Gestational diabetes management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gestational diabetes management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gestational diabetes management US Medical PG Question 1: A 52-year-old man presents to his primary care physician to discuss laboratory results that were obtained during his annual checkup. He has no symptoms or concerns and denies changes in eating or urination patterns. Specifically, the physician ordered a panel of metabolic laboratory tests to look for signs of diabetes, hyperlipidemia, or other chronic disorders. A spot glucose check from a random blood sample showed a glucose level of 211 mg/dL. A hemoglobin A1c level was obtained at the same time that showed a level of 6.3%. A fasting blood glucose was obtained that showed a blood glucose level of 125 mg/dL. Finally, a 2-hour glucose level was obtained after an oral glucose tolerance test that showed a glucose level of 201 mg/dL. Which of the following statements is most accurate for this patient?
- A. This patient does not have type 2 diabetes
- B. This patient has type 2 diabetes as diagnosed by his fasting blood glucose
- C. This patient has type 2 diabetes as diagnosed by his oral tolerance blood glucose (Correct Answer)
- D. This patient has type 2 diabetes as diagnosed by his random blood glucose
- E. This patient has type 2 diabetes as diagnosed by his hemoglobin A1c
Gestational diabetes management Explanation: **This patient has type 2 diabetes as diagnosed by his oral tolerance blood glucose**
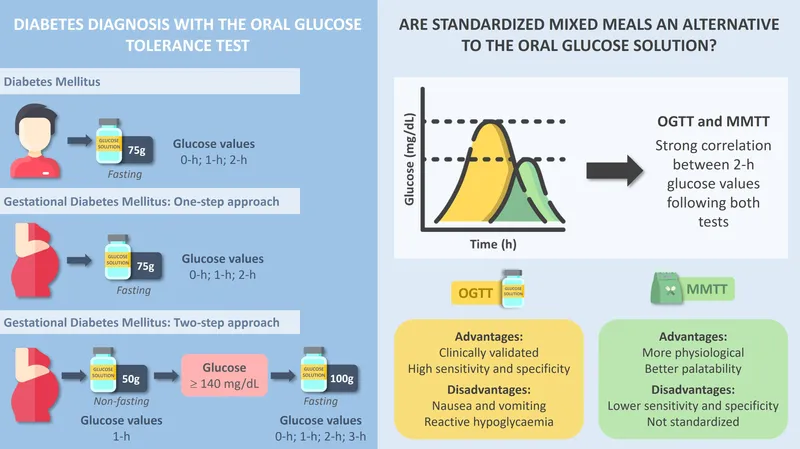
- A 2-hour plasma glucose of **200 mg/dL or higher** during an Oral Glucose Tolerance Test (OGTT) is a diagnostic criterion for diabetes. This patient's 2-hour glucose level of **201 mg/dL** meets this criterion.
- The combination of this elevated OGTT result with a random glucose over 200 mg/dL further supports the diagnosis, even in an asymptomatic individual.
*This patient does not have type 2 diabetes*
- The patient has multiple laboratory values that meet or exceed diagnostic thresholds for diabetes, including a random glucose of **211 mg/dL**, an HbA1c of **6.3%**, and a 2-hour OGTT glucose of **201 mg/dL**.
- While one individual threshold might not be conclusive, the overall pattern of results clearly indicates diabetes.
*This patient has type 2 diabetes as diagnosed by his fasting blood glucose*
- A fasting plasma glucose (FPG) of **126 mg/dL or higher** is diagnostic for diabetes. This patient's FPG of **125 mg/dL** is just below this threshold.
- While concerning, an FPG of 125 mg/dL alone is considered **impaired fasting glucose** (pre-diabetes), not diabetes.
*This patient has type 2 diabetes as diagnosed by his random blood glucose*
- A random plasma glucose of **200 mg/dL or higher** in a symptomatic patient is diagnostic for diabetes. However, this patient is **asymptomatic**.
- In an asymptomatic patient, an elevated random glucose requires confirmation by another diagnostic test (e.g., FPG, OGTT, or HbA1c) on a subsequent day, or concurrent with another positive test (like the OGTT in this case).
*This patient has type 2 diabetes as diagnosed by his hemoglobin A1c*
- An HbA1c level of **6.5% or higher** is diagnostic for diabetes. This patient's HbA1c of **6.3%** is below this cutoff.
- An HbA1c between 5.7% and 6.4% indicates **pre-diabetes**, specifically increased risk for diabetes.
Gestational diabetes management US Medical PG Question 2: A 31-year-old G1P0 woman at 26 weeks gestation presents to the clinic for evaluation of an abnormal glucose tolerance test. She denies any symptoms, but states that she was given 50 g of oral glucose 1 week earlier and demonstrated a subsequent venous plasma glucose level of 156 mg/dL 1 hour later. The vital signs are: blood pressure, 112/78 mm Hg; pulse, 81/min; and respiratory rate, 16/min. Physical examination is within normal limits. Which of the following is the most appropriate next step in management?
- A. Administer an oral, 3-hour 100 g glucose dose (Correct Answer)
- B. Advise the patient to follow an American Diabetic Association diet plan
- C. Repeat the 50 g oral glucose challenge
- D. Begin insulin treatment
- E. Order a fetal ultrasound examination
Gestational diabetes management Explanation: ***Administer an oral, 3-hour 100 g glucose dose***
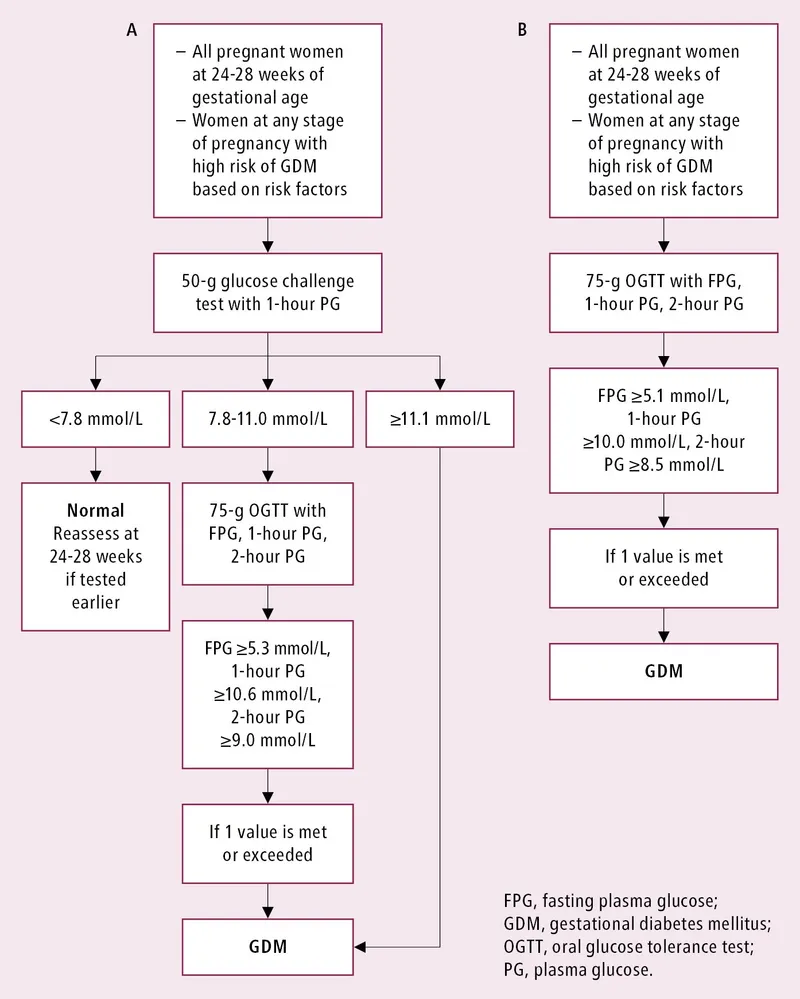
- This patient failed the initial **50 g, 1-hour glucose challenge test** (screen) because her plasma glucose was 156 mg/dL, which is above the typical threshold of 130-140 mg/dL.
- The next appropriate step for a failed screening test is to perform a **diagnostic 3-hour, 100 g oral glucose tolerance test (OGTT)** to confirm or rule out gestational diabetes.
*Advise the patient to follow an American Diabetic Association diet plan*
- While lifestyle modifications are important for managing gestational diabetes, this step is premature as the diagnosis has not yet been confirmed by the **diagnostic 3-hour OGTT**.
- Diet modification is part of the treatment for confirmed gestational diabetes, not the next diagnostic step.
*Repeat the 50 g oral glucose challenge*
- Repeating the screening test is not appropriate after a positive result; a diagnostic test is required to confirm the condition.
- The **50 g challenge** is a screening test with a high sensitivity but lower specificity, thus requiring a follow-up diagnostic test.
*Begin insulin treatment*
- **Insulin treatment** is reserved for patients officially diagnosed with gestational diabetes whose blood glucose levels cannot be controlled with diet and exercise alone.
- Prescribing insulin without a confirmed diagnosis is inappropriate and potentially harmful.
*Order a fetal ultrasound examination*
- A fetal ultrasound is used to monitor for complications of gestational diabetes like **macrosomia**, but it is not the next step in diagnosing the condition.
- While important for fetal surveillance in confirmed cases, it does not aid in the initial diagnosis of gestational diabetes itself.
Gestational diabetes management US Medical PG Question 3: A 21-year-old primigravida presents to her physician for a prenatal visit. She has a positive pregnancy test 1 week ago. The estimated gestational age is 16 weeks. She has no complaints. She has a history of type 1 diabetes mellitus and takes insulin for glucose control. The urine dipstick test shows 3+ glucose and negative for protein. The blood tests ordered at the last visit 1 week ago are as follows:
Fasting glucose 110 mg/dL
HbA1c 8.3%
Which of the following tests should be highly recommended for this patient?
- A. Chorionic villus sampling
- B. Triple test (Correct Answer)
- C. Serum creatinine
- D. C-peptide assessment
- E. Oral glucose tolerance test
Gestational diabetes management Explanation: ***Triple test***
- This 21-year-old patient with **pre-existing diabetes** and an **HbA1c of 8.3%** has a significantly increased risk of fetal neural tube defects and other chromosomal abnormalities. The triple test, performed between **15 and 20 weeks**, can screen for these risks by measuring **alpha-fetoprotein (AFP)**, **human chorionic gonadotropin (hCG)**, and **unconjugated estriol (uE3)**.
- Given the patient's **poor glycemic control** (HbA1c 8.3% indicates consistently high blood glucose levels), the triple test offers a non-invasive screening method to assess these elevated risks.
*Chorionic villus sampling*
- While CVS can detect chromosomal abnormalities and some genetic disorders, it is an **invasive procedure** associated with a risk of miscarriage and is typically performed earlier in pregnancy (10-13 weeks).
- It is usually reserved for cases with **higher risk factors** identified through non-invasive screening or a history of genetic disorders, which are not explicitly stated as the primary concern here compared to the hyperglycemia-related defects.
*Serum creatinine*
- **Serum creatinine** is used to assess kidney function and is essential in diabetic patients to monitor for nephropathy, but it is **not a screening test for fetal abnormalities**.
- While important for the mother's health management, it does not directly address the immediate concern of fetal risk due to uncontrolled diabetes during pregnancy.
*C-peptide assessment*
- **C-peptide** is a marker of endogenous insulin production and is useful in classifying diabetes type or assessing residual beta-cell function; however, this patient is a known **type 1 diabetic** taking insulin.
- While it has diagnostic utility for the mother's condition, it does not provide information about fetal well-being or the risk of congenital anomalies.
*Oral glucose tolerance test*
- An **oral glucose tolerance test (OGTT)** is used to diagnose **gestational diabetes mellitus** (GDM) in women without pre-existing diabetes, or to confirm it in those with borderline values.
- This patient already has a confirmed diagnosis of **type 1 diabetes**; therefore, an OGTT is not indicated for her as she is already being treated for diabetes.
Gestational diabetes management US Medical PG Question 4: A 37-year-old woman, gravida 3, para 2, at 28 weeks' gestation comes to the physician for a follow-up examination. One week ago, an oral glucose tolerance screening test showed elevated serum glucose levels. She has complied with the recommended diet and lifestyle modifications. Over the past week, home blood glucose monitoring showed elevated fasting and post-prandial blood glucose levels. Which of the following describes the mechanism of action of the most appropriate pharmacotherapy for this patient?
- A. Inhibition of alpha-glucosidase
- B. Closure of ATP-dependent K+-channels
- C. Inhibition of dipeptidyl peptidase 4
- D. Activation of peroxisome proliferator-activated receptor-gamma
- E. Binding to receptors with tyrosine kinase activity (Correct Answer)
Gestational diabetes management Explanation: ***Binding to receptors with tyrosine kinase activity***
- This mechanism describes **insulin**, which is the **first-line pharmacotherapy for gestational diabetes mellitus (GDM)** that is not controlled by diet and lifestyle modifications. Insulin binds to its receptor, activating **tyrosine kinase activity** and initiating a cascade of intracellular signaling that promotes glucose uptake and utilization.
- Given the **elevated fasting and post-prandial blood glucose levels** despite dietary changes, insulin therapy is indicated to manage GDM, which relies on this mechanism of action.
*Inhibition of alpha-glucosidase*
- **Alpha-glucosidase inhibitors** (e.g., acarbose, miglitol) delay carbohydrate absorption in the gut, primarily targeting post-prandial hyperglycemia.
- While these can be used in some forms of diabetes, they are generally **not preferred for GDM due to potential gastrointestinal side effects** and less effective control over fasting hyperglycemia compared to insulin.
*Closure of ATP-dependent K+-channels*
- Drugs like **sulfonylureas** (e.g., glyburide) act by **closing ATP-dependent K+-channels** on pancreatic beta cells, leading to depolarization and insulin release.
- **Glyburide** can be used in GDM but is a controversial choice due to its potential to **cross the placenta** and cause fetal hypoglycemia.
*Inhibition of dipeptidyl peptidase 4*
- **Dipeptidyl peptidase-4 (DPP-4) inhibitors** (e.g., sitagliptin, saxagliptin) enhance the action of incretin hormones, stimulating glucose-dependent insulin release and suppressing glucagon secretion.
- There is **limited data on the safety and efficacy of DPP-4 inhibitors in pregnancy**, and they are not typically recommended for GDM.
*Activation of peroxisome proliferator-activated receptor-gamma*
- This mechanism describes **thiazolidinediones (TZDs)**, such as pioglitazone and rosiglitazone, which improve insulin sensitivity.
- **TZDs are contraindicated in pregnancy** due to potential adverse effects on the fetus, including increased risk of cardiovascular defects and fluid retention.
Gestational diabetes management US Medical PG Question 5: A 27-year-old Hispanic G2P1 presents for a routine antepartum visit at 26 weeks gestation. She has no complaints. The vital signs are normal, the physical examination is within normal limits, and the gynecologic examination corresponds to 25 weeks gestation. The oral glucose tolerance test (OGTT) with a 75-g glucose load is significant for a glucose level of 177 mg/dL at 1 hour and 167 mg/dL at 2 hour. The fasting blood glucose level is 138 mg/dL (7.7 mmol/L), and the HbA1c is 7%. Which of the following represents the proper initial management?
- A. Sitagliptin
- B. Dietary and lifestyle modification
- C. Metformin
- D. Glyburide
- E. Insulin (Correct Answer)
Gestational diabetes management Explanation: **Insulin**
- The patient's **fasting glucose of 138 mg/dL** and **HbA1c of 7%** indicate pre-existing **Type 2 Diabetes Mellitus**, not just gestational diabetes. Both values exceed the diagnostic thresholds for overt diabetes in pregnancy.
- **Insulin** is the preferred initial pharmacologic treatment for **overt diabetes in pregnancy** because it does not cross the placenta, ensuring fetal safety, and is highly effective in controlling maternal glucose levels.
*Sitagliptin*
- **Sitagliptin** is a **DPP-4 inhibitor** and is not recommended during pregnancy due to limited safety data and the availability of safer alternatives.
- Oral hypoglycemic agents are generally avoided as first-line therapy for established diabetes in pregnancy due to potential for placental transfer and adverse fetal effects.
*Dietary and lifestyle modification*
- While crucial, **dietary and lifestyle modification** alone are insufficient for managing overt diabetes with such high fasting glucose and HbA1c levels.
- These measures are usually the first step for **gestational diabetes**, but a patient with overt diabetes requires immediate pharmacologic intervention to prevent complications.
*Metformin*
- **Metformin** can be used in pregnancy but is primarily considered for **gestational diabetes** or as an alternative to insulin if the patient has milder hyperglycemia, or if insulin is poorly tolerated.
- Given the patient's significantly elevated fasting glucose and HbA1c, **insulin** is a more effective and immediate treatment to achieve glycemic control and reduce risks.
*Glyburide*
- **Glyburide** is an **oral sulfonylurea** that can cross the placenta, leading to potential fetal hyperinsulinemia and neonatal hypoglycemia.
- Its use in pregnancy is generally discouraged due to these risks, making **insulin** a safer and more appropriate choice.
Gestational diabetes management US Medical PG Question 6: A 31-year-old G1P0000 presents to her obstetrician for her first prenatal visit after having a positive home pregnancy test one week ago. She states that her last menstrual period was 8 weeks ago. The patient has a past medical history of type I diabetes mellitus since childhood and is on insulin. Her hemoglobin A1c two weeks ago was 13.7%. At that time, she was also found to have microalbuminuria on routine urinalysis, and her primary care provider prescribed lisinopril but the patient has not yet started taking it. The patient’s brother is autistic, but family history is otherwise unremarkable. At this visit, her temperature is 98.6°F (37.0°C), blood pressure is 124/81 mmHg, pulse is 75/min, and respirations are 14/min. Exam is unremarkable. This fetus is at increased risk for which of the following?
- A. Post-term delivery
- B. Oligohydramnios
- C. Neural tube defect (Correct Answer)
- D. Aneuploidy
- E. Neonatal hyperglycemia
Gestational diabetes management Explanation: ***Neural tube defect***
- The patient's **poorly controlled type 1 diabetes mellitus** is evidenced by her **HbA1c of 13.7%**. Uncontrolled maternal hyperglycemia during organogenesis significantly increases the risk for fetal malformations, including neural tube defects due to impaired folate metabolism.
- This risk is highest when hyperglycemia occurs during the first 8 weeks of gestation, a period crucial for neural tube closure, which aligns with this patient's presentation at 8 weeks' gestation.
*Post-term delivery*
- **Uncontrolled maternal diabetes** is typically associated with **macrosomia and polyhydramnios**, which can lead to complications such as **shoulder dystocia, premature rupture of membranes (PROM)**, and often precipitates **earlier induction of labor** rather than post-term delivery.
- While exact delivery timing can vary, the direct causal link between uncontrolled diabetes and post-term delivery is not primary; rather, such pregnancies are often managed with earlier interventions.
*Oligohydramnios*
- Poorly controlled maternal diabetes, particularly type 1, is generally associated with **polyhydramnios** due to fetal polyuria caused by hyperglycemia, not oligohydramnios.
- **Oligohydramnios** can be associated with severe **placental insufficiency**, prolonged rupture of membranes, or fetal renal agenesis, none of which are directly indicated by uncontrolled maternal diabetes alone.
*Aneuploidy*
- The primary risk factor for **aneuploidy** (e.g., Down syndrome) is **advanced maternal age**, which is not present in this 31-year-old patient.
- **Maternal diabetes** itself is not a direct risk factor for aneuploidy; genetic factors related to nondisjunction are the main cause.
*Neonatal hyperglycemia*
- Maternal hyperglycemia leads to fetal hyperglycemia, causing **fetal hyperinsulinemia**. After birth, the neonate's elevated insulin levels, in the absence of maternal glucose supply, result in **neonatal hypoglycemia**, not hyperglycemia.
- **Neonatal hyperglycemia** is rare and usually associated with specific genetic defects or administration of excessive glucose postnatally, not maternal diabetes.
Gestational diabetes management US Medical PG Question 7: A 31-year-old G3P2 who is at 24 weeks gestation presents for a regular check-up. She has no complaints, no concurrent diseases, and her previous pregnancies were vaginal deliveries with birth weights of 3100 g and 4180 g. The patient weighs 78 kg (172 lb) and is 164 cm (5 ft 5 in) in height. She has gained 10 kg (22 lb) during the current pregnancy. Her vital signs and physical examination are normal. The plasma glucose level is 190 mg/dL after a 75-g oral glucose load. Which of the listed factors contributes to the pathogenesis of the patient’s condition?
- A. Decrease in insulin gene expression
- B. Insulin antagonism of human placental lactogen (Correct Answer)
- C. Production of autoantibodies against pancreatic beta cells
- D. Decrease in insulin sensitivity of maternal tissues caused by alpha-fetoprotein
- E. Point mutations in the gene coding for insulin
Gestational diabetes management Explanation: ***Insulin antagonism of human placental lactogen***
- The patient's elevated plasma glucose indicates **gestational diabetes mellitus (GDM)**, a condition characterized by **insulin resistance** that emerges during pregnancy.
- **Human placental lactogen (hPL)**, secreted by the placenta, is a key hormone that **antagonizes maternal insulin**, contributing significantly to the insulin resistance seen in GDM.
*Decrease in insulin gene expression*
- A decrease in insulin gene expression would lead to **reduced insulin production**, which is not the primary mechanism of insulin resistance in GDM.
- While pancreatic beta cells compensate by increasing insulin secretion in GDM, the underlying problem is the **tissue's reduced response** to insulin.
*Production of autoantibodies against pancreatic beta cells*
- This mechanism is characteristic of **Type 1 diabetes**, where the immune system destroys insulin-producing beta cells, leading to absolute insulin deficiency.
- GDM is primarily a condition of **insulin resistance**, not autoimmune destruction of beta cells.
*Decrease in insulin sensitivity of maternal tissues caused by alpha-fetoprotein*
- **Alpha-fetoprotein (AFP)** is primarily involved in fetal development and is not known to directly cause a decrease in maternal insulin sensitivity.
- The main placental hormones contributing to insulin resistance are **hPL**, progesterone, and cortisol, not AFP.
*Point mutations in the gene coding for insulin*
- **Point mutations** in the insulin gene are rare and would typically manifest as forms of monogenic diabetes or insulin-related disorders, not characteristic GDM.
- GDM is generally a polygenic or multifactorial condition influenced by pregnancy hormones and pre-existing insulin resistance.
Gestational diabetes management US Medical PG Question 8: A 29-year-old primigravid woman at 24 weeks' gestation comes to the physician for a prenatal visit. She feels well. She has no personal history of serious illness. Medications include iron supplements and a multivitamin. Her temperature is 37.2°C (99°F) and blood pressure is 108/60 mm Hg. Pelvic examination shows a uterus consistent in size with a 24-week gestation. A 1-hour 50-g glucose challenge shows a glucose concentration of 155 mg/dL (N < 135 mg/dL). A 100-g oral glucose tolerance test shows glucose concentrations of 205 mg/dL (N < 180 mg/dL) and 154 mg/dL (N <140 mg/dL) at 1 and 3 hours, respectively. She refuses treatment with insulin. Which of the following complications is her infant at greatest risk of developing at birth?
- A. Respiratory distress syndrome
- B. Hyperbilirubinemia (Correct Answer)
- C. Birth trauma/shoulder dystocia
- D. Macrosomia
- E. Neonatal hypoglycemia
Gestational diabetes management Explanation: ***Hyperbilirubinemia***
- Uncontrolled maternal diabetes leads to **fetal hyperglycemia**, causing fetal hyperinsulinemia.
- **Fetal hyperinsulinemia** contributes to accelerated breakdown of fetal red blood cells, leading to increased bilirubin production and, consequently, **neonatal hyperbilirubinemia**.
*Respiratory distress syndrome*
- While fetal hyperinsulinemia can delay fetal lung maturation and increase the risk of respiratory distress syndrome, it is typically due to **inhibition of surfactant production**.
- However, in term infants of diabetic mothers, the primary risk is often related to other metabolic complications like hypoglycemia or hyperbilirubinemia, and RDS is more characteristic of prematurity or poorly controlled diabetes overall, not the most direct or immediate risk over hyperbilirubinemia here.
*Birth trauma/shoulder dystocia*
- This complication is related to **macrosomia**, where the large size of the infant increases the risk during delivery.
- While severe macrosomia can increase the risk of birth trauma, fetal hyperinsulinemia also directly causes effects that raise the risk of hyperbilirubinemia.
*Macrosomia*
- Fetal hyperglycemia in uncontrolled diabetes leads to an increase in **fetal insulin production**, which acts as a growth factor, leading to excessive fetal growth or **macrosomia**.
- While macrosomia is a significant complication, the question asks for the greatest risk at birth, and macrosomia itself is a condition, while hyperbilirubinemia is a direct consequence that typically manifests shortly after birth.
*Neonatal hypoglycemia*
- After birth, the sudden cessation of maternal glucose supply, coupled with continued **fetal hyperinsulinemia**, can lead to a rapid drop in the neonate's blood glucose levels.
- Although neonatal hypoglycemia is a significant risk, the question asks for the greatest risk at birth, and hyperbilirubinemia is also a prominent and often more prolonged metabolic issue.
Gestational diabetes management US Medical PG Question 9: A 22-year-old Caucasian G1 presents to her physician at 29 weeks gestation for a checkup. The medical history is unremarkable and the current pregnancy has been uncomplicated. Her weight is 81 kg (178.6 lb) and the height is 169 cm (5 ft 6 in). She has gained 13 kg (28.6 lb) during the pregnancy. She has no abnormalities on physical examination. Which of the following screening tests should be obtained ?
- A. Measurement of HbA1c
- B. Fasting glucose level
- C. Fasting oral glucose test with 50 g of glucose
- D. Non-fasting oral glucose load test with 75 g of glucose
- E. Non-fasting oral glucose challenge test with 50 g of glucose (Correct Answer)
Gestational diabetes management Explanation: ***Non-fasting oral glucose challenge test with 50 g of glucose***
- This patient is at 29 weeks gestation, which is the recommended time for **gestational diabetes mellitus (GDM) screening** between **24 and 28 weeks**.
- A 50g non-fasting glucose challenge test is the **initial screening step**, followed by a diagnostic 100g 3-hour oral glucose tolerance test if the screen is abnormal.
*Measurement of HbA1c*
- **HbA1c** is used to diagnose pre-existing diabetes or to monitor long-term glycemic control, but it is **not the primary screening test for GDM** due to its limitations in reflecting acute glucose fluctuations in pregnancy.
- While it can be useful in some cases, it's not the standard initial screening tool for GDM.
*Fasting glucose level*
- A **fasting glucose level** is part of the diagnostic oral glucose tolerance test (OGTT) but is **not typically used as a standalone screening test** for GDM.
- It would require the patient to fast, which is not part of the initial screening challenge.
*Fasting oral glucose test with 50 g of glucose*
- The initial glucose challenge test is **non-fasting** and involves 50g of glucose.
- A **fasting** state is reserved for the **diagnostic 100g or 75g OGTT**, not the initial screening.
*Non-fasting oral glucose load test with 75 g of glucose*
- A **75g oral glucose tolerance test (OGTT)** is a diagnostic test for GDM, **not an initial screening test**.
- It is used when the 50g glucose challenge test is abnormal or in certain high-risk populations as the sole diagnostic step.
Gestational diabetes management US Medical PG Question 10: A 36-year-old primigravida presents to her obstetrician for antenatal care. She is at 24 weeks of gestation and does not have any current complaint except for occasional leg cramps. She does not smoke or drink alcohol. Family history is irrelevant. Her temperature is 36.9°C (98.42°F), blood pressure is 100/60 mm Hg, and pulse of 95/minute. Her body mass index is 21 kg/m² (46 pounds/m²). Physical examination reveals a palpable uterus above the umbilicus with no other abnormalities. Which of the following screening tests is suitable for this patient?
- A. Fasting and random glucose testing for gestational diabetes mellitus
- B. HbA1C for gestational diabetes mellitus
- C. Oral glucose tolerance test for gestational diabetes mellitus (Correct Answer)
- D. Complete blood count for iron deficiency anemia
- E. Wet mount microscopy of vaginal secretions for bacterial vaginosis
Gestational diabetes management Explanation: ***Oral glucose tolerance test for gestational diabetes mellitus***
- The **oral glucose tolerance test (OGTT)**, typically performed between **24 and 28 weeks of gestation**, is the gold standard for screening and diagnosing **gestational diabetes mellitus (GDM)**. This patient is at 24 weeks, making it the appropriate time for this screening.
- GDM, if undiagnosed and untreated, can lead to significant maternal and fetal complications, including **macrosomia**, **preeclampsia**, **neonatal hypoglycemia**, and **shoulder dystocia**.
*Fasting and random glucose testing for gestational diabetes mellitus*
- While **fasting** or **random glucose** values can indicate hyperglycemia, they are **not sensitive or specific enough** on their own to reliably screen for or diagnose GDM.
- A single elevated reading might prompt further testing, but it's not the primary or most suitable screening method.
*HbA1C for gestational diabetes mellitus*
- **HbA1c** reflects **average blood glucose levels over the past 2-3 months** and is primarily used for diagnosing and monitoring **pre-existing diabetes** or assessing glycemic control in non-pregnant individuals.
- Due to the **physiological changes in red blood cell turnover during pregnancy** and the acute onset nature of GDM, HbA1c is **not recommended** as a first-line screening tool for GDM.
*Complete blood count for iron deficiency anemia*
- While **complete blood count (CBC)** is a routine prenatal screening test to check for **anemia**, it is typically done earlier in pregnancy and again in the third trimester. There are no specific symptoms in this patient that strongly suggest immediate concern for anemia beyond routine.
- The question specifically asks for the "most suitable" screening test at this gestational age, and the **GDM screening** takes precedence given the timing.
*Wet mount microscopy of vaginal secretions for bacterial vaginosis*
- There are **no symptoms of vaginal infection** (e.g., unusual discharge, itching, odor) mentioned in the patient's presentation that would warrant immediate screening for **bacterial vaginosis (BV)** at this visit.
- While BV can be associated with adverse pregnancy outcomes, routine asymptomatic screening by wet mount is **not universally recommended** at 24 weeks gestation without other indications.
More Gestational diabetes management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.