Medication safety in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Medication safety in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Medication safety in pregnancy US Medical PG Question 1: A 25-year-old G1P0 woman at an estimated gestational age of 9 weeks presents for her first prenatal visit following a positive home pregnancy test. She says she missed 2 periods but assumed it was due to stress at work. She has decided to continue with the pregnancy. Her past medical history is significant for migraine headaches, seizures, and asthma. She takes multiple medications for her condition. Physical examination is unremarkable. An ultrasound confirms a 9-week-old intrauterine pregnancy. Which of the following medications poses the greatest risk to the fetus?
- A. Valproic acid (Correct Answer)
- B. Budesonide
- C. Acetaminophen
- D. Sumatriptan
- E. Albuterol
Medication safety in pregnancy Explanation: ***Valproic acid***
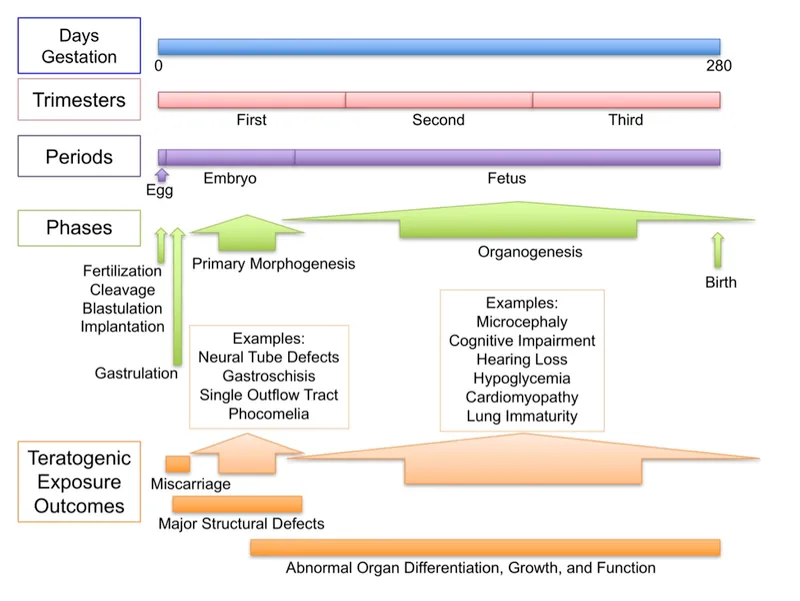
- **Valproic acid** is a known **teratogen** strongly associated with a high incidence of **neural tube defects** (e.g., spina bifida, anencephaly) when used during the first trimester of pregnancy.
- It can also lead to other malformations, including cardiac defects and facial dysmorphism, as part of **fetal valproate syndrome**.
*Budesonide*
- **Budesonide** is an inhaled corticosteroid commonly used for asthma, considered a relatively **safe medication** during pregnancy (FDA pregnancy category B).
- Studies have shown no increased risk of major congenital malformations with its use.
*Acetaminophen*
- **Acetaminophen** is a widely used analgesic and antipyretic considered **safe** for use throughout pregnancy at recommended doses.
- There is no strong evidence linking acetaminophen to an increased risk of birth defects.
*Sumatriptan*
- **Sumatriptan** is a serotonin receptor agonist used for migraine headaches. It is generally considered to be of **low risk** during pregnancy (FDA pregnancy category C).
- While some studies have suggested a minimal risk of certain birth defects, overall data supports its use when necessary.
*Albuterol*
- **Albuterol** is a short-acting beta-agonist used to treat asthma symptoms and is considered **safe** for use during pregnancy (FDA pregnancy category C).
- There is no evidence of teratogenicity, and the benefits of controlling asthma outweigh the potential risks.
Medication safety in pregnancy US Medical PG Question 2: A 30-year-old woman, gravida 2, para 1, comes to the physician because she had a positive pregnancy test at home. During the last two weeks, she has had nausea and two episodes of non-bloody vomiting. She also reports increased urinary frequency. Her pregnancy and delivery of her first child were uncomplicated. Last year, she had two episodes of grand-mal seizure. She is sexually active with her husband and they use condoms inconsistently. She does not smoke or drink alcohol. She does not use illicit drugs. Current medications include valproic acid and a multivitamin. Her vital signs are within normal limits. Physical examination shows no abnormalities. A urine pregnancy test is positive. The child is at increased risk for requiring which of the following interventions?
- A. Lower spinal surgery (Correct Answer)
- B. Cochlear implantation
- C. Kidney transplantation
- D. Dental treatment
- E. Respiratory support
Medication safety in pregnancy Explanation: ***Lower spinal surgery***
- The patient is taking **valproic acid** which is associated with an increased risk of **neural tube defects** (NTDs), such as spina bifida, in the fetus.
- Infants with **spina bifida** often require surgical intervention to close the spinal defect and manage associated neurological complications such as hydrocephalus, which may consequently require a shunt.
*Cochlear implantation*
- **Cochlear implantation** is a treatment for severe hearing loss, and there is no direct link between maternal valproic acid use and an increased risk of congenital hearing impairment requiring this intervention.
- While some congenital syndromes can include hearing loss, it is not a hallmark teratogenic effect of **valproic acid**.
*Kidney transplantation*
- There is no strong evidence to suggest that maternal use of **valproic acid** significantly increases the risk of fetal renal malformations or end-stage renal disease requiring **kidney transplantation**.
- Issues requiring kidney transplantation are not a common outcome of valproic acid exposure.
*Dental treatment*
- Routine **dental treatment** is common in children, but there is no specific increased risk of severe dental anomalies or conditions requiring extensive early intervention directly attributable to maternal valproic acid use.
- While some medications can cause dental issues, **valproic acid** is not specifically noted for this teratogenic effect.
*Respiratory support*
- Although some birth defects can indirectly affect respiratory function, there is no direct and significant link between maternal **valproic acid** use and primary pulmonary hypoplasia or other severe respiratory conditions requiring **long-term respiratory support** in the newborn.
- **Neural tube defects** are the primary concern, and while they can have systemic effects, primary respiratory failure is not a direct result.
Medication safety in pregnancy US Medical PG Question 3: A 33-year-old Hispanic woman who recently immigrated to the United States with her newborn daughter is presenting to a free clinic for a wellness checkup for her baby. As part of screening for those immigrating or seeking refuge in the United States, she and her child are both evaluated for tuberculosis. The child’s purified protein derivative (PPD) test and chest radiograph are negative, and although the mother’s chest radiograph is also negative, her PPD is positive. She states that she is currently asymptomatic and has no known history of tuberculosis (TB). The mother’s vital signs include: blood pressure 124/76 mm Hg, heart rate 74/min, and respiratory rate 14/min. She is advised to begin treatment with isoniazid, supplemented with pyridoxine for the next 9 months. She asks about the potential for harm to the child if she begins this course of treatment since she is breastfeeding. Which of the following is the most appropriate response to this patient’s concerns?
- A. “You should not breastfeed your baby for the next 9 months because isoniazid in breast milk can damage your child’s liver.”
- B. “You should not breastfeed your baby for the next 9 months because pyridoxine in breast milk can damage your child’s liver.”
- C. “You may breastfeed your baby because you are asymptomatic and because neither isoniazid nor pyridoxine will harm your child.” (Correct Answer)
- D. “You should not breastfeed your baby because she is at greater risk for infection with TB than for adverse side effects of your treatment regimen.”
- E. “You may breastfeed your baby because pyridoxine will prevent isoniazid from causing peripheral neuropathy.”
Medication safety in pregnancy Explanation: ***“You may breastfeed your baby because you are asymptomatic and because neither isoniazid nor pyridoxine will harm your child.”***
- The **benefits of breastfeeding** (providing immunity, nutrition, and bonding) generally outweigh the minimal risks associated with isoniazid and pyridoxine secretion into breast milk.
- Since the mother is **asymptomatic** and her chest X-ray is negative, she has **latent tuberculosis infection (LTBI)**, making transmission to the infant highly unlikely through casual contact, and therefore breastfeeding is safe.
*“You should not breastfeed your baby for the next 9 months because isoniazid in breast milk can damage your child’s liver.”*
- While **isoniazid (INH)** can cause drug-induced hepatitis in adults, the amount excreted in breast milk is typically very low and **not considered harmful** to the infant's liver.
- The American Academy of Pediatrics states that INH is **compatible with breastfeeding**.
*“You should not breastfeed your baby for the next 9 months because pyridoxine in breast milk can damage your child’s liver.”*
- **Pyridoxine (vitamin B6)** is a vitamin and is added to the treatment regimen to **prevent INH-induced peripheral neuropathy**; it is not harmful to the infant's liver and is naturally present in breast milk.
- There is **no evidence** that pyridoxine in breast milk can cause liver damage in an infant.
*“You should not breastfeed your baby because she is at greater risk for infection with TB than for adverse side effects of your treatment regimen.”*
- The mother has **latent TB**, not active TB, meaning she is **not contagious** and cannot spread the infection to her infant.
- Breastfeeding does not increase the risk of TB transmission from a mother with LTBI, and preventing transmission is best achieved through treating the mother's LTBI.
*“You may breastfeed your baby because pyridoxine will prevent isoniazid from causing peripheral neuropathy.”*
- This statement accurately describes a function of **pyridoxine** for the mother (preventing **peripheral neuropathy**), but it does not address the infant's safety concerning breast milk intake.
- While correct that pyridoxine prevents this side effect in the mother, it's not the primary reason why breastfeeding is safe for the infant.
Medication safety in pregnancy US Medical PG Question 4: A 32-year-old primigravid woman with a history of seizures comes to the physician because she had a positive pregnancy test at home. Medications include valproic acid and a multivitamin. Physical examination shows no abnormalities. A urine pregnancy test is positive. Her baby is at increased risk for requiring which of the following interventions?
- A. Lower spinal surgery (Correct Answer)
- B. Kidney transplantation
- C. Arm surgery
- D. Cochlear implantation
- E. Respiratory support
Medication safety in pregnancy Explanation: ***Lower spinal surgery***
- Maternal use of **valproic acid** during pregnancy significantly increases the risk of neural tube defects, particularly **spina bifida**, which often requires surgical correction of the lower spine in affected infants.
- **Spina bifida** results from the incomplete closure of the neural tube, leading to exposed spinal cord or meninges, and frequently necessitates surgical intervention to prevent further neurological damage and infection.
*Kidney transplantation*
- While some fetal anomalies can involve the kidneys, **valproic acid** exposure is not primarily associated with renal agenesis or severe kidney malformations requiring transplantation.
- Birth defects affecting the kidneys are more commonly linked to genetic syndromes or other teratogens, not specifically valproic acid.
*Arm surgery*
- **Valproic acid** has been associated with limb defects, but these are typically minor and do not usually directly necessitate extensive arm surgery.
- **Phocomelia** (shortened or absent limbs) is more typically associated with **thalidomide** exposure, not valproic acid.
*Cochlear implantation*
- Although **valproic acid** exposure has been occasionally linked to some congenital anomalies, it is not a primary risk factor for **severe hearing loss** requiring cochlear implantation.
- Hearing loss requiring such intervention is more often due to genetic factors, congenital infections, or other specific teratogens.
*Respiratory support*
- While a variety of congenital conditions can lead to respiratory compromise, **valproic acid** exposure does not specifically cause severe pulmonary hypoplasia or other defects that commonly necessitate prolonged or intense neonatal respiratory support.
- Respiratory distress in neonates is often related to prematurity, meconium aspiration, or other direct pulmonary issues.
Medication safety in pregnancy US Medical PG Question 5: A 25-year-old G1P1 with a history of diabetes and epilepsy gives birth to a female infant at 32 weeks gestation. The mother had no prenatal care and took no prenatal vitamins. The child's temperature is 98.6°F (37°C), blood pressure is 100/70 mmHg, pulse is 130/min, and respirations are 25/min. On physical examination in the delivery room, the child's skin is pink throughout and she cries on stimulation. All four extremities are moving spontaneously. A tuft of hair is found overlying the infant's lumbosacral region. Which of the following medications was this patient most likely taking during her pregnancy?
- A. Valproic acid (Correct Answer)
- B. Warfarin
- C. Gentamicin
- D. Lithium
- E. Ethosuximide
Medication safety in pregnancy Explanation: ***Valproic acid***
- The presence of a **tuft of hair over the lumbosacral region** strongly suggests an underlying **neural tube defect**, such as spina bifida.
- **Valproic acid** is an antiepileptic drug known for its significant association with an increased risk of neural tube defects when taken during pregnancy, especially in the first trimester.
*Warfarin*
- **Warfarin** is a known teratogen associated with **fetal warfarin syndrome**, characterized by bone abnormalities (e.g., nasal hypoplasia, stippled epiphyses), not primarily neural tube defects.
- It works as a **vitamin K antagonist** and causes bleeding if taken during pregnancy.
*Gentamicin*
- **Gentamicin** is an aminoglycoside antibiotic primarily associated with **ototoxicity** (hearing loss) and **nephrotoxicity** in the fetus.
- It is not known to cause neural tube defects.
*Lithium*
- **Lithium** is a mood stabilizer linked to **Ebstein's anomaly**, a congenital heart defect affecting the tricuspid valve, when taken during pregnancy.
- It is not associated with neural tube defects.
*Ethosuximide*
- **Ethosuximide** is an antiepileptic drug primarily used for absence seizures.
- While all antiepileptic drugs carry some teratogenic risk, ethosuximide has a lower risk of neural tube defects compared to valproic acid.
Medication safety in pregnancy US Medical PG Question 6: A 3670-g (8 lb 1 oz) male newborn is delivered to a 26-year-old primigravid woman. She received adequate prenatal care and labor was uncomplicated. She has chronic hepatitis B infection and gastroesophageal reflux disease. Her only medication is ranitidine. She admits to smoking cannabis and one half-pack of cigarettes daily. She drinks two beers on the weekend. The mother is apprehensive about taking care of her baby and requests for some information regarding breastfeeding. Which of the following is a contraindication to breastfeeding?
- A. Cannabis use (Correct Answer)
- B. Ranitidine use
- C. Hepatitis B infection
- D. Smoking
- E. Seropositive for cytomegalovirus
Medication safety in pregnancy Explanation: ***Cannabis use***
- **Cannabis** and its active compounds, particularly **tetrahydrocannabinol (THC)**, are secreted into breast milk and can accumulate in breastfed infants' adipose tissue and brain.
- Exposure via breast milk can lead to potential neurodevelopmental effects, sedation, and impaired motor development in the infant, making it a contraindication to breastfeeding.
*Ranitidine use*
- **Ranitidine** (now largely replaced by famotidine) is generally considered safe during breastfeeding because only very small amounts are transferred into breast milk and are unlikely to cause adverse effects in the infant.
- The benefits of breastfeeding typically outweigh the minimal risks associated with commonly used medications like ranitidine for maternal conditions.
*Hepatitis B infection*
- **Maternal hepatitis B infection** is not a contraindication to breastfeeding, especially if the infant receives **hepatitis B vaccine** and **hepatitis B immunoglobulin (HBIG)** at birth.
- These interventions effectively protect the infant from acquiring the virus, and the benefits of breastfeeding for nutrition and immunity are significant.
*Smoking*
- While **smoking** by the mother is harmful and linked to various health issues in the infant, it is generally considered a strong caution rather than an absolute contraindication to breastfeeding.
- Mothers are encouraged to quit or reduce smoking, and to smoke away from the infant and breastfeed after a longer interval, but the immunological and nutritional benefits of breast milk still often outweigh the risks in mild to moderate smoking.
*Seropositive for cytomegalovirus*
- **Cytomegalovirus (CMV)** is excreted in breast milk by seropositive mothers, but for **healthy, term infants**, breastfeeding is generally considered safe and beneficial despite the presence of CMV antibodies.
- In contrast, for **premature or immunocompromised infants**, there might be a theoretical risk, and pasteurization of breast milk or temporary cessation might be considered, but it's not an absolute contraindication for a full-term, healthy baby.
Medication safety in pregnancy US Medical PG Question 7: A 32-year-old G2P0A1 woman presents at 36 weeks of gestation for the first time during her pregnancy. The patient has no complaints, currently. However, her past medical history reveals seizure disorder, which is under control with valproic acid and lithium. She has not seen her neurologist during the past 2 years, in the absence of any complaints. She also reports a previous history of elective abortion. The physical examination is insignificant. Her blood pressure is 130/75 mm Hg and pulse is 80/min. The patient is scheduled to undergo regular laboratory tests and abdominal ultrasound. Given her past medical history, which of the following conditions is her fetus most likely going to develop?
- A. Neural tube defects (NTDs) (Correct Answer)
- B. Intrauterine growth restriction
- C. Iron deficiency anemia
- D. Trisomy 21
- E. Limb anomalies
Medication safety in pregnancy Explanation: **Neural tube defects (NTDs)**
* The use of **valproic acid** during pregnancy is significantly associated with an increased risk of **neural tube defects (NTDs)**, such as spina bifida and anencephaly, in the fetus.
* Valproic acid interferes with **folate metabolism**, which is crucial for proper neural tube closure during early fetal development.
*Intrauterine growth restriction*
* While some medications and maternal conditions can cause **intrauterine growth restriction (IUGR)**, valproic acid and lithium are **not primary causes** of IUGR.
* Other factors, such as **placental insufficiency**, severe maternal hypertension, or infections, are more commonly associated with IUGR.
*Iron deficiency anemia*
* **Iron deficiency anemia** is a common maternal condition in pregnancy, but it is **not a direct fetal outcome** of maternal valproic acid or lithium use.
* Fetal anemia might occur due to other causes like **Rh incompatibility** or parvovirus infection.
*Trisomy 21*
* **Trisomy 21 (Down syndrome)** is a **chromosomal anomaly** caused by the presence of an extra copy of chromosome 21.
* It is not related to maternal medication use like valproic acid or lithium; its incidence is primarily correlated with **advanced maternal age**.
*Limb anomalies*
* Although several teratogenic medications can cause **limb anomalies**, **valproic acid** is more strongly linked to **neural tube defects** and certain **cardiac anomalies**.
* **Thalidomide**, for example, is notoriously associated with severe limb malformations.
Medication safety in pregnancy US Medical PG Question 8: A 44-year-old woman with high blood pressure and diabetes presents to the outpatient clinic and informs you that she is trying to get pregnant. Her current medications include lisinopril, metformin, and sitagliptin. Her blood pressure is 136/92 mm Hg and heart rate is 79/min. Her physical examination is unremarkable. What should you do regarding her medication for high blood pressure?
- A. Discontinue lisinopril and initiate aliskiren
- B. Discontinue lisinopril and initiate labetalol (Correct Answer)
- C. Continue her current regimen
- D. Continue her current regimen and add a beta-blocker for increased control
- E. Discontinue lisinopril and initiate candesartan
Medication safety in pregnancy Explanation: ***Discontinue lisinopril and initiate labetalol***
- **Lisinopril**, an ACE inhibitor, is **teratogenic** and is contraindicated in pregnancy due to the risk of fetal renal dysfunction, oligohydramnios, and neonatal death.
- **Labetalol** is a **beta-blocker** commonly used in pregnancy for hypertension as it is considered safe and effective in this population.
*Discontinue lisinopril and initiate aliskiren*
- **Aliskiren**, a direct renin inhibitor, is also **teratogenic** and contraindicated in pregnancy due to similar risks as ACE inhibitors and ARBs.
- Replacing one teratogenic drug with another does not solve the primary concern of fetal safety.
*Continue her current regimen*
- **Continuing lisinopril** would expose the fetus to significant risks, as it is a known teratogen.
- The patient is actively trying to conceive, making it imperative to switch medications immediately.
*Continue her current regimen and add a beta-blocker for increased control*
- Adding a beta-blocker while continuing lisinopril is still inappropriate because **lisinopril itself is harmful during pregnancy**.
- The primary goal is to **discontinue teratogenic medications**, not simply to improve blood pressure control with an additional drug.
*Discontinue lisinopril and initiate candesartan*
- **Candesartan**, an **angiotensin receptor blocker (ARB)**, shares the same **teratogenic risks** as ACE inhibitors and is contraindicated in pregnancy.
- Replacing an ACE inhibitor with an ARB provides no benefit in terms of fetal safety.
Medication safety in pregnancy US Medical PG Question 9: A 30-year-old female with a history of epilepsy becomes pregnant. Her epilepsy has been well controlled by taking a medication that inhibits GABA transaminase and blocks voltage-gated sodium and calcium channels. Her obstetrician informs her that her epilepsy medication has been shown to have teratogenic effects. Of the following, which teratogenic effect is this woman's medication most likely to cause?
- A. Limb defects
- B. Neural tube defect (Correct Answer)
- C. Renal damage
- D. Ebstein's anomaly
- E. Discolored teeth
Medication safety in pregnancy Explanation: ***Neural tube defect***
- The medication described, which **inhibits GABA transaminase** and has multiple mechanisms including effects on voltage-gated channels, is **valproic acid** (valproate).
- **Valproic acid** is the antiepileptic drug with the **highest risk of neural tube defects** (e.g., spina bifida), with an incidence of approximately 1-2% when taken during pregnancy.
- This teratogenic effect occurs primarily during the first trimester and is believed to be due to interference with **folate metabolism** and **histone deacetylase inhibition**, which are crucial for proper neural tube closure.
- Folic acid supplementation is recommended for women of childbearing age taking valproate.
*Limb defects*
- **Limb defects** (e.g., phocomelia, limb reduction defects) are classically associated with **thalidomide** exposure during early pregnancy.
- While **phenytoin** (fetal hydantoin syndrome) can cause limb abnormalities including hypoplastic nails and distal phalanges, this is not the primary teratogenic concern with valproic acid.
*Renal damage*
- **Fetal renal damage** can be caused by medications such as **ACE inhibitors**, **ARBs**, and **NSAIDs** when taken during pregnancy.
- This is not a characteristic teratogenic effect of valproic acid or other antiepileptic medications.
*Ebstein's anomaly*
- **Ebstein's anomaly**, a congenital heart defect characterized by apical displacement of the tricuspid valve, is most notably associated with **lithium exposure** during the first trimester of pregnancy.
- This cardiac anomaly is not typically linked to valproic acid or other anticonvulsant medications.
*Discolored teeth*
- **Discolored teeth** (yellow-brown staining) and enamel hypoplasia are classic adverse effects of **tetracycline antibiotics** when administered during pregnancy (second and third trimesters) or early childhood.
- This effect is not associated with antiepileptic medications.
Medication safety in pregnancy US Medical PG Question 10: A 29-year-old woman presents to a medical office complaining of fatigue, nausea, and vomiting for 1 week. Recently, the smell of certain foods makes her nauseous. Her symptoms are more pronounced in the mornings. The emesis is clear-to-yellow without blood. She has had no recent travel out of the country. The medical history is significant for peptic ulcer, for which she takes pantoprazole. The blood pressure is 100/60 mm Hg, the pulse is 70/min, and the respiratory rate is 12/min. The physical examination reveals pale mucosa and conjunctiva, and bilateral breast tenderness. The LMP was 9 weeks ago. What is the most appropriate next step in the management of this patient?
- A. Beta-HCG levels and a transvaginal ultrasound (Correct Answer)
- B. Beta-HCG levels and a transabdominal ultrasound
- C. Beta-HCG levels and a pelvic CT
- D. Abdominal x-ray
- E. Abdominal CT with contrast
Medication safety in pregnancy Explanation: ***Beta-HCG levels and a transvaginal ultrasound***
- The patient's symptoms (fatigue, nausea, vomiting, morning sickness, breast tenderness, and **amenorrhea** for 9 weeks) strongly suggest **early pregnancy**.
- **Urine or serum beta-HCG** confirms pregnancy, and a **transvaginal ultrasound** is crucial for confirming an **intrauterine pregnancy**, estimating gestational age, and ruling out complications like ectopic pregnancy, especially at this early stage when transabdominal ultrasound might not provide clear images.
*Beta-HCG levels and a transabdominal ultrasound*
- While beta-HCG levels are appropriate, a **transabdominal ultrasound** may not be sufficient to visualize an early intrauterine pregnancy at 9 weeks due to limited resolution compared to transvaginal ultrasound.
- A definitive confirmation of **intrauterine pregnancy** is critical to rule out an **ectopic pregnancy**, which is better achieved with transvaginal imaging in early gestation.
*Beta-HCG levels and a pelvic CT*
- **CT scans** expose the patient to significant **ionizing radiation**, which is **contraindicated in pregnancy** unless absolutely necessary for life-threatening conditions.
- While it could identify some pelvic pathologies, it is **not the primary imaging modality** for confirming or evaluating early pregnancy due to radiation risks and inferior soft tissue resolution for early gestational sacs compared to ultrasound.
*Abdominal x-ray*
- An **abdominal X-ray** involves **ionizing radiation** and offers very limited diagnostic value for early pregnancy, as it cannot visualize the gestational sac, fetus, or fetal heart activity.
- It is **contraindicated** in suspected pregnancy due to the risk of fetal harm.
*Abdominal CT with contrast*
- **Abdominal CT with contrast** involves both **ionizing radiation** and **contrast agents**, both of which pose significant risks to a developing fetus.
- It is an **inappropriate initial step** for suspected pregnancy and offers no specific diagnostic benefits for confirming or characterizing early gestation.
More Medication safety in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.