Surgical management of PPH US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surgical management of PPH. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surgical management of PPH US Medical PG Question 1: A 29-year-old G2P2 female gives birth to a healthy baby boy at 39 weeks of gestation via vaginal delivery. Immediately after the delivery of the placenta, she experiences profuse vaginal hemorrhage. Her prior birthing history is notable for an emergency cesarean section during her first pregnancy. She did not receive any prenatal care during either pregnancy. Her past medical history is notable for obesity and diabetes mellitus, which is well controlled on metformin. Her temperature is 99.0°F (37.2°C), blood pressure is 95/50 mmHg, pulse is 125/min, and respirations are 22/min. On physical examination, the patient is in moderate distress. Her extremities are pale, cool, and clammy. Capillary refill is delayed. Which of the following is the most likely cause of this patient’s bleeding?
- A. Chorionic villi invading into the myometrium
- B. Placental implantation over internal cervical os
- C. Chorionic villi attaching to the decidua basalis
- D. Chorionic villi invading into the serosa
- E. Chorionic villi attaching to the myometrium (Correct Answer)
Surgical management of PPH Explanation: ***Chorionic villi attaching to the myometrium***
- This describes **placenta accreta**, where the **chorionic villi adhere directly to the myometrium** without invading beyond it. This condition is strongly associated with a history of **prior C-sections**, as the scar tissue increases the risk of abnormal placental implantation.
- The profuse hemorrhage immediately following placental delivery, despite the placenta being delivered, suggests a problem with normal placental separation from the uterine wall. **Placenta accreta** can lead to massive postpartum hemorrhage when the placenta attempts to separate, tearing the maternal vessels.
*Chorionic villi invading into the myometrium*
- This describes **placenta increta**, where the **chorionic villi invade deeper into the myometrium**. While also causing severe hemorrhage, the term "attaching to the myometrium" (accreta) is a more common and slightly less severe form often seen with prior C-sections.
- Both accreta and increta present similarly with hemorrhage, but accreta is the initial and most common form of abnormal adherence to the myometrium.
*Placental implantation over internal cervical os*
- This describes **placenta previa**, which is characterized by **painless vaginal bleeding** typically in the **second or third trimester**, before delivery.
- While a prior C-section is a risk factor for placenta previa, the hemorrhage in this case occurred *after* the delivery of the placenta, not before or during labor, ruling out active previa.
*Chorionic villi invading into the serosa*
- This describes **placenta percreta**, the most severe form where **chorionic villi invade through the myometrium and into the uterine serosa**, potentially involving adjacent organs.
- While it causes massive hemorrhage, "attaching to" or even "invading into" the myometrium (accreta/increta) are more probable, given the description, than invasion *through* to the serosa, though all are part of the placenta accreta spectrum.
*Chorionic villi invading beyond the serosa*
- This is an alternative description for **placenta percreta**, indicating invasion through the uterus and potentially into surrounding structures like the bladder.
- While this is a severe cause of postpartum hemorrhage, the provided option "Chorionic villi attaching to the myometrium" (placenta accreta) is the most common form of abnormally adherent placenta in the spectrum and is highly consistent with the patient's history of prior C-section and the clinical presentation of hemorrhage after placental delivery.
Surgical management of PPH US Medical PG Question 2: A 22-year-old G4P2 at 35 weeks gestation presents to the hospital after she noticed that "her water broke." Her prenatal course is unremarkable, but her obstetric history includes postpartum hemorrhage after her third pregnancy, attributed to a retained placenta. The patient undergoes augmentation of labor with oxytocin and within four hours delivers a male infant with Apgar scores of 8 and 9 at 1 and 5 minutes, respectively. Three minutes later, the placenta passes the vagina, but a smooth mass attached to the placenta continues to follow. Her temperature is 98.6°F (37°C), blood pressure is 110/70 mmHg, pulse is 90/min, and respirations are 20/min. What is the most likely complication in the absence of intervention?
- A. Hypertension
- B. Hemorrhagic shock (Correct Answer)
- C. Tachypnea
- D. Heart failure
- E. Hyperthermia
Surgical management of PPH Explanation: ***Hemorrhagic shock***
- The presenting symptoms suggest **uterine inversion**, a rare but serious obstetrical emergency where the uterus turns inside out, which is usually accompanied by a **sudden gush of blood** or **postpartum hemorrhage**.
- Without immediate intervention to correct the uterine inversion and manage bleeding, the rapid and significant blood loss will lead to **hemorrhagic shock**, characterized by inadequate tissue perfusion and oxygen delivery.
*Hypertension*
- **Uterine inversion** and associated significant blood loss would typically lead to **hypotension** and shock, not hypertension.
- Hypertension in the postpartum period is usually linked to conditions like **preeclampsia** or **essential hypertension**, which are not indicated here.
*Tachypnea*
- While tachypnea can be a symptom of **hemorrhagic shock** due to metabolic acidosis and compensatory mechanisms, it is a *symptom* of the underlying problem, not the most likely primary complication itself.
- The immediate life-threatening complication from uterine inversion is **massive blood loss**, leading to shock.
*Heart failure*
- **Acute heart failure** due to uterine inversion or postpartum hemorrhage is unlikely unless the patient has pre-existing cardiac conditions or develops severe, prolonged shock leading to multi-organ dysfunction.
- The immediate concern is the **circulatory collapse** from blood loss, not primary cardiac failure.
*Hyperthermia*
- **Hyperthermia** (fever) is typically associated with **infection**, such as endometritis or chorioamnionitis, and not a direct consequence of uterine inversion or immediate postpartum hemorrhage.
- The patient's temperature is normal, indicating no infection at presentation.
Surgical management of PPH US Medical PG Question 3: A 27-year-old woman, gravida 3, para 2, at 41 weeks' gestation is admitted to the hospital in active labor. Her pregnancy has been uncomplicated. Both of her prior children were delivered by vaginal birth. She has a history of asthma. Current medications include iron and vitamin supplements. After a prolonged labor, she undergoes vaginal delivery. Shortly afterwards, she begins to have heavy vaginal bleeding with clots. Her temperature is 37.2°C (98.9°F), pulse is 90/min, respirations are 17/min, and blood pressure is 130/72 mm Hg. Examination shows a soft, enlarged, and boggy uterus on palpation. Laboratory studies show:
Hemoglobin 10.8 g/dL
Hematocrit 32.3%
Leukocyte Count 9,000/mm3
Platelet Count 140,000/mm3
Prothrombin time 14 seconds
Partial thromboplastin time 38 seconds
Her bleeding continues despite bimanual uterine massage and administration of oxytocin. Which of the following is the most appropriate next step in management?
- A. Administer methylergonovine (Correct Answer)
- B. Transfuse blood
- C. Perform hysterectomy
- D. Administer carboprost tromethamine
- E. Perform curettage
Surgical management of PPH Explanation: ***Administer methylergonovine***
- The patient is likely experiencing **postpartum hemorrhage (PPH)** due to **uterine atony**, characterized by a soft, enlarged, and boggy uterus after delivery, with continued bleeding despite initial measures (massage, oxytocin).
- Given her history of **asthma**, carboprost tromethamine (prostaglandin F2-alpha) is **contraindicated** due to its potential to cause severe bronchospasm, making methylergonovine (an ergot alkaloid) the appropriate next uterotonic agent.
*Transfuse blood*
- While blood transfusions may eventually be necessary if bleeding is severe and leads to significant hemodynamic instability or severe anemia, it is **not the immediate next step** in managing the underlying cause of the hemorrhage (uterine atony).
- **Uterotonic agents** should be tried first to contract the uterus and stop the bleeding, as indicated by the patient's current vital signs being relatively stable (pulse 90/min, BP 130/72 mm Hg).
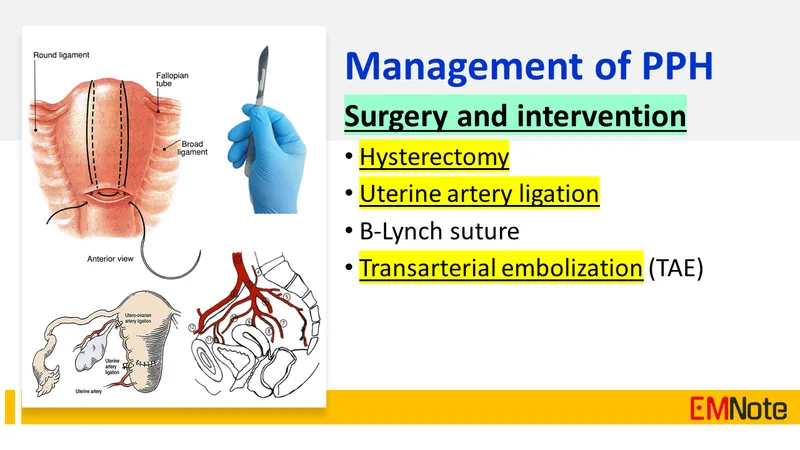
*Perform hysterectomy*
- **Hysterectomy** is a drastic measure considered only after all less invasive medical and surgical interventions (e.g., uterotonic agents, uterine tamponade, suturing techniques) have failed to control severe PPH.
- It would be **premature** to proceed directly to hysterectomy without attempting additional medical management for uterine atony.
*Administer carboprost tromethamine*
- **Carboprost tromethamine** is a prostaglandin analog that is effective in treating uterine atony but is **contraindicated in patients with asthma** due to its known side effect of inducing bronchospasm.
- The patient's history of asthma makes this a **dangerous option**, and an alternative uterotonic like methylergonovine should be chosen.
*Perform curettage*
- **Curettage** (removing retained placental fragments) would be appropriate if the cause of PPH was **retained placental tissue**.
- However, the examination finding of a **soft, enlarged, and boggy uterus** is characteristic of uterine atony, not retained placenta, and the initial management of atony involves uterotonic agents.
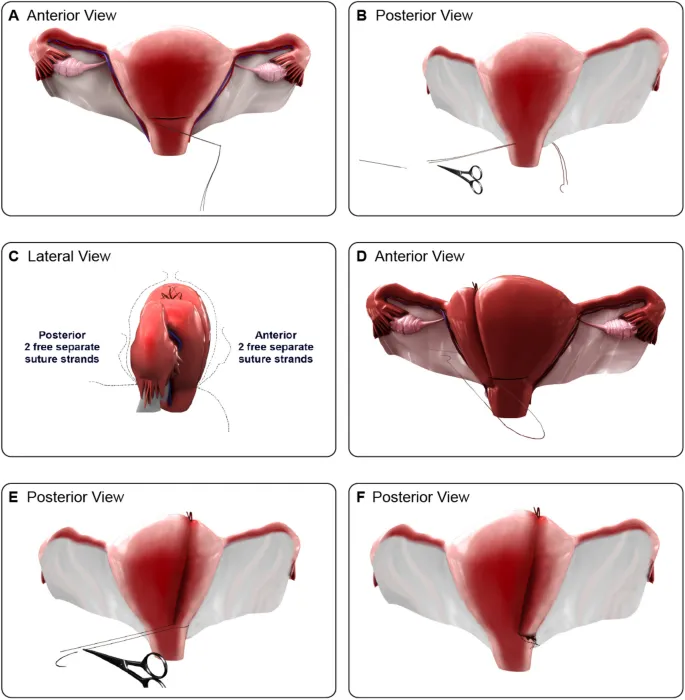
Surgical management of PPH US Medical PG Question 4: A 30-year-old woman, gravida 2, para 1, at 42 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been complicated by gestational diabetes, for which she has been receiving insulin injections. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 90/min, respirations are 18/min, and blood pressure is 135/80 mm Hg. The fetal heart rate tracing shows a baseline heart rate of 145/min and moderate variation with frequent accelerations and occasional early decelerations. She undergoes an elective repeat lower segment transverse cesarean section with complete removal of the placenta. Shortly after the operation, she starts having heavy uterine bleeding with passage of clots. Examination shows a soft uterus on palpation. Her bleeding continues despite fundal massage and the use of packing, oxytocin, misoprostol, and carboprost. Her pulse rate is now 120/min, respirations are 20/min, and blood pressure is 90/70 mm Hg. Her hemoglobin is 8 g/dL, hematocrit is 24%, platelet count is 120,000 mm3, prothrombin time is 11 seconds, and partial thromboplastin time is 30 seconds. Mass transfusion protocol is activated and a B-Lynch uterine compression suture is placed to control her bleeding. Which of the following is the mostly likely cause of her postpartum complication?
- A. Adherent placenta to myometrium
- B. Uterine inversion
- C. Infection of the endometrial lining of the uterus
- D. Uterine rupture
- E. Lack of uterine muscle contraction (Correct Answer)
Surgical management of PPH Explanation: ***Lack of uterine muscle contraction***
- The presentation of a **soft uterus** on palpation and continued severe bleeding despite fundal massage and uterotonics (**oxytocin, misoprostol, carboprost**) is highly indicative of **uterine atony**, which is a lack of effective uterine muscle contraction.
- Uterine atony is the most common cause of **postpartum hemorrhage**, and risk factors include **macrosomia** (due to gestational diabetes), **multiparity**, and a prolonged labor or rapid delivery, though the latter two are less clear here.
*Adherent placenta to myometrium*
- While a history of prior C-section and **macrosomia** (due to gestational diabetes) could increase the risk of an **abnormally adherent placenta** (accreta, increta, percreta), the description notes **complete removal of the placenta**.
- If the placenta were morbidly adherent and not completely removed, bleeding would likely stem from retained placental tissue, and this would typically be explicitly noted or suspected due to difficulty with manual removal.
*Uterine inversion*
- **Uterine inversion** involves the uterus turning inside out, which would present with a **mass protruding from the vagina** or a visible inversion of the fundus upon examination, along with sudden onset of severe pain and shock.
- The description of a **soft uterus** and an absence of a physical description of uterine inversion makes this diagnosis less likely.
*Infection of the endometrial lining of the uterus*
- **Endometritis** (infection of the endometrial lining) typically presents with fever, foul-smelling lochia, uterine tenderness, and prolonged postpartum bleeding, usually occurring a few days postpartum rather than immediately following delivery.
- The acute, massive hemorrhage immediately following delivery, coupled with a normal initial temperature, does not align with the typical presentation of endometritis.
*Uterine rupture*
- **Uterine rupture** is a serious complication, especially with a history of prior C-section, but it typically presents with **sudden severe abdominal pain**, fetal heart rate abnormalities (if it occurs before delivery), and **hemodynamic instability**, often with cessation of contractions.
- While the patient is hemodynamically unstable, the primary issue described is heavy uterine bleeding with a soft uterus, and no mention of severe abdominal pain or clear signs of rupture during the C-section make uterine atony a more direct explanation for the described symptoms.
Surgical management of PPH US Medical PG Question 5: A 34-year-old G5P5 woman gave birth to a healthy infant 30 minutes ago by vacuum-assisted vaginal delivery and is now experiencing vaginal bleeding. The placenta was delivered spontaneously and was intact upon examination. The infant weighed 5.2 kg and had Apgar scores of 8 and 9. No perineal tear or intentional episiotomy occurred. The patient has type 1 diabetes. She had good glycemic control throughout her pregnancy. She took a prenatal vitamin daily. Blood pressure is 135/72 mmHg, pulse is 102/min, and respirations are 18/min. Upon physical examination, the uterine fundus is soft and palpated 4 cm above the umbilicus. There are 3-cm blood clots on the patient’s bed pad. Which of the following is the next best step in management for the patient’s bleeding?
- A. Administer misoprostol
- B. Manually remove retained placental fragments
- C. Perform uterine massage and administer oxytocin (Correct Answer)
- D. Perform uterine artery embolization
- E. Perform hysterectomy
Surgical management of PPH Explanation: ***Perform uterine massage and administer oxytocin***
- The patient's presentation of a **soft, boggy uterus** palpated 4 cm above the umbilicus after delivery, along with significant vaginal bleeding and clots, is highly indicative of **uterine atony**.
- **Uterine massage** and administration of **oxytocin** are the first-line interventions to stimulate uterine contractions and reduce bleeding by compressing placental site blood vessels.
*Administer misoprostol*
- **Misoprostol** is a prostaglandin analog that can be used for uterine atony when oxytocin is insufficient or contraindicated, but it is not the *first-line* treatment.
- Its onset of action may be slower than immediate uterine massage and IV oxytocin, which are preferred for initial management of acute uterine atony.
*Manually remove retained placental fragments*
- The question states that the **placenta was delivered spontaneously and was intact upon examination**, which makes retained placental fragments less likely as the primary cause of bleeding.
- While retained fragments can cause postpartum hemorrhage, the boggy uterus points more strongly to atony, and manual removal is indicated *after* confirming retained placental tissue.
*Perform uterine artery embolization*
- **Uterine artery embolization** is an interventional radiology procedure typically reserved for cases of postpartum hemorrhage that are refractory to conventional medical and surgical management.
- It is an invasive procedure and not the appropriate *next best step* for initial management of suspected uterine atony.
*Perform hysterectomy*
- **Hysterectomy** is a last-resort, life-saving measure for intractable postpartum hemorrhage when all other medical and surgical options have failed.
- It is a highly invasive and irreversible procedure, certainly not the *next best step* in a patient who has just begun to bleed.
Surgical management of PPH US Medical PG Question 6: Five minutes after initiating a change of position and oxygen inhalation, the oxytocin infusion is discontinued. A repeat CTG that is done 10 minutes later shows recurrent variable decelerations and a total of 3 uterine contractions in 10 minutes. Which of the following is the most appropriate next step in management?
- A. Restart oxytocin infusion
- B. Emergent Cesarean section
- C. Administer terbutaline
- D. Monitor without intervention
- E. Amnioinfusion (Correct Answer)
Surgical management of PPH Explanation: ***Amnioinfusion***
- **Recurrent variable decelerations** persisting after discontinuing oxytocin and changing maternal position often indicate **cord compression**, which can be relieved by amnioinfusion.
- Adding fluid to the amniotic cavity **cushions the umbilical cord**, reducing compression during uterine contractions.
*Restart oxytocin infusion*
- Reinitiating oxytocin would likely **worsen the recurrent variable decelerations** by increasing uterine contraction frequency and intensity, thereby exacerbating cord compression.
- The goal is to alleviate fetal distress, not to intensify uterine activity that is already causing issues.
*Emergent Cesarean section*
- While an emergent Cesarean section is indicated for **unresolved fetal distress**, it's usually considered after less invasive measures, such as amnioinfusion, have failed.
- There is still an opportunity for a simpler intervention to resolve the issue before resorting to surgery.
*Administer terbutaline*
- Terbutaline is a **tocolytic agent** used to reduce uterine contractions, which can be helpful in cases of tachysystole or hyperstimulation.
- In this scenario, the contraction frequency is low (3 in 10 minutes), so reducing contractions is not the primary aim; rather, the focus is on resolving the cord compression causing decelerations.
*Monitor without intervention*
- **Recurrent variable decelerations** are an concerning sign of **fetal distress** and require intervention to prevent potential harm to the fetus.
- Simply monitoring without intervention would be inappropriate and could lead to worsening fetal hypoxemia and acidosis.
Surgical management of PPH US Medical PG Question 7: A 32-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the emergency department because of vaginal bleeding for the past hour. The patient reports that she felt contractions prior to the onset of the bleeding, but the contractions stopped after the bleeding started. She also has severe abdominal pain. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 110/min, respirations are 17/min, and blood pressure is 90/60 mm Hg. Examination shows diffuse abdominal tenderness with no rebound or guarding; no contractions are felt. The fetal heart rate shows recurrent variable decelerations. Which of the following is the most likely diagnosis?
- A. Uterine inertia
- B. Amniotic fluid embolism
- C. Uterine rupture (Correct Answer)
- D. Vasa previa
- E. Abruptio placentae
Surgical management of PPH Explanation: ***Uterine rupture***
- The patient's history of a prior **cesarean section**, sudden onset of **vaginal bleeding** and **severe abdominal pain**, resolution of contractions, and signs of **hypovolemic shock** (tachycardia, hypotension) coupled with fetal distress (variable decelerations) are highly indicative of uterine rupture.
- Diffuse abdominal tenderness without rebound or guarding, and no palpable contractions, are also consistent with rupture.
*Uterine inertia*
- This condition is characterized by **weak or uncoordinated uterine contractions** leading to prolonged labor, but it does not typically present with acute vaginal bleeding, sudden severe abdominal pain, or hypovolemic shock.
- Fetal distress in uterine inertia would more likely be due to prolonged labor rather than acute compromise following a sudden event.
*Amniotic fluid embolism*
- This is a rare, life-threatening obstetric emergency characterized by sudden **cardiovascular collapse, respiratory distress**, and **coagulopathy**, often occurring during labor or immediately postpartum.
- While it can cause fetal distress, vaginal bleeding and severe abdominal pain are not primary presenting symptoms.
*Vasa previa*
- Characterized by **painless vaginal bleeding** when fetal vessels within the membranes cross the internal cervical os, making them vulnerable to rupture during cervical dilation or amniotomy.
- The bleeding is typically fetal blood, and fetal distress occurs rapidly, but the mother would not experience severe abdominal pain or signs of hypovolemic shock unless the bleeding is substantial and prolonged.
*Abruptio placentae*
- This involves the **premature separation of the placenta**, causing painful vaginal bleeding, uterine tenderness, and frequent, strong contractions.
- While it can cause hypovolemic shock and fetal distress, the description of contractions stopping after bleeding started, along with a previous C-section scar, points more specifically to uterine rupture rather than an abruption.
Surgical management of PPH US Medical PG Question 8: A 31-year-old G6P6 woman with a history of fibroids gives birth to twins via vaginal delivery. Her pregnancy was uneventful, and she reported having good prenatal care. Both placentas are delivered immediately after the birth. The patient continues to bleed significantly over the next 20 minutes. Her temperature is 97.0°F (36.1°C), blood pressure is 124/84 mmHg, pulse is 95/min, respirations are 16/min, and oxygen saturation is 98% on room air. Continued vaginal bleeding is noted. Which of the following is the most appropriate initial step in management?
- A. Oxytocin
- B. Blood product transfusion
- C. Uterine artery embolization
- D. Hysterectomy
- E. Bimanual massage (Correct Answer)
Surgical management of PPH Explanation: ***Bimanual massage***
- The patient is experiencing **postpartum hemorrhage (PPH)**, indicated by significant bleeding post-delivery. **Uterine atony** is the most common cause of PPH, and bimanual massage helps stimulate uterine contractions to reduce bleeding.
- This is a **first-line, non-pharmacological intervention** that can be rapidly initiated to manage uterine atony.
*Oxytocin*
- While **oxytocin** is a uterotonic agent used to treat PPH, the initial step is typically **bimanual massage** to physically stimulate the uterus while preparing for medication administration.
- Oxytocin infusion would be administered concurrent with or immediately following bimanual massage, but manual compression is often initiated first.
*Blood product transfusion*
- Blood product transfusion is indicated for significant blood loss and hemodynamic instability, but it is a **supportive measure** rather than an initial intervention to stop the bleeding.
- The patient's current **blood pressure (124/84 mmHg)** and **pulse (95/min)** do not immediately suggest severe hypovolemic shock requiring immediate transfusion as the *first* step before attempting to control the source of bleeding.
*Uterine artery embolization*
- **Uterine artery embolization** is a highly invasive procedure typically reserved for cases where conservative measures, including uterotonic agents and bimanual compression, have failed to control PPH.
- It is not an appropriate initial step, as it requires specialized equipment and personnel and would delay immediate management of active bleeding.
*Hysterectomy*
- **Hysterectomy** is a last-resort intervention for intractable PPH that cannot be controlled by all other methods, including uterotonics, uterine massage, and other surgical or interventional radiology techniques.
- It is a highly invasive procedure with significant morbidity and is not considered an initial management step.
Surgical management of PPH US Medical PG Question 9: A 30-year-old woman, gravida 2, para 1, abortus 1, comes to the physician because of failure to conceive for 12 months. She is sexually active with her husband 2–3 times per week. Her first child was born at term after vaginal delivery 2 years ago. At that time, the postpartum course was complicated by hemorrhage from retained placental products, and the patient underwent dilation and curettage. Menses occur at regular 28-day intervals and previously lasted for 5 days with normal flow, but now last for 2 days with significantly reduced flow. She stopped taking oral contraceptives 1 year after the birth of her son. Her vital signs are within normal limits. Speculum examination shows a normal vagina and cervix. The uterus is normal in size, and no adnexal masses are palpated. Which of the following is the most appropriate next step in management?
- A. Hysteroscopy with potential adhesiolysis (Correct Answer)
- B. Measurement of serum FSH and LH concentrations
- C. Measurement of antisperm antibody concentration
- D. Dilation and curettage
- E. Estrogen/progestin withdrawal test
Surgical management of PPH Explanation: ***Hysteroscopy with potential adhesiolysis***
- The patient's history of **postpartum hemorrhage** requiring D&C, followed by significantly **reduced menstrual flow**, strongly suggests **intrauterine adhesions (Asherman's syndrome)**.
- **Hysteroscopy** is the definitive diagnostic and therapeutic procedure for Asherman's syndrome, allowing direct visualization and surgical lysis of adhesions.
*Measurement of serum FSH and LH concentrations*
- This step is typically used to evaluate **ovarian reserve** or **hypothalamic-pituitary-ovarian axis dysfunction** in cases of anovulation or primary ovarian insufficiency.
- Given the patient's regular menstrual cycles, ovulatory dysfunction is less likely to be the primary cause of her infertility symptoms.
*Measurement of antisperm antibody concentration*
- **Antisperm antibodies** are a cause of infertility in a small percentage of couples, affecting sperm function or fertilization.
- This test is usually pursued after more common causes of infertility have been ruled out, as there are stronger indicators for Asherman's syndrome in this case.
*Dilation and curettage*
- A **D&C** was previously performed and is the likely iatrogenic cause of her current symptoms (Asherman's syndrome).
- Performing another D&C without addressing the adhesions would likely worsen her condition and lead to further scarring.
*Estrogen/progestin withdrawal test*
- This test assesses the integrity of the **endometrium** and the presence of sufficient endogenous estrogen if a patient has **amenorrhea**, as bleeding after withdrawal indicates a responsive endometrium.
- The patient has regular, albeit reduced, menstrual cycles, making this test less relevant for her specific symptoms.
Surgical management of PPH US Medical PG Question 10: A 25-year-old woman comes to the emergency department one hour after the sudden onset of diffuse abdominal pain and nausea. She has no history of serious illness. Menses occur at regular 27-day intervals and last 4 to 6 days with moderate flow. Her last menstrual period was 6 weeks ago. She is sexually active with two sexual partners and uses oral contraceptive pills inconsistently. She appears pale and diaphoretic. Her temperature is 37.7°C (99.9°F), pulse is 120/min, respirations are 20/min, and blood pressure is 85/70 mm Hg. Abdominal examination shows diffuse abdominal tenderness. Pelvic examination shows a normal appearing vagina, cervix, and uterus, with right adnexal tenderness. Her hemoglobin concentration is 13 g/dL, leukocyte count is 10,000/mm3, and platelet count is 350,000/mm3. Results of a pregnancy test are pending. Which of the following is the most appropriate next step in management?
- A. Perform exploratory laparoscopy
- B. Perform pelvic ultrasound
- C. Perform CT scan of the abdomen and pelvis with contrast
- D. Administer intravenous normal saline fluids (Correct Answer)
- E. Transfuse O negative packed red blood cells
Surgical management of PPH Explanation: ***Administer intravenous normal saline fluids***
- The patient presents with classic signs of **hypovolemic shock**: sudden onset of severe abdominal pain, nausea, pallor, diaphoresis, tachycardia (120/min), and hypotension (85/70 mm Hg).
- Immediate administration of **intravenous fluids** is crucial to restore blood volume and stabilize her hemodynamics before further diagnostic or surgical interventions.
*Perform exploratory laparoscopy*
- While exploratory laparoscopy may ultimately be necessary if an **ectopic pregnancy rupture** is suspected, it is not the *immediate* next step before attempting hemodynamic stabilization.
- Performing surgery on a patient in **unresuscitatable shock** significantly increases morbidity and mortality.
*Perform pelvic ultrasound*
- A pelvic ultrasound is a valuable diagnostic tool, especially if an **ectopic pregnancy** is suspected given her missed period, sexual activity, and inconsistent contraception.
- However, in a patient with signs of **hemodynamic instability**, performing an ultrasound before fluid resuscitation wastes critical time and could worsen her condition.
*Perform CT scan of the abdomen and pelvis with contrast*
- A CT scan can provide detailed imaging of the abdomen and pelvis but is **less appropriate** than a pelvic ultrasound for initial evaluation of suspected gynecological causes of acute abdominal pain in a young woman.
- Furthermore, administering contrast to a patient in **shock** could exacerbate her condition and delay immediate life-saving interventions.
*Transfuse O negative packed red blood cells*
- Although the patient's symptoms strongly suggest **internal hemorrhage** (e.g., ruptured ectopic pregnancy), her initial hemoglobin (13 g/dL) is within the normal range.
- While blood products may eventually be needed, initial management of hypovolemic shock prioritizes **crystalloid fluid resuscitation** until blood products can be prepared and cross-matched, unless massive transfusion protocol is activated for severe, ongoing hemorrhage.
More Surgical management of PPH US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.