Fetal growth assessment US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fetal growth assessment. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fetal growth assessment US Medical PG Question 1: A 25-year-old woman, gravida 2, para 1, comes to the physician for her initial prenatal visit at 18 weeks’ gestation. She is a recent immigrant from Thailand. Her history is significant for anemia since childhood that has not required any treatment. Her mother and husband have anemia, as well. She has no history of serious illness and takes no medications. Her vital signs are within normal limits. Fundal height measures at 22 weeks. Ultrasound shows polyhydramnios and pleural and peritoneal effusion in the fetus with fetal subcutaneous edema. Which of the following is the most likely clinical course for this fetus?
- A. Neonatal death
- B. Normal development with regular blood transfusion
- C. Asymptomatic anemia
- D. Intrauterine fetal demise (Correct Answer)
- E. Carrier state
Fetal growth assessment Explanation: ***Intrauterine fetal demise***
- The ultrasound findings of **polyhydramnios**, **pleural and peritoneal effusion**, and **fetal subcutaneous edema** are classic signs of **hydrops fetalis**.
- In a patient from Thailand with a history of lifelong anemia and a family history of anemia, these findings are highly suggestive of **alpha-thalassemia major (Hb Barts disease)**, which is almost always lethal in utero or shortly after birth.
*Neonatal death*
- While many cases of **hydrops fetalis** due to **alpha-thalassemia major** result in neonatal death, the severe findings often lead to **intrauterine fetal demise** before viability or at term.
- The combination of severe fetal compromise (multiple effusions, edema) and polyhydramnios often indicates a very poor prognosis and high likelihood of demise prior to full term delivery.
*Normal development with regular blood transfusion*
- This is typical for less severe forms of **thalassemia**, such as **beta-thalassemia major**, but not for **alpha-thalassemia major (Hb Barts disease)**, which is characterized by the complete absence of alpha-globin chains.
- **Hb Barts disease** is incompatible with life due to severe tissue hypoxia, as this hemoglobin has an extremely high affinity for oxygen and cannot release it to tissues effectively.
*Asymptomatic anemia*
- **Asymptomatic anemia** is generally associated with milder forms of anemia, such as alpha-thalassemia trait (two gene deletion) or beta-thalassemia minor.
- The severe manifestations of **hydrops fetalis** clearly indicate a profound, life-threatening condition for the fetus, not asymptomatic anemia.
*Carrier state*
- A **carrier state** (e.g., alpha-thalassemia trait) would typically involve mild or no anemia and would not cause **hydrops fetalis** in the fetus.
- The significant fetal pathology rules out a simple carrier state for the fetus; this fetus is severely affected by a major genetic disorder.
Fetal growth assessment US Medical PG Question 2: A 38-year-old G1P0 woman presents to her obstetrician for a prenatal visit. She reports feeling well and has no acute concerns. She is currently at 28 weeks gestation previously confirmed by ultrasound. She takes her folate supplements daily. She has a 10-pack-year smoking history and currently smokes half a pack per day. On physical exam, the uterus is soft and globular. The top of the uterine fundus is found around the level of the umbilicus. A fetal ultrasound demonstrates a reduced liver volume and subcutaneous fat with relative sparing of the head. Which of the following is most likely the cause of this patient's ultrasound findings?
- A. Cigarette smoking (Correct Answer)
- B. Aneuploidy
- C. Fetal congenital heart disease
- D. Neural tube defect
- E. Fetal infection
Fetal growth assessment Explanation: ***Cigarette smoking***
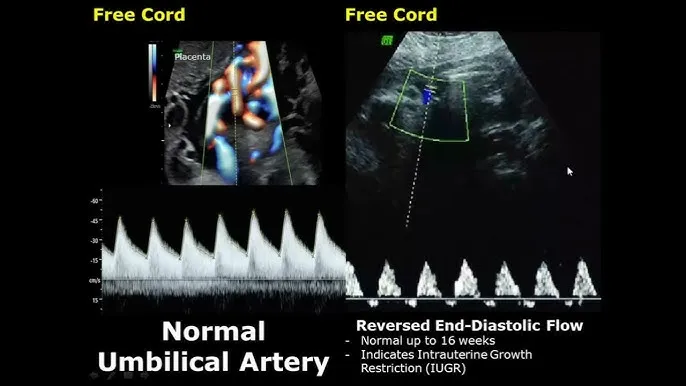
- Maternal cigarette smoking is a significant risk factor for **intrauterine growth restriction (IUGR)** due to reduced uteroplacental blood flow and hypoxia, leading to the observed findings of reduced liver volume and subcutaneous fat.
- The **"head-sparing"** growth pattern, where the head circumference remains relatively normal while abdominal circumference and overall growth are restricted, is characteristic of IUGR often caused by placental insufficiency, which is frequently associated with smoking.
*Aneuploidy*
- While aneuploidy can cause IUGR and congenital anomalies, the specific ultrasound findings of **reduced liver volume** and **subcutaneous fat** with **head sparing** are not uniquely indicative of aneuploidy.
- Aneuploidy often presents with multiple structural anomalies or specific dysmorphic features which are not mentioned here.
*Fetal congenital heart disease*
- Severe congenital heart disease can lead to IUGR and fetal hydrops; however, it typically results in a more global growth restriction or specific anomalies detectable on echocardiography, not selectively impacting liver volume and subcutaneous fat in a **head-sparing** manner without other overt cardiac signs.
- The primary defect would be cardiac, potentially leading to secondary growth restriction, but the direct findings described are more consistent with placental insufficiency.
*Neural tube defect*
- Neural tube defects primarily involve abnormalities of the **brain** and **spinal cord**, such as anencephaly or spina bifida.
- These defects do not typically cause isolated **reduced liver volume** or loss of **subcutaneous fat** in a head-sparing pattern.
*Fetal infection*
- Fetal infections (e.g., TORCH infections) can cause IUGR, but they are often associated with other specific findings such as **intracranial calcifications**, **hepatosplenomegaly**, **hydrops**, or specific organ damage, which are not described.
- The "head-sparing" pattern is less typical for acute fetal infections causing growth restriction, which often have a more symmetrical impact on growth.
Fetal growth assessment US Medical PG Question 3: A 40-year-old, gravida 2, nulliparous woman, at 14 weeks' gestation comes to the physician because of a 6-hour history of light vaginal bleeding and lower abdominal discomfort. Eight months ago she had a spontaneous abortion at 10 weeks' gestation. Her pulse is 92/min, respirations are 18/min, and blood pressure is 134/76 mm Hg. Abdominal examination shows no tenderness or masses; bowel sounds are normal. On pelvic examination, there is old blood in the vaginal vault and at the closed cervical os. The uterus is larger than expected for the length of gestation and there are bilateral adnexal masses. Serum β-hCG concentration is 120,000 mIU/ml. Which of the following is the most appropriate next step in management?
- A. Fetal blood sampling
- B. Fetal Doppler ultrasound
- C. Chorionic villus sampling
- D. Thyroid function tests
- E. Transvaginal ultrasound (Correct Answer)
Fetal growth assessment Explanation: ***Transvaginal ultrasound***
- The patient's presentation with **vaginal bleeding**, **uterus larger than expected**, **bilateral adnexal masses**, and **extremely elevated β-hCG (120,000 mIU/ml at 14 weeks)** strongly suggests a **hydatidiform mole** (a type of gestational trophoblastic disease).
- A **transvaginal ultrasound** is the definitive diagnostic tool to confirm a molar pregnancy, visualize the characteristic "snowstorm" appearance, and assess for any retained products of conception or ovarian theca-lutein cysts associated with high β-hCG.
*Fetal blood sampling*
- This procedure is typically performed later in pregnancy (after 18-20 weeks) to diagnose **fetal anemia**, **infections**, or **chromosomal abnormalities**, none of which are indicated by the current findings.
- The likelihood of a viable fetus with the clinical picture of a molar pregnancy is very low, making this intervention inappropriate.
*Fetal Doppler ultrasound*
- A fetal Doppler ultrasound primarily assesses **fetal blood flow** and well-being, which is not the priority given the high suspicion of a molar pregnancy.
- While it can detect a fetal heart rate in normal pregnancies, it would not provide the structural detail needed to diagnose a molar pregnancy.
*Chorionic villus sampling*
- This procedure is used for **prenatal genetic diagnosis** in early pregnancy (10-13 weeks) but would not be the first line of investigation for suspected molar pregnancy.
- The primary concern here is the diagnosis of a growth abnormality of the placenta, not fetal genetics, especially given the other strongly suggestive signs of a molar pregnancy.
*Thyroid function tests*
- While **hyperthyroidism** can be a rare complication of exceptionally high β-hCG levels due to its structural similarity to TSH, it is a secondary concern.
- Diagnosing the underlying cause of the high β-hCG and abnormal pregnancy, which is most likely a molar pregnancy, takes precedence over evaluating for potential secondary complications at this stage.
Fetal growth assessment US Medical PG Question 4: A 30-year-old woman, gravida 2, para 1, comes for a prenatal visit at 33 weeks' gestation. She delivered her first child spontaneously at 38 weeks' gestation; pregnancy was complicated by oligohydramnios. She has no other history of serious illness. Her blood pressure is 100/70 mm Hg. On pelvic examination, uterine size is found to be smaller than expected for dates. The fetus is in a longitudinal lie, with vertex presentation. The fetal heart rate is 144/min. Ultrasonography shows an estimated fetal weight below the 10th percentile, and decreased amniotic fluid volume. Which of the following is the most appropriate next step in this patient?
- A. Serial nonstress tests (Correct Answer)
- B. Emergent cesarean delivery
- C. Amnioinfusion
- D. Reassurance only
- E. Weekly fetal weight estimation
Fetal growth assessment Explanation: ***Serial nonstress tests***
- This patient presents with **intrauterine growth restriction (IUGR)** and **oligohydramnios**, placing her fetus at high risk for fetal compromise and stillbirth.
- **Serial nonstress tests (NSTs)** are essential for monitoring fetal well-being in such high-risk pregnancies, as they assess fetal heart rate accelerations in response to fetal movement, indicating a healthy central nervous system and adequate oxygenation.
*Emergent cesarean delivery*
- While the fetus has IUGR and oligohydramnios, there is no immediate evidence of **fetal distress** (e.g., severe decelerations or persistent bradycardia) that would warrant an **emergent** delivery at 33 weeks.
- Delivery at 33 weeks increases the risk of **neonatal complications** associated with prematurity, so conservative management with close monitoring is preferred if the fetus is not in acute distress.
*Amnioinfusion*
- **Amnioinfusion** involves introducing saline into the amniotic cavity and is primarily used to alleviate **umbilical cord compression** during labor by increasing amniotic fluid volume.
- It is **not indicated** for chronic oligohydramnios in the antepartum period as a primary treatment and does not address the underlying pathology of IUGR.
*Reassurance only*
- Given the findings of **IUGR** (estimated fetal weight below 10th percentile) and **oligohydramnios**, the situation is not benign and requires active management and monitoring.
- **Reassurance only** would be inappropriate and potentially harmful, as these conditions significantly increase the risk of adverse perinatal outcomes.
*Weekly fetal weight estimation*
- While **fetal weight estimation** is important for diagnosing and tracking IUGR, performing it **weekly** is unnecessarily frequent and not the primary method for ongoing surveillance of fetal well-being.
- **Biophysical profiles (BPPs)** or **nonstress tests (NSTs)** combined with amniotic fluid index measurements are more appropriate for regular surveillance of fetal compromise in IUGR.
Fetal growth assessment US Medical PG Question 5: A 4-month-old boy is brought to the physician for a well-child examination. He was born at 39 weeks gestation via spontaneous vaginal delivery and is exclusively breastfed. He weighed 3,400 g (7 lb 8 oz) at birth. At the physician's office, he appears well. His pulse is 146/min, the respirations are 39/min, and the blood pressure is 78/44 mm Hg. He weighs 7.5 kg (16 lb 9 oz) and measures 65 cm (25.6 in) in length. The remainder of the physical examination is normal. Which of the following developmental milestones has this patient most likely met?
- A. Sits with support of pelvis
- B. Grasps small objects between thumb and finger
- C. Transfers objects from hand to hand
- D. Intentionally rolls over (Correct Answer)
- E. Bounces actively when held in standing position
Fetal growth assessment Explanation: ***Intentionally rolls over***
- Rolling over is a common developmental milestone achieved between **4 to 6 months** of age.
- At 4 months, an infant typically has sufficient **head control** and **trunk strength** to intentionally roll from tummy to back or back to tummy.
*Sits with support of pelvis*
- Sitting with **pelvic support** (tripod sitting) is generally achieved around **6 to 7 months** of age.
- A 4-month-old typically lacks the necessary **trunk stability** and strength for this milestone.
*Grasps small objects between thumb and finger*
- This describes a **pincer grasp**, which is a fine motor skill usually developed around **9-12 months** of age.
- At 4 months, infants primarily use a **palmar grasp** (raking motion) to pick up objects.
*Transfers objects from hand to hand*
- Transferring objects from hand to hand is a fine motor milestone typically achieved between **5 and 7 months** of age.
- A 4-month-old is beginning to reach for objects but usually has difficulty with **smooth transfers** between hands.
*Bounces actively when held in standing position*
- Active bouncing when held in a standing position is typically seen around **6 months** when infants start putting more weight on their legs.
- At 4 months, while an infant might bear some weight, **active bouncing** is usually more rudimentary or absent.
Fetal growth assessment US Medical PG Question 6: A 24-year-old primigravida at 28 weeks gestation presents to the office stating that she “can’t feel her baby kicking anymore.” She also noticed mild-to-moderate vaginal bleeding. A prenatal visit a few days ago confirmed the fetal cardiac activity by Doppler. The medical history is significant for GERD, hypertension, and SLE. The temperature is 36.78°C (98.2°F), the blood pressure is 125/80 mm Hg, the pulse is 70/min, and the respiratory rate is 14/min. Which of the following is the next best step in evaluation?
- A. Confirmation of cardiac activity by Doppler (Correct Answer)
- B. Order platelet count, fibrinogen, PT and PTT levels
- C. Abdominal delivery
- D. Speculum examination
- E. Misoprostol
Fetal growth assessment Explanation: ***Confirmation of cardiac activity by Doppler***
- The patient presents with **decreased fetal movement** and **vaginal bleeding** at 28 weeks, which are concerning signs for complications like **placental abruption** or **fetal demise**.
- The immediate priority is to assess **fetal viability** by confirming the presence of a **fetal heartbeat**, with **Doppler ultrasonography** being the quickest and most accessible method.
*Order platelet count, fibrinogen, PT and PTT levels*
- While **coagulation studies** are important in cases of significant vaginal bleeding, especially if **placental abruption** is suspected, they are not the *next best step*.
- Assessing **fetal well-being** takes precedence, as the presence or absence of a **fetal heart rate** will guide subsequent emergency management.
*Abdominal delivery*
- **Abdominal delivery (C-section)** is a definitive intervention and should only be considered *after* an immediate assessment of **fetal status** and maternal stability.
- Delivery at 28 weeks gestation would be considered **preterm**, and careful evaluation is needed before making such a critical decision.
*Speculum examination*
- A **speculum examination** is used to investigate the source of vaginal bleeding, assess the cervix, and rule out causes such as **cervical lesions** or **cervical dilation**.
- However, given the *decreased fetal movement* and the potential for severe obstetrical emergencies, **fetal viability** must be confirmed first.
*Misoprostol*
- **Misoprostol** is a **prostaglandin analog** used to induce cervical ripening and uterine contractions, primarily for **labor induction** or **abortion**.
- It is not indicated as an initial diagnostic or therapeutic step in a patient with *decreased fetal movement* and *vaginal bleeding* without a clear diagnosis or indication for delivery.
Fetal growth assessment US Medical PG Question 7: A P2G1 diabetic woman is at risk of delivering at 29 weeks gestation. Her obstetrician counsels her that there is a risk the baby could have significant pulmonary distress after it is born. However, she states she will give the mother corticosteroids, which will help prevent this from occurring. Additionally, the obstetrician states she will perform a test on the amniotic fluid which will indicate the likelihood of the infant being affected by this syndrome. Which of the following ratios would be most predictive of the infant having pulmonary distress?
- A. lecithin:phosphatidylserine < 1.5
- B. lecithin:sphingomyelin < 1.5 (Correct Answer)
- C. lecithin:sphingomyelin > 1.5
- D. lecithin:phosphatidylserine > 3.0
- E. lecithin:sphingomyelin > 3.0
Fetal growth assessment Explanation: ***lecithin:sphingomyelin < 1.5***
- A lecithin:sphingomyelin (L:S) ratio less than 2:1 (or 1.5 in some clinical contexts) indicates **fetal lung immaturity** and a **high risk for respiratory distress syndrome (RDS)**.
- The **lecithin level increases** significantly in the amniotic fluid during the third trimester as fetal lungs mature, while **sphingomyelin levels remain relatively constant**.
*lecithin:phosphatidylserine < 1.5*
- While **phosphatidylserine** is a component of surfactant, the **Lecithin:Sphingomyelin (L:S) ratio** is the established and most commonly used marker for fetal lung maturity.
- There is **no widely recognized or clinically validated threshold** for a lecithin:phosphatidylserine ratio in predicting respiratory distress syndrome.
*lecithin:sphingomyelin > 1.5*
- An L:S ratio **greater than 2:1 (or 1.5, in some labs)** generally indicates **fetal lung maturity** and a low risk for respiratory distress syndrome.
- Therefore, this ratio would suggest a **lower likelihood of pulmonary distress**, which contradicts the aim of identifying risk.
*lecithin:phosphatidylserine > 3.0*
- As with an L:S ratio, a higher ratio would generally indicate **lung maturity**, not increased risk for pulmonary distress.
- There is **no clinical standard for lecithin:phosphatidylserine ratio** to assess lung maturity for preventing RDS.
*lecithin:sphingomyelin > 3.0*
- An L:S ratio of **greater than 2:1 (or 3.0 in certain clinical scenarios)** is a strong indicator of **fetal lung maturity**, meaning the risk of respiratory distress syndrome is low.
- The question asks for a ratio that would be **predictive of pulmonary distress**, whereas this ratio indicates the opposite.
Fetal growth assessment US Medical PG Question 8: A 25-year-old G1P0000 presents to her obstetrician’s office for her first prenatal visit. She had a positive pregnancy test 6 weeks ago, and her last period was about two months ago, though at baseline her periods are irregular. Aside from some slight nausea in the mornings, she feels well. Which of the following measurements would provide the most accurate dating of this patient’s pregnancy?
- A. Crown-rump length (Correct Answer)
- B. Femur length
- C. Abdominal circumference
- D. Biparietal diameter
- E. Serum beta-hCG
Fetal growth assessment Explanation: ***Crown-rump length***
- This measurement, typically obtained via **transvaginal ultrasound** in the first trimester (up to 13 weeks 6 days), provides the **most accurate gestational age dating**.
- It's highly precise because fetal growth is very consistent during this early period, minimizing variability.
*Femur length*
- This is a biometric measurement typically used for dating in the **second and third trimesters**.
- Its accuracy for dating is lower than CRL in the first trimester and becomes more variable in later pregnancy due to individual fetal growth differences.
*Abdominal circumference*
- This measurement is primarily used in the **late second and third trimetes**r to assess fetal growth and weight, rather than for accurate dating.
- It is highly susceptible to variations based on fetal nutrition and health, making it a poor choice for initial dating.
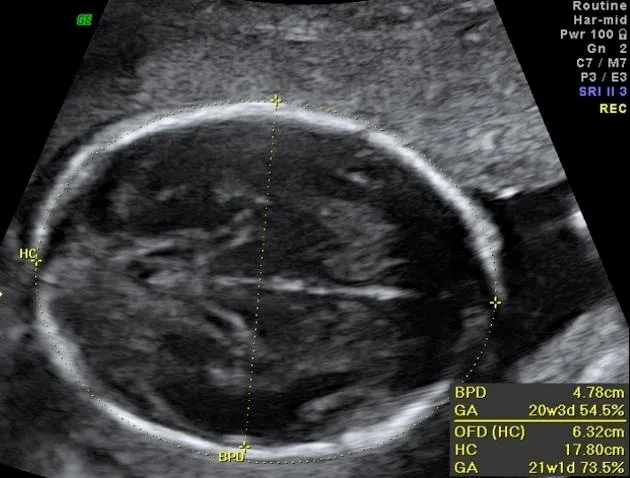
*Biparietal diameter*
- This is a reliable measurement for dating from the **late first trimester through the second trimester**, but it is less accurate than CRL in the very early first trimester.
- After the first trimester, its accuracy declines compared to earlier measurements as individual variations in head size become more prominent.
*Serum beta-hCG*
- While a **positive beta-hCG test** confirms pregnancy and quantitative levels can suggest gestational age ranges, it's not a precise dating tool.
- Levels vary widely among individuals and with different types of pregnancies (e.g., multiples), making it unsuitable for accurate dating.
Fetal growth assessment US Medical PG Question 9: A 30-year-old primigravida schedules an appointment with her obstetrician for a regular check-up. She says that everything is fine, although she reports that her baby has stopped moving as much as previously. She is 22 weeks gestation. She denies any pain or vaginal bleeding. The obstetrician performs an ultrasound and also orders routine blood and urine tests. On ultrasound, there is no fetal cardiac activity or movement. The patient is asked to wait for 1 hour, after which the scan is to be repeated. The second scan shows the same findings. Which of the following is the most likely diagnosis?
- A. Missed abortion
- B. Ectopic pregnancy
- C. Complete abortion
- D. Fetal demise (Correct Answer)
- E. Incomplete abortion
Fetal growth assessment Explanation: ***Fetal demise***
- The absence of fetal cardiac activity and movement on repeated ultrasound scans at 22 weeks' gestation, after previously reporting fetal movement, is consistent with **fetal demise**.
- **Fetal demise** refers to the death of a fetus in utero at or after 20 weeks of gestation, or when the fetus weighs 350 grams or more.
*Missed abortion*
- **Missed abortion** (or missed miscarriage) is typically defined as a non-viable intrauterine pregnancy with a retained fetus or embryo without cardiac activity before 20 weeks of gestation.
- The patient is 22 weeks gestation, which places the condition beyond the general definition of a missed abortion.
*Ectopic pregnancy*
- In an **ectopic pregnancy**, the fertilized egg implants outside the uterus, most commonly in the fallopian tube, and would not have reached 22 weeks with reported fetal movement.
- An ectopic pregnancy would present with earlier symptoms like **abdominal pain** and **vaginal bleeding**, and an ultrasound would show an empty uterus or evidence of extrauterine pregnancy.
*Complete abortion*
- A **complete abortion** involves the complete expulsion of all products of conception from the uterus.
- This would be characterized by **heavy vaginal bleeding** and the passage of tissue, which the patient denies.
*Incomplete abortion*
- An **incomplete abortion** occurs when some, but not all, products of conception have been expelled from the uterus.
- Similar to complete abortion, an incomplete abortion would typically involve **vaginal bleeding** and retained tissue, accompanied by **cramping**, which are absent in this case.
Fetal growth assessment US Medical PG Question 10: A 32-year-old G1P0 woman presents to her obstetrician for a prenatal visit. She is 30 weeks pregnant. She reports some fatigue and complains of urinary urgency. Prior to this pregnancy, she had no significant medical history. She takes a prenatal vitamin and folate supplements daily. Her mother has diabetes, and her brother has coronary artery disease. On physical examination, the fundal height is 25 centimeters. A fetal ultrasound shows a proportional reduction in head circumference, trunk size, and limb length. Which of the following is the most likely cause of the patient’s presentation?
- A. Gestational diabetes
- B. Antiphospholipid syndrome
- C. Rubella infection (Correct Answer)
- D. Pre-eclampsia
- E. Cigarette smoking
Fetal growth assessment Explanation: **Rubella infection**
- The **reduced fundal height** (25 cm at 30 weeks) and **symmetrically small fetus** (proportional reduction in head, trunk, and limbs) are characteristic findings of **intrauterine growth restriction (IUGR)** due to a congenital infection like rubella.
- Maternal symptoms like **fatigue** and **urinary urgency** are non-specific but, in the context of fetal findings, point towards a systemic process affecting both mother and fetus.
*Gestational diabetes*
- Fetal growth in gestational diabetes is typically characterized by **macrosomia** (large for gestational age), not IUGR.
- Clinical findings would usually include a **fundal height larger than expected** for gestational age due to a larger fetus.
*Antiphospholipid syndrome*
- This condition is associated with **recurrent pregnancy loss**, **thrombosis**, and **placental insufficiency**, which can lead to IUGR.
- However, the IUGR associated with antiphospholipid syndrome is typically **asymmetric**, meaning the head circumference is spared while the abdomen and other body parts are disproportionately small.
*Pre-eclampsia*
- Pre-eclampsia can cause **IUGR** due to placental insufficiency, but it is primarily characterized by **new-onset hypertension** and **proteinuria** after 20 weeks of gestation, which are not mentioned in this case.
- While fatigue and urgency can be present, the absence of hypertension and proteinuria makes pre-eclampsia less likely as the primary cause.
*Cigarette smoking*
- Maternal cigarette smoking is a known risk factor for **IUGR**, particularly **symmetrical IUGR**.
- However, the patient's medical history states "no significant medical history" and does not mention smoking, making an infection a more likely explanation given the context.
More Fetal growth assessment US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.