **thrombocytopenia (low platelet count)** are hallmarks of HELLP syndrome, which requires urgent evaluation and management.
*Reassurance and follow-up*
- Given the concerning symptoms and risk factors, simply reassuring the patient without further investigation would be **inappropriate** and could lead to delayed diagnosis and potential harm.
- The symptoms described are not typical minor complaints of pregnancy and warrant a prompt workup.
*Serum bile acid levels*
- Elevated serum bile acid levels are primarily indicative of **intrahepatic cholestasis of pregnancy (ICP)**, which typically presents with **pruritus** (itching), especially on the palms and soles, without significant right upper quadrant pain or other systemic symptoms seen here.
- While ICP can cause some abdominal discomfort, the constellation of symptoms in this patient points more strongly towards preeclampsia/HELLP.
*HBsAg and IgM anti-HBc serology*
- These tests are used to diagnose **Hepatitis B infection**. While hepatitis could cause similar symptoms like nausea and abdominal discomfort, there is no specific risk factor or clinical sign (e.g., jaundice, dark urine) in this patient to prioritize hepatitis screening as the immediate next step over evaluating for preeclampsia/HELLP.
- The symptoms are more consistent with pregnancy-related hypertensive disorders.
*Stool antigen assay for H. pylori*
- This assay is used to diagnose **Helicobacter pylori infection**, which can cause gastritis or peptic ulcer disease.
- While H. pylori can cause upper abdominal discomfort and nausea, the patient's existing hypertension, late-stage pregnancy, and lack of symptoms specific to gastritis (e.g., burning pain, response to antacids) make preeclampsia/HELLP a more pressing concern.
Screening for preeclampsia risk factors US Medical PG Question 9: Six hours after giving birth to a healthy 3100 g (6 lb 13oz) girl, a 40-year-old woman, gravida 1, para 1 suddenly has a tonic-clonic seizure for 2-minutes while on the ward. She had been complaining of headache, blurry vision, and abdominal pain for an hour before the incident. Her pregnancy was complicated by gestational hypertension and iron deficiency anemia. Her medications until birth included labetalol, iron supplements, and a multivitamin. Her temperature is 37°C (98.7°F), pulse is 95/min, respirations are 18/min, and blood pressure is 152/100 mm Hg. The cranial nerves are intact. Muscle strength is normal. Deep tendon reflexes are 3+ with a shortened relaxation phase. Which of the following is the most appropriate next step in management?
- A. Calcium gluconate
- B. Phenytoin
- C. Magnesium sulfate (Correct Answer)
- D. Hydralazine
- E. Valproic acid
Screening for preeclampsia risk factors Explanation: ***Magnesium sulfate***
- The patient's presentation with a **tonic-clonic seizure**, headache, blurry vision, abdominal pain, hypertension, and hyperreflexia in the postpartum period is highly suggestive of **eclampsia**.
- **Magnesium sulfate** is the first-line and most appropriate agent for both the prevention and treatment of seizures in patients with eclampsia due to its neuroprotective and anticonvulsant effects.
*Calcium gluconate*
- **Calcium gluconate** is the antidote for **magnesium sulfate toxicity**, not a primary treatment for eclamptic seizures.
- Administering calcium gluconate before magnesium sulfate would be incorrect as it would counteract a beneficial medication that isn't yet administered.
*Phenytoin*
- **Phenytoin** is an **antiepileptic drug** that can be used for seizure control, but it is considered a second-line agent for eclampsia, after magnesium sulfate has been tried or is contraindicated.
- Magnesium sulfate has superior efficacy and a better side-effect profile for eclamptic seizures compared to phenytoin.
*Hydralazine*
- **Hydralazine** is an **antihypertensive medication** used to manage severe hypertension, particularly in pregnancy.
- While the patient's blood pressure is elevated, the priority in eclampsia is seizure control, which is not directly addressed by hydralazine.
*Valproic acid*
- **Valproic acid** is a broad-spectrum **antiepileptic drug** used for various seizure types.
- It is not the first-line agent for eclamptic seizures and its use in this context is less established and less effective than magnesium sulfate.
Screening for preeclampsia risk factors US Medical PG Question 10: A 26-year-old primigravida presents to her physician’s office at 35 weeks gestation with new onset lower leg edema. The course of her pregnancy was uneventful up to the time of presentation and she has been compliant with the recommended prenatal care. She reports a 4 pack-year history of smoking prior to her pregnancy. She also used oral contraceptives for birth control before considering the pregnancy. Prior to pregnancy, she weighed 52 kg (114.6 lb). She gained 11 kg (24.3 lb) during the pregnancy thus far, and 2 kg (4.4 lb) during the last 2 weeks. Her height is 169 cm (5 ft 7 in). She has a family history of hypertension in her mother (diagnosed at 46 years of age) and aunt (diagnosed at 51 years of age). The blood pressure is 145/90 mm Hg, the heart rate is 91/min, the respiratory rate is 15/min, and the temperature is 36.6℃ (97.9℉). The blood pressure is unchanged 15 minutes and 4 hours after the initial measurement. The fetal heart rate is 144/min. The examination is remarkable for 2+ pitting lower leg edema. The neurologic examination shows no focality. A urine dipstick test shows 2+ proteinuria. Which of the following factors is a risk factor for her condition?
- A. Primigravida (Correct Answer)
- B. Oral contraceptives intake
- C. BMI < 18.5 kg/m2 prior to pregnancy
- D. Smoking prior to pregnancy
- E. Family history of hypertension
Screening for preeclampsia risk factors Explanation: *Primigravida*
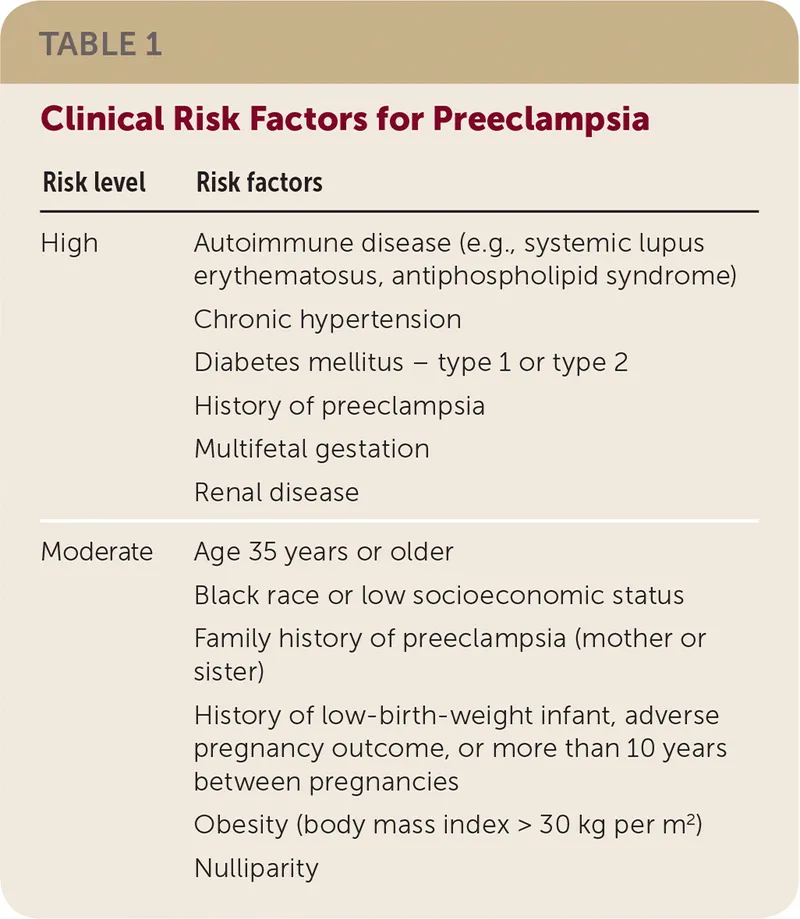
- **Nulliparity** (being a primigravida) is a significant risk factor for **preeclampsia**, the condition described by new-onset hypertension and proteinuria after 20 weeks of gestation.
- The risk of **preeclampsia** is typically highest in women experiencing their first pregnancy.
*Oral contraceptives intake*
- Past use of **oral contraceptives** is not associated with an increased risk of developing **preeclampsia**.
- Some studies suggest that prior use of combined oral contraceptives might even be associated with a *reduced* risk of preeclampsia, though this is not a consistent finding.
*BMI < 18.5 kg/m2 prior to pregnancy*
- This patient's pre-pregnancy BMI is 18.2 kg/m², indicating she was **underweight** (BMI < 18.5 kg/m²).
- **Underweight** status prior to pregnancy is generally *not* considered a risk factor for preeclampsia; rather, **obesity** (BMI > 30 kg/m²) is a known risk factor.
*Smoking prior to pregnancy*
- Smoking is generally harmful during pregnancy, but surprisingly, current **smoking** has been associated with a *reduced* risk of preeclampsia.
- While the patient has a history of smoking, it was prior to pregnancy and she is not currently smoking, and even active smoking is protective rather than a risk factor for preeclampsia.
*Family history of hypertension*
- While a family history of **essential hypertension** (chronic hypertension) is present (mother at 46, aunt at 51), it is *not* a direct risk factor for **preeclampsia**.
- The main genetic risk factor for preeclampsia is a family history of preeclampsia itself, not general hypertension.
More Screening for preeclampsia risk factors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.