Exercise in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Exercise in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Exercise in pregnancy US Medical PG Question 1: A 29-year-old woman, gravida 1, para 0, at 36 weeks' gestation is brought to the emergency department after an episode of dizziness and vomiting followed by loss of consciousness lasting 1 minute. She reports that her symptoms started after lying down on her back to rest, as she felt tired during yoga class. Her pregnancy has been uncomplicated. On arrival, she is diaphoretic and pale. Her pulse is 115/min and blood pressure is 90/58 mm Hg. On examination, the patient is lying in the supine position with a fundal height of 36 cm. There is a prolonged fetal heart rate deceleration to 80/min. Which of the following is the most appropriate action to reverse this patient's symptoms in the future?
- A. Performing the Muller maneuver
- B. Gentle compression with an abdominal binder
- C. Lying in the supine position and elevating legs
- D. Lying in the left lateral decubitus position (Correct Answer)
- E. Performing the Valsava maneuver
Exercise in pregnancy Explanation: ***Lying in the left lateral decubitus position***
- This position relieves **aortocaval compression** by moving the uterus off the **inferior vena cava (IVC)** and aorta.
- Alleviating IVC compression increases **venous return** to the heart, improving **cardiac output** and blood pressure, thereby resolving the patient's symptoms and improving **fetal oxygenation**.
*Performing the Muller maneuver*
- The **Muller maneuver** involves forced inspiration against a closed glottis, creating **negative intrathoracic pressure**.
- This maneuver is used to evaluate **upper airway compromise** and would not address the underlying issue of aortocaval compression.
*Gentle compression with an abdominal binder*
- An **abdominal binder** would apply external pressure to the abdomen, which could worsen rather than alleviate **aortocaval compression**.
- This would further reduce **venous return** and potentially exacerbate the patient's **hypotension** and fetal distress.
*Lying in the supine position and elevating legs*
- Lying in the **supine position** is the cause of the patient's symptoms due to **aortocaval syndrome**.
- While **elevating the legs** can temporarily increase venous return from the legs, it would not relieve the compression of the IVC by the gravid uterus.
*Performing the Valsava maneuver*
- The **Valsalva maneuver** involves forced exhalation against a closed glottis, which increases **intrathoracic pressure** and decreases **venous return**.
- This would further reduce **cardiac output** and worsen the symptoms of **hypotension** and **fetal compromise**.
Exercise in pregnancy US Medical PG Question 2: A 40-year-old pregnant woman, G4 P3, visits your office at week 30 of gestation. She is very excited about her pregnancy and wants to be the healthiest she can be in preparation for labor and for her baby. What vaccination should she receive at this visit?
- A. Measles, mumps, and rubella (MMR)
- B. Varicella vaccine
- C. Herpes zoster vaccine
- D. Live attenuated influenza vaccine
- E. Tetanus, diphtheria, and acellular pertussis (Tdap) (Correct Answer)
Exercise in pregnancy Explanation: ***Tetanus, diphtheria, and acellular pertussis (Tdap)***
- The Tdap vaccine is recommended during each pregnancy, preferably between **27 and 36 weeks of gestation**, to maximize maternal antibody response and passive antibody transfer to the fetus.
- This provides critical protection against **pertussis (whooping cough)** for the newborn, who is too young to be vaccinated.
*Measles, mumps, and rubella (MMR)*
- The **MMR vaccine is a live vaccine** and is **contraindicated during pregnancy** due to the theoretical risk of congenital rubella syndrome, although no cases have been reported.
- It should be administered **postpartum** if the mother is not immune to rubella.
*Varicella vaccine*
- The **varicella vaccine is a live vaccine** and is **contraindicated during pregnancy** due to the theoretical risk of congenital varicella syndrome.
- Like MMR, it should be offered in the **postpartum period** if the woman is not immune.
*Herpes zoster vaccine*
- The herpes zoster vaccine is typically recommended for **older adults** (50 years and older) for shingles prevention.
- It is **not routinely recommended during pregnancy**, and its safety and efficacy in this population have not been sufficiently established.
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is **contraindicated during pregnancy** due to its live virus content.
- Pregnant women should receive the **inactivated influenza vaccine (IIV)**, which is safe and recommended during any trimester.
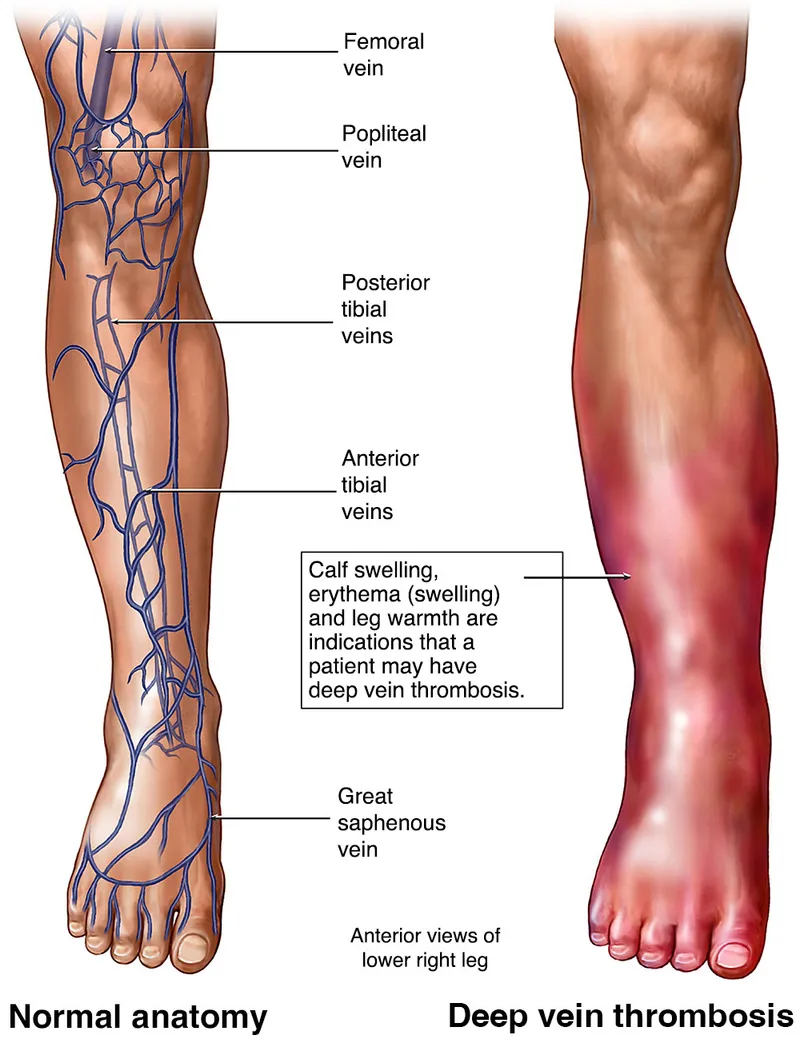
Exercise in pregnancy US Medical PG Question 3: A 32-year-old primigravida at 35 weeks gestation seeks evaluation at the emergency department for swelling and redness of the left calf, which started 2 hours ago. She reports that the pain has worsened since the onset. The patient denies a history of insect bites or trauma. She has never experienced something like this in the past. Her pregnancy has been uneventful so far. She does not use alcohol, tobacco, or any illicit drugs. She does not take any medications other than prenatal vitamins. Her temperature is 36.8℃ (98.2℉), the blood pressure is 105/60 mm Hg, the pulse is 110/min, and the respirations are 15/min. The left calf is edematous with the presence of erythema. The skin feels warm and pain is elicited with passive dorsiflexion of the foot. The femoral, popliteal, and pedal pulses are palpable bilaterally. An abdominal examination reveals a fundal height consistent with the gestational age. The lungs are clear to auscultation bilaterally. The patient is admitted to the hospital and appropriate treatment is initiated. Which of the following hormones is most likely implicated in the development of this patient’s condition?
- A. Human placental lactogen
- B. Human chorionic gonadotropin
- C. Progesterone (Correct Answer)
- D. Prolactin
- E. Estriol
Exercise in pregnancy Explanation: ***Progesterone***
- This patient presents with symptoms highly suggestive of **deep vein thrombosis (DVT)**, including unilateral leg swelling, warmth, erythema, and pain with dorsiflexion (**Homans' sign**). Pregnancy is a significant risk factor for DVT due to a **hypercoagulable state**.
- **Progesterone** is a key hormone in pregnancy that contributes to venous stasis by causing **venodilation** and decreasing vascular tone, making pregnant women more susceptible to DVT. It also contributes to the overall hypercoagulable state.
*Human placental lactogen*
- **Human placental lactogen (hPL)** is primarily involved in **insulin resistance** and glucose regulation in the mother to ensure nutrient supply to the fetus.
- It does not directly contribute to the thrombotic risk or venous changes seen in DVT.
*Human chorionic gonadotropin*
- **Human chorionic gonadotropin (hCG)** maintains the **corpus luteum** in early pregnancy and is associated with morning sickness.
- While essential for pregnancy, it does not directly influence coagulation or venous status to predispose to DVT.
*Prolactin*
- **Prolactin** is crucial for **mammary gland development** and **lactation**.
- It does not have a direct role in the physiological changes that increase DVT risk during pregnancy.
*Estriol*
- **Estriol** is a major estrogen in pregnancy, and like other estrogens, it contributes to the **hypercoagulable state** by increasing clotting factors and decreasing natural anticoagulants.
- However, progesterone's role in **venodilation and venous stasis** is more directly implicated in the acute development of DVT symptoms in the lower extremities during late pregnancy than the broad procoagulant effects of estrogen.
Exercise in pregnancy US Medical PG Question 4: Immediately following prolonged delivery of the placenta at 40 weeks gestation, a 32-year-old multiparous woman develops vaginal bleeding. Other than mild asthma, the patient’s pregnancy has been uncomplicated. She has attended many prenatal appointments and followed the physician's advice about screening for diseases, laboratory testing, diet, and exercise. Previous pregnancies were uncomplicated. She has no history of a serious illness. She is currently on intravenous infusion of oxytocin. Her temperature is 37.2°C (99.0°F), blood pressure is 108/60 mm Hg, pulse is 88/min, and respirations are 17/min. Uterine palpation reveals a soft enlarged fundus that extends above the umbilicus. Based on the assessment of the birth canal and placenta, which of the following options is the most appropriate initial step in patient management?
- A. Intramuscular carboprost
- B. Manual exploration of the uterus
- C. Discontinuing oxytocin
- D. Intravenous methylergonovine
- E. Uterine fundal massage (Correct Answer)
Exercise in pregnancy Explanation: ***Uterine fundal massage***
- The patient presents with **postpartum hemorrhage** indicated by vaginal bleeding and a **soft, enlarged fundus** after placental delivery, suggesting **uterine atony**.
- **Uterine fundal massage** is the **first-line intervention** to encourage uterine contraction and reduce bleeding by expelling clots and compressing vessels.
*Intramuscular carboprost*
- **Carboprost** is a **prostaglandin F2 alpha analog** used to treat **uterine atony** when initial measures like uterine massage and oxytocin are insufficient.
- It is contraindicated in patients with **asthma** due to its bronchoconstrictive effects, which this patient has.
*Manual exploration of the uterus*
- **Manual exploration of the uterus** is indicated when there is suspicion of **retained placental fragments** or **uterine rupture**.
- While these can cause postpartum hemorrhage, the primary finding of a soft, boggy uterus points more strongly to atony, making massage the immediate priority.
*Discontinuing oxytocin*
- The patient is already on an **intravenous oxytocin infusion**, which is a uterotonic agent used to prevent and treat uterine atony.
- Discontinuing it would worsen **uterine atony** and increase blood loss, directly contradicting the goal of management.
*Intravenous methylergonovine*
- **Methylergonovine** is an **ergot alkaloid** used to treat **uterine atony**, but it is contraindicated in patients with **hypertension**, which is not explicitly present here, but it is a potent vasoconstrictor and second-line.
- It is often used as a **second-line agent** if oxytocin and massage are ineffective and there are no contraindications.
Exercise in pregnancy US Medical PG Question 5: A 27-year-old Hispanic G2P1 presents for a routine antepartum visit at 26 weeks gestation. She has no complaints. The vital signs are normal, the physical examination is within normal limits, and the gynecologic examination corresponds to 25 weeks gestation. The oral glucose tolerance test (OGTT) with a 75-g glucose load is significant for a glucose level of 177 mg/dL at 1 hour and 167 mg/dL at 2 hour. The fasting blood glucose level is 138 mg/dL (7.7 mmol/L), and the HbA1c is 7%. Which of the following represents the proper initial management?
- A. Sitagliptin
- B. Dietary and lifestyle modification
- C. Metformin
- D. Glyburide
- E. Insulin (Correct Answer)
Exercise in pregnancy Explanation: **Insulin**
- The patient's **fasting glucose of 138 mg/dL** and **HbA1c of 7%** indicate pre-existing **Type 2 Diabetes Mellitus**, not just gestational diabetes. Both values exceed the diagnostic thresholds for overt diabetes in pregnancy.
- **Insulin** is the preferred initial pharmacologic treatment for **overt diabetes in pregnancy** because it does not cross the placenta, ensuring fetal safety, and is highly effective in controlling maternal glucose levels.
*Sitagliptin*
- **Sitagliptin** is a **DPP-4 inhibitor** and is not recommended during pregnancy due to limited safety data and the availability of safer alternatives.
- Oral hypoglycemic agents are generally avoided as first-line therapy for established diabetes in pregnancy due to potential for placental transfer and adverse fetal effects.
*Dietary and lifestyle modification*
- While crucial, **dietary and lifestyle modification** alone are insufficient for managing overt diabetes with such high fasting glucose and HbA1c levels.
- These measures are usually the first step for **gestational diabetes**, but a patient with overt diabetes requires immediate pharmacologic intervention to prevent complications.
*Metformin*
- **Metformin** can be used in pregnancy but is primarily considered for **gestational diabetes** or as an alternative to insulin if the patient has milder hyperglycemia, or if insulin is poorly tolerated.
- Given the patient's significantly elevated fasting glucose and HbA1c, **insulin** is a more effective and immediate treatment to achieve glycemic control and reduce risks.
*Glyburide*
- **Glyburide** is an **oral sulfonylurea** that can cross the placenta, leading to potential fetal hyperinsulinemia and neonatal hypoglycemia.
- Its use in pregnancy is generally discouraged due to these risks, making **insulin** a safer and more appropriate choice.
Exercise in pregnancy US Medical PG Question 6: A 44-year-old woman with high blood pressure and diabetes presents to the outpatient clinic and informs you that she is trying to get pregnant. Her current medications include lisinopril, metformin, and sitagliptin. Her blood pressure is 136/92 mm Hg and heart rate is 79/min. Her physical examination is unremarkable. What should you do regarding her medication for high blood pressure?
- A. Discontinue lisinopril and initiate aliskiren
- B. Discontinue lisinopril and initiate labetalol (Correct Answer)
- C. Continue her current regimen
- D. Continue her current regimen and add a beta-blocker for increased control
- E. Discontinue lisinopril and initiate candesartan
Exercise in pregnancy Explanation: ***Discontinue lisinopril and initiate labetalol***
- **Lisinopril**, an ACE inhibitor, is **teratogenic** and is contraindicated in pregnancy due to the risk of fetal renal dysfunction, oligohydramnios, and neonatal death.
- **Labetalol** is a **beta-blocker** commonly used in pregnancy for hypertension as it is considered safe and effective in this population.
*Discontinue lisinopril and initiate aliskiren*
- **Aliskiren**, a direct renin inhibitor, is also **teratogenic** and contraindicated in pregnancy due to similar risks as ACE inhibitors and ARBs.
- Replacing one teratogenic drug with another does not solve the primary concern of fetal safety.
*Continue her current regimen*
- **Continuing lisinopril** would expose the fetus to significant risks, as it is a known teratogen.
- The patient is actively trying to conceive, making it imperative to switch medications immediately.
*Continue her current regimen and add a beta-blocker for increased control*
- Adding a beta-blocker while continuing lisinopril is still inappropriate because **lisinopril itself is harmful during pregnancy**.
- The primary goal is to **discontinue teratogenic medications**, not simply to improve blood pressure control with an additional drug.
*Discontinue lisinopril and initiate candesartan*
- **Candesartan**, an **angiotensin receptor blocker (ARB)**, shares the same **teratogenic risks** as ACE inhibitors and is contraindicated in pregnancy.
- Replacing an ACE inhibitor with an ARB provides no benefit in terms of fetal safety.
Exercise in pregnancy US Medical PG Question 7: A 21-year-old female presents to her primary care doctor for prenatal counseling before attempting to become pregnant for the first time. She is an avid runner, and the physician notes her BMI of 17.5. The patient complains of chronic fatigue, which she attributes to her busy lifestyle. The physician orders a complete blood count that reveals a Hgb 10.2 g/dL (normal 12.1 to 15.1 g/dL) with an MCV 102 µm^3 (normal 78 to 98 µm^3). A serum measurement of a catabolic derivative of methionine returns elevated. Which of the following complications is the patient at most risk for if she becomes pregnant?
- A. Placenta abruptio (Correct Answer)
- B. Placenta previa
- C. Placenta accreta
- D. Neural tube defects
- E. Gestational diabetes
Exercise in pregnancy Explanation: **Placenta abruptio**
* The patient presents with several risk factors for **placental abruption**, including **low BMI**, **anemia** (Hgb 10.2), and **elevated homocysteine** (indicated by elevated catabolic derivative of methionine, implying **folate or B12 deficiency**, which leads to high homocysteine).
* **Anemia** and **folate deficiency** are associated with an increased risk of placental abruption.
*Placenta previa*
* **Placenta previa** is characterized by the placenta covering the cervical os, typically associated with risk factors like **previous C-section**, **multiparity**, and **advanced maternal age**.
* The patient's profile (first pregnancy, young) does not align with the typical risk factors for placenta previa.
*Placenta accreta*
* **Placenta accreta** involves abnormal placental adherence to the uterine wall, most commonly linked to **prior uterine surgery** (especially C-sections) and **placenta previa**.
* The patient has no history of uterine surgery, making placenta accreta an unlikely primary risk.
*Neural tube defects*
* **Neural tube defects** are associated with **folate deficiency**, which is likely present given the **macrocytic anemia** (MCV 102) and elevated homocysteine.
* However, the question asks for the complication the patient is *most* at risk for due to her overall profile including her low BMI and anemia, and while NTDs are a risk, the combination of factors points more strongly to placental abruption.
*Gestational diabetes*
* **Gestational diabetes** is linked to risk factors like **obesity**, **family history of diabetes**, and **advanced maternal age**.
* The patient's **low BMI** (17.5) and young age make gestational diabetes an unlikely significant risk.
Exercise in pregnancy US Medical PG Question 8: A 23-year-old nulligravida presents for evaluation 5 weeks after her last menstrual period. Her previous menstruation cycle was regular, and her medical history is benign. She is sexually active with one partner and does not use contraception. A urine dipstick pregnancy test is negative. The vital signs are as follows: blood pressure 120/80 mm Hg, heart rate 71/min, respiratory rate 13/min, and temperature 36.8°C (98.2°F). The physical examination is notable for breast engorgement, increased pigmentation of the nipples, and linea nigra. The gynecologic examination demonstrates cervical and vaginal cyanosis.
Measurement of which of the following substances is most appropriate in this case?
- A. Blood estriol
- B. Blood human chorionic gonadotropin (Correct Answer)
- C. Urinary estrogen metabolites
- D. Urinary human chorionic gonadotropin
- E. Blood progesterone
Exercise in pregnancy Explanation: ***Blood human chorionic gonadotropin***
- The patient exhibits classic signs of early pregnancy, including **breast engorgement**, **nipple hyperpigmentation**, **linea nigra**, and **cervical and vaginal cyanosis** (Chadwick's sign). These signs, combined with a missed menstrual period and unprotected intercourse, strongly indicate pregnancy despite the negative urine dipstick.
- A **blood human chorionic gonadotropin (hCG)** test is more sensitive than a urine test, detecting lower levels of hCG earlier in pregnancy, and is therefore the most appropriate next step to confirm pregnancy.
*Blood estriol*
- **Estriol** levels are used to assess fetal well-being in the late second and third trimesters, typically as part of the **triple or quadruple screen**, not for early pregnancy detection.
- Its levels become significantly elevated much later in pregnancy, making it unsuitable for confirming a pregnancy at 5 weeks.
*Urinary estrogen metabolites*
- **Urinary estrogen metabolites** are primarily used to assess ovarian function and fertility, or to monitor hormone replacement therapy.
- They are not a reliable or standard method for the early detection or confirmation of pregnancy.
*Urinary human chorionic gonadotropin*
- While **urinary hCG** is used for pregnancy detection (e.g., home pregnancy tests), a negative result at 5 weeks, especially in the presence of strong clinical signs of pregnancy, suggests that the levels might be below the detection threshold of the urine test.
- A **quantitative blood hCG** test is superior in sensitivity and can detect very low levels of hCG, confirming or ruling out early pregnancy more definitively.
*Blood progesterone*
- **Progesterone** levels are necessary to maintain a pregnancy, but they do not confirm a pregnancy itself. High progesterone can indicate ovulation and potential luteal phase support.
- While useful for assessing the viability of a confirmed early pregnancy or diagnosing conditions like ectopic pregnancy, it's not the primary test to confirm the presence of pregnancy.
Exercise in pregnancy US Medical PG Question 9: A 29-year-old woman presents to a medical office complaining of fatigue, nausea, and vomiting for 1 week. Recently, the smell of certain foods makes her nauseous. Her symptoms are more pronounced in the mornings. The emesis is clear-to-yellow without blood. She has had no recent travel out of the country. The medical history is significant for peptic ulcer, for which she takes pantoprazole. The blood pressure is 100/60 mm Hg, the pulse is 70/min, and the respiratory rate is 12/min. The physical examination reveals pale mucosa and conjunctiva, and bilateral breast tenderness. The LMP was 9 weeks ago. What is the most appropriate next step in the management of this patient?
- A. Beta-HCG levels and a transvaginal ultrasound (Correct Answer)
- B. Beta-HCG levels and a transabdominal ultrasound
- C. Beta-HCG levels and a pelvic CT
- D. Abdominal x-ray
- E. Abdominal CT with contrast
Exercise in pregnancy Explanation: ***Beta-HCG levels and a transvaginal ultrasound***
- The patient's symptoms (fatigue, nausea, vomiting, morning sickness, breast tenderness, and **amenorrhea** for 9 weeks) strongly suggest **early pregnancy**.
- **Urine or serum beta-HCG** confirms pregnancy, and a **transvaginal ultrasound** is crucial for confirming an **intrauterine pregnancy**, estimating gestational age, and ruling out complications like ectopic pregnancy, especially at this early stage when transabdominal ultrasound might not provide clear images.
*Beta-HCG levels and a transabdominal ultrasound*
- While beta-HCG levels are appropriate, a **transabdominal ultrasound** may not be sufficient to visualize an early intrauterine pregnancy at 9 weeks due to limited resolution compared to transvaginal ultrasound.
- A definitive confirmation of **intrauterine pregnancy** is critical to rule out an **ectopic pregnancy**, which is better achieved with transvaginal imaging in early gestation.
*Beta-HCG levels and a pelvic CT*
- **CT scans** expose the patient to significant **ionizing radiation**, which is **contraindicated in pregnancy** unless absolutely necessary for life-threatening conditions.
- While it could identify some pelvic pathologies, it is **not the primary imaging modality** for confirming or evaluating early pregnancy due to radiation risks and inferior soft tissue resolution for early gestational sacs compared to ultrasound.
*Abdominal x-ray*
- An **abdominal X-ray** involves **ionizing radiation** and offers very limited diagnostic value for early pregnancy, as it cannot visualize the gestational sac, fetus, or fetal heart activity.
- It is **contraindicated** in suspected pregnancy due to the risk of fetal harm.
*Abdominal CT with contrast*
- **Abdominal CT with contrast** involves both **ionizing radiation** and **contrast agents**, both of which pose significant risks to a developing fetus.
- It is an **inappropriate initial step** for suspected pregnancy and offers no specific diagnostic benefits for confirming or characterizing early gestation.
Exercise in pregnancy US Medical PG Question 10: Three days after delivery of a male newborn, a 36-year-old gravida 1, para 1 woman has fever and pain in her left leg. Pregnancy was complicated by premature rupture of membranes; the child was delivered at 35 weeks' gestation by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. The patient has smoked half a pack of cigarettes daily for 5 years and continued to smoke during her pregnancy. Her temperature is 38.9°C (102°F), pulse is 110/min, and blood pressure is 110/80 mm Hg. Examination shows an edematous, erythematous, and warm left leg. Passive dorsiflexion of the left foot elicits pain in the calf. The peripheral pulses are palpated bilaterally. The uterus is nontender and palpated at the umbilicus. Ultrasonography of the left leg shows an incompressible left popliteal vein. Which of the following is the most appropriate initial step in management?
- A. Graduated compression stockings
- B. Urokinase
- C. Low molecular weight heparin (Correct Answer)
- D. Embolectomy
- E. Warfarin
Exercise in pregnancy Explanation: ***Low molecular weight heparin***
- The patient's symptoms (leg pain, edema, erythema, warmth, positive Homan's sign), fever, and ultrasound findings of an **incompressible popliteal vein** are highly suggestive of **deep vein thrombosis (DVT)**, for which LMWH is the first-line treatment.
- She has several risk factors for DVT, including pregnancy/postpartum state, premature rupture of membranes, C-section, smoking, and fever (possibly indicating an underlying inflammatory state or infection).
*Graduated compression stockings*
- While compression stockings can be used as an adjunct to DVT treatment or for prevention, they are **not sufficient as a sole initial treatment** for an acute, symptomatic DVT confirmed by ultrasound.
- Their primary role is often in preventing post-thrombotic syndrome after adequate anticoagulation has been established or for prophylaxis in high-risk individuals.
*Urokinase*
- **Urokinase is a thrombolytic agent** used in specific, severe cases of DVT (e.g., iliofemoral DVT with limb-threatening ischemia or pulmonary embolism with hemodynamic instability) and carries a significant risk of bleeding.
- It is **not the initial management** for an uncomplicated DVT.
*Embolectomy*
- **Embolectomy (surgical removal of a clot)** is reserved for very severe cases of DVT or pulmonary embolism, especially when there is **limb ischemia** or life-threatening pulmonary embolism despite thrombolysis.
- It is an invasive procedure with higher risks and is not indicated as an initial step for this patient's presentation.
*Warfarin*
- **Warfarin is an oral anticoagulant** that is typically started after initial anticoagulation with heparin (either unfractionated or low molecular weight) has been established.
- It has a **delayed onset of action** (due to depletion of vitamin K-dependent clotting factors) and requires careful monitoring with INR, making it unsuitable for initial rapid anticoagulation in acute DVT.
More Exercise in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.