Cell-free DNA screening US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cell-free DNA screening. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cell-free DNA screening US Medical PG Question 1: A newlywed couple comes to your office for genetic counseling. Both potential parents are known to be carriers of the same Cystic Fibrosis (CF) mutation. What is the probability that at least one of their next three children will have CF if they are all single births?
- A. 37/64 (Correct Answer)
- B. 0
- C. 1/64
- D. 1
- E. 27/64
Cell-free DNA screening Explanation: ***37/64***
- The probability of a child having CF from two carrier parents is **1/4** (recessive inheritance), and the probability of a child not having CF is **3/4**.
- The probability that *none* of the three children will have CF is (3/4)³ = **27/64**. Therefore, the probability that *at least one* child will have CF is 1 - 27/64 = **37/64**.
*0*
- This option is incorrect because there is a **definite statistical probability** for a child to inherit CF when both parents are carriers.
- CF is an **autosomal recessive disorder**, meaning there is a 25% chance per child, not a 0% chance.
*1/64*
- This represents the probability that ***all three children*** would have CF: (1/4)³ = 1/64.
- This is an **underestimation** of the probability for at least one child to be affected, as the question asks about "at least one" not "all three."
*1*
- This would imply that it's an **absolute certainty** that at least one child will have CF, which is incorrect.
- Each child's outcome is independent, and there is always a chance (27/64) that none of the three children will have the disease.
*27/64*
- This calculation represents the probability that **none of the three children will have CF**: (3/4)³ = 27/64.
- This is the **complementary probability** to "at least one child having CF", not the actual answer to the question asked.
Cell-free DNA screening US Medical PG Question 2: A 39-year-old pregnant woman at 16 weeks gestation recently underwent a quad-screen which revealed elevated beta-hCG, elevated inhibin A, decreased alpha-fetoprotein, and decreased estradiol. An ultrasound was performed which found increased nuchal translucency. Which of the following is recommended for diagnosis?
- A. Biopsy and pathologic examination of fetus
- B. Confirmatory amniocentesis and chromosomal analysis of the fetal cells (Correct Answer)
- C. Fetus is normal, continue with pregnancy as expected
- D. Maternal karyotype
- E. Cell-free fetal DNA analysis
Cell-free DNA screening Explanation: ***Confirmatory amniocentesis and chromosomal analysis of the fetal cells***
- The combination of **quad-screen results** (elevated 𝛽-hCG, elevated inhibin A, decreased AFP, decreased estradiol) and **increased nuchal translucency** strongly suggests an aneuploidy, particularly **Down Syndrome (Trisomy 21)**.
- **Amniocentesis** is a **diagnostic procedure** that provides fetal cells for definitive chromosomal analysis (karyotyping), confirming or ruling out aneuploidy with high accuracy.
*Biopsy and pathologic examination of fetus*
- A **fetal biopsy** is generally not a standard diagnostic test for aneuploidy and carries higher risks than amniocentesis or chorionic villus sampling (CVS).
- This procedure would typically be considered for specific fetal anomalies requiring tissue diagnosis, not for confirming chromosomal disorders.
*Fetus is normal, continue with pregnancy as expected*
- The abnormal **quad-screen results** and **increased nuchal translucency** are significant indicators of potential chromosomal abnormalities, making it unlikely that the fetus is normal.
- Ignoring these findings could lead to the birth of a child with an undiagnosed genetic condition.
*Maternal karyotype*
- A **maternal karyotype** evaluates the mother's chromosomes to identify balanced translocations or other inherited chromosomal abnormalities that could increase the risk in offspring.
- While helpful for identifying a parental genetic cause, it does not directly diagnose the fetal condition; a fetal sample is still needed for that.
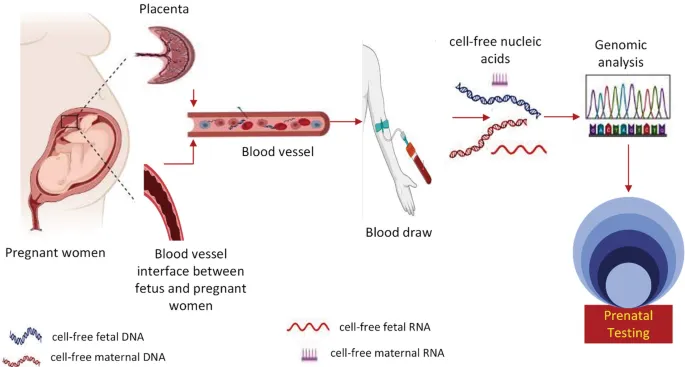
*Cell-free fetal DNA analysis*
- **Cell-free fetal DNA (cfDNA) analysis** is a **screening test** with high sensitivity and specificity for common aneuploidies, but it is not a diagnostic test.
- While it can guide further investigation, a positive cfDNA result still requires a **confirmatory diagnostic procedure** like amniocentesis or CVS before making definitive clinical decisions.
Cell-free DNA screening US Medical PG Question 3: A 36-year old pregnant woman (gravida 4, para 1) presents at week 11 of pregnancy. Currently, she has no complaints. She had an uncomplicated 1st pregnancy that ended in an uncomplicated vaginal delivery at the age of 28 years. Her male child was born healthy, with normal physical and psychological development over the years. Two of her previous pregnancies were spontaneously terminated in the 1st trimester. Her elder sister has a child born with Down syndrome. The patient denies smoking and alcohol consumption. Her blood analysis reveals the following findings:
Measured values
Beta human chorionic gonadotropin (beta-hCG) High
Pregnancy-associated plasma protein-A (PAPP-A) Low
Which of the following is the most appropriate next step in the management of this patient?
- A. Perform an ultrasound examination with nuchal translucency and crown-rump length measurement
- B. Recommend chorionic villus sampling with subsequent cell culturing and karyotyping (Correct Answer)
- C. Offer a blood test for rubella virus, cytomegalovirus, and toxoplasma IgG
- D. Recommend amniocentesis with subsequent cell culturing and karyotyping
- E. Schedule a quadruple test at the 15th week of pregnancy
Cell-free DNA screening Explanation: ***Recommend chorionic villus sampling with subsequent cell culturing and karyotyping***
- The patient's **advanced maternal age** (36 years), history of **recurrent first-trimester miscarriages**, and a **family history of Down syndrome** in her sister's child are significant risk factors for **chromosomal abnormalities**.
- The abnormal first-trimester screening results (**high beta-hCG, low PAPP-A**) are highly suggestive of **aneuploidies**, particularly **Down syndrome (Trisomy 21)**. **Chorionic villus sampling (CVS)** is the most appropriate next step for definitive diagnosis as it can be performed earlier (10-13 weeks) than amniocentesis for definitive diagnosis via karyotyping.
*Perform an ultrasound examination with nuchal translucency and crown-rump length measurement*
- While a **nuchal translucency (NT) measurement** is part of the first-trimester screening and would confirm an increased risk, it is a screening, not a diagnostic, test.
- Given the patient's strong risk factors and abnormal biochemical markers, a definitive diagnostic test is warranted rather than another screening measure.
*Offer a blood test for rubella virus, cytomegalovirus, and toxoplasma IgG*
- This patient has a history of recurrent miscarriages and a family history suggestive of chromosomal abnormalities, along with abnormal first-trimester biochemical markers.
- While infections can cause miscarriage, the clinical picture strongly points towards a **chromosomal etiology**, making infection screening less urgent as a primary next step.
*Recommend amniocentesis with subsequent cell culturing and karyotyping*
- **Amniocentesis** is a diagnostic test for chromosomal abnormalities but is typically performed later in pregnancy, usually between **15 and 20 weeks**.
- Given the patient is at 11 weeks, **CVS** is the more appropriate and earlier diagnostic option for definitive diagnosis of potential aneuploidies.
*Schedule a quadruple test at the 15th week of pregnancy*
- The **quadruple test** is a second-trimester screening test and would provide more risk assessment rather than a definitive diagnosis.
- The patient already has strong indications for a chromosomal abnormality based on age, history, and first-trimester screening, necessitating an **earlier definitive diagnostic test**.
Cell-free DNA screening US Medical PG Question 4: A 35-year-old woman gravida 2, para 1, comes to the physician for her first prenatal visit. Pregnancy and delivery of her first child were uncomplicated. She is not sure about the date of her last menstrual period. Pelvic examination shows a uterus consistent in size with a 10-week gestation. An ultrasound examination confirms the gestational age and shows one fetus with no indication of multiple gestations. During counseling on pregnancy risks and possible screening and diagnostic tests, the patient states she would like to undergo screening for Down syndrome. She would prefer immediate and secure screening with a low risk to herself and the fetus. Which of the following is the most appropriate next step in management at this time?
- A. Nuchal translucency, pregnancy-associated plasma protein-A, human chorionic gonadotropin
- B. Maternal serum α-fetoprotein, human chorionic gonadotropin, unconjugated estriol, and inhibin A
- C. Chorionic villus sampling
- D. Amniocentesis
- E. Cell-free fetal DNA testing (Correct Answer)
Cell-free DNA screening Explanation: ***Cell-free fetal DNA testing***
- This is the most appropriate choice given the patient's desire for **immediate and secure screening with low risk** because it is a **non-invasive prenatal screening (NIPS)** method offering high sensitivity and specificity for Down syndrome, particularly in higher-risk pregnancies.
- It involves a simple maternal blood draw and can be performed as early as **10 weeks of gestation**, perfectly aligning with the patient's current gestational age and desire for early screening.
*Nuchal translucency, pregnancy-associated plasma protein-A, human chorionic gonadotropin*
- This combination represents the **first-trimester combined screen**, which is typically performed between 11 and 14 weeks of gestation. While suitable for early screening, **cell-free DNA testing offers higher detection rates and lower false-positive rates** for Down syndrome.
- The patient specifically asked for the most **secure and least risky** screening, and NIPS outperforms the combined screen in terms of diagnostic accuracy for aneuploidies.
*Maternal serum α-fetoprotein, human chorionic gonadotropin, unconjugated estriol, and inhibin A*
- This refers to the **quad screen**, which is typically performed in the **second trimester (15-20 weeks)**, making it too late for the patient's desire for immediate screening at 10 weeks gestational age.
- While a widely used screening tool, the quad screen has a **lower detection rate** for Down syndrome compared to cell-free DNA testing.
*Chorionic villus sampling*
- **Chorionic villus sampling (CVS)** is a **diagnostic, invasive procedure** that carries a small risk of miscarriage (approximately 1 in 455 or 0.22%) and is not a screening test.
- Although it can be performed earlier (typically between 10 and 13 weeks), the patient specifically requested a **low-risk screening** option, which CVS is not.
*Amniocentesis*
- **Amniocentesis** is also an **invasive diagnostic procedure** with a risk of miscarriage (approximately 1 in 900 or 0.11%) and is typically performed in the **second trimester (15-20 weeks)**.
- This option is unsuitable because the patient is at 10 weeks gestation and desires **immediate and low-risk screening**, not a diagnostic procedure with procedural risks a few weeks later.
Cell-free DNA screening US Medical PG Question 5: A 34-year-old gravida 2 para 1 woman at 16 weeks gestation presents for prenatal care. Her prenatal course has been uncomplicated. She takes no medications besides her prenatal vitamin which she takes every day, and she has been compliant with routine prenatal care. She has a 7-year-old daughter who is healthy. The results of her recent quadruple screen are listed below:
AFP: Low
hCG: Low
Estriol: Low
Inhibin-A: Normal
Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Chorionic villus sampling
- B. Amniocentesis (Correct Answer)
- C. Ultrasound for nuchal translucency
- D. Folic acid supplementation
- E. Return to clinic in 4 weeks
Cell-free DNA screening Explanation: ***Amniocentesis***
- The presented quad screen results (low AFP, low hCG, low estriol, normal Inhibin-A) are highly suggestive of **trisomy 18 (Edwards syndrome)**. Amniocentesis is a **definitive diagnostic test** that can confirm aneuploidy by providing a fetal karyotype.
- While typically performed between **15 and 20 weeks gestation**, it can differentiate between trisomy 18 and trisomy 21 (Down syndrome), which usually presents with high hCG and high Inhibin-A.
*Chorionic villus sampling (CVS)*
- **CVS** is typically performed earlier in pregnancy, between **10 and 13 weeks gestation**, meaning it is too late to perform at 16 weeks gestation.
- While it can provide a fetal karyotype for genetic diagnosis, the gestational age presented in the vignette makes this option currently inappropriate.
*Ultrasound for nuchal translucency*
- **Nuchal translucency (NT)** is part of the first-trimester screening, usually measured between **11 and 14 weeks gestation**.
- At 16 weeks gestation, measuring NT would be **outside the appropriate timeframe**, and the second-trimester quad screen has already been completed, making further screening rather than diagnosis less useful.
*Folic acid supplementation*
- **Folic acid supplementation** is crucial before and during early pregnancy to prevent neural tube defects, which would be associated with high AFP.
- The patient is already taking prenatal vitamins (which contain folic acid), and her quad screen results are not indicative of a neural tube defect but rather a chromosomal abnormality.
*Return to clinic in 4 weeks*
- The abnormal quad screen results indicate a **high risk for aneuploidy**, specifically trisomy 18, which requires immediate follow-up and definitive diagnosis.
- Delaying further assessment for 4 weeks would be clinically inappropriate and could increase patient anxiety and potentially reduce options for further management.
Cell-free DNA screening US Medical PG Question 6: A cell biologist is studying the activity of a novel chemotherapeutic agent against a cancer cell line. After incubation with the agent and cell detachment from the tissue culture plate, the DNA is harvested from the cells and run on a gel. Of note, there are large bands at every multiple of 180 base pairs on the gel. Which of the following explains the pathophysiology of this finding?
- A. Protein denaturation
- B. Release of lysosomal enzymes
- C. Cellular swelling
- D. ATP depletion
- E. Caspase activation (Correct Answer)
Cell-free DNA screening Explanation: ***Caspase activation***
- The presence of large bands at multiples of **180 base pairs** on a gel indicates a characteristic ladder-like fragmentation pattern of DNA. This fragmentation is a hallmark of **apoptosis**, a form of programmed cell death.
- **Caspase activation**, particularly that of **endonucleases** like caspase-activated DNase (CAD), is responsible for cleaving DNA between nucleosomes, leading to these distinct 180-bp fragments.
*Protein denaturation*
- **Protein denaturation** involves the unfolding of proteins due to stressors but does not directly cause DNA fragmentation into specific band sizes.
- While it can be a part of apoptosis or necrosis, it's not the primary mechanism explaining the observed **DNA laddering**.
*Release of lysosomal enzymes*
- **Lysosomal enzymes** are typically released during **necrosis** or severe cellular injury, leading to widespread, indiscriminate degradation of cellular components, including DNA.
- This degradation would result in a **smear** rather than discrete bands on a gel, as the DNA would be randomly fragmented.
*Cellular swelling*
- **Cellular swelling** is an early, reversible sign of cell injury often associated with **necrosis** or hydropic change due to ion pump dysfunction.
- It does not directly lead to **DNA fragmentation** or the specific laddering pattern seen in apoptosis.
*ATP depletion*
- **ATP depletion** is a critical event in cell injury, often leading to activation of anaerobic glycolysis, failure of ion pumps, and ultimately cell death.
- While **ATP depletion** can contribute to necrosis, apoptosis often requires ATP for the energy-dependent cascade of caspase activation and DNA fragmentation.
Cell-free DNA screening US Medical PG Question 7: A 39-year-old woman presents to her gynecologist for a routine visit. She has no complaints during this visit. She had an abnormal pap test 6 years ago that showed atypical squamous cells of undetermined significance. The sample was negative for human papillomavirus. On her follow-up Pap test 3 years later, there was no abnormality. The latest pap test results show atypical glandular cells with reactive changes in the cervical epithelium. The gynecologist decides to perform a colposcopy, and some changes are noted in this study of the cervical epithelium. The biopsy shows dysplastic changes in the epithelial cells. Which of the following is the next best step in the management of this patient?
- A. Follow-up pap smear in one year
- B. Follow-up pap smear in 3 years
- C. Cold knife conization (Correct Answer)
- D. Repeat colposcopy in 6 months
- E. Loop electrosurgical excision procedure
Cell-free DNA screening Explanation: ***Cold knife conization***
- This patient presents with **atypical glandular cells** and **dysplastic changes** on biopsy, which can indicate **adenocarcinoma in situ** or **invasive adenocarcinoma**. **Cold knife conization** allows for a complete excision of the transformation zone, including the endocervical canal, which is essential for accurate diagnosis and treatment of glandular lesions.
- This procedure provides a high-quality, intact specimen for thorough histopathological examination, enabling the pathologist to determine the extent and depth of the lesion, which guides further management.
*Follow-up pap smear in one year*
- This option is inappropriate given the presence of **dysplastic changes** on biopsy following atypical glandular cells; these findings indicate a high risk that requires immediate definitive action, not merely observation.
- Delaying further diagnostic or therapeutic interventions for a year could allow a potentially significant lesion, especially a glandular one, to progress.
*Follow-up pap smear in 3 years*
- This is not an appropriate next step due to the finding of **atypical glandular cells** and **dysplastic changes** on biopsy, which necessitate prompt and comprehensive evaluation and management.
- Longer follow-up intervals are reserved for women with normal screens and no high-risk findings, not for those with confirmed dysplasia.
*Repeat colposcopy in 6 months*
- A repeat colposcopy without excisional biopsy would be insufficient because the **dysplastic changes** on biopsy already confirm the presence of a lesion that requires definitive management.
- **Atypical glandular cells** and dysplasia frequently originate higher in the endocervical canal, beyond the view of colposcopy, necessitating an excisional procedure like conization for complete evaluation.
*Loop electrosurgical excision procedure*
- A **LEEP** might be considered for squamous lesions, but for **atypical glandular cells** and suspected glandular dysplasia, **cold knife conization** is generally preferred.
- While LEEP can be used, it may not provide as clear or deep margins as cold knife conization, potentially leading to incomplete excision or difficulty in histological assessment, especially if the lesion extends high into the endocervical canal.
Cell-free DNA screening US Medical PG Question 8: An investigator is studying the biology of human sperm cells. She isolates spermatogonia obtained on a testicular biopsy from a group of healthy male volunteers. She finds that the DNA of spermatogonia obtained from these men show a large number of TTAGGG sequence repeats. This finding can best be explained by increased activity of an enzyme with which of the following functions?
- A. Ligation of Okazaki fragments
- B. Proofreading of synthesized daughter strands
- C. RNA-dependent synthesis of DNA (Correct Answer)
- D. Production of short RNA sequences
- E. Hemimethylation of DNA strand
Cell-free DNA screening Explanation: ***RNA-dependent synthesis of DNA***
- The TTAGGG sequence repeats are **telomeric sequences**, which are maintained by **telomerase**, an enzyme that synthesizes DNA from an RNA template.
- **Spermatogonia** are germline stem cells that express high levels of telomerase to maintain telomere length across generations.
*Ligation of Okazaki fragments*
- This function is carried out by **DNA ligase**, which joins discontinuous DNA fragments during replication on the lagging strand.
- This process is essential for general DNA replication but is not specific to the formation or maintenance of telomeric repeats.
*Proofreading of synthesized daughter strands*
- This is a function of **DNA polymerase exonuclease activity**, which corrects errors during DNA replication.
- While important for genetic fidelity, it does not explain the presence or increase of specific TTAGGG repeat sequences at telomeres.
*Production of short RNA sequences*
- This function is performed by **primase**, which synthesizes RNA primers necessary to initiate DNA synthesis during replication.
- These RNA primers are later removed and replaced with DNA, and this process is not directly responsible for generating or extending telomeric repeats.
*Hemimethylation of DNA strand*
- Hemimethylation occurs during **DNA replication** when new DNA strands are unmethylated while parental strands are methylated.
- This phenomenon is involved in DNA repair and gene regulation but is unrelated to the synthesis or regulation of telomeric sequences.
Cell-free DNA screening US Medical PG Question 9: A 22-year-old Caucasian G1 presents to her physician at 29 weeks gestation for a checkup. The medical history is unremarkable and the current pregnancy has been uncomplicated. Her weight is 81 kg (178.6 lb) and the height is 169 cm (5 ft 6 in). She has gained 13 kg (28.6 lb) during the pregnancy. She has no abnormalities on physical examination. Which of the following screening tests should be obtained ?
- A. Measurement of HbA1c
- B. Fasting glucose level
- C. Fasting oral glucose test with 50 g of glucose
- D. Non-fasting oral glucose load test with 75 g of glucose
- E. Non-fasting oral glucose challenge test with 50 g of glucose (Correct Answer)
Cell-free DNA screening Explanation: ***Non-fasting oral glucose challenge test with 50 g of glucose***
- This patient is at 29 weeks gestation, which is the recommended time for **gestational diabetes mellitus (GDM) screening** between **24 and 28 weeks**.
- A 50g non-fasting glucose challenge test is the **initial screening step**, followed by a diagnostic 100g 3-hour oral glucose tolerance test if the screen is abnormal.
*Measurement of HbA1c*
- **HbA1c** is used to diagnose pre-existing diabetes or to monitor long-term glycemic control, but it is **not the primary screening test for GDM** due to its limitations in reflecting acute glucose fluctuations in pregnancy.
- While it can be useful in some cases, it's not the standard initial screening tool for GDM.
*Fasting glucose level*
- A **fasting glucose level** is part of the diagnostic oral glucose tolerance test (OGTT) but is **not typically used as a standalone screening test** for GDM.
- It would require the patient to fast, which is not part of the initial screening challenge.
*Fasting oral glucose test with 50 g of glucose*
- The initial glucose challenge test is **non-fasting** and involves 50g of glucose.
- A **fasting** state is reserved for the **diagnostic 100g or 75g OGTT**, not the initial screening.
*Non-fasting oral glucose load test with 75 g of glucose*
- A **75g oral glucose tolerance test (OGTT)** is a diagnostic test for GDM, **not an initial screening test**.
- It is used when the 50g glucose challenge test is abnormal or in certain high-risk populations as the sole diagnostic step.
Cell-free DNA screening US Medical PG Question 10: A 37-year-old primigravid woman comes to the physician at 13 weeks' gestation for a prenatal visit. She feels well. Her only medication is folic acid. Vital signs are within normal limits. Pelvic examination shows a uterus consistent in size with a 13-week gestation. Ultrasonography shows a nuchal translucency above the 99th percentile. Maternal serum pregnancy-associated plasma protein A is decreased and human chorionic gonadotropin concentrations are elevated to 2 times the median level. Which of the following is most likely to confirm the diagnosis?
- A. Chorionic villus sampling (Correct Answer)
- B. Cell-free DNA testing
- C. Triple screening test
- D. Amniocentesis
- E. Quadruple marker test
Cell-free DNA screening Explanation: ***Chorionic villus sampling***
- This procedure can be performed between **10 to 13 weeks of gestation** to obtain fetal cells for genetic analysis, which is within the patient's gestational age.
- It provides a definitive diagnosis of **chromosomal abnormalities** by directly sampling placental tissue, which shares the same genetic material as the fetus.
*Cell-free DNA testing*
- While it has high sensitivity and specificity for various **aneuploidies**, it is a **screening test**, not a diagnostic one.
- An abnormal result from cell-free DNA testing still requires **confirmatory diagnostic testing** such as CVS or amniocentesis.
*Triple screening test*
- This test is typically performed between **15 and 20 weeks of gestation**, which is too late to confirm the findings presented at 13 weeks gestation.
- It measures **AFP, hCG, and unconjugated estriol**, and an abnormal result would indicate a need for further diagnostic testing.
*Amniocentesis*
- This procedure is generally performed later in pregnancy, typically between **15 and 20 weeks gestation**, so it would require waiting several more weeks.
- While it provides definitive genetic results, **chorionic villus sampling is preferred at 13 weeks** due to earlier diagnostic potential.
*Quadruple marker test*
- This test is also performed between **15 and 20 weeks of gestation** and measures **AFP, hCG, unconjugated estriol, and inhibin A**.
- It is a **screening test**, similar to the triple screen, and does not provide a definitive diagnosis, requiring further confirmatory testing if abnormal.
More Cell-free DNA screening US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.