Antepartum fetal surveillance (NST, BPP) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antepartum fetal surveillance (NST, BPP). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
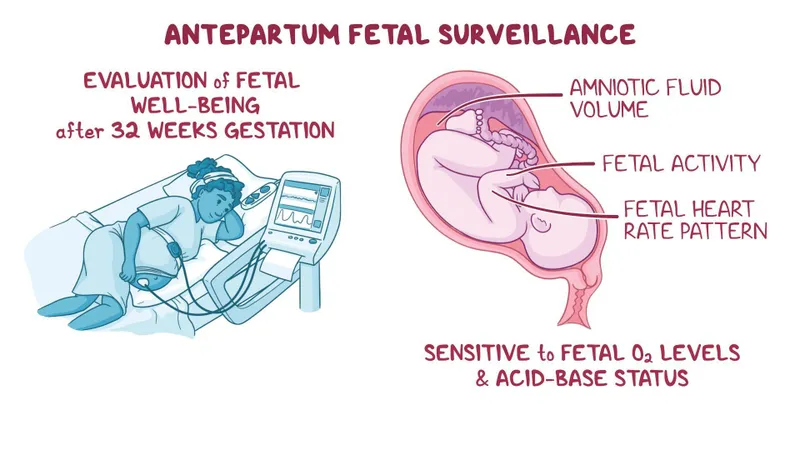
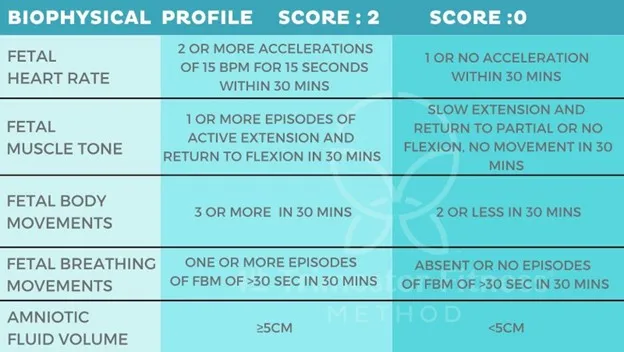
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 1: A 29-year-old woman, gravida 1, para 0, at 33 weeks' gestation comes to her doctor for a routine visit. Her pregnancy has been uncomplicated. She has systemic lupus erythematosus and has had no flares during her pregnancy. She does not smoke cigarettes, drink alcohol, or use illicit drugs. Current medications include iron, vitamin supplements, and hydroxychloroquine. Her temperature is 37.2°C (98.9°F), pulse is 70/min, respirations are 17/min, and blood pressure is 134/70 mm Hg. She appears well. Physical examination shows no abnormalities. Ultrasound demonstrates fetal rhythmic breathing for > 30 seconds, amniotic fluid with deepest vertical pocket of 1 cm, one distinct fetal body movement over 30 minutes, and no episodes of extremity extension over 30 minutes. Nonstress test is reactive and reassuring. Which of the following is the next best step in management?
- A. Administer corticosteroids and continue close monitoring (Correct Answer)
- B. Perform cesarean delivery
- C. Discontinue hydroxychloroquine and continue close monitoring
- D. Induction of labor
- E. Reassurance with expectant management
Antepartum fetal surveillance (NST, BPP) Explanation: ***Administer corticosteroids and continue close monitoring***
- The combination of a **nonreactive nonstress test (NST)** and an **amniotic fluid index (AFI) < 5 cm** (deepest vertical pocket of 1 cm) indicates **oligohydramnios** and potential fetal compromise, necessitating corticosteroid administration for lung maturity and close monitoring.
- While the NST is reassuring, the oligohydramnios is a significant concern that warrants intervention to optimize fetal outcomes and prepare for potential preterm delivery.
*Perform cesarean delivery*
- This step is **overly aggressive** given the reactive nonstress test and stable maternal condition.
- There are no immediate signs of **acute fetal distress** that would necessitate emergent delivery.
*Discontinue hydroxychloroquine and continue close monitoring*
- **Hydroxychloroquine** is safe and often continued during pregnancy for patients with systemic lupus erythematosus, as it helps prevent flares and is not associated with adverse fetal outcomes.
- Discontinuing it without a clear indication could lead to a **maternal SLE flare**, which could be detrimental to both mother and fetus.
*Induction of labor*
- Induction of labor is not indicated at this gestational age (33 weeks) unless there is clear evidence of **significant fetal distress** or maternal complications.
- While there is oligohydramnios, the **reactive NST** suggests sufficient fetal reserve to allow for corticosteroid administration to promote lung maturity first.
*Reassurance with expectant management*
- The finding of **oligohydramnios** (deepest vertical pocket of 1 cm) is a significant concern, as it is associated with increased risks of **cord compression**, fetal growth restriction, and adverse perinatal outcomes.
- Therefore, expectant management without intervention would be **inappropriate** given this finding.
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 2: A 36-year-old primigravid woman at 26 weeks' gestation comes to the physician complaining of absent fetal movements for the last 2 days. Pregnancy was confirmed by ultrasonography 14 weeks earlier. She has no vaginal bleeding or discharge. She has a history of type 1 diabetes mellitus controlled with insulin. Vital signs are all within the normal limits. Pelvic examination shows a soft, 2-cm long cervix in the midline with a cervical os measuring 3 cm and a uterus consistent in size with 24 weeks' gestation. Transvaginal ultrasonography shows a fetus with no cardiac activity. Which of the following is the most appropriate next step in management?
- A. Plan for oxytocin administration (Correct Answer)
- B. Perform weekly pelvic ultrasound
- C. Perform dilation and curettage
- D. Perform cesarean delivery
- E. Administer magnesium sulfate
Antepartum fetal surveillance (NST, BPP) Explanation: ***Plan for oxytocin administration***
- The patient is at 26 weeks' gestation with confirmed fetal demise and an effaced, dilated cervix (2 cm long, 3 cm dilated). This indicates the cervix is already preparing for delivery.
- **Oxytocin** is the most appropriate next step to induce labor and facilitate vaginal delivery in cases of **intrauterine fetal demise** (IUFD) after the first trimester, especially when cervical changes have begun.
*Perform weekly pelvic ultrasound*
- The ultrasound has already confirmed **absent fetal cardiac activity**, making repeated ultrasounds unnecessary as the diagnosis of IUFD is already established.
- This option would delay necessary management and exposure to the deceased fetus in utero could increase risks such as **coagulopathy** if prolonged.
*Perform dilation and curettage*
- **Dilation and curettage (D&C)** is generally reserved for termination of pregnancy or management of miscarriage up to **16-18 weeks' gestation**.
- At **26 weeks' gestation**, the size of the fetus and uterus makes D&C a less safe and less effective procedure compared to labor induction.
*Perform cesarean delivery*
- **Cesarean delivery** for IUFD is typically reserved for cases with maternal indications (e.g., prior classical C-section scar, placenta previa obstructing the birth canal) or when labor induction fails.
- There are no maternal or fetal contraindications to vaginal delivery in this scenario, and a C-section would primarily increase maternal morbidity without fetal benefit.
*Administer magnesium sulfate*
- **Magnesium sulfate** is used for **neuroprotection** in preterm deliveries (usually before 32 weeks) and seizure prophylaxis in **preeclampsia/eclampsia**.
- As the fetus is deceased, neuroprotection is not applicable, and there are no signs of preeclampsia, making this intervention inappropriate.
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 3: A 32-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the emergency department because of vaginal bleeding for the past hour. The patient reports that she felt contractions prior to the onset of the bleeding, but the contractions stopped after the bleeding started. She also has severe abdominal pain. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 110/min, respirations are 17/min, and blood pressure is 90/60 mm Hg. Examination shows diffuse abdominal tenderness with no rebound or guarding; no contractions are felt. The fetal heart rate shows recurrent variable decelerations. Which of the following is the most likely diagnosis?
- A. Uterine inertia
- B. Amniotic fluid embolism
- C. Uterine rupture (Correct Answer)
- D. Vasa previa
- E. Abruptio placentae
Antepartum fetal surveillance (NST, BPP) Explanation: ***Uterine rupture***
- The patient's history of a prior **cesarean section**, sudden onset of **vaginal bleeding** and **severe abdominal pain**, resolution of contractions, and signs of **hypovolemic shock** (tachycardia, hypotension) coupled with fetal distress (variable decelerations) are highly indicative of uterine rupture.
- Diffuse abdominal tenderness without rebound or guarding, and no palpable contractions, are also consistent with rupture.
*Uterine inertia*
- This condition is characterized by **weak or uncoordinated uterine contractions** leading to prolonged labor, but it does not typically present with acute vaginal bleeding, sudden severe abdominal pain, or hypovolemic shock.
- Fetal distress in uterine inertia would more likely be due to prolonged labor rather than acute compromise following a sudden event.
*Amniotic fluid embolism*
- This is a rare, life-threatening obstetric emergency characterized by sudden **cardiovascular collapse, respiratory distress**, and **coagulopathy**, often occurring during labor or immediately postpartum.
- While it can cause fetal distress, vaginal bleeding and severe abdominal pain are not primary presenting symptoms.
*Vasa previa*
- Characterized by **painless vaginal bleeding** when fetal vessels within the membranes cross the internal cervical os, making them vulnerable to rupture during cervical dilation or amniotomy.
- The bleeding is typically fetal blood, and fetal distress occurs rapidly, but the mother would not experience severe abdominal pain or signs of hypovolemic shock unless the bleeding is substantial and prolonged.
*Abruptio placentae*
- This involves the **premature separation of the placenta**, causing painful vaginal bleeding, uterine tenderness, and frequent, strong contractions.
- While it can cause hypovolemic shock and fetal distress, the description of contractions stopping after bleeding started, along with a previous C-section scar, points more specifically to uterine rupture rather than an abruption.
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 4: A 29-year-old G1P0 female at 32 weeks gestation presents to the emergency department with vaginal bleeding. She has had minimal prenatal care to-date with only an initial visit with an obstetrician after a positive home pregnancy test. She describes minimal spotting that she noticed earlier today that has progressed to larger amounts of blood; she estimates 30 mL of blood loss. She denies any cramping, pain, or contractions, and she reports feeling continued movements of the baby. Ultrasound and fetal heart rate monitoring confirm the presence of a healthy fetus without any evidence of current or impending complications. The consulted obstetrician orders blood testing for Rh-status of both the mother as well as the father, who brought the patient to the hospital. Which of the following represents the best management strategy for this situation?
- A. After 28 weeks gestation, administration of RhoGAM will have no benefit
- B. If mother is Rh-positive and father is Rh-negative then administer RhoGAM
- C. If mother is Rh-negative and father is Rh-negative then administer RhoGAM
- D. If mother is Rh-negative and father is Rh-positive, RhoGAM administration is not needed
- E. If mother is Rh-negative and father is Rh-positive then administer RhoGAM (Correct Answer)
Antepartum fetal surveillance (NST, BPP) Explanation: ***If mother is Rh-negative and father is Rh-positive then administer RhoGAM***
- This combination creates a risk for **Rh incompatibility**, meaning the fetus could be Rh-positive and the mother's immune system could form antibodies against fetal red blood cells, which can harm the fetus in future pregnancies.
- **RhoGAM (Rh immunoglobulin)** administration prevents the mother from forming these antibodies when there's a risk of maternal-fetal blood mixing, as indicated by vaginal bleeding.
*After 28 weeks gestation, administration of RhoGAM will have no benefit*
- This statement is incorrect; **RhoGAM is routinely administered around 28 weeks gestation** as prophylaxis in Rh-negative mothers, even without bleeding episodes, to prevent sensitization.
- In cases of potential fetal-maternal hemorrhage, such as vaginal bleeding, RhoGAM is indicated regardless of gestational age beyond the first trimester.
*If mother is Rh-positive and father is Rh-negative then administer RhoGAM*
- This scenario does not pose a risk for **Rh incompatibility hemolytic disease of the newborn**, as the mother already possesses the Rh antigen.
- RhoGAM is specifically given to Rh-negative mothers to prevent their immune system from reacting to an Rh-positive fetus.
*If mother is Rh-negative and father is Rh-negative then administer RhoGAM*
- In this case, both parents are **Rh-negative**, meaning the fetus will also be Rh-negative.
- There is no risk of **Rh incompatibility** or sensitization, so RhoGAM administration is not indicated.
*If mother is Rh-negative and father is Rh-positive, RhoGAM administration is not needed*
- This statement is incorrect and represents a critical misunderstanding of **Rh incompatibility prophylaxis**.
- This specific genetic combination creates the highest risk for **Rh sensitization** during pregnancy, especially with events like vaginal bleeding, making RhoGAM administration essential.
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 5: A 24-year-old primigravida at 28 weeks gestation presents to the office stating that she “can’t feel her baby kicking anymore.” She also noticed mild-to-moderate vaginal bleeding. A prenatal visit a few days ago confirmed the fetal cardiac activity by Doppler. The medical history is significant for GERD, hypertension, and SLE. The temperature is 36.78°C (98.2°F), the blood pressure is 125/80 mm Hg, the pulse is 70/min, and the respiratory rate is 14/min. Which of the following is the next best step in evaluation?
- A. Confirmation of cardiac activity by Doppler (Correct Answer)
- B. Order platelet count, fibrinogen, PT and PTT levels
- C. Abdominal delivery
- D. Speculum examination
- E. Misoprostol
Antepartum fetal surveillance (NST, BPP) Explanation: ***Confirmation of cardiac activity by Doppler***
- The patient presents with **decreased fetal movement** and **vaginal bleeding** at 28 weeks, which are concerning signs for complications like **placental abruption** or **fetal demise**.
- The immediate priority is to assess **fetal viability** by confirming the presence of a **fetal heartbeat**, with **Doppler ultrasonography** being the quickest and most accessible method.
*Order platelet count, fibrinogen, PT and PTT levels*
- While **coagulation studies** are important in cases of significant vaginal bleeding, especially if **placental abruption** is suspected, they are not the *next best step*.
- Assessing **fetal well-being** takes precedence, as the presence or absence of a **fetal heart rate** will guide subsequent emergency management.
*Abdominal delivery*
- **Abdominal delivery (C-section)** is a definitive intervention and should only be considered *after* an immediate assessment of **fetal status** and maternal stability.
- Delivery at 28 weeks gestation would be considered **preterm**, and careful evaluation is needed before making such a critical decision.
*Speculum examination*
- A **speculum examination** is used to investigate the source of vaginal bleeding, assess the cervix, and rule out causes such as **cervical lesions** or **cervical dilation**.
- However, given the *decreased fetal movement* and the potential for severe obstetrical emergencies, **fetal viability** must be confirmed first.
*Misoprostol*
- **Misoprostol** is a **prostaglandin analog** used to induce cervical ripening and uterine contractions, primarily for **labor induction** or **abortion**.
- It is not indicated as an initial diagnostic or therapeutic step in a patient with *decreased fetal movement* and *vaginal bleeding* without a clear diagnosis or indication for delivery.
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 6: A 26-year-old G1P0 female who is 39 weeks pregnant presents to the emergency department in labor. She reports following her primary care physician’s recommendations throughout her pregnancy and has not had any complications. During delivery, the baby’s head turtled back into the vaginal canal and did not advance any further. The neonatal intensivist was called for shoulder dystocia and a baby girl was able to be delivered vaginally 6 minutes later. Upon initial assessment, the baby appeared pale throughout, had her arms and legs flexed without active motion, and had some flexion of extremities when stimulated. Her pulse is 120/min and had irregular respirations. What is this baby’s initial APGAR score?
- A. 5 (Correct Answer)
- B. 6
- C. 7
- D. 4
- E. 3
Antepartum fetal surveillance (NST, BPP) Explanation: ***5***
- The APGAR score is calculated based on five criteria: **Appearance**, **Pulse**, **Grimace**, **Activity**, and **Respiration**.
- This baby's score is calculated as follows: **Appearance** (pale all over) = 0, **Pulse** (120/min) = 2, **Grimace** (some flexion of extremities with stimulation) = 1, **Activity** (arms and legs flexed without active motion) = 1, and **Respiration** (irregular) = 1.
- Total score: 0 + 2 + 1 + 1 + 1 = **5 points**
- A score of 5 indicates **moderate neonatal compromise** requiring close monitoring and possible intervention.
*4*
- A score of 4 would indicate more severe compromise, such as absent respirations (0 points) rather than irregular respirations (1 point).
- This baby has irregular respirations present, which earns 1 point, not 0 points.
*6*
- A score of 6 would require improvement in at least one category, such as **acrocyanosis** (blue extremities but pink body = 1 point for appearance) instead of pallor throughout.
- This baby's complete pallor limits the score to 5.
*7*
- A score of 7 or higher is generally considered reassuring and indicates a **healthy transition** from intrauterine to extrauterine life.
- This baby's concerning signs, including **complete pallor**, **irregular respirations**, and **poor muscle tone**, are inconsistent with a score of 7.
*3*
- A score of 3 would indicate severe depression with findings such as **heart rate less than 100 bpm**, completely absent reflexes, or flaccid muscle tone.
- This baby has a reassuring pulse of 120/min (2 points), some reflex response (1 point), and some muscle tone (1 point), making the total score higher than 3.
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 7: A student health coordinator plans on leading a campus-wide HIV screening program that will be free for the entire undergraduate student body. The goal is to capture as many correct HIV diagnoses as possible with the fewest false positives. The coordinator consults with the hospital to see which tests are available to use for this program. Test A has a sensitivity of 0.92 and a specificity of 0.99. Test B has a sensitivity of 0.95 and a specificity of 0.96. Test C has a sensitivity of 0.98 and a specificity of 0.93. Which of the following testing schemes should the coordinator pursue?
- A. Test A on the entire student body followed by Test B on those who are positive
- B. Test A on the entire student body followed by Test C on those who are positive
- C. Test C on the entire student body followed by Test B on those who are positive
- D. Test C on the entire student body followed by Test A on those who are positive (Correct Answer)
- E. Test B on the entire student body followed by Test A on those who are positive
Antepartum fetal surveillance (NST, BPP) Explanation: ***Test C on the entire student body followed by Test A on those who are positive***
- To "capture as many correct HIV diagnoses as possible" (maximize true positives), the initial screening test should have the **highest sensitivity**. Test C has the highest sensitivity (0.98).
- To "capture as few false positives as possible" (maximize true negatives and confirm diagnoses), the confirmatory test should have the **highest specificity**. Test A has the highest specificity (0.99).
*Test A on the entire student body followed by Test B on those who are positive*
- Starting with Test A (sensitivity 0.92) would miss more true positive cases than starting with Test C (sensitivity 0.98), failing the goal of **capturing as many cases as possible**.
- Following with Test B (specificity 0.96) would result in more false positives than following with Test A (specificity 0.99).
*Test A on the entire student body followed by Test C on those who are positive*
- This scheme would miss many true positive cases initially due to Test A's lower sensitivity compared to Test C.
- Following with Test C would introduce more false positives than necessary, as it has a lower specificity (0.93) than Test A (0.99).
*Test C on the entire student body followed by Test B on those who are positive*
- While Test C is a good initial screen for its high sensitivity, following it with Test B (specificity 0.96) is less optimal than Test A (specificity 0.99) for minimizing false positives in the confirmation step.
- This combination would therefore yield more false positives in the confirmatory stage than using Test A.
*Test B on the entire student body followed by Test A on those who are positive*
- Test B has a sensitivity of 0.95, which is lower than Test C's sensitivity of 0.98, meaning it would miss more true positive cases at the initial screening stage.
- While Test A provides excellent specificity for confirmation, the initial screening step is suboptimal for the goal of capturing as many diagnoses as possible.
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 8: A 30-year-old primigravida schedules an appointment with her obstetrician for a regular check-up. She says that everything is fine, although she reports that her baby has stopped moving as much as previously. She is 22 weeks gestation. She denies any pain or vaginal bleeding. The obstetrician performs an ultrasound and also orders routine blood and urine tests. On ultrasound, there is no fetal cardiac activity or movement. The patient is asked to wait for 1 hour, after which the scan is to be repeated. The second scan shows the same findings. Which of the following is the most likely diagnosis?
- A. Missed abortion
- B. Ectopic pregnancy
- C. Complete abortion
- D. Fetal demise (Correct Answer)
- E. Incomplete abortion
Antepartum fetal surveillance (NST, BPP) Explanation: ***Fetal demise***
- The absence of fetal cardiac activity and movement on repeated ultrasound scans at 22 weeks' gestation, after previously reporting fetal movement, is consistent with **fetal demise**.
- **Fetal demise** refers to the death of a fetus in utero at or after 20 weeks of gestation, or when the fetus weighs 350 grams or more.
*Missed abortion*
- **Missed abortion** (or missed miscarriage) is typically defined as a non-viable intrauterine pregnancy with a retained fetus or embryo without cardiac activity before 20 weeks of gestation.
- The patient is 22 weeks gestation, which places the condition beyond the general definition of a missed abortion.
*Ectopic pregnancy*
- In an **ectopic pregnancy**, the fertilized egg implants outside the uterus, most commonly in the fallopian tube, and would not have reached 22 weeks with reported fetal movement.
- An ectopic pregnancy would present with earlier symptoms like **abdominal pain** and **vaginal bleeding**, and an ultrasound would show an empty uterus or evidence of extrauterine pregnancy.
*Complete abortion*
- A **complete abortion** involves the complete expulsion of all products of conception from the uterus.
- This would be characterized by **heavy vaginal bleeding** and the passage of tissue, which the patient denies.
*Incomplete abortion*
- An **incomplete abortion** occurs when some, but not all, products of conception have been expelled from the uterus.
- Similar to complete abortion, an incomplete abortion would typically involve **vaginal bleeding** and retained tissue, accompanied by **cramping**, which are absent in this case.
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 9: A 30-year-old G3P0 woman who is 28 weeks pregnant presents for a prenatal care visit. She reports occasionally feeling her baby move but has not kept count over the past couple weeks. She denies any bleeding, loss of fluid, or contractions. Her previous pregnancies resulted in spontaneous abortions at 12 and 14 weeks. She works as a business executive, has been in excellent health, and has had no surgeries. She states that she hired a nutritionist and pregnancy coach to ensure good prospects for this pregnancy. On physical exam, fetal heart tones are not detected. Abdominal ultrasound shows a 24-week fetal demise. The patient requests an autopsy on the fetus and wishes for the fetus to pass "as naturally as possible." What is the best next step in management?
- A. Induction of labor now (Correct Answer)
- B. Dilation and evacuation
- C. Dilation and curettage
- D. Induction of labor at term
- E. Caesarean delivery
Antepartum fetal surveillance (NST, BPP) Explanation: ***Induction of labor now***
- With a confirmed **fetal demise at 28 weeks**, induction of labor is the most appropriate and respectful approach, allowing the patient's request to pass "as naturally as possible" to be honored and initiating the grieving process.
- Delaying labor induction can lead to increased risks of **coagulopathy** (disseminated intravascular coagulation) due to retained fetal tissue, and also prolonged emotional distress for the patient.
*Dilation and evacuation*
- While D&E is a common method for second-trimester termination or fetal demise, it is typically performed earlier in pregnancy (up to 24 weeks) and may not align with the patient's wish for the fetus to pass "as naturally as possible" for a 28-week demise.
- Given the patient's strong emotional investment in this pregnancy and desire for an autopsy, a D&E might be perceived as less respectful or less natural than labor induction.
*Dilation and curettage*
- **Dilation and curettage (D&C)** is primarily used for first-trimester miscarriages or early second-trimester procedures and is not suitable for a 28-week fetal demise due to the size of the fetus.
- Performing a D&C at this gestational age would be technically difficult and carry a higher risk of complications, including uterine perforation.
*Induction of labor at term*
- Waiting until term for a known fetal demise at 28 weeks is medically inappropriate and dangerous due to the significant risk of **disseminated intravascular coagulation (DIC)** developing from retained fetal tissue.
- Prolonged retention of a deceased fetus also significantly increases the emotional and psychological burden on the patient.
*Caesarean delivery*
- **Caesarean delivery** is generally reserved for live births where there is a medical indication for surgical delivery or in cases of an intact dilation and extraction procedure which is not typically first line for fetal demise at this gestation.
- Performing a C-section for a fetal demise offers no benefit to the fetus and carries unnecessary surgical risks for the mother, including infection, hemorrhage, and complications in future pregnancies.
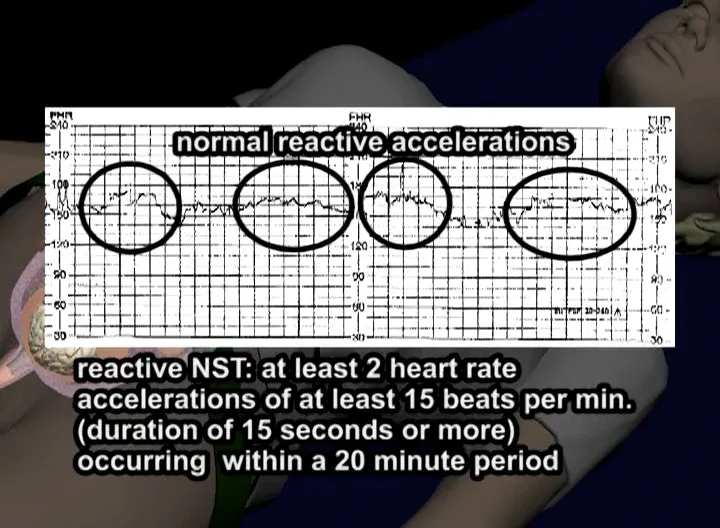
Antepartum fetal surveillance (NST, BPP) US Medical PG Question 10: A 30-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the hospital for regular, painful contractions that have been increasing in frequency. Her pregnancy has been complicated by gestational diabetes treated with insulin. Pelvic examination shows the cervix is 50% effaced and 4 cm dilated; the vertex is at -1 station. Ultrasonography shows no abnormalities. A tocometer and Doppler fetal heart monitor are placed on the patient's abdomen. The fetal heart rate monitoring strip shows a baseline heart rate of 145/min with a variability of ≥ 15/min. Within a 20-minute recording, there are 7 uterine contractions, 4 accelerations, and 3 decelerations that have a nadir occurring within half a minute. The decelerations occur at differing intervals relative to the contractions. Which of the following is the most appropriate next step in the management of this patient?
- A. Vibroacoustic stimulation
- B. Routine monitoring (Correct Answer)
- C. Administer tocolytics
- D. Emergent cesarean delivery
- E. Placement of fetal scalp electrode
Antepartum fetal surveillance (NST, BPP) Explanation: ***Routine monitoring***
- The presented FHR tracing exhibits a **normal baseline rate** (145/min), **moderate variability** (≥15/min), and the presence of **accelerations**, indicating a reassuring fetal status.
- The described decelerations are **variable decelerations** due to their sudden onset, nadir within 30 seconds, and variable relationship to contractions, which are generally benign unless prolonged, deep, or repetitive. Given the otherwise reassuring status, continued routine monitoring is appropriate.
*Vibroacoustic stimulation*
- This intervention is used to elicit **fetal accelerations** or movement during non-stress tests (NSTs) when the fetus is quiet or shows a non-reactive pattern.
- In this case, the fetus is already showing **accelerations** and moderate variability, so stimulation is not needed to assess fetal well-being.
*Administer tocolytics*
- **Tocolytics** are used to stop or slow down labor, typically in cases of preterm labor or uterine tachysystole causing fetal distress.
- This patient is at **38 weeks' gestation** and in active labor, and there are no signs of fetal distress warranting the cessation of contractions.
*Emergent cesarean delivery*
- **Emergent cesarean delivery** is indicated for acute fetal distress, such as prolonged decelerations, significant bradycardia, or absent variability in conjunction with other concerning FHR patterns.
- The FHR tracing described is largely reassuring with moderate variability and accelerations, and the variable decelerations are not indicative of immediate threat, making emergent delivery unnecessary.
*Placement of fetal scalp electrode*
- A **fetal scalp electrode** provides a more accurate and continuous measure of the FHR, often used when external monitoring is difficult or when there are concerns about the reliability of the tracing.
- While it can be useful in some situations, the current tracing is **interpretable as reassuring**, making invasive monitoring currently unnecessary.
More Antepartum fetal surveillance (NST, BPP) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.