Prenatal Care

On this page
🏥 The Prenatal Care Command Center: Orchestrating Optimal Outcomes
Prenatal care transforms pregnancy from a biological event into a strategically managed journey where early detection, risk stratification, and evidence-based interventions dramatically reduce maternal and fetal morbidity. You'll master how to build a comprehensive surveillance system that identifies high-risk patients, deploys targeted screening protocols, confirms diagnoses with precision, and orchestrates multi-system care networks. This lesson equips you with the clinical algorithms and decision frameworks that separate routine monitoring from life-saving intervention, ensuring you can confidently guide every pregnancy toward optimal outcomes.
📌 Remember: CARE - Continuous monitoring, Assessment protocols, Risk stratification, Early intervention
The prenatal care framework encompasses three phases of pregnancy management:
-
Preconceptional Phase (3-6 months before conception)
- Folic acid supplementation: 400-800 mcg daily
- Chronic disease optimization: HbA1c <7% for diabetics
- Immunization updates: MMR, Tdap, influenza
- Genetic counseling for high-risk couples
- Lifestyle modification: smoking cessation, alcohol elimination
- Weight optimization: BMI 18.5-24.9 kg/m² ideal
-
Antepartum Phase (conception through 37 weeks)
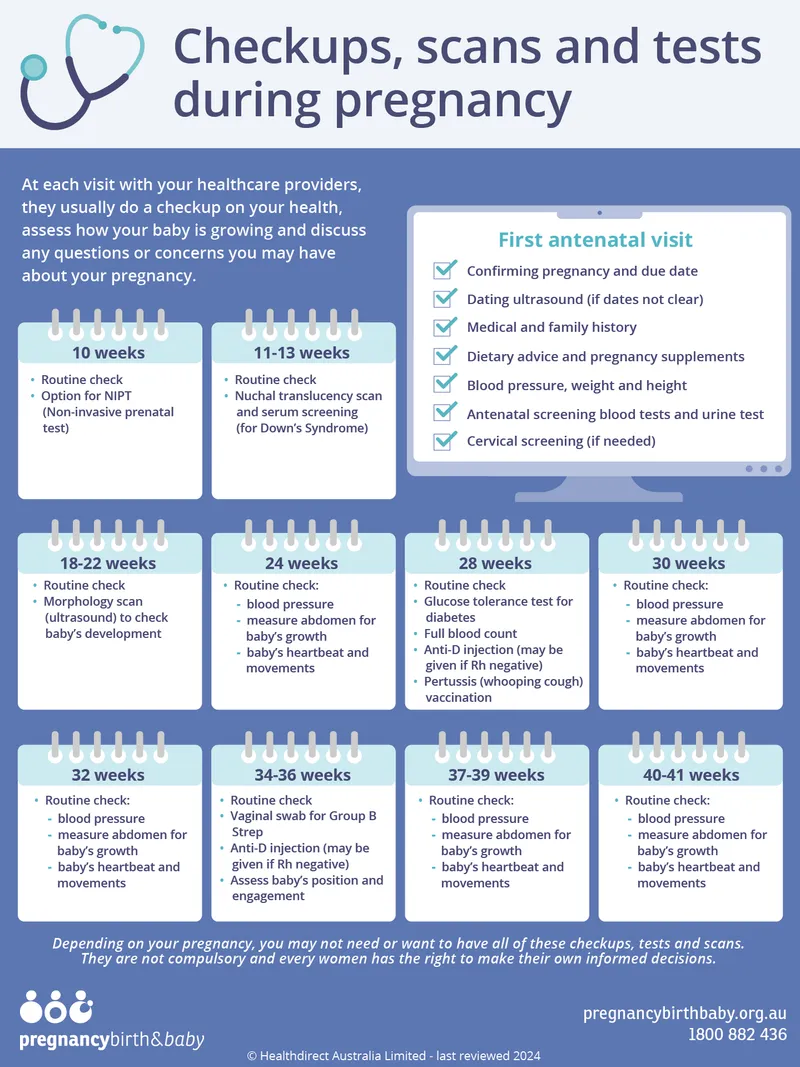
- Regular visit schedule: every 4 weeks until 28 weeks
- Biweekly visits: 28-36 weeks gestation
- Weekly visits: 36 weeks until delivery
- Maternal weight gain monitoring: 25-35 lbs for normal BMI
- Fetal growth assessment: EFW 10th-90th percentile
- Laboratory surveillance: CBC, urinalysis, glucose screening
-
Intrapartum Preparation (37-42 weeks)
- Cervical ripening assessment: Bishop score >8
- Fetal lung maturity confirmation: lecithin:sphingomyelin ratio >2:1
- Birth plan finalization and emergency preparedness
| Visit Type | Timing | Key Assessments | Critical Thresholds | Intervention Triggers |
|---|---|---|---|---|
| Initial | 8-12 weeks | Complete H&P, labs, dating | BP >140/90, proteinuria >300mg | Hypertension workup |
| Routine | Every 4 weeks | Weight, BP, fundal height, FHR | Weight gain >2 lbs/week | Preeclampsia screening |
| Glucose Screen | 24-28 weeks | 1-hour GTT | >140 mg/dL | 3-hour GTT |
| Group B Strep | 35-37 weeks | Vaginal-rectal culture | Positive culture | Intrapartum antibiotics |
| Term Assessment | 37+ weeks | Cervical exam, fetal presentation | Bishop score >8 | Labor readiness |
💡 Master This: The "Rule of 4s" governs prenatal visit frequency-every 4 weeks until 28 weeks, then every 2 weeks until 36 weeks, then weekly. This schedule captures 95% of pregnancy complications when combined with appropriate screening protocols.
Understanding this systematic approach to prenatal care establishes the foundation for recognizing normal pregnancy progression and identifying deviations that require intervention. Connect this framework through comprehensive risk assessment to understand how individual patient factors modify standard care protocols.
🏥 The Prenatal Care Command Center: Orchestrating Optimal Outcomes
🎯 Risk Stratification Matrix: Precision Pregnancy Profiling
📌 Remember: RISC - Review history, Identify factors, Stratify risk, Customize care
The risk stratification framework evaluates four domains of pregnancy risk:
-
Maternal Medical Factors (chronic conditions affecting pregnancy)
- Diabetes mellitus: Type 1/2 requires HbA1c <7%, q2-week visits
- Chronic hypertension: BP >140/90 pre-pregnancy, weekly BP monitoring
- Autoimmune disorders: SLE, APS require monthly labs, serial growth scans
- Cardiac disease: NYHA Class III-IV contraindication to pregnancy
- Renal disease: creatinine >1.4 mg/dL increases preeclampsia risk 5-fold
- Thrombophilia: Factor V Leiden requires anticoagulation protocols
-
Obstetric History Factors (prior pregnancy complications)
- Previous preeclampsia: recurrence risk 15-25%, low-dose aspirin 81mg
- Prior preterm birth: recurrence risk 30-40%, progesterone supplementation
- Pregnancy loss: ≥2 losses warrant thrombophilia workup
- Previous cesarean: VBAC success rate 70-80% with appropriate selection
- Gestational diabetes: recurrence risk 35-70%, early glucose screening
- Fetal growth restriction: recurrence risk 20-25%, serial biometry
-
Current Pregnancy Factors (present pregnancy complications)
- Multiple gestation: preterm delivery risk 50-60% for twins
- Placental abnormalities: placenta previa 0.5% incidence, bleeding risk
- Fetal anomalies: 2-3% major anomalies, genetic counseling indicated
-
Social Risk Factors (environmental and behavioral risks)
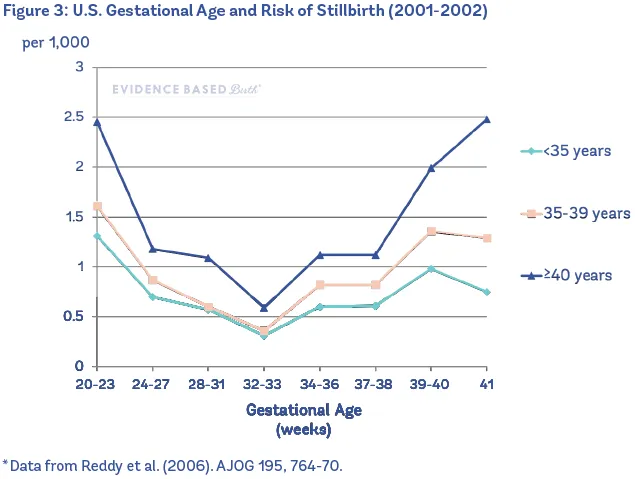
- Maternal age: <18 years or >35 years increases complications
- Substance use: smoking reduces birth weight 200-300g
- Domestic violence: affects 4-8% of pregnancies, screening mandatory
| Risk Category | Surveillance Frequency | Specialist Referrals | Additional Testing | Delivery Planning |
|---|---|---|---|---|
| Low Risk | Standard schedule | None required | Routine screening only | Term delivery 39-41 weeks |
| Moderate Risk | Every 2-3 weeks | MFM consultation | Serial growth scans | Delivery 37-39 weeks |
| High Risk | Weekly visits | MFM co-management | Biweekly NSTs, BPPs | Delivery 34-37 weeks |
| Critical Risk | Twice weekly | Tertiary center transfer | Daily fetal monitoring | Delivery <34 weeks |
💡 Master This: Risk stratification is dynamic-patients can move between categories as pregnancy progresses. A low-risk patient developing gestational hypertension at 32 weeks immediately becomes high-risk requiring weekly visits and twice-weekly NSTs.
This precision profiling approach enables clinicians to allocate resources efficiently while ensuring high-risk patients receive appropriate intensive monitoring. Connect this risk framework through evidence-based screening protocols to understand how specific tests and interventions reduce identified risks.
🎯 Risk Stratification Matrix: Precision Pregnancy Profiling
🔬 Screening Protocol Arsenal: Evidence-Based Detection Systems
📌 Remember: SCREEN - Systematic timing, Combined markers, Risk assessment, Early detection, Evidence-based, Normal variants
The comprehensive screening framework operates through four sequential phases:
-
First Trimester Screening (11-14 weeks)
- Combined screening: NT + PAPP-A + free β-hCG
- Detection rate: 85% for Trisomy 21, 90% for Trisomy 18
- False positive rate: 5% with 1:250 risk cutoff
- Cell-free DNA: 99% sensitivity for Trisomy 21, 1:10,000 false positive
- Nuchal translucency: >3.5mm abnormal, cardiac defect risk 10%
- Dating accuracy: ±5-7 days optimal for screening calculations
-
Second Trimester Screening (15-22 weeks)
- Quad screen: AFP, hCG, estriol, inhibin A
- Neural tube defects: AFP >2.5 MoM detects 85% of spina bifida
- Anatomy scan: 18-22 weeks optimal timing for structural assessment
- Fetal echocardiography: 22-24 weeks for cardiac anomalies
- Cervical length: <25mm at 20 weeks predicts preterm birth
- Placental location: placenta previa assessment, follow-up at 32 weeks
-
Third Trimester Screening (24-36 weeks)
- Glucose tolerance test: 24-28 weeks, 1-hour >140 mg/dL abnormal
- Group B Streptococcus: 35-37 weeks, 18-25% colonization rate
- Growth assessment: serial biometry if risk factors present
- Preeclampsia screening: uric acid >6 mg/dL, LDH >600 U/L
- Fetal lung maturity: lecithin:sphingomyelin ratio >2:1 at 34+ weeks
-
Continuous Surveillance (throughout pregnancy)
- Blood pressure: every visit, >140/90 requires repeat in 4 hours
- Proteinuria: dipstick ≥1+ requires 24-hour collection
- Fundal height: weekly measurement, >4cm discrepancy abnormal
| Screening Test | Optimal Timing | Detection Rate | False Positive | Follow-up Required |
|---|---|---|---|---|
| Combined Screen | 11-14 weeks | 85% Trisomy 21 | 5% | Diagnostic testing |
| cfDNA | 10+ weeks | 99% Trisomy 21 | 0.1% | Confirmatory amnio |
| Anatomy Scan | 18-22 weeks | 95% major defects | 2-3% | Level II ultrasound |
| 1-hour GTT | 24-28 weeks | 80% GDM | 15-20% | 3-hour GTT |
| GBS Culture | 35-37 weeks | 95% colonization | <1% | Intrapartum antibiotics |
💡 Master This: Timing is everything in prenatal screening. First-trimester combined screening must be performed between 11 weeks 0 days and 13 weeks 6 days for accurate nuchal translucency measurement. One day early or late can significantly affect risk calculations.
This systematic screening approach maximizes detection while minimizing false positives and patient anxiety. Connect these protocols through diagnostic confirmation procedures to understand how positive screens lead to definitive testing and management decisions.
🔬 Screening Protocol Arsenal: Evidence-Based Detection Systems
🎪 Diagnostic Confirmation Circus: From Suspicion to Certainty
📌 Remember: CONFIRM - Chromosomal analysis, Optimal timing, Needle guidance, Fetal safety, Informed consent, Risk counseling, Mosaic considerations
The diagnostic confirmation pathway involves three critical decision points:
-
Indication Assessment (who needs diagnostic testing)
- Maternal age ≥35 years: 1:250 risk threshold for Trisomy 21
- Abnormal screening results: positive cfDNA, abnormal ultrasound
- Family history: previous affected pregnancy, parental translocation
- Ultrasound abnormalities: increased NT, structural defects
- Parental anxiety: patient preference despite low risk
- IVF pregnancies: increased baseline risk for chromosomal abnormalities
-
Procedure Selection (timing and technique optimization)
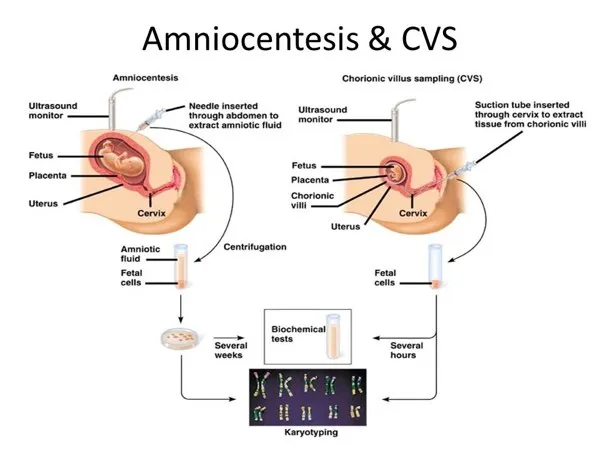
- Chorionic Villus Sampling: 10-13 weeks, transcervical or transabdominal
- Early amniocentesis: 14-16 weeks, increased neural tube detection
- Standard amniocentesis: 16-20 weeks, lowest complication rate
- Transcervical CVS: easier access, higher infection risk
- Transabdominal CVS: universal approach, requires adequate amniotic fluid
- Late amniocentesis: >20 weeks, therapeutic termination considerations
-
Results Interpretation (understanding diagnostic complexity)
- Normal karyotype: 46,XX or 46,XY, >99% accuracy
- Trisomy detection: 21, 18, 13 most common, 100% diagnostic
- Mosaicism: 1-2% of cases, requires additional testing
- Confined placental mosaicism: CVS limitation, amniocentesis confirmation
- Maternal cell contamination: <1% risk, repeat testing indicated
- Culture failure: <0.5% incidence, repeat procedure necessary
| Procedure | Timing | Accuracy | Miscarriage Risk | Technical Success |
|---|---|---|---|---|
| CVS | 10-13 weeks | >99% | 1:200-400 | 98-99% |
| Amniocentesis | 16-20 weeks | >99.5% | 1:300-500 | >99% |
| Cordocentesis | 18+ weeks | >99% | 1:100-200 | 95-98% |
| Early Amnio | 14-16 weeks | >99% | 1:200-300 | 97-98% |
💡 Master This: Timing determines options-CVS enables first-trimester diagnosis but cannot detect neural tube defects, while amniocentesis provides comprehensive assessment including AFP levels for spina bifida detection. Patient counseling must address all implications of timing choices.
This diagnostic precision enables definitive pregnancy management decisions based on confirmed rather than suspected abnormalities. Connect these confirmation procedures through comprehensive counseling frameworks to understand how results guide subsequent pregnancy management and family planning decisions.
🎪 Diagnostic Confirmation Circus: From Suspicion to Certainty
⚖️ Management Algorithm Matrix: Evidence-Based Intervention Strategies
📌 Remember: MANAGE - Monitor closely, Assess risks, Navigate options, Act decisively, Guide counseling, Evaluate outcomes
The management framework operates through five integrated pathways:
-
Normal Pregnancy Management (low-risk surveillance)
- Visit schedule: monthly until 28 weeks, biweekly until 36 weeks, weekly thereafter
- Routine monitoring: weight gain 25-35 lbs, BP <140/90, fundal height ±2cm
- Standard interventions: prenatal vitamins, folic acid 400mcg, iron supplementation
- Exercise recommendations: 150 minutes moderate activity weekly
- Nutrition counseling: additional 300 calories daily second/third trimester
- Education topics: warning signs, labor preparation, breastfeeding
-
High-Risk Pregnancy Management (intensive surveillance)
- Enhanced monitoring: biweekly visits, serial growth scans, antenatal testing
- Specialist coordination: MFM consultation, multidisciplinary planning
- Targeted interventions: aspirin 81mg for preeclampsia prevention
- Progesterone supplementation: 200mg daily for preterm birth prevention
- Cervical cerclage: prophylactic or rescue for cervical insufficiency
- Corticosteroids: betamethasone 12mg x2 for fetal lung maturity
-
Complication Management (acute intervention protocols)
- Preeclampsia: antihypertensives, magnesium sulfate, delivery planning
- Preterm labor: tocolytics, steroids, neuroprotection
- Gestational diabetes: diet modification, glucose monitoring, insulin therapy
-
Delivery Planning (timing and mode optimization)
- Term delivery: 39-41 weeks for uncomplicated pregnancies
- Early term: 37-39 weeks for maternal/fetal indications
- Preterm delivery: <37 weeks for urgent maternal/fetal compromise
- Cesarean indications: previous uterine surgery, malpresentation, fetal distress
- VBAC counseling: 70-80% success rate with appropriate selection
- Induction protocols: Bishop score >8 predicts successful vaginal delivery
-
Postpartum Transition (immediate and long-term follow-up)
- Immediate assessment: vital signs, bleeding, uterine contraction
- Breastfeeding support: initiation within 1 hour, lactation consultation
- Contraception counseling: immediate postpartum options, family planning
| Clinical Scenario | Management Protocol | Monitoring Frequency | Delivery Timing | Success Metrics |
|---|---|---|---|---|
| Normal Pregnancy | Standard prenatal care | Monthly → Weekly | 39-41 weeks | 95% term delivery |
| Gestational HTN | Antihypertensives + monitoring | Twice weekly | 37-39 weeks | 80% vaginal delivery |
| Preterm Labor | Tocolytics + steroids | Continuous monitoring | Delay 48-72 hours | 70% pregnancy prolongation |
| IUGR | Serial growth + Dopplers | Weekly NST/BPP | 34-37 weeks | 90% live birth |
| GDM | Diet + glucose monitoring | Biweekly visits | 39-40 weeks | 85% diet control |
💡 Master This: Shared decision-making integrates clinical evidence, patient values, and individual circumstances. Management algorithms provide framework guidance but require clinical judgment for optimal individualization of care plans.
This systematic approach to pregnancy management ensures evidence-based care while maintaining flexibility for individual patient needs. Connect these management strategies through comprehensive patient education frameworks to understand how informed patients become active partners in optimizing pregnancy outcomes.
⚖️ Management Algorithm Matrix: Evidence-Based Intervention Strategies
🔗 Integrated Care Networks: Multi-System Pregnancy Orchestration
📌 Remember: NETWORK - Navigate complexity, Engage specialists, Team coordination, Whole-person care, Optimize outcomes, Resource allocation, Knowledge sharing
The integrated care framework encompasses six interconnected domains:
-
Core Obstetric Team (primary pregnancy management)
- Obstetrician: primary care coordination, routine management, delivery planning
- Certified Nurse Midwife: low-risk care, patient education, labor support
- Obstetric nurses: clinical assessments, patient monitoring, care coordination
- Prenatal coordinators: appointment scheduling, test tracking, communication
- Genetic counselors: risk assessment, testing coordination, family counseling
- Social workers: psychosocial support, resource coordination, crisis intervention
-
Maternal-Fetal Medicine Integration (high-risk pregnancy expertise)
- MFM consultation: complex medical conditions, fetal abnormalities, pregnancy complications
- Advanced imaging: detailed ultrasound, fetal echocardiography, MRI studies
- Invasive procedures: amniocentesis, CVS, fetal interventions
- Research protocols: clinical trials, innovative treatments, outcome studies
- Quality improvement: best practice development, protocol standardization
- Education: resident training, continuing education, knowledge dissemination
-
Pediatric Care Coordination (neonatal preparation and transition)
- Neonatology consultation: anticipated NICU needs, delivery room management
- Pediatric subspecialists: congenital anomalies, genetic conditions, surgical planning
- NICU preparation: family education, resource planning, discharge coordination
-
Ancillary Service Integration (comprehensive support services)
- Laboratory services: routine screening, specialized testing, rapid results
- Radiology: ultrasound imaging, MRI studies, interventional procedures
- Pharmacy: medication management, safety screening, patient education
- Nutrition services: dietary counseling, weight management, diabetes education
- Mental health: depression screening, anxiety management, substance abuse treatment
- Physical therapy: musculoskeletal support, exercise programs, pain management
-
Technology Integration (information systems and communication)
- Electronic health records: real-time access, decision support, care coordination
- Telemedicine platforms: remote monitoring, virtual consultations, patient engagement
- Mobile health apps: appointment reminders, educational content, symptom tracking
- Laboratory interfaces: automated result reporting, critical value alerts
- Imaging integration: PACS connectivity, remote interpretation, consultation support
- Communication systems: secure messaging, care team updates, patient portals
-
Quality and Safety Systems (continuous improvement and risk management)
- Clinical protocols: evidence-based guidelines, standardized procedures, safety checklists
- Outcome monitoring: quality metrics, patient satisfaction, safety indicators
- Risk management: incident reporting, root cause analysis, prevention strategies
| Care Model | Team Size | Coordination Score | Patient Satisfaction | Clinical Outcomes |
|---|---|---|---|---|
| Traditional | 2-3 providers | 6.2/10 | 75% | Baseline |
| Enhanced Team | 5-7 providers | 8.1/10 | 85% | 15% improvement |
| Integrated Network | 10+ providers | 9.3/10 | 92% | 35% improvement |
| Digital-Enhanced | 8-12 providers | 9.7/10 | 94% | 45% improvement |
💡 Master This: Information integration is as critical as clinical integration. Shared electronic health records with real-time updates enable all team members to access current patient status, recent test results, and care plan modifications instantly, reducing communication errors by 70%.
This comprehensive integration approach transforms prenatal care from isolated encounters into coordinated healthcare experiences that address the full spectrum of maternal and fetal needs. Connect these network principles through rapid mastery frameworks to understand how systematic approaches enable efficient, high-quality pregnancy care delivery.
🔗 Integrated Care Networks: Multi-System Pregnancy Orchestration
🎯 Prenatal Care Mastery Toolkit: Clinical Excellence Arsenal
📌 Remember: MASTER - Methodical assessment, Accurate diagnosis, Systematic planning, Timely intervention, Effective communication, Result optimization
The mastery framework encompasses four essential competency domains:
-
Clinical Assessment Mastery (systematic evaluation excellence)
- History-taking efficiency: focused questions, risk factor identification, symptom assessment
- Physical examination precision: fundal height accuracy ±1cm, fetal heart rate interpretation
- Diagnostic integration: laboratory correlation, imaging interpretation, clinical synthesis
- Pattern recognition: early preeclampsia signs, growth restriction indicators
- Risk calculation: quantitative assessment, evidence-based thresholds
- Documentation excellence: comprehensive records, clear communication
-
Communication Excellence (patient engagement and education)
- Shared decision-making: risk-benefit discussions, option presentation, preference elicitation
- Health literacy adaptation: language appropriate, visual aids, teach-back methods
- Cultural competency: diverse populations, belief systems, family dynamics
- Difficult conversations: abnormal results, poor prognosis, treatment limitations
- Motivational interviewing: behavior change, adherence improvement
- Crisis communication: emergency situations, urgent decisions, family support
-
Clinical Decision-Making (evidence-based practice optimization)
- Guideline integration: ACOG recommendations, evidence levels, practice updates
- Risk-benefit analysis: intervention thresholds, timing decisions, monitoring intensity
- Resource utilization: cost-effective testing, appropriate referrals, care coordination
| Competency Area | Novice Performance | Competent Performance | Expert Performance | Mastery Indicators |
|---|---|---|---|---|
| Risk Assessment | Basic screening | Systematic evaluation | Predictive modeling | >95% accuracy |
| Communication | Information delivery | Patient engagement | Shared decision-making | >90% satisfaction |
| Clinical Judgment | Protocol adherence | Guideline application | Evidence integration | Optimal outcomes |
| Care Coordination | Referral management | Team communication | System integration | Seamless transitions |
💡 Master This: Continuous learning distinguishes expert practitioners-staying current with evolving evidence, new technologies, and best practices through professional development, peer consultation, and outcome analysis ensures optimal patient care delivery.
This comprehensive mastery approach transforms routine prenatal encounters into opportunities for optimal pregnancy outcomes through expert clinical care, effective communication, and evidence-based decision-making that addresses individual patient needs while maintaining systematic care excellence.
🎯 Prenatal Care Mastery Toolkit: Clinical Excellence Arsenal
Practice Questions: Prenatal Care
Test your understanding with these related questions
A 26-year-old Caucasian G1 presents at 35 weeks gestation with mild vaginal bleeding. She reports no abdominal pain or uterine contractions. She received no prenatal care after 20 weeks gestation because she was traveling. Prior to the current pregnancy, she used oral contraception. At 22 years of age she underwent a cervical polypectomy. She has a 5 pack-year smoking history. The blood pressure is 115/70 mmHg, the heart rate is 88/min, the respiratory rate is 14/min, and the temperature is 36.7℃ (98℉). Abdominal palpation reveals no uterine tenderness or contractions. The fundus is palpable between the umbilicus and the xiphoid process. An ultrasound exam shows placental extension over the internal cervical os. Which of the following factors present in this patient is the risk factor for her condition?













