Anemia in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Anemia in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Anemia in pregnancy US Medical PG Question 1: A 25-year-old African-American woman visits the doctor’s office complaining of fatigue for a couple of months. She says that she feels exhausted by the end of the day. She works as a dental assistant and is on her feet most of the time. However, she eats well and also tries to walk for 30 minutes every morning. She also says that she sometimes feels breathless and has to gasp for air, especially when she is walking or jogging. Her past medical history is insignificant, except for occasional bouts of cold during the winters. Her physical exam findings are within normal limits except for moderate conjunctival pallor. Complete blood count results and iron profile are as follows:
Hemoglobin 9 g/dL
Hematocrit 28.5%
RBC count 5.85 x 106/mm3
WBC count 5,500/mm3
Platelet count 212,000/mm3
MCV 56.1 fl
MCH 20.9 pg/cell
MCHC 25.6 g/dL
RDW 11.7% Hb/cell
Serum iron 170 mcg/dL
Total iron-binding capacity (TIBC) 458 mcg/dL
Transferrin saturation 60%
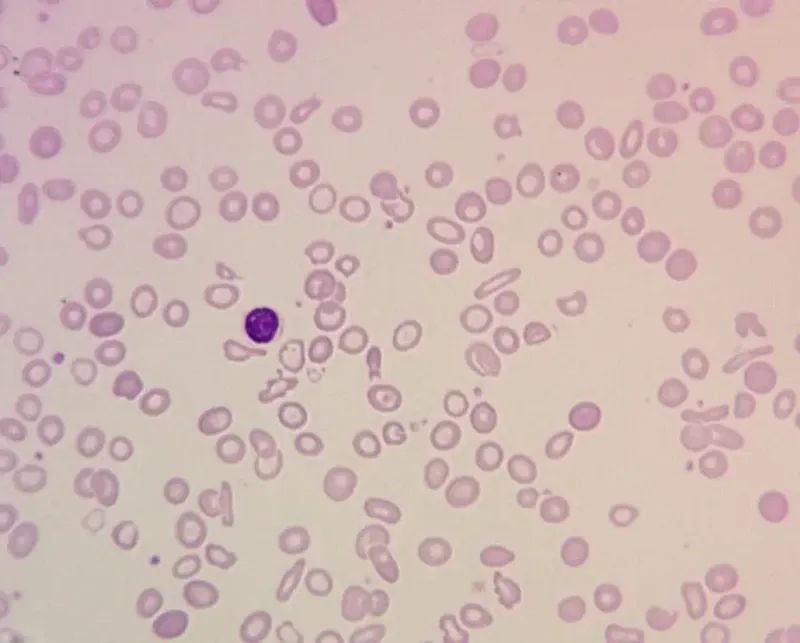
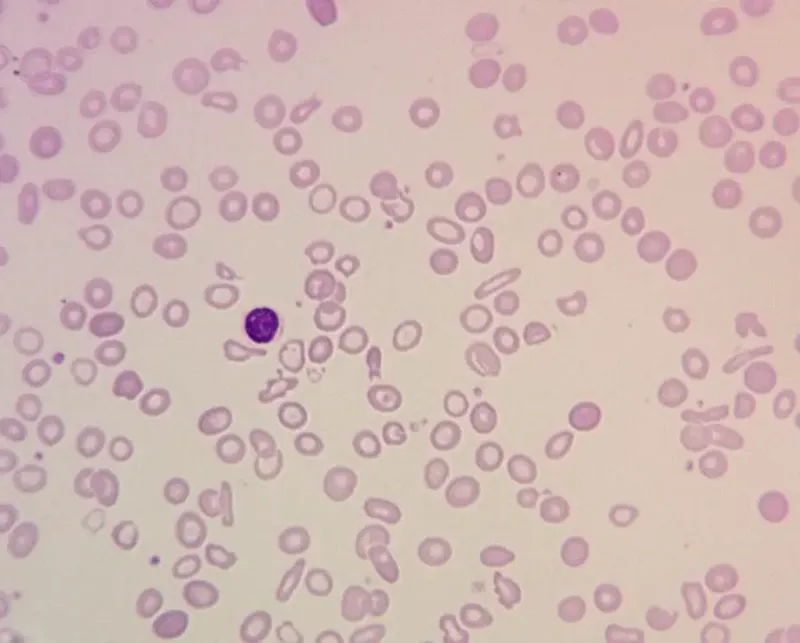
A peripheral blood smear is given. When questioned about her family history of anemia, she says that all she remembers is her dad was never allowed to donate blood as he was anemic. Which of the following most likely explains her cell counts and blood smear results?
- A. Thalassemia (Correct Answer)
- B. Iron-deficiency anemia
- C. B12 deficiency
- D. Hemolysis
- E. Folate deficiency
Anemia in pregnancy Explanation: ***Thalassemia***
- The patient presents with **microcytic, hypochromic anemia** (low MCV, MCH, MCHC) despite elevated iron stores, which is characteristic of thalassemia.
- The **elevated RBC count** (5.85 x 10^6/mm³) in the presence of anemia (hemoglobin 9 g/dL) is a hallmark of thalassemia, as the body attempts to compensate for ineffective erythropoiesis.
- The **elevated serum iron (170 mcg/dL) and high transferrin saturation (60%)** indicate iron overload, not iron deficiency, which occurs in thalassemia due to ineffective erythropoiesis and increased iron absorption.
- The **low RDW (11.7%)** indicates uniform cell size despite microcytosis, typical of thalassemia (vs. high RDW in iron deficiency).
- **Positive family history** (father was anemic and couldn't donate blood) supports an inherited disorder.
*Iron-deficiency anemia*
- This condition typically presents with **low serum iron**, **high TIBC**, and **low transferrin saturation** (<20%), which contradicts the patient's iron profile showing elevated iron and high transferrin saturation (60%).
- While iron-deficiency anemia also causes **microcytic, hypochromic RBCs**, the RBC count would be low or normal (not elevated), and RDW would be elevated (>14%) due to anisocytosis.
*B12 deficiency*
- **B12 deficiency** causes **macrocytic anemia** (high MCV >100 fl), which is inconsistent with the patient's low MCV (56.1 fl).
- It also often presents with neurological symptoms (peripheral neuropathy, subacute combined degeneration), which are absent in this case.
*Hemolysis*
- While hemolysis can cause anemia and fatigue, it is usually associated with elevated **reticulocyte count**, **indirect bilirubin**, and **LDH**, and decreased **haptoglobin**, none of which are indicated here.
- Hemolysis typically presents with **normocytic anemia** (normal MCV), not the marked **microcytosis** (MCV 56.1 fl) seen in this patient.
*Folate deficiency*
- Similar to B12 deficiency, **folate deficiency** leads to **macrocytic anemia** (high MCV >100 fl), which is not observed in this patient with MCV of 56.1 fl.
- Folate deficiency does not cause neurological symptoms (unlike B12 deficiency), but the **macrocytic** red cell morphology is the key differentiator here.
Anemia in pregnancy US Medical PG Question 2: A 61-year-old woman presents for a routine health visit. She complains of generalized fatigue and lethargy on most days of the week for the past 4 months. She has no significant past medical history and is not taking any medications. She denies any history of smoking or recreational drug use but states that she drinks "socially" approx. 6 nights a week. She says she also enjoys a "nightcap," which is 1–2 glasses of wine before bed every night. The patient is afebrile, and her vital signs are within normal limits. On physical examination, there is significant pallor of the mucous membranes. Laboratory findings are significant for a mean corpuscular volume (MCV) of 72 fL, leukocyte count of 4,800/mL, hemoglobin of 11.0 g/dL, and platelet count of 611,000/mL. Stool guaiac test is negative. She is started on oral ferrous sulfate supplements. On follow-up, her laboratory parameters show no interval change in her MCV or platelet level, and she reports good compliance with the medication. Which of the following is the best next step in the management of this patient?
- A. Transfuse the patient with whole blood
- B. Administer folate
- C. Administer iron intravenously (Correct Answer)
- D. Continue oral ferrous sulfate and supplement with omeprazole
- E. Continue oral ferrous sulfate and supplement with ascorbic acid
Anemia in pregnancy Explanation: **Administer iron intravenously**
- The patient shows **microcytic anemia** (MCV 72 fL) and **thrombocytosis** (platelet count 611,000/mL), which are classic signs of **iron deficiency anemia**.
- Given the failure of oral ferrous sulfate to improve her parameters, despite likely good adherence given the repeat visit, **intravenous iron** is the next appropriate step to ensure adequate iron repletion.
*Transfuse the patient with whole blood*
- **Blood transfusion** is reserved for patients with severe, symptomatic anemia, often with a hemoglobin level much lower than 11.0 g/dL, or in cases of acute hemorrhage.
- This patient's anemia is chronic and her hemoglobin level, while low, is not critically low enough to warrant immediate transfusion.
*Administer folate*
- **Folate deficiency** typically causes **macrocytic anemia** (high MCV), not microcytic anemia, making it an inappropriate treatment for this patient.
- Though chronic alcohol use can affect folate levels, the patient's presentation is more consistent with iron deficiency.
*Continue oral ferrous sulfate and supplement with omeprazole*
- **Omeprazole** is a **proton pump inhibitor** that can actually *reduce* iron absorption by decreasing gastric acidity, making it counterproductive in treating iron deficiency.
- Continuing oral iron alone was already proven ineffective, necessitating a more aggressive approach.
*Continue oral ferrous sulfate and supplement with ascorbic acid*
- **Ascorbic acid (vitamin C)** can enhance the absorption of non-heme iron; however, since the initial trial of oral ferrous sulfate alone was ineffective, merely adding ascorbic acid may not be sufficient.
- The lack of improvement suggests either poor absorption or significant ongoing loss, which intravenous iron addresses more directly.
Anemia in pregnancy US Medical PG Question 3: A 36-year-old primigravid woman who recently immigrated to the United States presents to her gynecologist for the first time during the 28th week of her pregnancy. She hasn’t received any prenatal care or folic acid supplementation. The patient’s history reveals that she has received blood transfusions in the past due to “severe anemia.” Which of the following blood type situations would put the fetus at risk for hemolytic disease of the newborn?
- A. Mother is AB negative, father is O negative
- B. Mother is O positive, father is B negative
- C. Mother is O positive, father is AB negative
- D. Mother is B positive, father is O negative
- E. Mother is A negative, father is B positive (Correct Answer)
Anemia in pregnancy Explanation: ***Mother is A negative, father is B positive***
- This scenario presents a risk for **Rh incompatibility** because the mother is Rh-negative and the father is Rh-positive, meaning the fetus could inherit the Rh-positive antigen.
- The mother's history of blood transfusions for "severe anemia" could also indicate prior exposure to Rh-positive blood, which would have sensitized her system and led to the production of anti-Rh antibodies, putting the fetus at higher risk for **hemolytic disease of the newborn (HDN)** during a subsequent pregnancy.
*Mother is AB negative, father is O negative*
- In this case, both parents are **Rh-negative**, so there is no risk of Rh incompatibility.
- While ABO incompatibility can occur, it is generally **less severe** than Rh incompatibility and usually does not cause severe hemolytic disease requiring transfusions.
*Mother is O positive, father is B negative*
- The mother is **Rh-positive**, which means there is no risk of Rh incompatibility with an Rh-negative father.
- Although there is a potential for **ABO incompatibility**, this is typically less concerning for severe HDN compared to Rh incompatibility, and the Rh factor is the primary concern here.
*Mother is O positive, father is AB negative*
- The mother is **Rh-positive**, so Rh incompatibility is not a risk.
- While there is a potential for **ABO incompatibility** (mother is O, father has A and B antigens), this form of HDN is generally milder and rarely requires clinical intervention.
*Mother is B positive, father is O negative*
- The mother is **Rh-positive**, eliminating the risk of Rh incompatibility.
- Potential for **ABO incompatibility** exists, but the more severe forms of HDN are typically associated with Rh incompatibility.
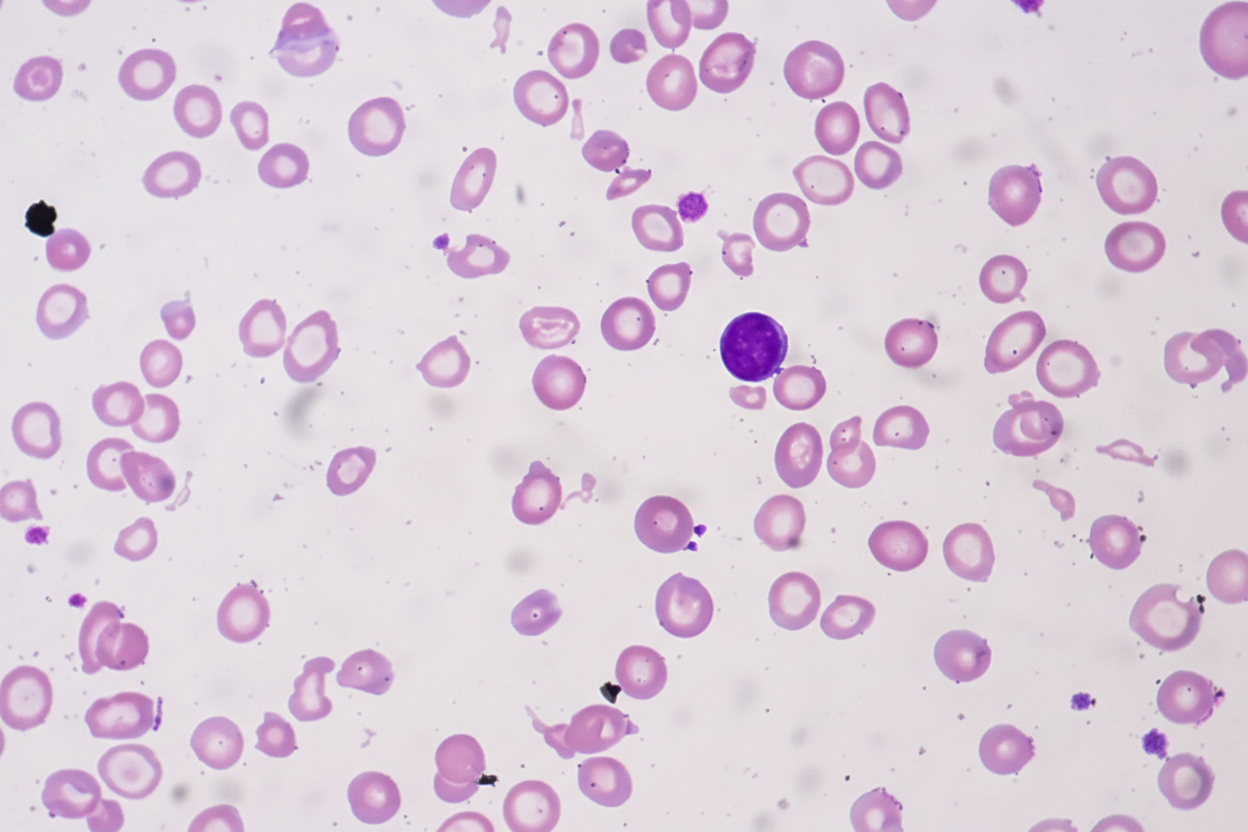
Anemia in pregnancy US Medical PG Question 4: A 36-year-old woman gravida 5, para 4 was admitted at 31 weeks of gestation with worsening fatigue and shortness of breath on exertion for the past month. She also has nausea and loss of appetite. No significant past medical history. The patient denies any smoking history, alcohol or illicit drug use. Her vital signs include: blood pressure 110/60 mm Hg, pulse 120/min, respiratory rate 22/min and temperature 35.1℃ (97.0℉). A complete blood count reveals a macrocytosis with severe pancytopenia, as follows:
Hb 7.2 g/dL
RBC 3.6 million/uL
WBC 4,400/mm3
Neutrophils 40%
Lymphocytes 20%
Platelets 15,000/mm3
MCV 104 fL
Reticulocytes 0.9%
Serum ferritin and vitamin B12 levels were within normal limits. There was an elevated homocysteine level and a normal methylmalonic acid level. Which of the following is the most likely diagnosis in this patient?
- A. Normal pregnancy
- B. Aplastic anemia
- C. Vitamin B12 deficiency
- D. Iron deficiency anemia
- E. Folate deficiency (Correct Answer)
Anemia in pregnancy Explanation: ***Folate deficiency***
- The patient presents with **macrocytic anemia** (MCV 104 fL), **pancytopenia**, and symptoms of severe anemia. The elevated **homocysteine** and normal **methylmalonic acid** levels are classic indicators of folate deficiency, as folate is required to convert homocysteine to methionine but not for MMA metabolism.
- Her status as **gravida 5, para 4** in the **third trimester** (31 weeks) significantly increases her risk for folate deficiency due to high fetal demands, even without poor nutritional intake.
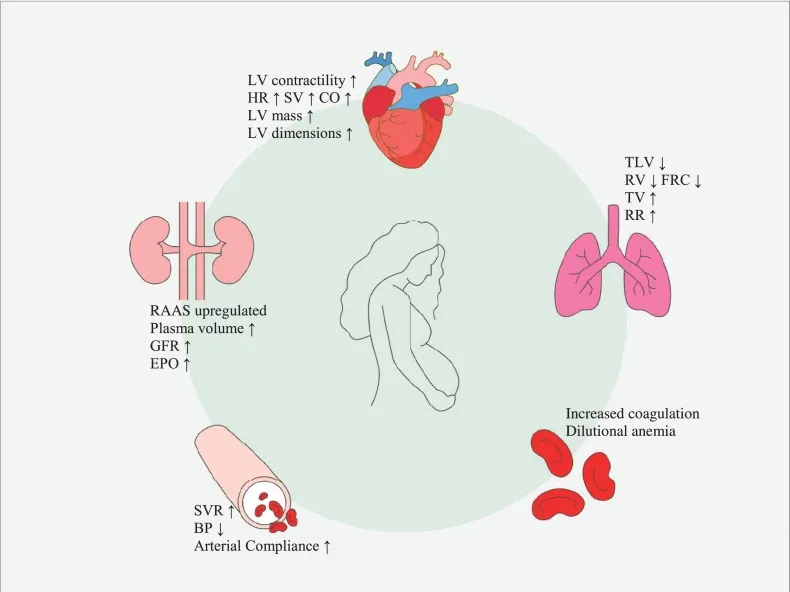
*Normal pregnancy*
- While **fatigue and shortness of breath** are common in pregnancy, severe **pancytopenia** and **macrocytosis (MCV 104)** are not normal physiological changes.
- Hemoglobin of 7.2 g/dL indicates severe anemia, far below the expected physiological decrease in Hb during pregnancy due to **hemodilution**.
*Aplastic anemia*
- Aplastic anemia is characterized by **pancytopenia** but typically presents with **normocytic or mildly macrocytic RBCs**, and there would be severe **reticulocytopenia** (which is present here, 0.9%).
- However, the distinct biochemical markers of elevated **homocysteine** and normal **methylmalonic acid** point more specifically towards a nutritional deficiency rather than bone marrow failure.
*Vitamin B12 deficiency*
- **Vitamin B12 deficiency** also causes **macrocytic anemia** and **pancytopenia**, with elevated **homocysteine levels**.
- However, a key differentiating factor is that **methylmalonic acid (MMA)** levels would also be **elevated** in B12 deficiency, which is normal in this patient.
*Iron deficiency anemia*
- **Iron deficiency anemia** is typically characterized by **microcytic, hypochromic** red blood cells (low MCV), not macrocytic.
- While it can cause fatigue and shortness of breath, the laboratory findings of a **normal ferritin** (suggesting adequate iron stores), **macrocytosis**, and **pancytopenia** do not fit with iron deficiency.
Anemia in pregnancy US Medical PG Question 5: A 34-year-old woman comes to a physician for a routine health maintenance examination. She moved to Denver 1 week ago after having lived in New York City all her life. She has no history of serious illness and takes no medications. Which of the following sets of changes is most likely on analysis of a blood sample obtained now compared to prior to her move?
Erythropoietin level | O2 saturation | Plasma volume
- A. ↑ unchanged unchanged
- B. ↑ ↓ ↓ (Correct Answer)
- C. Unchanged ↓ unchanged
- D. ↓ unchanged ↑
- E. Unchanged unchanged ↓
Anemia in pregnancy Explanation: ***↑ ↓ ↓***
- Moving to a high altitude like Denver (from sea level NYC) leads to **hypoxia**, which triggers increased **erythropoietin (EPO)** production to stimulate red blood cell formation.
- The immediate physiological response to high altitude is a **decrease in arterial PO2** and thus **oxygen saturation**, along with a **reduction in plasma volume** due to increased diuresis and fluid shifts.
*↑ unchanged unchanged*
- While **erythropoietin** would increase due to hypoxia at higher altitudes, **oxygen saturation** would decrease, not remain unchanged.
- **Plasma volume** also tends to decrease acutely at high altitudes, rather than staying unchanged.
*Unchanged ↓ unchanged*
- **Erythropoietin** would be expected to increase, not remain unchanged, as a compensatory mechanism to hypoxia.
- While **oxygen saturation** would decrease, **plasma volume** typically decreases acutely, not remaining unchanged.
*↓ unchanged ↑*
- **Erythropoietin** would increase, not decrease, in response to the lower atmospheric oxygen.
- Both **oxygen saturation** and **plasma volume** would decrease, not remain unchanged or increase, respectively.
*Unchanged unchanged ↓*
- **Erythropoietin** would increase, not remain unchanged, to stimulate red blood cell production in response to hypoxia.
- **Oxygen saturation** would decrease, not remain unchanged, at higher altitudes.
Anemia in pregnancy US Medical PG Question 6: A 27-year-old African-American woman, gravida 1, para 0, at 11 weeks' gestation comes to her physician for a prenatal visit. She feels more fatigued than usual but has no other symptoms. She has no history of serious illness. She takes no medications. Her mother has systemic lupus erythematosus. Her temperature is 37.2°C (98.9°F), pulse is 80/min, respirations are 18/min, and blood pressure is 120/75 mm Hg. Examination shows no abnormalities. Laboratory studies show:
Hemoglobin 9.2 g/dL
Hematocrit 27.5%
Leukocyte count 6,000/mm3
Platelet Count 180,000/mm3
MCV 74 μm3
MCH 24 pg/cell
Serum
Na+ 138 mEq/L
K+ 4.5 mEq/L
Cl- 100 mEq/L
HCO3- 25 mEq/L
Urea Nitrogen 15 mg/dL
Creatinine 1.0 mg/dL
Total Bilirubin 0.4 mg/dL
Iron 67 U/L
Ferritin 98 ng/mL
Which of the following is the most appropriate next step in management?
- A. Measure LDH and haptoglobin
- B. Hemoglobin electrophoresis (Correct Answer)
- C. Perform direct Coombs test
- D. Measure anticardiolipin antibody titers
- E. Amniocentesis
Anemia in pregnancy Explanation: **Hemoglobin electrophoresis**
- The patient's **microcytic anemia** (MCV 74) with normal ferritin suggests a diagnosis other than iron deficiency, such as a **hemoglobinopathy**, particularly given her African-American ethnicity and the possibility of **thalassemia** or **sickle cell trait**.
- **Prenatal screening for hemoglobinopathies** is crucial, and hemoglobin electrophoresis is the definitive test to identify different hemoglobin variants and diagnose conditions like **alpha and beta thalassemia traits** or **sickle cell trait**, which are important for genetic counseling and management during pregnancy.
*Measure LDH and haptoglobin*
- These tests are used to evaluate for **hemolytic anemia** (elevated LDH, low haptoglobin).
- While the patient has anemia, there are no other signs of hemolysis (e.g., elevated bilirubin, reticulocytosis, jaundice), and a primary focus should be on identifying the cause of the microcytic anemia before investigating hemolysis.
*Perform direct Coombs test*
- A direct Coombs test is used to detect **autoimmune hemolytic anemia**.
- There is no clinical or laboratory evidence to suggest an autoimmune hemolytic process (e.g., no spherocytes, no significant reticulocytosis, normal bilirubin).
*Measure anticardiolipin antibody titers*
- This test screens for **antiphospholipid syndrome**, which is associated with recurrent pregnancy loss and thrombosis.
- While her mother has SLE, which can be associated with antiphospholipid syndrome, the patient's primary presenting problem is unexplained microcytic anemia, not a history of pregnancy complications or thrombotic events.
*Amniocentesis*
- Amniocentesis is an invasive procedure used for **fetal genetic testing** and is typically performed later in pregnancy (15-20 weeks).
- There is no medical indication for amniocentesis at 11 weeks' gestation based on the current presentation; the immediate concern is diagnosing and managing the maternal anemia.
Anemia in pregnancy US Medical PG Question 7: A 43-year-old woman presents to her physician’s office complaining of fatigue and light headedness for one month. She has regular periods but notes that they have become heavier in the last year. She endorses increased urination and feels that she has gained weight in her abdomen, but review of systems is otherwise negative. She is a daycare teacher and has a first cousin with von Willebrand disease. Temperature is 98.4°F (36.9°C), pulse is 92/min, blood pressure is 109/72 mmHg, and respirations are 14/min.
A CBC demonstrates:
Hemoglobin: 9.9 g/dL
Leukocyte count: 6,300/mm^3
Platelet count: 180,000/mm^3
Which of the following is the best next step to evaluate the etiology of this patient’s findings?
- A. von Willebrand factor antigen
- B. TSH
- C. Parvovirus B19 IgM and IgG
- D. Hysteroscopy
- E. Pelvic ultrasound (Correct Answer)
Anemia in pregnancy Explanation: ***Pelvic ultrasound***
- This patient presents with **heavy menstrual bleeding (menorrhagia)**, symptoms of **anemia** (fatigue, lightheadedness), and abdominal distension/weight gain. These symptoms, particularly the abdominal weight gain and increased urination, strongly suggest a pelvic mass or uterine pathology, such as **leiomyomas (fibroids)**.
- A pelvic ultrasound is the initial, **non-invasive imaging modality** of choice to evaluate for uterine or adnexal pathology in women presenting with menorrhagia, pelvic pain, or suspected masses.
*von Willebrand factor antigen*
- While the patient has a **first cousin with von Willebrand disease** and experiences menorrhagia, a bleeding disorder is less likely to fully explain the **abdominal weight gain** and **increased urination**, which point more towards a mass effect.
- Labs for von Willebrand disease (vWF antigen, ristocetin cofactor activity, factor VIII activity) would be considered if a structural cause for bleeding is ruled out, or if there's a strong personal history of bleeding.
*TSH*
- **Hypothyroidism** can cause menorrhagia and fatigue, but it does not typically lead to significant **abdominal weight gain** attributable to an anatomical mass or increased urination from uterine pressure.
- While thyroid dysfunction can cause menstrual irregularities, the compressive symptoms make a primary uterine cause more likely.
*Parvovirus B19 IgM and IgG*
- **Parvovirus B19 infection** can cause anemia (particularly in individuals with underlying hematologic conditions) and fatigue, but it **does not explain menorrhagia** or the abdominal symptoms like weight gain and increased urination.
- This evaluation would be considered in cases of unexplained anemia, especially with known exposure or aplastic crisis, not as a primary evaluation for heavy menstrual bleeding and mass effect.
*Hysteroscopy*
- **Hysteroscopy** is a procedure to visualize the inside of the uterus and is often used to evaluate for **intrauterine pathologies** such as polyps or submucosal fibroids after initial imaging, like ultrasound, has identified or suggested such findings.
- It is an **invasive procedure** and not the **best initial step** compared to a non-invasive pelvic ultrasound to broadly evaluate the uterus and adnexa.
Anemia in pregnancy US Medical PG Question 8: A 27-year-old woman, gravida 2, para 1, at 36 weeks' gestation comes to the physician for a prenatal visit. She feels well. Fetal movements are adequate. This is her 7th prenatal visit. She had an ultrasound scan performed 1 month ago that showed a live intrauterine pregnancy consistent with a 32-week gestation with no anomalies. She had a Pap smear performed 1 year ago, which was normal. Vital signs are within normal limits. Pelvic examination shows a uterus consistent in size with a 36-week gestation. Her blood group and type is A negative. Which of the following is the most appropriate next step in management?
- A. Transabdominal doppler ultrasonography
- B. Rh antibody testing
- C. Swab for GBS culture (Correct Answer)
- D. Serum PAPP-A and HCG levels
- E. Complete blood count
Anemia in pregnancy Explanation: ***Swab for GBS culture***
- All pregnant women should be screened for **Group B Streptococcus (GBS)** between **36 weeks 0 days and 37 weeks 6 days** of gestation.
- A positive GBS culture requires **intrapartum antibiotic prophylaxis** to prevent early-onset neonatal GBS disease.
*Transabdominal doppler ultrasonography*
- **Doppler ultrasonography** is primarily used to assess **fetal well-being** in cases of **fetal growth restriction**, preeclampsia, or other high-risk conditions.
- This patient has a **normal-sized uterus** and **adequate fetal movements**, indicating no immediate need for fetal Doppler assessment.
*Rh antibody testing*
- **Rh antibody testing** (indirect Coombs test) is performed early in pregnancy for Rh-negative women and typically repeated at **28 weeks' gestation** before anti-D immune globulin administration.
- Repeating this test at 36 weeks is not the most appropriate *next* step as the routine schedule for Rh immune globulin would typically be managed prior to this point.
*Serum PAPP-A and HCG levels*
- **Serum PAPP-A and HCG levels** are components of **first-trimester screening** for chromosomal abnormalities, performed between 11 and 14 weeks of gestation.
- At 36 weeks' gestation, these markers are not relevant for current fetal assessment.
*Complete blood count*
- A **complete blood count (CBC)** is routinely performed in the first trimester and often repeated in the **late second or early third trimester** (around 28 weeks) to check for anemia.
- While a CBC might be done as part of general prenatal care, it is not the most urgent or specifically indicated test at 36 weeks in the absence of symptoms.
Anemia in pregnancy US Medical PG Question 9: A 29-year-old G1P0 presents to her obstetrician for her first prenatal care visit at 12 weeks gestation by last menstrual period. She states that her breasts are very tender and swollen, and her exercise endurance has declined. She otherwise feels well. She is concerned about preterm birth, as she heard that certain cervical procedures increase the risk. The patient has a gynecologic history of loop electrosurgical excision procedure (LEEP) for cervical dysplasia several years ago and has had negative Pap smears since then. She also has mild intermittent asthma that is well controlled with occasional use of her albuterol inhaler. At this visit, this patient’s temperature is 98.6°F (37.0°C), pulse is 69/min, blood pressure is 119/61 mmHg, and respirations are 13/min. Cardiopulmonary exam is unremarkable, and the uterine fundus is just palpable at the pelvic brim. Pelvic exam reveals normal female external genitalia, a closed and slightly soft cervix, a 12-week-size uterus, and no adnexal masses. Which of the following is the best method for evaluating for possible cervical incompetence in this patient?
- A. Transabdominal ultrasound in the first trimester
- B. Transvaginal ultrasound in the first trimester
- C. Serial transvaginal ultrasounds starting at 16 weeks gestation
- D. Transabdominal ultrasound at 18 weeks gestation
- E. Transvaginal ultrasound at 18 weeks gestation (Correct Answer)
Anemia in pregnancy Explanation: ***Transvaginal ultrasound at 18 weeks gestation***
- A history of **LEEP** is a risk factor for **cervical incompetence** and warrants screening with transvaginal ultrasound.
- The optimal timing for **cervical length** screening in women with a history of cervical procedures is typically between **18 and 24 weeks gestation**, as the risk of cervical shortening usually manifests during this period.
*Transabdominal ultrasound in the first trimester*
- **Transabdominal ultrasound** is generally not ideal for precise **cervical length measurement** due to potential shadowing from the fetus or maternal obesity.
- **First-trimester cervical length measurement** is not typically recommended for routine screening of cervical incompetence, as changes are less pronounced early in pregnancy.
*Transvaginal ultrasound in the first trimester*
- While more accurate than transabdominal, **first-trimester transvaginal ultrasound** for cervical length is not standard for predicting cervical incompetence.
- Significant cervical shortening due to incompetence often occurs later in the second trimester, so early screening may miss the condition.
*Serial transvaginal ultrasounds starting at 16 weeks gestation*
- While **serial transvaginal ultrasounds** starting at 16 weeks can be part of a management plan for high-risk patients, the most critical single assessment typically occurs at **18-24 weeks**.
- Starting serial scans too early may not be necessary if the cervix is long and closed at the initial key screening, unless there are other strong indications.
*Transabdominal ultrasound at 18 weeks gestation*
- Similar to first-trimester transabdominal ultrasound, **transabdominal imaging** at 18 weeks is generally **less accurate** than transvaginal for measuring cervical length.
- **Transvaginal ultrasound** offers a clearer and more precise view of the cervix, which is crucial for assessing potential shortening or funneling.
Anemia in pregnancy US Medical PG Question 10: A 26-year-old woman presents to the women’s health clinic with a 9-week delay in menses. The patient has a history of grand mal seizures, and was recently diagnosed with acute sinusitis. She is prescribed lamotrigine and amoxicillin. The patient smokes one-half pack of cigarettes every day for 10 years, and drinks socially a few weekends every month. Her mother died of breast cancer when she was 61 years old. The vital signs are stable during the current office visit. Physical examination is grossly normal. The physician orders a urine beta-hCG that comes back positive. Abdominal ultrasound shows an embryo consistent in dates with the first day of last menstrual period. Given the history of the patient, which of the following would most likely decrease congenital malformations in the newborn?
- A. Decrease alcohol consumption
- B. Switching to cephalexin
- C. Folic acid supplementation (Correct Answer)
- D. Smoking cessation
- E. Switching to another antiepileptic medication
Anemia in pregnancy Explanation: ***Folic acid supplementation***
- **Folic acid** (vitamin B9) is crucial in early pregnancy for **neural tube development** and significantly reduces the risk of **neural tube defects** and other congenital malformations.
- Given the patient’s history of **lamotrigine** use, which can increase the risk of neural tube defects, folic acid supplementation is even more critical.
*Decrease alcohol consumption*
- While **alcohol cessation** is important to prevent **fetal alcohol syndrome** and other alcohol-related developmental issues, it primarily affects neurological development and facial dysmorphology rather than primarily preventing
- The effects of alcohol are typically more pronounced with **chronic heavy consumption**, and while any reduction is beneficial, it is not the most likely intervention to decrease general congenital malformations.
*Switching to cephalexin*
- **Amoxicillin** is considered **safe in pregnancy** and is a penicillin-class antibiotic, while **cephalexin** is a cephalosporin.
- Switching antibiotics from one safe drug to another without a clear medical indication (e.g., allergy, resistance) would **not decrease the risk of congenital malformations**.
*Smoking cessation*
- **Smoking cessation** is vital during pregnancy as it reduces the risk of **low birth weight**, **preterm birth**, and other complications like placental abruption.
- However, the primary link of smoking is not directly with **congenital malformations** like neural tube defects, but rather with growth restriction and adverse perinatal outcomes.
*Switching to another antiepileptic medication*
- This patient is on **lamotrigine**, which is considered one of the **safer antiepileptic drugs (AEDs)** in pregnancy, especially compared to others like **valproic acid**.
- Switching to an alternative AED might even carry a **higher risk for congenital malformations** and is generally not recommended unless lamotrigine is ineffective or contraindicated.
More Anemia in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.