Uterine atony management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Uterine atony management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Uterine atony management US Medical PG Question 1: A 26-year-old woman, gravida 2, para 1, at 28 weeks' gestation comes to the physician for a prenatal visit. She feels well. Pregnancy and delivery of her first child were uncomplicated. Her temperature is 37.2°C (99°F) and blood pressure is 163/105 mm Hg. Her blood pressure 10 weeks ago was 128/84 mm Hg. At her last visit two weeks ago, her blood pressure was 142/92 mm Hg. Pelvic examination shows a uterus consistent in size with a 28-week gestation. A complete blood count and serum concentrations of electrolytes, creatinine, and hepatic transaminases are within the reference range. A urinalysis is within normal limits. Which of the following is the most appropriate next step in management?
- A. Oral labetalol therapy (Correct Answer)
- B. Lisinopril therapy
- C. Magnesium sulfate therapy
- D. Complete bed rest
- E. Dietary salt restriction
Uterine atony management Explanation: **Oral labetalol therapy**
- The patient has developed **gestational hypertension** (blood pressure ≥140/90 mmHg on two occasions at least 4 hours apart after 20 weeks gestation, without proteinuria or other signs of preeclampsia), with her current BP of 163/105 mmHg confirming **severe range hypertension** (systolic ≥160 mmHg or diastolic ≥110 mmHg).
- **Labetalol** is a first-line agent for managing hypertension in pregnancy due to its established safety profile and efficacy in lowering blood pressure.
*Lisinopril therapy*
- **Angiotensin-converting enzyme (ACE) inhibitors** like lisinopril are **contraindicated in pregnancy** as they can cause fetal renal dysfunction, oligohydramnios, and neonatal hypotension.
- This medication choice would be harmful to the fetus.
*Magnesium sulfate therapy*
- **Magnesium sulfate** is indicated for the **prevention and treatment of seizures in preeclampsia/eclampsia**, not for blood pressure control itself.
- While the patient has hypertension, there are no signs of preeclampsia (e.g., proteinuria, signs of end-organ damage), making magnesium sulfate inappropriate at this stage.
*Complete bed rest*
- **Complete bed rest** is no longer recommended for the management of gestational hypertension or preeclampsia, as studies have shown it does not improve maternal or fetal outcomes and can increase the risk of **thromboembolism**.
- It can also negatively impact a patient's quality of life without providing therapeutic benefit.
*Dietary salt restriction*
- While generally recommended for hypertension outside of pregnancy, **severe salt restriction** in pregnancy is **not typically recommended** for gestational hypertension or preeclampsia, as it has not been shown to improve outcomes and could potentially worsen maternal fluid balance.
- The primary management for severe range gestational hypertension involves antihypertensive medications.
Uterine atony management US Medical PG Question 2: Immediately following prolonged delivery of the placenta at 40 weeks gestation, a 32-year-old multiparous woman develops vaginal bleeding. Other than mild asthma, the patient’s pregnancy has been uncomplicated. She has attended many prenatal appointments and followed the physician's advice about screening for diseases, laboratory testing, diet, and exercise. Previous pregnancies were uncomplicated. She has no history of a serious illness. She is currently on intravenous infusion of oxytocin. Her temperature is 37.2°C (99.0°F), blood pressure is 108/60 mm Hg, pulse is 88/min, and respirations are 17/min. Uterine palpation reveals a soft enlarged fundus that extends above the umbilicus. Based on the assessment of the birth canal and placenta, which of the following options is the most appropriate initial step in patient management?
- A. Intramuscular carboprost
- B. Manual exploration of the uterus
- C. Discontinuing oxytocin
- D. Intravenous methylergonovine
- E. Uterine fundal massage (Correct Answer)
Uterine atony management Explanation: ***Uterine fundal massage***
- The patient presents with **postpartum hemorrhage** indicated by vaginal bleeding and a **soft, enlarged fundus** after placental delivery, suggesting **uterine atony**.
- **Uterine fundal massage** is the **first-line intervention** to encourage uterine contraction and reduce bleeding by expelling clots and compressing vessels.
*Intramuscular carboprost*
- **Carboprost** is a **prostaglandin F2 alpha analog** used to treat **uterine atony** when initial measures like uterine massage and oxytocin are insufficient.
- It is contraindicated in patients with **asthma** due to its bronchoconstrictive effects, which this patient has.
*Manual exploration of the uterus*
- **Manual exploration of the uterus** is indicated when there is suspicion of **retained placental fragments** or **uterine rupture**.
- While these can cause postpartum hemorrhage, the primary finding of a soft, boggy uterus points more strongly to atony, making massage the immediate priority.
*Discontinuing oxytocin*
- The patient is already on an **intravenous oxytocin infusion**, which is a uterotonic agent used to prevent and treat uterine atony.
- Discontinuing it would worsen **uterine atony** and increase blood loss, directly contradicting the goal of management.
*Intravenous methylergonovine*
- **Methylergonovine** is an **ergot alkaloid** used to treat **uterine atony**, but it is contraindicated in patients with **hypertension**, which is not explicitly present here, but it is a potent vasoconstrictor and second-line.
- It is often used as a **second-line agent** if oxytocin and massage are ineffective and there are no contraindications.
Uterine atony management US Medical PG Question 3: A 25-year-old G2P1001 at 32 weeks gestation presents to the hospital with painless vaginal bleeding. The patient states that she was taking care of laundry at home when she experienced a sudden sensation of her water breaking and saw that her groin was covered in blood. Her prenatal history is unremarkable according to the clinic records, but she has not seen an obstetrician for the past 14 weeks. Her previous delivery was by urgent cesarean section for placenta previa. Her temperature is 95°F (35°C), blood pressure is 125/75 mmHg, pulse is 79/min, respirations are 18/min, and oxygen saturation is 98% on room air. Cervical exam shows gross blood in the vaginal os. The fetal head is not palpable. Fetal heart rate monitoring demonstrates decelerations and bradycardia. Labs are pending. IV fluids are started. What is the best next step in management?
- A. Cesarean section (Correct Answer)
- B. Betamethasone
- C. Red blood cell transfusion
- D. Vaginal delivery
- E. Lumbar epidural block
Uterine atony management Explanation: ***Cesarean section***
- This patient presents with signs highly suggestive of **placenta previa with possible vasa previa or placental abruption**, with life-threatening complications for both mother and fetus. The presence of **painless vaginal bleeding**, a prior **cesarean section for placenta previa**, and **fetal heart rate decelerations/bradycardia** necessitate immediate delivery via cesarean section to prevent **fetal demise** and severe **maternal hemorrhage**.
- The rapid deterioration of the fetal status, indicated by **decelerations and bradycardia**, confirms the urgency. A **cesarean section** is the quickest and safest way to deliver the baby and address the underlying obstetric emergency.
*Betamethasone*
- **Betamethasone** is administered to promote **fetal lung maturity** in cases of preterm delivery. While this patient is preterm at 32 weeks, the critical nature of the fetal distress and bleeding requires immediate delivery, making the delay for betamethasone administration inappropriate.
- The benefits of steroids for lung maturity are outweighed by the **immediate risk of fetal demise** and severe maternal complications if delivery is delayed.
*Red blood cell transfusion*
- While the patient is actively bleeding and may eventually require a **blood transfusion**, starting IV fluids and proceeding with an **immediate cesarean section** are higher priorities to stabilize the mother and rescue the fetus.
- Transfusions are supportive measures once the source of hemorrhage is addressed and vital signs are stabilized during or after surgery.
*Vaginal delivery*
- Given the patient's history of **placenta previa**, current **painless vaginal bleeding**, and signs of **fetal distress**, a vaginal delivery is contraindicated due to the high risk of **exsanguinating hemorrhage** for the mother and severe fetal compromise.
- The prior **cesarean section for placenta previa** also increases the risk of recurrent previa and **placenta accreta spectrum**, further contraindicating vaginal delivery.
*Lumbar epidural block*
- A **lumbar epidural block** is used for pain management during labor, but in this emergent situation with active bleeding and fetal distress, immediate delivery is paramount.
- The time required to safely administer an **epidural**, along with the potential for **hypotension** in a hypovolemic patient, makes it an inappropriate next step.
Uterine atony management US Medical PG Question 4: Thirty minutes after vaginal delivery of a 2780-g (6-lb 2-oz) newborn at term, a 25-year-old woman, gravida 1, para 1, has heavy vaginal bleeding. Her pregnancy was complicated by pre-eclampsia. Her pulse is 111/min and blood pressure is 95/65 mm Hg. Physical examination shows a fundal height 2 inches below the xiphoid process of the sternum. A drug with which of the following mechanisms of action is most appropriate for this patient?
- A. Activation of phospholipase C (Correct Answer)
- B. Depolarization of the motor end plate
- C. Increased synthesis of cyclic AMP
- D. Inhibition of norepinephrine reuptake
- E. Binding to prostaglandin I2 receptors
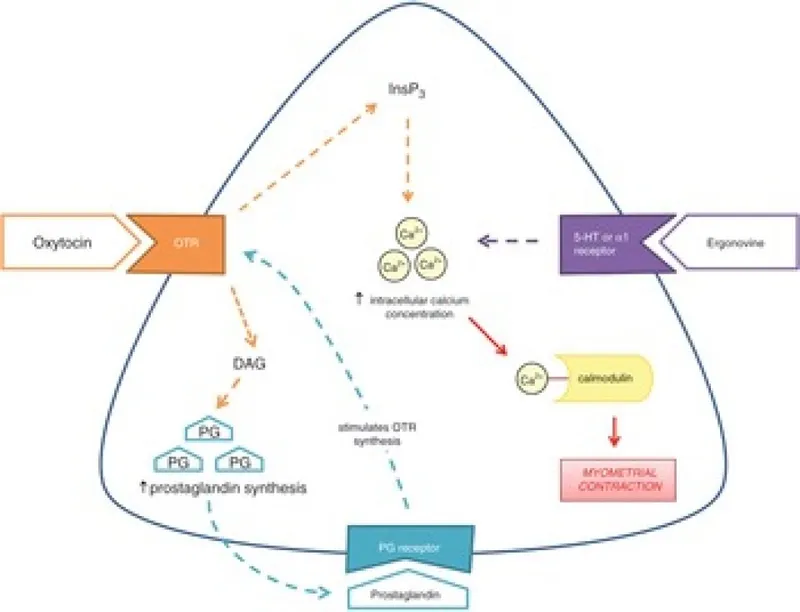
Uterine atony management Explanation: ***Activation of phospholipase C***
- This patient presents with **postpartum hemorrhage (PPH)**, characterized by heavy vaginal bleeding, tachycardia, hypotension, and a poorly contracted uterus (normal fundal height is at the umbilicus immediately after delivery; 2 inches below the xiphoid is high indicating uterine atony).
- The most appropriate first-line treatment for uterine atony is **oxytocin**, which acts by binding to G protein-coupled receptors, leading to the **activation of phospholipase C** and an increase in intracellular calcium, causing uterine muscle contraction.
*Depolarization of the motor end plate*
- This mechanism describes the action of **neuromuscular blocking agents** or agonists at the nicotinic acetylcholine receptor, which are not used for treating postpartum hemorrhage.
- The motor end plate is involved in skeletal muscle contraction, not smooth muscle contraction of the uterus.
*Increased synthesis of cyclic AMP*
- **Increased cyclic AMP** generally leads to smooth muscle relaxation (e.g., beta-2 agonists like terbutaline), which would worsen uterine atony and postpartum hemorrhage.
- Tocolytic agents that would cause uterine relaxation would be contraindicated in this scenario.
*Inhibition of norepinephrine reuptake*
- This mechanism describes the action of certain **antidepressants** (e.g., tricyclic antidepressants, SNRIs) or **stimulants**, which primarily affect the central nervous system and are not used to manage postpartum hemorrhage.
- This action does not directly cause uterine contraction.
*Binding to prostaglandin I2 receptors*
- **Prostaglandin I2 (PGI2)**, also known as prostacyclin, is a potent vasodilator and inhibitor of platelet aggregation. Binding to its receptors would lead to smooth muscle relaxation and would increase bleeding, directly worsening postpartum hemorrhage.
- Uterotonic agents like carboprost (PGF2α analog) act on different prostaglandin receptors to induce uterine contraction.
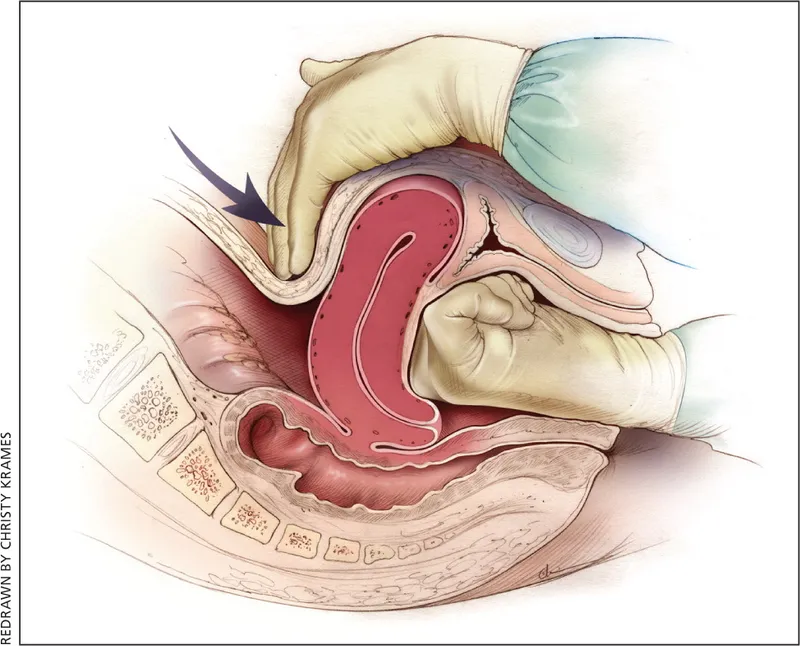
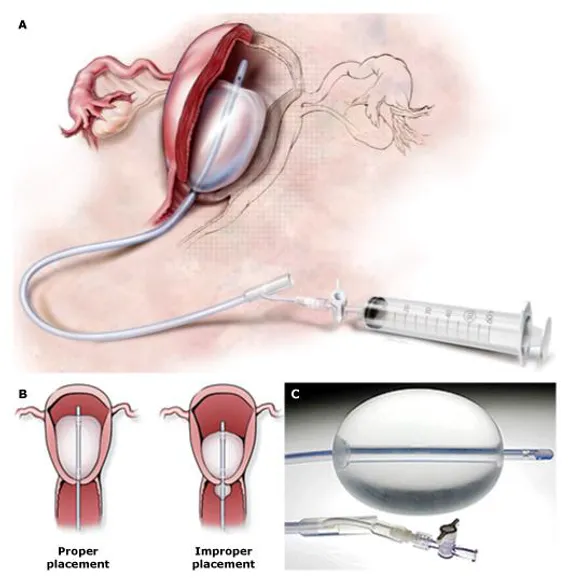
Uterine atony management US Medical PG Question 5: Thirty minutes after normal vaginal delivery of twins, a 35-year-old woman, gravida 5, para 4, has heavy vaginal bleeding with clots. Physical examination shows a soft, enlarged, and boggy uterus. Despite bimanual uterine massage, administration of uterotonic drugs, and placement of an intrauterine balloon for tamponade, the bleeding continues. A hysterectomy is performed. Vessels running through which of the following structures must be ligated during the surgery to achieve hemostasis?
- A. Suspensory ligament
- B. Round ligament
- C. Ovarian ligament
- D. Uterosacral ligament
- E. Cardinal ligament (Correct Answer)
Uterine atony management Explanation: ***Cardinal ligament***
- The **uterine artery** and **uterine vein**, which supply the uterus, run through the **cardinal ligament** (also known as the transverse cervical ligament).
- Ligation of these vessels is crucial during a hysterectomy to control bleeding from the uterus.
*Suspensory ligament*
- The **suspensory ligament of the ovary** contains the **ovarian artery** and vein, which primarily supply the ovaries and fallopian tubes.
- While these may be ligated during a hysterectomy if the ovaries are removed, they are not the primary vessels causing uterine bleeding in postpartum hemorrhage.
*Round ligament*
- The **round ligament of the uterus** extends from the uterus to the labia majora and contains relatively small vessels, primarily contributing to uterine support.
- Ligation of this ligament alone would not effectively control heavy uterine bleeding.
*Ovarian ligament*
- The **ovarian ligament** connects the ovary to the uterus and contains small vessels that mainly supply the ovary.
- It does not house the major blood supply to the uterus itself.
*Uterosacral ligament*
- The **uterosacral ligaments** primarily provide support to the uterus by connecting it to the sacrum and contain small nerves and vessels.
- Ligation of these ligaments would not control the main arterial supply to the uterus.
Uterine atony management US Medical PG Question 6: A 31-year-old G6P6 woman with a history of fibroids gives birth to twins via vaginal delivery. Her pregnancy was uneventful, and she reported having good prenatal care. Both placentas are delivered immediately after the birth. The patient continues to bleed significantly over the next 20 minutes. Her temperature is 97.0°F (36.1°C), blood pressure is 124/84 mmHg, pulse is 95/min, respirations are 16/min, and oxygen saturation is 98% on room air. Continued vaginal bleeding is noted. Which of the following is the most appropriate initial step in management?
- A. Oxytocin
- B. Blood product transfusion
- C. Uterine artery embolization
- D. Hysterectomy
- E. Bimanual massage (Correct Answer)
Uterine atony management Explanation: ***Bimanual massage***
- The patient is experiencing **postpartum hemorrhage (PPH)**, indicated by significant bleeding post-delivery. **Uterine atony** is the most common cause of PPH, and bimanual massage helps stimulate uterine contractions to reduce bleeding.
- This is a **first-line, non-pharmacological intervention** that can be rapidly initiated to manage uterine atony.
*Oxytocin*
- While **oxytocin** is a uterotonic agent used to treat PPH, the initial step is typically **bimanual massage** to physically stimulate the uterus while preparing for medication administration.
- Oxytocin infusion would be administered concurrent with or immediately following bimanual massage, but manual compression is often initiated first.
*Blood product transfusion*
- Blood product transfusion is indicated for significant blood loss and hemodynamic instability, but it is a **supportive measure** rather than an initial intervention to stop the bleeding.
- The patient's current **blood pressure (124/84 mmHg)** and **pulse (95/min)** do not immediately suggest severe hypovolemic shock requiring immediate transfusion as the *first* step before attempting to control the source of bleeding.
*Uterine artery embolization*
- **Uterine artery embolization** is a highly invasive procedure typically reserved for cases where conservative measures, including uterotonic agents and bimanual compression, have failed to control PPH.
- It is not an appropriate initial step, as it requires specialized equipment and personnel and would delay immediate management of active bleeding.
*Hysterectomy*
- **Hysterectomy** is a last-resort intervention for intractable PPH that cannot be controlled by all other methods, including uterotonics, uterine massage, and other surgical or interventional radiology techniques.
- It is a highly invasive procedure with significant morbidity and is not considered an initial management step.
Uterine atony management US Medical PG Question 7: A 35-year-old woman presents to the emergency room with severe right lower quadrant abdominal pain. She has a history of tubal ligation 3 years ago and a history of chlamydia treated 15 years ago. She usually has very regular periods, but her last menstrual period was 10 weeks ago. On exam, she is afebrile, HR 117, blood pressure of 88/56 mmHg, and she has peritoneal signs including rebound tenderness. Urine Beta-hCG is positive. Hgb is 9.9 g/dL. What is the appropriate treatment?
- A. Laparotomy (Correct Answer)
- B. Methotrexate
- C. Serial beta-hCG levels
- D. Blood transfusion
- E. Azithromycin
Uterine atony management Explanation: ***Laparotomy***
- The patient presents with classic signs of a **ruptured ectopic pregnancy**, including abdominal pain, **peritoneal signs**, **hypotension** (88/56 mmHg), and **tachycardia** (HR 117), all indicative of hemodynamic instability and internal bleeding.
- Given the patient's hemodynamic instability, a **laparotomy** is the most urgent and appropriate treatment to directly visualize, control bleeding, and remove the ectopic pregnancy, as medical management or less invasive surgical options would be too slow and risky.
*Methotrexate*
- **Methotrexate** is a medical treatment for ectopic pregnancy, but it is contraindicated in cases of **hemodynamic instability**, suspected rupture, or significant intra-abdominal bleeding.
- The patient's **hypotension**, **tachycardia**, and **peritoneal signs** strongly suggest rupture and active bleeding, making methotrexate an inappropriate and dangerous choice.
*Serial beta-hCG levels*
- Monitoring **serial beta-hCG levels** is used to diagnose and follow the resolution of an ectopic pregnancy, especially if managed medically or watchfully.
- However, in a patient with signs of **hemodynamic instability** and presumed rupture, this diagnostic approach is too slow and does not address the immediate life-threatening bleeding.
*Blood transfusion*
- While the patient's hemoglobin (Hgb 9.9 g/dL) is slightly low, a **blood transfusion** alone does not address the underlying cause of the bleeding, which is a ruptured ectopic pregnancy.
- Transfusion might be necessary as an adjunct to surgery, but it is not the primary treatment for stopping the hemorrhage.
*Azithromycin*
- **Azithromycin** is an antibiotic used to treat bacterial infections, such as Chlamydia. While the patient has a history of chlamydia, there is no indication of an active infection requiring antibiotic treatment.
- Her current symptoms are indicative of an **ectopic pregnancy rupture**, not an infection.
Uterine atony management US Medical PG Question 8: 29-year-old G2P2002 presents with foul-smelling lochia and fever. She is post-partum day three status-post cesarean section due to eclampsia. Her temperature is 101 F, and heart rate is 103. She denies chills. On physical exam, lower abdominal and uterine tenderness is present. Leukocytosis with left shift is seen in labs. Which of the following is the next best step in management?
- A. Endometrial culture
- B. Intravenous clindamycin and gentamicin treatment (Correct Answer)
- C. Prophylactic intravenous cefazolin treatment
- D. Intramuscular cefotetan treatment
- E. Blood culture
Uterine atony management Explanation: **Intravenous clindamycin and gentamicin treatment**
* This patient presents with **fever**, **foul-smelling lochia**, **uterine tenderness**, and **leukocytosis with left shift** on postpartum day three after a cesarean section, which are classic signs of **postpartum endometritis**.
* The recommended first-line treatment for **postpartum endometritis** is **broad-spectrum intravenous antibiotics**, typically a combination of **clindamycin** and **gentamicin**, which covers the polymicrobial nature of the infection, including anaerobes and gram-negative rods.
*Endometrial culture*
* While useful for identifying specific pathogens, **endometrial cultures** are generally **not recommended prior to initiating treatment for postpartum endometritis** as the infection is typically polymicrobial, and treatment should be started empirically.
* **Contamination with normal vaginal flora** is a significant concern, making interpretation of cultures difficult and potentially delaying appropriate treatment.
*Prophylactic intravenous cefazolin treatment*
* **Cefazolin** is a first-generation cephalosporin often used for **surgical prophylaxis** before a cesarean section to prevent infection.
* This patient already has clear signs of an established **postpartum infection (endometritis)**, so prophylactic antibiotics are no longer appropriate; she requires therapeutic treatment.
*Intramuscular cefotetan treatment*
* **Cefotetan** is a second-generation cephalosporin with good coverage against some anaerobes and gram-negative bacteria.
* However, for established **postpartum endometritis**, especially after a cesarean section, **intravenous administration** of broad-spectrum antibiotics is preferred for faster therapeutic levels and better efficacy than intramuscular delivery.
*Blood culture*
* **Blood cultures** are important to rule out **bacteremia** or **sepsis**, especially in patients with high fever or signs of systemic illness.
* While an important diagnostic step, it is **not the *next best step in management*** for a patient with clear signs of endometritis; empirical antibiotic therapy should be initiated promptly while awaiting culture results.
Uterine atony management US Medical PG Question 9: A pregnant woman with a known case of asthma is experiencing postpartum hemorrhage (PPH). Which drug is contraindicated?
- A. Methyl ergometrine
- B. Carboprost (Correct Answer)
- C. Misoprostol
- D. Oxytocin
Uterine atony management Explanation: ***Carboprost***
- **Carboprost** is a **prostaglandin F2-alpha analog** that causes strong uterine contractions but also leads to **bronchoconstriction** and increased airway resistance.
- Due to its potent bronchoconstrictive effects, **carboprost** is **absolutely contraindicated in patients with asthma** as it can precipitate a severe asthmatic attack.
*Methyl ergometrine*
- **Methyl ergometrine** is an **ergot alkaloid** that causes sustained uterine contractions and is effective for PPH.
- It is contraindicated in patients with **hypertension** or **pre-eclampsia** due to its vasoconstrictive properties, but not typically in asthma.
*Misoprostol*
- **Misoprostol** is a **prostaglandin E1 analog** used for PPH management, causing uterine contractions.
- It is generally safe for use in patients with asthma as it does not have significant bronchoconstrictive side effects.
*Oxytocin*
- **Oxytocin** is a first-line uterotonic agent for PPH, working by causing rhythmic uterine contractions.
- It is generally considered safe in patients with asthma and is not known to exacerbate respiratory conditions.
Uterine atony management US Medical PG Question 10: A 27-year-old woman who delivered a female child 9 months ago presents with complaints of absent periods since childbirth. She has been using contraceptive methods for family planning. Her serum beta-hCG level is 4.9 mIU/ ml , prolactin level is $88 \mathrm{ng} / \mathrm{ml}$, and TSH is 3.8 $\mu \mathrm{IU} / \mathrm{ml}$. What is the most likely reason for her amenorrhea?
- A. Lactational amenorrhea (Correct Answer)
- B. Hypothyroidism
- C. Prolactinoma
- D. Normal pregnancy
Uterine atony management Explanation: ***Lactational amenorrhea***
- The patient describes a history of recent childbirth (9 months ago), amenorrhea, and an elevated **prolactin level** (**88 ng/mL**).
- While contraceptive methods are being used, persistent **postpartum amenorrhea** with hyperprolactinemia is commonly seen in women who are breastfeeding, even if intermittently.
*Hypothyroidism*
- Although **hypothyroidism** can cause amenorrhea, the patient's TSH level of **3.8 μIU/mL** is within the normal reference range, making hypothyroidism an unlikely cause.
- While mild thyroid dysfunction can impact menstrual cycles, this TSH level alone is not sufficient to explain **amenorrhea**.
*Prolactinoma*
- A **prolactinoma** is characterized by significantly elevated prolactin levels, often much higher than the **88 ng/mL** seen in this patient (typically > 100-200 ng/mL).
- Given the recent childbirth, the elevated prolactin is more likely physiological due to lactation rather than a **pathological tumor**.
*Normal pregnancy*
- The patient's serum **beta-hCG level of 4.9 mIU/mL** is below the threshold typically considered diagnostic for pregnancy (usually >25 mIU/mL).
- This value indicates that a **normal ongoing pregnancy** is highly unlikely.
More Uterine atony management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.