Diagnostic testing (amniocentesis, CVS) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diagnostic testing (amniocentesis, CVS). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 1: A 36-year old pregnant woman (gravida 4, para 1) presents at week 11 of pregnancy. Currently, she has no complaints. She had an uncomplicated 1st pregnancy that ended in an uncomplicated vaginal delivery at the age of 28 years. Her male child was born healthy, with normal physical and psychological development over the years. Two of her previous pregnancies were spontaneously terminated in the 1st trimester. Her elder sister has a child born with Down syndrome. The patient denies smoking and alcohol consumption. Her blood analysis reveals the following findings:
Measured values
Beta human chorionic gonadotropin (beta-hCG) High
Pregnancy-associated plasma protein-A (PAPP-A) Low
Which of the following is the most appropriate next step in the management of this patient?
- A. Perform an ultrasound examination with nuchal translucency and crown-rump length measurement
- B. Recommend chorionic villus sampling with subsequent cell culturing and karyotyping (Correct Answer)
- C. Offer a blood test for rubella virus, cytomegalovirus, and toxoplasma IgG
- D. Recommend amniocentesis with subsequent cell culturing and karyotyping
- E. Schedule a quadruple test at the 15th week of pregnancy
Diagnostic testing (amniocentesis, CVS) Explanation: ***Recommend chorionic villus sampling with subsequent cell culturing and karyotyping***
- The patient's **advanced maternal age** (36 years), history of **recurrent first-trimester miscarriages**, and a **family history of Down syndrome** in her sister's child are significant risk factors for **chromosomal abnormalities**.
- The abnormal first-trimester screening results (**high beta-hCG, low PAPP-A**) are highly suggestive of **aneuploidies**, particularly **Down syndrome (Trisomy 21)**. **Chorionic villus sampling (CVS)** is the most appropriate next step for definitive diagnosis as it can be performed earlier (10-13 weeks) than amniocentesis for definitive diagnosis via karyotyping.
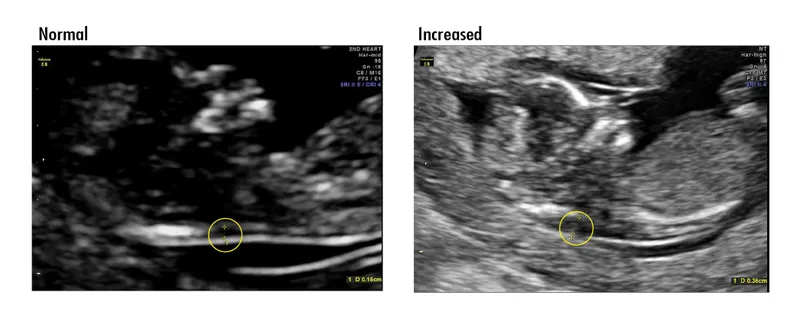
*Perform an ultrasound examination with nuchal translucency and crown-rump length measurement*
- While a **nuchal translucency (NT) measurement** is part of the first-trimester screening and would confirm an increased risk, it is a screening, not a diagnostic, test.
- Given the patient's strong risk factors and abnormal biochemical markers, a definitive diagnostic test is warranted rather than another screening measure.
*Offer a blood test for rubella virus, cytomegalovirus, and toxoplasma IgG*
- This patient has a history of recurrent miscarriages and a family history suggestive of chromosomal abnormalities, along with abnormal first-trimester biochemical markers.
- While infections can cause miscarriage, the clinical picture strongly points towards a **chromosomal etiology**, making infection screening less urgent as a primary next step.
*Recommend amniocentesis with subsequent cell culturing and karyotyping*
- **Amniocentesis** is a diagnostic test for chromosomal abnormalities but is typically performed later in pregnancy, usually between **15 and 20 weeks**.
- Given the patient is at 11 weeks, **CVS** is the more appropriate and earlier diagnostic option for definitive diagnosis of potential aneuploidies.
*Schedule a quadruple test at the 15th week of pregnancy*
- The **quadruple test** is a second-trimester screening test and would provide more risk assessment rather than a definitive diagnosis.
- The patient already has strong indications for a chromosomal abnormality based on age, history, and first-trimester screening, necessitating an **earlier definitive diagnostic test**.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 2: A 36-year-old G3P2002 presents to her obstetrician’s office for her first prenatal visit at ten weeks and two days gestation. She notes that she has felt nauseous the last several mornings and has been especially tired for a few weeks. Otherwise, she feels well. The patient has had two uncomplicated spontaneous vaginal deliveries at full term with her last child born six years ago. She is concerned about the risk of Down syndrome in this fetus, as her sister gave birth to an affected child at age 43. The patient has a history of generalized anxiety disorder, atopic dermatitis, and she is currently on escitalopram. At this visit, this patient’s temperature is 98.6°F (37.0°C), pulse is 70/min, blood pressure is 121/67 mmHg, and respirations are 13/min. The patient appears anxious, but overall comfortable, and cardiopulmonary and abdominal exams are unremarkable. Pelvic exam reveals normal female external genitalia, a closed and slightly soft cervix, a ten-week-sized uterus, and no adnexal masses. Which of the following is the best next step for definitively determining whether this patient’s fetus has Down syndrome?
- A. Anatomy ultrasound
- B. Genetic testing of patient’s sister
- C. Chorionic villus sampling (Correct Answer)
- D. Nuchal translucency test
- E. Amniocentesis
Diagnostic testing (amniocentesis, CVS) Explanation: ***Chorionic villus sampling***
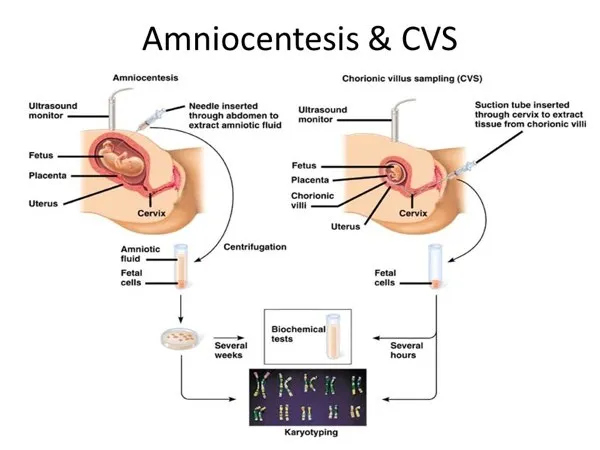
- **Chorionic villus sampling (CVS)** is a diagnostic procedure performed between 10 and 13 weeks of gestation that involves taking a sample of placental tissue for genetic analysis. It provides a definitive diagnosis for chromosomal abnormalities like **Down syndrome** earlier in pregnancy than amniocentesis.
- Given the patient's anxiety and desire for definitive diagnosis due to family history, CVS is the most appropriate next step for an early and conclusive result.
*Anatomy ultrasound*
- An **anatomy ultrasound** (typically performed at 18-20 weeks) is a screening, not diagnostic, tool for fetal anomalies. While it can detect **structural abnormalities** associated with Down syndrome, it cannot definitively diagnose the condition.
- It would be too late to provide the early definitive diagnosis the patient is seeking regarding **Down syndrome**.
*Genetic testing of patient’s sister*
- The sister's genetic testing would confirm her child's diagnosis or carrier status for **chromosomal translocations**, but it does not provide information about the current patient's fetus.
- A definitive diagnosis for the current pregnancy must come from **fetal genetic material**.
*Nuchal translucency test*
- The **nuchal translucency test** is a **screening test** performed between 11 and 14 weeks that measures the fluid at the back of the fetal neck and is used in conjunction with biochemical markers (first-trimester screening) to assess the risk of Down syndrome. It is not diagnostic.
- An abnormal result would indicate an increased risk but would still require a **diagnostic test** like CVS or amniocentesis for confirmation.
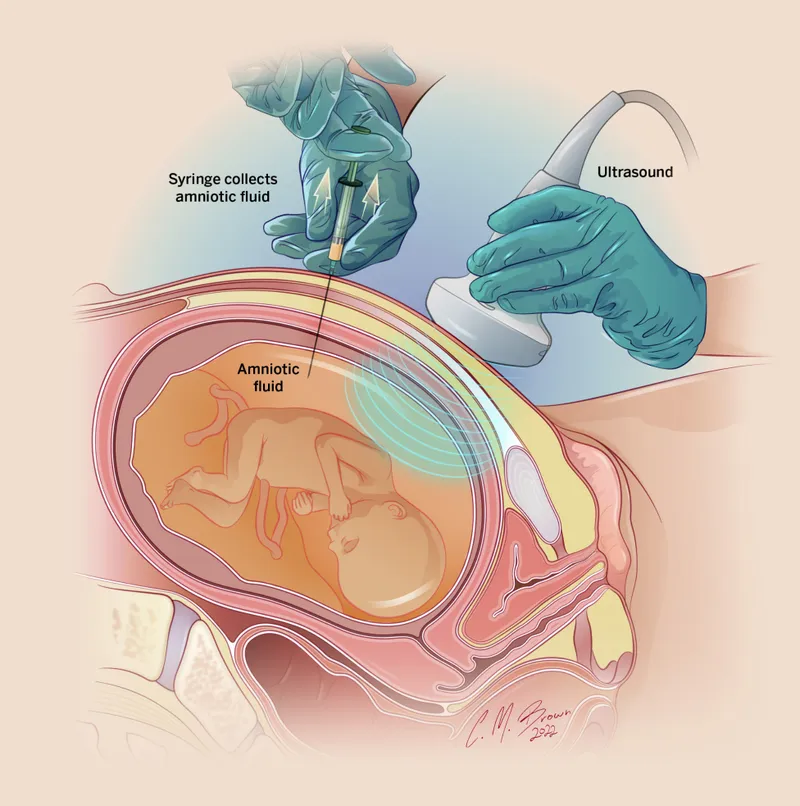
*Amniocentesis*
- **Amniocentesis** is a diagnostic procedure that samples amniotic fluid for genetic analysis, typically performed between 15 and 20 weeks of gestation.
- While it provides a definitive diagnosis for **chromosomal abnormalities**, it is usually performed later in pregnancy than CVS. The patient is at 10 weeks and two days, making CVS a timelier option for early diagnosis.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 3: A 26-year-old pregnant woman (gravida 2, para 1) presents on her 25th week of pregnancy. Currently, she has no complaints. Her previous pregnancy was unremarkable. No abnormalities were detected on the previous ultrasound (US) examination at week 13 of pregnancy. She had normal results on the triple test. She is human immunodeficiency virus (HIV), hepatitis B virus (HBV), and hepatitis C virus (HCV)-negative. Her blood type is III(B) Rh+, and her partner has blood type I(0) Rh-. She and her husband are both of Sardinian descent, do not consume alcohol, and do not smoke. Her cousin had a child who died soon after the birth, but she doesn't know the reason. She does not report a history of any genetic conditions in her family, although notes that her grandfather “was always yellowish-pale, fatigued easily, and had problems with his gallbladder”. Below are her and her partner’s complete blood count and electrophoresis results.
Complete blood count
Patient Her husband
Erythrocytes 3.3 million/mm3 4.2 million/mm3
Hb 11.9 g/dL 13.3 g/dL
MCV 71 fL 77 fL
Reticulocyte count 0.005 0.008
Leukocyte count 7,500/mm3 6,300/mm3
Platelet count 190,000/mm3 256,000/mm3
Electrophoresis
HbA1 95% 98%
HbA2 3% 2%
HbS 0% 0%
HbH 2% 0%
The patient undergoes ultrasound examination which reveals ascites, liver enlargement, and pleural effusion in the fetus. Further evaluation with Doppler ultrasound shows elevated peak systolic velocity of the fetal middle cerebral artery. Which of the following procedures can be performed for both diagnostic and therapeutic purposes in this case?
- A. Fetoscopy
- B. Cordocentesis (Correct Answer)
- C. Percutaneous fetal thoracentesis
- D. Chorionic villus sampling
- E. Amniocentesis
Diagnostic testing (amniocentesis, CVS) Explanation: ***Cordocentesis***
- **Cordocentesis** involves obtaining a fetal blood sample from the umbilical cord, which is crucial for diagnosing fetal anemia and can also be used for **intrauterine blood transfusions** if severe anemia is detected.
- The ultrasound findings of **ascites**, **liver enlargement**, **pleural effusion** (suggesting **hydrops fetalis**), and elevated peak systolic velocity of the fetal middle cerebral artery are highly indicative of severe fetal anemia, making cordocentesis a diagnostic and therapeutic option.
*Fetoscopy*
- **Fetoscopy** currently has limited diagnostic and therapeutic applications in cases of fetal anemia and is primarily used for direct visualization and certain surgical procedures like **laser coagulation** in twin-twin transfusion syndrome, which is not the primary issue here.
- While it offers direct visualization, it is more invasive and carries higher risks compared to cordocentesis for the specific diagnosis and management of fetal anemia.
*Percutaneous fetal thoracentesis*
- **Percutaneous fetal thoracentesis** is used to drain fetal pleural effusions, which is a symptom of hydrops fetalis, but it does not address the underlying cause of fetal anemia itself.
- It is a therapeutic procedure for a specific complication, not a diagnostic tool for anemia or a therapy for the anemia itself.
*Chorionic villus sampling*
- **Chorionic villus sampling (CVS)** is typically performed earlier in pregnancy (10-13 weeks) for **chromosomal analysis** and genetic disorders.
- It provides genetic information but cannot assess the current state of fetal anemia or provide therapeutic intervention like blood transfusion.
*Amniocentesis*
- **Amniocentesis** is primarily used for **genetic testing** and evaluating fetal lung maturity, usually performed after 15 weeks.
- It involves sampling amniotic fluid and does not directly provide a fetal blood sample for diagnosing or treating anemia.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 4: A 35-year-old woman gravida 2, para 1, comes to the physician for her first prenatal visit. Pregnancy and delivery of her first child were uncomplicated. She is not sure about the date of her last menstrual period. Pelvic examination shows a uterus consistent in size with a 10-week gestation. An ultrasound examination confirms the gestational age and shows one fetus with no indication of multiple gestations. During counseling on pregnancy risks and possible screening and diagnostic tests, the patient states she would like to undergo screening for Down syndrome. She would prefer immediate and secure screening with a low risk to herself and the fetus. Which of the following is the most appropriate next step in management at this time?
- A. Nuchal translucency, pregnancy-associated plasma protein-A, human chorionic gonadotropin
- B. Maternal serum α-fetoprotein, human chorionic gonadotropin, unconjugated estriol, and inhibin A
- C. Chorionic villus sampling
- D. Amniocentesis
- E. Cell-free fetal DNA testing (Correct Answer)
Diagnostic testing (amniocentesis, CVS) Explanation: ***Cell-free fetal DNA testing***
- This is the most appropriate choice given the patient's desire for **immediate and secure screening with low risk** because it is a **non-invasive prenatal screening (NIPS)** method offering high sensitivity and specificity for Down syndrome, particularly in higher-risk pregnancies.
- It involves a simple maternal blood draw and can be performed as early as **10 weeks of gestation**, perfectly aligning with the patient's current gestational age and desire for early screening.
*Nuchal translucency, pregnancy-associated plasma protein-A, human chorionic gonadotropin*
- This combination represents the **first-trimester combined screen**, which is typically performed between 11 and 14 weeks of gestation. While suitable for early screening, **cell-free DNA testing offers higher detection rates and lower false-positive rates** for Down syndrome.
- The patient specifically asked for the most **secure and least risky** screening, and NIPS outperforms the combined screen in terms of diagnostic accuracy for aneuploidies.
*Maternal serum α-fetoprotein, human chorionic gonadotropin, unconjugated estriol, and inhibin A*
- This refers to the **quad screen**, which is typically performed in the **second trimester (15-20 weeks)**, making it too late for the patient's desire for immediate screening at 10 weeks gestational age.
- While a widely used screening tool, the quad screen has a **lower detection rate** for Down syndrome compared to cell-free DNA testing.
*Chorionic villus sampling*
- **Chorionic villus sampling (CVS)** is a **diagnostic, invasive procedure** that carries a small risk of miscarriage (approximately 1 in 455 or 0.22%) and is not a screening test.
- Although it can be performed earlier (typically between 10 and 13 weeks), the patient specifically requested a **low-risk screening** option, which CVS is not.
*Amniocentesis*
- **Amniocentesis** is also an **invasive diagnostic procedure** with a risk of miscarriage (approximately 1 in 900 or 0.11%) and is typically performed in the **second trimester (15-20 weeks)**.
- This option is unsuitable because the patient is at 10 weeks gestation and desires **immediate and low-risk screening**, not a diagnostic procedure with procedural risks a few weeks later.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 5: A 28-year-old G2P1 female is concerned that she may give birth to another child with Down syndrome. She states that she may not be able to take care of another child with this disorder. Which of the following tests can confirm the diagnosis of Down syndrome in utero?
- A. Ultrasound
- B. Triple marker test
- C. Integrated test
- D. Quadruple marker test
- E. Amniocentesis (Correct Answer)
Diagnostic testing (amniocentesis, CVS) Explanation: ***Amniocentesis***
- **Amniocentesis** is a **diagnostic procedure** that involves collecting amniotic fluid to obtain fetal cells for **karyotyping**, which can definitively confirm the presence of an extra chromosome 21, the cause of Down syndrome.
- This test is typically performed between **15 and 20 weeks of gestation** and carries a small risk of complication but offers conclusive results.
*Ultrasound*
- **Ultrasound** is a **screening tool** that can detect anatomical features suggestive of Down syndrome, such as **nuchal translucency** or heart defects, but it cannot definitively diagnose the condition.
- It identifies **markers** that increase the suspicion of Down syndrome, prompting further diagnostic testing, but does not provide genetic confirmation.
*Triple marker test*
- The **triple marker test** is a **screening test** that measures levels of **alpha-fetoprotein (AFP)**, **unconjugated estriol (uE3)**, and **human chorionic gonadotropin (hCG)** in maternal blood.
- While it can estimate the risk of Down syndrome, it is not a diagnostic test and only provides a **risk assessment**, not a definitive diagnosis.
*Integrated test*
- The **integrated test** combines results from first-trimester screening (nuchal translucency and PAPP-A) and second-trimester screening (quadruple marker test) to provide a **single risk assessment**.
- Like other screening tests, it calculates a **risk probability** for Down syndrome but does not offer a definitive diagnosis.
*Quadruple marker test*
- The **quadruple marker test** measures AFP, uE3, hCG, and **inhibin A** in maternal blood during the second trimester.
- It is a **screening test** used to assess the risk of Down syndrome and open neural tube defects, but it is not a diagnostic tool.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 6: A 37-year-old primigravid woman comes to the physician at 13 weeks' gestation for a prenatal visit. She feels well. Her only medication is folic acid. Vital signs are within normal limits. Pelvic examination shows a uterus consistent in size with a 13-week gestation. Ultrasonography shows a nuchal translucency above the 99th percentile. Maternal serum pregnancy-associated plasma protein A is decreased and human chorionic gonadotropin concentrations are elevated to 2 times the median level. Which of the following is most likely to confirm the diagnosis?
- A. Chorionic villus sampling (Correct Answer)
- B. Cell-free DNA testing
- C. Triple screening test
- D. Amniocentesis
- E. Quadruple marker test
Diagnostic testing (amniocentesis, CVS) Explanation: ***Chorionic villus sampling***
- This procedure can be performed between **10 to 13 weeks of gestation** to obtain fetal cells for genetic analysis, which is within the patient's gestational age.
- It provides a definitive diagnosis of **chromosomal abnormalities** by directly sampling placental tissue, which shares the same genetic material as the fetus.
*Cell-free DNA testing*
- While it has high sensitivity and specificity for various **aneuploidies**, it is a **screening test**, not a diagnostic one.
- An abnormal result from cell-free DNA testing still requires **confirmatory diagnostic testing** such as CVS or amniocentesis.
*Triple screening test*
- This test is typically performed between **15 and 20 weeks of gestation**, which is too late to confirm the findings presented at 13 weeks gestation.
- It measures **AFP, hCG, and unconjugated estriol**, and an abnormal result would indicate a need for further diagnostic testing.
*Amniocentesis*
- This procedure is generally performed later in pregnancy, typically between **15 and 20 weeks gestation**, so it would require waiting several more weeks.
- While it provides definitive genetic results, **chorionic villus sampling is preferred at 13 weeks** due to earlier diagnostic potential.
*Quadruple marker test*
- This test is also performed between **15 and 20 weeks of gestation** and measures **AFP, hCG, unconjugated estriol, and inhibin A**.
- It is a **screening test**, similar to the triple screen, and does not provide a definitive diagnosis, requiring further confirmatory testing if abnormal.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 7: A 34-year-old gravida 2 para 1 woman at 16 weeks gestation presents for prenatal care. Her prenatal course has been uncomplicated. She takes no medications besides her prenatal vitamin which she takes every day, and she has been compliant with routine prenatal care. She has a 7-year-old daughter who is healthy. The results of her recent quadruple screen are listed below:
AFP: Low
hCG: Low
Estriol: Low
Inhibin-A: Normal
Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Chorionic villus sampling
- B. Amniocentesis (Correct Answer)
- C. Ultrasound for nuchal translucency
- D. Folic acid supplementation
- E. Return to clinic in 4 weeks
Diagnostic testing (amniocentesis, CVS) Explanation: ***Amniocentesis***
- The presented quad screen results (low AFP, low hCG, low estriol, normal Inhibin-A) are highly suggestive of **trisomy 18 (Edwards syndrome)**. Amniocentesis is a **definitive diagnostic test** that can confirm aneuploidy by providing a fetal karyotype.
- While typically performed between **15 and 20 weeks gestation**, it can differentiate between trisomy 18 and trisomy 21 (Down syndrome), which usually presents with high hCG and high Inhibin-A.
*Chorionic villus sampling (CVS)*
- **CVS** is typically performed earlier in pregnancy, between **10 and 13 weeks gestation**, meaning it is too late to perform at 16 weeks gestation.
- While it can provide a fetal karyotype for genetic diagnosis, the gestational age presented in the vignette makes this option currently inappropriate.
*Ultrasound for nuchal translucency*
- **Nuchal translucency (NT)** is part of the first-trimester screening, usually measured between **11 and 14 weeks gestation**.
- At 16 weeks gestation, measuring NT would be **outside the appropriate timeframe**, and the second-trimester quad screen has already been completed, making further screening rather than diagnosis less useful.
*Folic acid supplementation*
- **Folic acid supplementation** is crucial before and during early pregnancy to prevent neural tube defects, which would be associated with high AFP.
- The patient is already taking prenatal vitamins (which contain folic acid), and her quad screen results are not indicative of a neural tube defect but rather a chromosomal abnormality.
*Return to clinic in 4 weeks*
- The abnormal quad screen results indicate a **high risk for aneuploidy**, specifically trisomy 18, which requires immediate follow-up and definitive diagnosis.
- Delaying further assessment for 4 weeks would be clinically inappropriate and could increase patient anxiety and potentially reduce options for further management.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 8: A 31-year-old G1P0 woman at 26 weeks gestation presents to the clinic for evaluation of an abnormal glucose tolerance test. She denies any symptoms, but states that she was given 50 g of oral glucose 1 week earlier and demonstrated a subsequent venous plasma glucose level of 156 mg/dL 1 hour later. The vital signs are: blood pressure, 112/78 mm Hg; pulse, 81/min; and respiratory rate, 16/min. Physical examination is within normal limits. Which of the following is the most appropriate next step in management?
- A. Administer an oral, 3-hour 100 g glucose dose (Correct Answer)
- B. Advise the patient to follow an American Diabetic Association diet plan
- C. Repeat the 50 g oral glucose challenge
- D. Begin insulin treatment
- E. Order a fetal ultrasound examination
Diagnostic testing (amniocentesis, CVS) Explanation: ***Administer an oral, 3-hour 100 g glucose dose***
- This patient failed the initial **50 g, 1-hour glucose challenge test** (screen) because her plasma glucose was 156 mg/dL, which is above the typical threshold of 130-140 mg/dL.
- The next appropriate step for a failed screening test is to perform a **diagnostic 3-hour, 100 g oral glucose tolerance test (OGTT)** to confirm or rule out gestational diabetes.
*Advise the patient to follow an American Diabetic Association diet plan*
- While lifestyle modifications are important for managing gestational diabetes, this step is premature as the diagnosis has not yet been confirmed by the **diagnostic 3-hour OGTT**.
- Diet modification is part of the treatment for confirmed gestational diabetes, not the next diagnostic step.
*Repeat the 50 g oral glucose challenge*
- Repeating the screening test is not appropriate after a positive result; a diagnostic test is required to confirm the condition.
- The **50 g challenge** is a screening test with a high sensitivity but lower specificity, thus requiring a follow-up diagnostic test.
*Begin insulin treatment*
- **Insulin treatment** is reserved for patients officially diagnosed with gestational diabetes whose blood glucose levels cannot be controlled with diet and exercise alone.
- Prescribing insulin without a confirmed diagnosis is inappropriate and potentially harmful.
*Order a fetal ultrasound examination*
- A fetal ultrasound is used to monitor for complications of gestational diabetes like **macrosomia**, but it is not the next step in diagnosing the condition.
- While important for fetal surveillance in confirmed cases, it does not aid in the initial diagnosis of gestational diabetes itself.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 9: A 26-year-old woman presents to the women’s health clinic with a 9-week delay in menses. The patient has a history of grand mal seizures, and was recently diagnosed with acute sinusitis. She is prescribed lamotrigine and amoxicillin. The patient smokes one-half pack of cigarettes every day for 10 years, and drinks socially a few weekends every month. Her mother died of breast cancer when she was 61 years old. The vital signs are stable during the current office visit. Physical examination is grossly normal. The physician orders a urine beta-hCG that comes back positive. Abdominal ultrasound shows an embryo consistent in dates with the first day of last menstrual period. Given the history of the patient, which of the following would most likely decrease congenital malformations in the newborn?
- A. Decrease alcohol consumption
- B. Switching to cephalexin
- C. Folic acid supplementation (Correct Answer)
- D. Smoking cessation
- E. Switching to another antiepileptic medication
Diagnostic testing (amniocentesis, CVS) Explanation: ***Folic acid supplementation***
- **Folic acid** (vitamin B9) is crucial in early pregnancy for **neural tube development** and significantly reduces the risk of **neural tube defects** and other congenital malformations.
- Given the patient’s history of **lamotrigine** use, which can increase the risk of neural tube defects, folic acid supplementation is even more critical.
*Decrease alcohol consumption*
- While **alcohol cessation** is important to prevent **fetal alcohol syndrome** and other alcohol-related developmental issues, it primarily affects neurological development and facial dysmorphology rather than primarily preventing
- The effects of alcohol are typically more pronounced with **chronic heavy consumption**, and while any reduction is beneficial, it is not the most likely intervention to decrease general congenital malformations.
*Switching to cephalexin*
- **Amoxicillin** is considered **safe in pregnancy** and is a penicillin-class antibiotic, while **cephalexin** is a cephalosporin.
- Switching antibiotics from one safe drug to another without a clear medical indication (e.g., allergy, resistance) would **not decrease the risk of congenital malformations**.
*Smoking cessation*
- **Smoking cessation** is vital during pregnancy as it reduces the risk of **low birth weight**, **preterm birth**, and other complications like placental abruption.
- However, the primary link of smoking is not directly with **congenital malformations** like neural tube defects, but rather with growth restriction and adverse perinatal outcomes.
*Switching to another antiepileptic medication*
- This patient is on **lamotrigine**, which is considered one of the **safer antiepileptic drugs (AEDs)** in pregnancy, especially compared to others like **valproic acid**.
- Switching to an alternative AED might even carry a **higher risk for congenital malformations** and is generally not recommended unless lamotrigine is ineffective or contraindicated.
Diagnostic testing (amniocentesis, CVS) US Medical PG Question 10: A 31-year-old G1P0000 presents to her obstetrician for her first prenatal visit after having a positive home pregnancy test one week ago. She states that her last menstrual period was 8 weeks ago. The patient has a past medical history of type I diabetes mellitus since childhood and is on insulin. Her hemoglobin A1c two weeks ago was 13.7%. At that time, she was also found to have microalbuminuria on routine urinalysis, and her primary care provider prescribed lisinopril but the patient has not yet started taking it. The patient’s brother is autistic, but family history is otherwise unremarkable. At this visit, her temperature is 98.6°F (37.0°C), blood pressure is 124/81 mmHg, pulse is 75/min, and respirations are 14/min. Exam is unremarkable. This fetus is at increased risk for which of the following?
- A. Post-term delivery
- B. Oligohydramnios
- C. Neural tube defect (Correct Answer)
- D. Aneuploidy
- E. Neonatal hyperglycemia
Diagnostic testing (amniocentesis, CVS) Explanation: ***Neural tube defect***
- The patient's **poorly controlled type 1 diabetes mellitus** is evidenced by her **HbA1c of 13.7%**. Uncontrolled maternal hyperglycemia during organogenesis significantly increases the risk for fetal malformations, including neural tube defects due to impaired folate metabolism.
- This risk is highest when hyperglycemia occurs during the first 8 weeks of gestation, a period crucial for neural tube closure, which aligns with this patient's presentation at 8 weeks' gestation.
*Post-term delivery*
- **Uncontrolled maternal diabetes** is typically associated with **macrosomia and polyhydramnios**, which can lead to complications such as **shoulder dystocia, premature rupture of membranes (PROM)**, and often precipitates **earlier induction of labor** rather than post-term delivery.
- While exact delivery timing can vary, the direct causal link between uncontrolled diabetes and post-term delivery is not primary; rather, such pregnancies are often managed with earlier interventions.
*Oligohydramnios*
- Poorly controlled maternal diabetes, particularly type 1, is generally associated with **polyhydramnios** due to fetal polyuria caused by hyperglycemia, not oligohydramnios.
- **Oligohydramnios** can be associated with severe **placental insufficiency**, prolonged rupture of membranes, or fetal renal agenesis, none of which are directly indicated by uncontrolled maternal diabetes alone.
*Aneuploidy*
- The primary risk factor for **aneuploidy** (e.g., Down syndrome) is **advanced maternal age**, which is not present in this 31-year-old patient.
- **Maternal diabetes** itself is not a direct risk factor for aneuploidy; genetic factors related to nondisjunction are the main cause.
*Neonatal hyperglycemia*
- Maternal hyperglycemia leads to fetal hyperglycemia, causing **fetal hyperinsulinemia**. After birth, the neonate's elevated insulin levels, in the absence of maternal glucose supply, result in **neonatal hypoglycemia**, not hyperglycemia.
- **Neonatal hyperglycemia** is rare and usually associated with specific genetic defects or administration of excessive glucose postnatally, not maternal diabetes.
More Diagnostic testing (amniocentesis, CVS) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.