Definition and classification US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Definition and classification. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Definition and classification US Medical PG Question 1: A 27-year-old woman, gravida 2, para 1, at 26 weeks' gestation comes to the emergency department because of vaginal bleeding and epistaxis for the past 2 days. She missed her last prenatal visit 2 weeks ago. Physical examination shows blood in the posterior pharynx and a uterus consistent in size with 23 weeks' gestation. Her hemoglobin concentration is 7.2 g/dL. Ultrasonography shows an intrauterine pregnancy with a small retroplacental hematoma and absent fetal cardiac activity. Further evaluation is most likely to show which of the following findings?
- A. Decreased fibrinogen concentration (Correct Answer)
- B. Increased antithrombin concentration
- C. Increased factor V concentration
- D. Increased platelet count
- E. Decreased prothrombin time
Definition and classification Explanation: ***Decreased fibrinogen concentration***
- The patient's presentation with **vaginal bleeding**, **epistaxis**, a **small retroplacental hematoma**, and **absent fetal cardiac activity** strongly suggests **abruptio placentae** complicated by **disseminated intravascular coagulation (DIC)**.
- In DIC, widespread activation of the **coagulation cascade** leads to consumption of clotting factors, including **fibrinogen**, resulting in **decreased plasma levels**.
*Increased antithrombin concentration*
- **Antithrombin** is a natural anticoagulant that inhibits activated clotting factors; its concentration is typically **decreased** in DIC due to its consumption in an attempt to control widespread coagulation.
- An increase in antithrombin would generally **reduce** clot formation, which is contrary to the hypercoagulable state seen initially in DIC.
*Increased factor V concentration*
- **Factor V** is a procoagulant factor that is **consumed** during DIC, leading to **decreased** rather than increased concentrations.
- Increased factor V would promote clotting, which is overridden by the massive consumption of factors and platelets in DIC.
*Increased platelet count*
- **Platelets** are actively consumed in the widespread microthrombi formation characteristic of DIC, leading to **thrombocytopenia** (decreased platelet count), not an increase.
- An increased platelet count would be protective against bleeding, which is not the case here.
*Decreased prothrombin time*
- **Prothrombin time (PT)** measures the extrinsic and common coagulation pathways; in DIC, the consumption of coagulation factors, including **prothrombin**, leads to a **prolonged (increased)** PT, not a decreased one.
- A decreased PT would indicate a hypercoagulable state with enhanced clotting factor activity, which is eventually exhausted in DIC.
Definition and classification US Medical PG Question 2: A 29-year-old G2P2 female gives birth to a healthy baby boy at 39 weeks of gestation via vaginal delivery. Immediately after the delivery of the placenta, she experiences profuse vaginal hemorrhage. Her prior birthing history is notable for an emergency cesarean section during her first pregnancy. She did not receive any prenatal care during either pregnancy. Her past medical history is notable for obesity and diabetes mellitus, which is well controlled on metformin. Her temperature is 99.0°F (37.2°C), blood pressure is 95/50 mmHg, pulse is 125/min, and respirations are 22/min. On physical examination, the patient is in moderate distress. Her extremities are pale, cool, and clammy. Capillary refill is delayed. Which of the following is the most likely cause of this patient’s bleeding?
- A. Chorionic villi invading into the myometrium
- B. Placental implantation over internal cervical os
- C. Chorionic villi attaching to the decidua basalis
- D. Chorionic villi invading into the serosa
- E. Chorionic villi attaching to the myometrium (Correct Answer)
Definition and classification Explanation: ***Chorionic villi attaching to the myometrium***
- This describes **placenta accreta**, where the **chorionic villi adhere directly to the myometrium** without invading beyond it. This condition is strongly associated with a history of **prior C-sections**, as the scar tissue increases the risk of abnormal placental implantation.
- The profuse hemorrhage immediately following placental delivery, despite the placenta being delivered, suggests a problem with normal placental separation from the uterine wall. **Placenta accreta** can lead to massive postpartum hemorrhage when the placenta attempts to separate, tearing the maternal vessels.
*Chorionic villi invading into the myometrium*
- This describes **placenta increta**, where the **chorionic villi invade deeper into the myometrium**. While also causing severe hemorrhage, the term "attaching to the myometrium" (accreta) is a more common and slightly less severe form often seen with prior C-sections.
- Both accreta and increta present similarly with hemorrhage, but accreta is the initial and most common form of abnormal adherence to the myometrium.
*Placental implantation over internal cervical os*
- This describes **placenta previa**, which is characterized by **painless vaginal bleeding** typically in the **second or third trimester**, before delivery.
- While a prior C-section is a risk factor for placenta previa, the hemorrhage in this case occurred *after* the delivery of the placenta, not before or during labor, ruling out active previa.
*Chorionic villi invading into the serosa*
- This describes **placenta percreta**, the most severe form where **chorionic villi invade through the myometrium and into the uterine serosa**, potentially involving adjacent organs.
- While it causes massive hemorrhage, "attaching to" or even "invading into" the myometrium (accreta/increta) are more probable, given the description, than invasion *through* to the serosa, though all are part of the placenta accreta spectrum.
*Chorionic villi invading beyond the serosa*
- This is an alternative description for **placenta percreta**, indicating invasion through the uterus and potentially into surrounding structures like the bladder.
- While this is a severe cause of postpartum hemorrhage, the provided option "Chorionic villi attaching to the myometrium" (placenta accreta) is the most common form of abnormally adherent placenta in the spectrum and is highly consistent with the patient's history of prior C-section and the clinical presentation of hemorrhage after placental delivery.
Definition and classification US Medical PG Question 3: A 30-year-old woman, gravida 2, para 1, at 42 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been complicated by gestational diabetes, for which she has been receiving insulin injections. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 90/min, respirations are 18/min, and blood pressure is 135/80 mm Hg. The fetal heart rate tracing shows a baseline heart rate of 145/min and moderate variation with frequent accelerations and occasional early decelerations. She undergoes an elective repeat lower segment transverse cesarean section with complete removal of the placenta. Shortly after the operation, she starts having heavy uterine bleeding with passage of clots. Examination shows a soft uterus on palpation. Her bleeding continues despite fundal massage and the use of packing, oxytocin, misoprostol, and carboprost. Her pulse rate is now 120/min, respirations are 20/min, and blood pressure is 90/70 mm Hg. Her hemoglobin is 8 g/dL, hematocrit is 24%, platelet count is 120,000 mm3, prothrombin time is 11 seconds, and partial thromboplastin time is 30 seconds. Mass transfusion protocol is activated and a B-Lynch uterine compression suture is placed to control her bleeding. Which of the following is the mostly likely cause of her postpartum complication?
- A. Adherent placenta to myometrium
- B. Uterine inversion
- C. Infection of the endometrial lining of the uterus
- D. Uterine rupture
- E. Lack of uterine muscle contraction (Correct Answer)
Definition and classification Explanation: ***Lack of uterine muscle contraction***
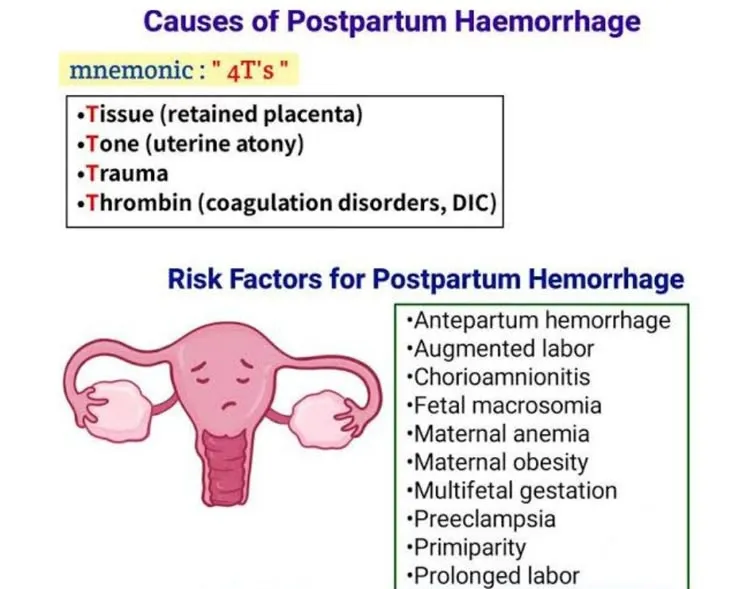
- The presentation of a **soft uterus** on palpation and continued severe bleeding despite fundal massage and uterotonics (**oxytocin, misoprostol, carboprost**) is highly indicative of **uterine atony**, which is a lack of effective uterine muscle contraction.
- Uterine atony is the most common cause of **postpartum hemorrhage**, and risk factors include **macrosomia** (due to gestational diabetes), **multiparity**, and a prolonged labor or rapid delivery, though the latter two are less clear here.
*Adherent placenta to myometrium*
- While a history of prior C-section and **macrosomia** (due to gestational diabetes) could increase the risk of an **abnormally adherent placenta** (accreta, increta, percreta), the description notes **complete removal of the placenta**.
- If the placenta were morbidly adherent and not completely removed, bleeding would likely stem from retained placental tissue, and this would typically be explicitly noted or suspected due to difficulty with manual removal.
*Uterine inversion*
- **Uterine inversion** involves the uterus turning inside out, which would present with a **mass protruding from the vagina** or a visible inversion of the fundus upon examination, along with sudden onset of severe pain and shock.
- The description of a **soft uterus** and an absence of a physical description of uterine inversion makes this diagnosis less likely.
*Infection of the endometrial lining of the uterus*
- **Endometritis** (infection of the endometrial lining) typically presents with fever, foul-smelling lochia, uterine tenderness, and prolonged postpartum bleeding, usually occurring a few days postpartum rather than immediately following delivery.
- The acute, massive hemorrhage immediately following delivery, coupled with a normal initial temperature, does not align with the typical presentation of endometritis.
*Uterine rupture*
- **Uterine rupture** is a serious complication, especially with a history of prior C-section, but it typically presents with **sudden severe abdominal pain**, fetal heart rate abnormalities (if it occurs before delivery), and **hemodynamic instability**, often with cessation of contractions.
- While the patient is hemodynamically unstable, the primary issue described is heavy uterine bleeding with a soft uterus, and no mention of severe abdominal pain or clear signs of rupture during the C-section make uterine atony a more direct explanation for the described symptoms.
Definition and classification US Medical PG Question 4: A 32-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the emergency department because of vaginal bleeding for the past hour. The patient reports that she felt contractions prior to the onset of the bleeding, but the contractions stopped after the bleeding started. She also has severe abdominal pain. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 110/min, respirations are 17/min, and blood pressure is 90/60 mm Hg. Examination shows diffuse abdominal tenderness with no rebound or guarding; no contractions are felt. The fetal heart rate shows recurrent variable decelerations. Which of the following is the most likely diagnosis?
- A. Uterine inertia
- B. Amniotic fluid embolism
- C. Uterine rupture (Correct Answer)
- D. Vasa previa
- E. Abruptio placentae
Definition and classification Explanation: ***Uterine rupture***
- The patient's history of a prior **cesarean section**, sudden onset of **vaginal bleeding** and **severe abdominal pain**, resolution of contractions, and signs of **hypovolemic shock** (tachycardia, hypotension) coupled with fetal distress (variable decelerations) are highly indicative of uterine rupture.
- Diffuse abdominal tenderness without rebound or guarding, and no palpable contractions, are also consistent with rupture.
*Uterine inertia*
- This condition is characterized by **weak or uncoordinated uterine contractions** leading to prolonged labor, but it does not typically present with acute vaginal bleeding, sudden severe abdominal pain, or hypovolemic shock.
- Fetal distress in uterine inertia would more likely be due to prolonged labor rather than acute compromise following a sudden event.
*Amniotic fluid embolism*
- This is a rare, life-threatening obstetric emergency characterized by sudden **cardiovascular collapse, respiratory distress**, and **coagulopathy**, often occurring during labor or immediately postpartum.
- While it can cause fetal distress, vaginal bleeding and severe abdominal pain are not primary presenting symptoms.
*Vasa previa*
- Characterized by **painless vaginal bleeding** when fetal vessels within the membranes cross the internal cervical os, making them vulnerable to rupture during cervical dilation or amniotomy.
- The bleeding is typically fetal blood, and fetal distress occurs rapidly, but the mother would not experience severe abdominal pain or signs of hypovolemic shock unless the bleeding is substantial and prolonged.
*Abruptio placentae*
- This involves the **premature separation of the placenta**, causing painful vaginal bleeding, uterine tenderness, and frequent, strong contractions.
- While it can cause hypovolemic shock and fetal distress, the description of contractions stopping after bleeding started, along with a previous C-section scar, points more specifically to uterine rupture rather than an abruption.
Definition and classification US Medical PG Question 5: A 37-year-old woman, gravida 4, para 3, at 35 weeks' gestation is admitted to the hospital in active labor. Her three children were delivered by Cesarean section. One hour after vaginal delivery, the placenta is not delivered. Manual separation of the placenta leads to profuse vaginal bleeding. Her pulse is 122/min and blood pressure is 90/67 mm Hg. A firm, nontender uterine fundus is palpated at the level of the umbilicus. Hemoglobin is 8.3 g/dL and platelet count is 220,000/mm3. Activated partial thromboplastin time and prothrombin time are within normal limits. Which of the following is the most likely underlying mechanism of this patient's postpartum bleeding?
- A. Defective decidual layer of the placenta (Correct Answer)
- B. Impaired uterine contractions
- C. Rupture of the fetal vessels
- D. Consumption of intravascular clotting factors
- E. Rupture of the uterine wall
Definition and classification Explanation: **Defective decidual layer of the placenta**
- The patient's history of three previous Cesarean sections significantly increases the risk of **placenta accreta**, where the **placenta abnormally invades the uterine wall** due to a defective decidual layer.
- The inability to deliver the placenta an hour after vaginal delivery and subsequent profuse bleeding upon manual separation are classic signs of **placenta accreta spectrum**, as the placenta is morbidly adherent.
*Impaired uterine contractions*
- This would typically present as a **boggy, soft uterus** on palpation, rather than the "firm, nontender uterine fundus" described.
- Uterine atony is the most common cause of postpartum hemorrhage, but it is ruled out by the firm fundus and lack of uterine relaxation.
*Rupture of the fetal vessels*
- This usually occurs *before* or *during* delivery, presenting as **fetal distress** or **vaginal bleeding originating from the fetus** (e.g., vasa previa), which is not the primary issue here after labor and delivery.
- The profuse bleeding is *maternal* and occurs *after* delivery due to placental adherence, not fetal vessel rupture.
*Consumption of intravascular clotting factors*
- While severe hemorrhage can eventually lead to **disseminated intravascular coagulation (DIC)** and consumption of clotting factors, the patient's normal aPTT and PT indicate that coagulopathy is not the *initial* underlying mechanism of bleeding.
- This would be a *secondary complication* rather than the primary cause of undelivered placenta and initial hemorrhage.
*Rupture of the uterine wall*
- Uterine rupture typically presents with **acute, severe abdominal pain**, **fetal distress** (if it occurs before delivery), and **loss of uterine tone or palpation of fetal parts outside the uterus**.
- Although previous C-sections increase the risk, the firm uterine fundus and the specific problem with placental non-separation point away from uterine rupture as the primary cause of hemorrhage here.
Definition and classification US Medical PG Question 6: A 34-year-old G3P2 is admitted to the hospital after being physically assaulted by her husband. She developed severe vaginal bleeding and abdominal pain. She is at 30 weeks gestation. Her previous pregnancies were uncomplicated, as has been the course of the current pregnancy. The vital signs are as follows: blood pressure, 80/50 mmHg; heart rate, 117/min and irregular; respiratory rate, 20/min; and temperature, 36.2℃ (97.1). The fetal heart rate is 103/min. On physical examination, the patient is pale and lethargic. Abdominal palpation reveals severe uterine tenderness and tetanic contractions. The perineum is grossly bloody. There are no vaginal or cervical lesions. There is active heavy bleeding with blood clots passing through the cervix. An ultrasound shows a retroplacental hematoma with a volume of approximately 400 ml.
Laboratory workup shows the following findings:
Red blood cells count: 3.0 millions/mL
Hb%: 7.2 g/dL
Platelet count: 61,000/mm3
Prothrombin time: 310 seconds (control 20 seconds)
Partial prothrombin time: 420 seconds
Serum fibrinogen: 16 mg/dL
Elevated levels of which of the following laboratory markers is characteristic for this patient’s complication?
- A. C-reactive protein
- B. D-dimer (Correct Answer)
- C. Creatinine
- D. Pro-brain natriuretic peptide
- E. Procalcitonin
Definition and classification Explanation: *** **D-dimer***
- This patient's presentation with **severe vaginal bleeding**, **abdominal pain**, **uterine tenderness**, **tetanic contractions**, and **fetal distress** following trauma, along with the ultrasound finding of a **retroplacental hematoma**, is highly suggestive of **abruptio placentae**.
- The abnormal coagulation panel (low platelets, prolonged PT/PTT, low fibrinogen) indicates **disseminated intravascular coagulation (DIC)**, a common complication of severe placental abruption due to extensive activation of the coagulation cascade and subsequent breakdown of clots. **D-dimer levels** are characteristically **elevated** in DIC as they are degradation products of **fibrin** from enhanced fibrinolysis.
*C-reactive protein*
- **C-reactive protein (CRP)** is an **acute-phase reactant** primarily elevated in response to **inflammation** or **infection**.
- While trauma could induce some inflammation, very high CRP levels are not specific for **DIC** or the direct complications of **placental abruption** described.
*Creatinine*
- **Creatinine** is a marker of **renal function**. While severe shock and hypoperfusion from significant bleeding could lead to **acute kidney injury** and elevated creatinine, it is not a direct or characteristic marker of the **coagulopathy** or **DIC** seen in this patient.
- The primary issue presented is one of **bleeding and coagulation abnormalities**, not primarily renal dysfunction.
*Pro-brain natriuretic peptide*
- **Pro-brain natriuretic peptide (pro-BNP)** is a biomarker primarily used to assess **cardiac stretch** and **heart failure**.
- There are no clinical signs or symptoms presented that suggest **cardiac dysfunction** as the primary or most characteristic complication in this setting.
*Procalcitonin*
- **Procalcitonin** is a biomarker that is significantly elevated in **bacterial infections** and **sepsis**.
- Although the patient's condition is critical, the clinical picture strongly points towards **hemorrhage** and **DIC** due to **placental abruption** rather than a primary **bacterial infection**.
Definition and classification US Medical PG Question 7: A 30-year-old woman, gravida 2, para 1, abortus 1, comes to the physician because of failure to conceive for 12 months. She is sexually active with her husband 2–3 times per week. Her first child was born at term after vaginal delivery 2 years ago. At that time, the postpartum course was complicated by hemorrhage from retained placental products, and the patient underwent dilation and curettage. Menses occur at regular 28-day intervals and previously lasted for 5 days with normal flow, but now last for 2 days with significantly reduced flow. She stopped taking oral contraceptives 1 year after the birth of her son. Her vital signs are within normal limits. Speculum examination shows a normal vagina and cervix. The uterus is normal in size, and no adnexal masses are palpated. Which of the following is the most appropriate next step in management?
- A. Hysteroscopy with potential adhesiolysis (Correct Answer)
- B. Measurement of serum FSH and LH concentrations
- C. Measurement of antisperm antibody concentration
- D. Dilation and curettage
- E. Estrogen/progestin withdrawal test
Definition and classification Explanation: ***Hysteroscopy with potential adhesiolysis***
- The patient's history of **postpartum hemorrhage** requiring D&C, followed by significantly **reduced menstrual flow**, strongly suggests **intrauterine adhesions (Asherman's syndrome)**.
- **Hysteroscopy** is the definitive diagnostic and therapeutic procedure for Asherman's syndrome, allowing direct visualization and surgical lysis of adhesions.
*Measurement of serum FSH and LH concentrations*
- This step is typically used to evaluate **ovarian reserve** or **hypothalamic-pituitary-ovarian axis dysfunction** in cases of anovulation or primary ovarian insufficiency.
- Given the patient's regular menstrual cycles, ovulatory dysfunction is less likely to be the primary cause of her infertility symptoms.
*Measurement of antisperm antibody concentration*
- **Antisperm antibodies** are a cause of infertility in a small percentage of couples, affecting sperm function or fertilization.
- This test is usually pursued after more common causes of infertility have been ruled out, as there are stronger indicators for Asherman's syndrome in this case.
*Dilation and curettage*
- A **D&C** was previously performed and is the likely iatrogenic cause of her current symptoms (Asherman's syndrome).
- Performing another D&C without addressing the adhesions would likely worsen her condition and lead to further scarring.
*Estrogen/progestin withdrawal test*
- This test assesses the integrity of the **endometrium** and the presence of sufficient endogenous estrogen if a patient has **amenorrhea**, as bleeding after withdrawal indicates a responsive endometrium.
- The patient has regular, albeit reduced, menstrual cycles, making this test less relevant for her specific symptoms.
Definition and classification US Medical PG Question 8: A 31-year-old G6P6 woman with a history of fibroids gives birth to twins via vaginal delivery. Her pregnancy was uneventful, and she reported having good prenatal care. Both placentas are delivered immediately after the birth. The patient continues to bleed significantly over the next 20 minutes. Her temperature is 97.0°F (36.1°C), blood pressure is 124/84 mmHg, pulse is 95/min, respirations are 16/min, and oxygen saturation is 98% on room air. Continued vaginal bleeding is noted. Which of the following is the most appropriate initial step in management?
- A. Oxytocin
- B. Blood product transfusion
- C. Uterine artery embolization
- D. Hysterectomy
- E. Bimanual massage (Correct Answer)
Definition and classification Explanation: ***Bimanual massage***
- The patient is experiencing **postpartum hemorrhage (PPH)**, indicated by significant bleeding post-delivery. **Uterine atony** is the most common cause of PPH, and bimanual massage helps stimulate uterine contractions to reduce bleeding.
- This is a **first-line, non-pharmacological intervention** that can be rapidly initiated to manage uterine atony.
*Oxytocin*
- While **oxytocin** is a uterotonic agent used to treat PPH, the initial step is typically **bimanual massage** to physically stimulate the uterus while preparing for medication administration.
- Oxytocin infusion would be administered concurrent with or immediately following bimanual massage, but manual compression is often initiated first.
*Blood product transfusion*
- Blood product transfusion is indicated for significant blood loss and hemodynamic instability, but it is a **supportive measure** rather than an initial intervention to stop the bleeding.
- The patient's current **blood pressure (124/84 mmHg)** and **pulse (95/min)** do not immediately suggest severe hypovolemic shock requiring immediate transfusion as the *first* step before attempting to control the source of bleeding.
*Uterine artery embolization*
- **Uterine artery embolization** is a highly invasive procedure typically reserved for cases where conservative measures, including uterotonic agents and bimanual compression, have failed to control PPH.
- It is not an appropriate initial step, as it requires specialized equipment and personnel and would delay immediate management of active bleeding.
*Hysterectomy*
- **Hysterectomy** is a last-resort intervention for intractable PPH that cannot be controlled by all other methods, including uterotonics, uterine massage, and other surgical or interventional radiology techniques.
- It is a highly invasive procedure with significant morbidity and is not considered an initial management step.
Definition and classification US Medical PG Question 9: Two days after being admitted to the hospital because of severe peripartum vaginal bleeding during a home birth, a 40-year-old woman, gravida 3, para 3, has a 30-second generalized convulsive seizure followed by unconsciousness. Prior to the event she complained of acute onset of sweating and uncontrollable shivering. She was hemodynamically unstable and required several liters of intravenous fluids and 5 units of packed red blood cells in the intensive care unit. The patient's two prior pregnancies, at ages 33 and 35, were uncomplicated. She is otherwise healthy. Prior to admission, her only medication was a daily prenatal vitamin. Temperature is 37.5°C (99.5°F), pulse is 120/min, respirations are 18/min, blood pressure is 101/61 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Examination shows very little milk expression from the breasts bilaterally. Finger-stick glucose level is 36 mg/dL. Which of the following is the most likely underlying cause of this patient's condition?
- A. Lactotrophic adenoma
- B. Hypothalamic infarction
- C. Pituitary ischemia (Correct Answer)
- D. Adrenal hemorrhage
- E. Hypoactive thyroid
Definition and classification Explanation: ***Pituitary ischemia***
- The patient's history of **severe peripartum hemorrhage** followed by **hypotension** and **seizure** is highly suggestive of **Sheehan syndrome**, which is caused by pituitary ischemia and necrosis.
- The inability to lactate (**little milk expression**) and **hypoglycemia** (finger-stick glucose 36 mg/dL) are consistent with deficiencies of **prolactin** and **adrenocorticotropic hormone (ACTH)**, respectively, due to pituitary damage.
*Lactotrophic adenoma*
- A lactotrophic adenoma would typically cause **hyperprolactinemia** leading to **galactorrhea** (excessive milk production), not decreased milk expression.
- While it can cause headaches and visual field defects, it does not explain the peripartum onset with hemorrhage or the subsequent hypoglycemia.
*Hypothalamic infarction*
- While hypothalamic damage can lead to endocrine dysfunction, an isolated hypothalamic infarction is a less common cause of this constellation of symptoms immediately following severe hemorrhage.
- **Pituitary infarction** is a more direct and common consequence of profound peripartum hypotension.
*Adrenal hemorrhage*
- **Adrenal hemorrhage** can lead to adrenal insufficiency with symptoms like hypotension, hypoglycemia, and shock.
- However, it does not explain the specific symptom of **agalactorrhea** (little milk expression), which points to pituitary involvement.
*Hypoactive thyroid*
- A **hypoactive thyroid (hypothyroidism)** can cause fatigue, bradycardia, and sometimes hypoglycemia, but it typically does not present with an acute seizure or agalactorrhea in the immediate postpartum period following hemorrhage.
- The acute presentation here is more consistent with a sudden and severe endocrine insult affecting multiple axes.
Definition and classification US Medical PG Question 10: A 36-year-old primigravid woman at 34 weeks' gestation comes to the physician because of a 1-week history of upper abdominal discomfort, nausea, and malaise. She had a mild upper respiratory tract infection a week ago. She has a 10-year history of polycystic ovarian syndrome and a 3-year history of hypertension. Her medications include metformin, labetalol, folic acid, and a multivitamin. Her pulse is 92/min, respirations are 18/min, and blood pressure is 147/84 mm Hg. Examination shows a nontender uterus consistent in size with a 34-week gestation. There is mild tenderness of the right upper quadrant of the abdomen. The fetal heart rate is reactive with no decelerations. Which of the following is the most appropriate next step in management?
- A. Reassurance and follow-up
- B. Serum transaminase levels and platelet count (Correct Answer)
- C. Serum bile acid levels
- D. HBsAg and IgM anti-HBc serology
- E. Stool antigen assay for H. pylori
Definition and classification Explanation: ***Serum transaminase levels and platelet count***
- The patient presents with symptoms such as **upper abdominal discomfort**, nausea, malaise, and **mild right upper quadrant tenderness**, along with a history of **hypertension** in pregnancy, raising concern for **preeclampsia with severe features** or **HELLP syndrome**.
- **Elevated liver transaminases** and **thrombocytopenia (low platelet count)** are hallmarks of HELLP syndrome, which requires urgent evaluation and management.
*Reassurance and follow-up*
- Given the concerning symptoms and risk factors, simply reassuring the patient without further investigation would be **inappropriate** and could lead to delayed diagnosis and potential harm.
- The symptoms described are not typical minor complaints of pregnancy and warrant a prompt workup.
*Serum bile acid levels*
- Elevated serum bile acid levels are primarily indicative of **intrahepatic cholestasis of pregnancy (ICP)**, which typically presents with **pruritus** (itching), especially on the palms and soles, without significant right upper quadrant pain or other systemic symptoms seen here.
- While ICP can cause some abdominal discomfort, the constellation of symptoms in this patient points more strongly towards preeclampsia/HELLP.
*HBsAg and IgM anti-HBc serology*
- These tests are used to diagnose **Hepatitis B infection**. While hepatitis could cause similar symptoms like nausea and abdominal discomfort, there is no specific risk factor or clinical sign (e.g., jaundice, dark urine) in this patient to prioritize hepatitis screening as the immediate next step over evaluating for preeclampsia/HELLP.
- The symptoms are more consistent with pregnancy-related hypertensive disorders.
*Stool antigen assay for H. pylori*
- This assay is used to diagnose **Helicobacter pylori infection**, which can cause gastritis or peptic ulcer disease.
- While H. pylori can cause upper abdominal discomfort and nausea, the patient's existing hypertension, late-stage pregnancy, and lack of symptoms specific to gastritis (e.g., burning pain, response to antacids) make preeclampsia/HELLP a more pressing concern.
More Definition and classification US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.