Blood product replacement strategies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Blood product replacement strategies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Blood product replacement strategies US Medical PG Question 1: A 36-year-old woman is brought to the emergency department 20 minutes after being involved in a high-speed motor vehicle collision. On arrival, she is unconscious. Her pulse is 140/min, respirations are 12/min and shallow, and blood pressure is 76/55 mm Hg. 0.9% saline infusion is begun. A focused assessment with sonography shows blood in the left upper quadrant of the abdomen. Her hemoglobin concentration is 7.6 g/dL and hematocrit is 22%. The surgeon decided to move the patient to the operating room for an emergent explorative laparotomy. Packed red blood cell transfusion is ordered prior to surgery. However, a friend of the patient asks for the transfusion to be held as the patient is a Jehovah's Witness. The patient has no advance directive and there is no documentation showing her refusal of blood transfusions. The patient's husband and children cannot be contacted. Which of the following is the most appropriate next best step in management?
- A. Administer hydroxyethyl starch
- B. Transfusion of packed red blood cells (Correct Answer)
- C. Consult hospital ethics committee
- D. Administer high-dose iron dextran
Blood product replacement strategies Explanation: ***Transfusion of packed red blood cells***
- This patient is in **hemorrhagic shock** (tachycardia, hypotension, low hemoglobin, and hematocrit with evidence of active bleeding), requiring emergent blood transfusion to prevent irreversible organ damage and death.
- In an **emergency setting** with an **unconscious patient** and **no documented refusal** of blood products, the principle of **presumed consent** for life-saving treatment takes precedence, especially when next of kin cannot be reached.
*Administer hydroxyethyl starch*
- **Colloids** like hydroxyethyl starch can temporarily increase intravascular volume but do not provide oxygen-carrying capacity, which is critically needed for a patient with severe anemia and hemorrhagic shock.
- While useful for volume expansion, it is **not a substitute for blood products** in severe bleeding and can have adverse effects such as kidney injury.
*Consult hospital ethics committee*
- Consulting an ethics committee is appropriate for **complex ethical dilemmas** when there is time for deliberation and the patient's life is not in immediate danger.
- In this acute, life-threatening emergency, **delaying treatment** to consult an ethics committee would jeopardize the patient's life and is not appropriate.
*Administer high-dose iron dextran*
- **Iron dextran** is used to treat iron-deficiency anemia and works by supporting red blood cell production over several days to weeks.
- It is **ineffective in acute hemorrhagic shock** where immediate restoration of oxygen-carrying capacity is required.
Blood product replacement strategies US Medical PG Question 2: A 27-year-old woman, gravida 3, para 2, at 41 weeks' gestation is admitted to the hospital in active labor. Her pregnancy has been uncomplicated. Both of her prior children were delivered by vaginal birth. She has a history of asthma. Current medications include iron and vitamin supplements. After a prolonged labor, she undergoes vaginal delivery. Shortly afterwards, she begins to have heavy vaginal bleeding with clots. Her temperature is 37.2°C (98.9°F), pulse is 90/min, respirations are 17/min, and blood pressure is 130/72 mm Hg. Examination shows a soft, enlarged, and boggy uterus on palpation. Laboratory studies show:
Hemoglobin 10.8 g/dL
Hematocrit 32.3%
Leukocyte Count 9,000/mm3
Platelet Count 140,000/mm3
Prothrombin time 14 seconds
Partial thromboplastin time 38 seconds
Her bleeding continues despite bimanual uterine massage and administration of oxytocin. Which of the following is the most appropriate next step in management?
- A. Administer methylergonovine (Correct Answer)
- B. Transfuse blood
- C. Perform hysterectomy
- D. Administer carboprost tromethamine
- E. Perform curettage
Blood product replacement strategies Explanation: ***Administer methylergonovine***
- The patient is likely experiencing **postpartum hemorrhage (PPH)** due to **uterine atony**, characterized by a soft, enlarged, and boggy uterus after delivery, with continued bleeding despite initial measures (massage, oxytocin).
- Given her history of **asthma**, carboprost tromethamine (prostaglandin F2-alpha) is **contraindicated** due to its potential to cause severe bronchospasm, making methylergonovine (an ergot alkaloid) the appropriate next uterotonic agent.
*Transfuse blood*
- While blood transfusions may eventually be necessary if bleeding is severe and leads to significant hemodynamic instability or severe anemia, it is **not the immediate next step** in managing the underlying cause of the hemorrhage (uterine atony).
- **Uterotonic agents** should be tried first to contract the uterus and stop the bleeding, as indicated by the patient's current vital signs being relatively stable (pulse 90/min, BP 130/72 mm Hg).
*Perform hysterectomy*
- **Hysterectomy** is a drastic measure considered only after all less invasive medical and surgical interventions (e.g., uterotonic agents, uterine tamponade, suturing techniques) have failed to control severe PPH.
- It would be **premature** to proceed directly to hysterectomy without attempting additional medical management for uterine atony.
*Administer carboprost tromethamine*
- **Carboprost tromethamine** is a prostaglandin analog that is effective in treating uterine atony but is **contraindicated in patients with asthma** due to its known side effect of inducing bronchospasm.
- The patient's history of asthma makes this a **dangerous option**, and an alternative uterotonic like methylergonovine should be chosen.
*Perform curettage*
- **Curettage** (removing retained placental fragments) would be appropriate if the cause of PPH was **retained placental tissue**.
- However, the examination finding of a **soft, enlarged, and boggy uterus** is characteristic of uterine atony, not retained placenta, and the initial management of atony involves uterotonic agents.
Blood product replacement strategies US Medical PG Question 3: A 34-year-old primigravida was brought to an obstetric clinic with a chief complaint of painless vaginal bleeding. She was diagnosed with placenta praevia and transfused with 2 units of whole blood. Five hours after the transfusion, she developed a fever and chills. How could the current situation be prevented?
- A. Administering prophylactic epinephrine
- B. ABO grouping and Rh typing before transfusion
- C. Transfusing leukocyte reduced blood products (Correct Answer)
- D. Performing Coombs test before transfusion
- E. Administering prophylactic immunoglobulins
Blood product replacement strategies Explanation: ***Transfusing leukocyte reduced blood products***
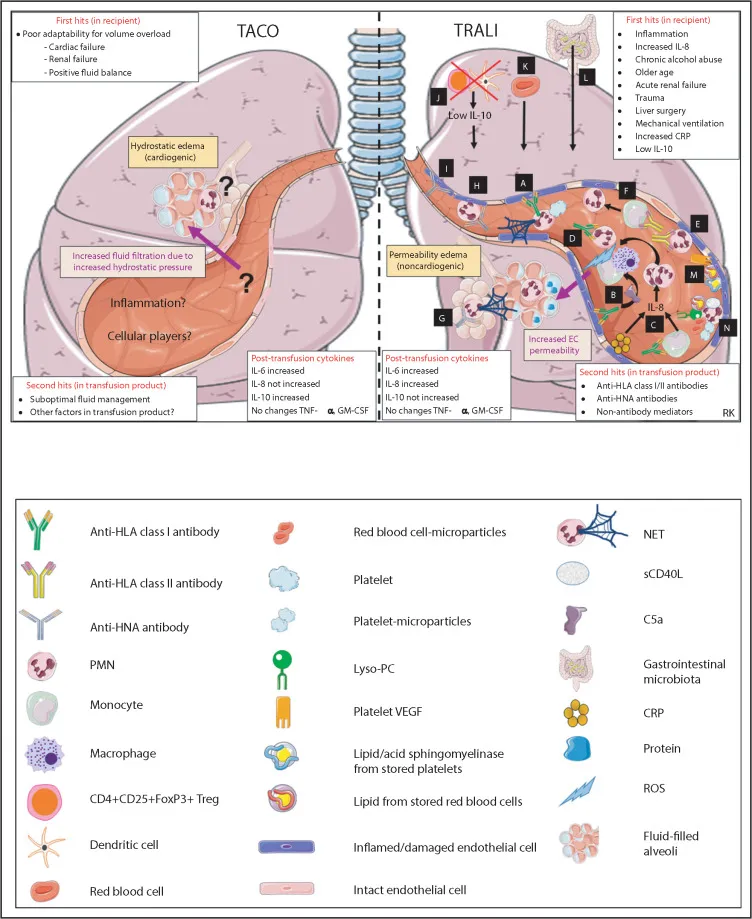
- The patient's symptoms of **fever and chills** occurring hours after transfusion are characteristic of a **febrile non-hemolytic transfusion reaction (FNHTR)**.
- FNHTRs are caused by residual **donor leukocytes** in the transfused blood product, which release **cytokines** during storage or react with recipient antibodies, and can be prevented by using **leukoreduced blood products**.
*Administering prophylactic epinephrine*
- **Epinephrine** is used to treat severe **anaphylactic and allergic reactions** but does not prevent the underlying mechanism of FNHTRs.
- Its prophylactic administration is not a standard practice for preventing transfusion reactions like FNHTRs.
*ABO grouping and Rh typing before transfusion*
- **ABO grouping and Rh typing** are crucial for preventing **acute hemolytic transfusion reactions**, which are much more severe and involve erythrocyte incompatibility.
- These tests would not prevent a **febrile non-hemolytic transfusion reaction (FNHTR)** caused by leukocyte components.
*Performing Coombs test before transfusion*
- The **Coombs test (Direct Antiglobulin Test)** detects antibodies attached to red blood cells and is primarily used to diagnose **autoimmune hemolytic anemia** or delayed hemolytic transfusion reactions.
- It does not prevent FNHTRs, which are unrelated to red blood cell incompatibility or antibody-mediated hemolysis.
*Administering prophylactic immunoglobulins*
- **Prophylactic immunoglobulins** are used in specific situations like **immunodeficiency** or **Rh incompatibility (RhoGAM)** to prevent alloimmunization, but not for preventing FNHTRs.
- This intervention would not target the mechanism leading to fever and chills caused by donor leukocyte interactions.
Blood product replacement strategies US Medical PG Question 4: A 34-year-old G5P5 woman gave birth to a healthy infant 30 minutes ago by vacuum-assisted vaginal delivery and is now experiencing vaginal bleeding. The placenta was delivered spontaneously and was intact upon examination. The infant weighed 5.2 kg and had Apgar scores of 8 and 9. No perineal tear or intentional episiotomy occurred. The patient has type 1 diabetes. She had good glycemic control throughout her pregnancy. She took a prenatal vitamin daily. Blood pressure is 135/72 mmHg, pulse is 102/min, and respirations are 18/min. Upon physical examination, the uterine fundus is soft and palpated 4 cm above the umbilicus. There are 3-cm blood clots on the patient’s bed pad. Which of the following is the next best step in management for the patient’s bleeding?
- A. Administer misoprostol
- B. Manually remove retained placental fragments
- C. Perform uterine massage and administer oxytocin (Correct Answer)
- D. Perform uterine artery embolization
- E. Perform hysterectomy
Blood product replacement strategies Explanation: ***Perform uterine massage and administer oxytocin***
- The patient's presentation of a **soft, boggy uterus** palpated 4 cm above the umbilicus after delivery, along with significant vaginal bleeding and clots, is highly indicative of **uterine atony**.
- **Uterine massage** and administration of **oxytocin** are the first-line interventions to stimulate uterine contractions and reduce bleeding by compressing placental site blood vessels.
*Administer misoprostol*
- **Misoprostol** is a prostaglandin analog that can be used for uterine atony when oxytocin is insufficient or contraindicated, but it is not the *first-line* treatment.
- Its onset of action may be slower than immediate uterine massage and IV oxytocin, which are preferred for initial management of acute uterine atony.
*Manually remove retained placental fragments*
- The question states that the **placenta was delivered spontaneously and was intact upon examination**, which makes retained placental fragments less likely as the primary cause of bleeding.
- While retained fragments can cause postpartum hemorrhage, the boggy uterus points more strongly to atony, and manual removal is indicated *after* confirming retained placental tissue.
*Perform uterine artery embolization*
- **Uterine artery embolization** is an interventional radiology procedure typically reserved for cases of postpartum hemorrhage that are refractory to conventional medical and surgical management.
- It is an invasive procedure and not the appropriate *next best step* for initial management of suspected uterine atony.
*Perform hysterectomy*
- **Hysterectomy** is a last-resort, life-saving measure for intractable postpartum hemorrhage when all other medical and surgical options have failed.
- It is a highly invasive and irreversible procedure, certainly not the *next best step* in a patient who has just begun to bleed.
Blood product replacement strategies US Medical PG Question 5: A 35-year-old male is brought into the emergency department for a trauma emergency. The emergency medical services states that the patient was wounded with a knife on his upper left thigh near the inguinal ligament. Upon examination in the trauma bay, the patient is awake and alert. His physical exam and FAST exam is normal other than the knife wound. Large bore intravenous lines are inserted into the patient for access and fluids are being administered. Pressure on the knife wound is being held by one of the physicians with adequate control of the bleeding, but the physician notices the blood was previously extravasating in a pulsatile manner. His vitals are BP 100/50, HR 110, T 97.8, RR 22. What is the next best step for this patient?
- A. CT lower extremities
- B. Radiograph lower extremities
- C. Coagulation studies and blood typing/crossmatch
- D. Tourniquet of proximal lower extremity
- E. Emergent surgery (Correct Answer)
Blood product replacement strategies Explanation: ***Emergent surgery***
- The pulsatile bleeding from a thigh wound near the inguinal ligament is highly suggestive of a major arterial injury, such as to the **femoral artery**.
- Given the potential for rapid blood loss and hemodynamic instability, **emergent surgical exploration and repair** are necessary to control the bleeding and prevent further compromise.
*CT lower extremities*
- While CT angiography could further delineate vascular injury, the presence of **active pulsatile bleeding** necessitates immediate surgical intervention rather than delaying for imaging.
- Delaying surgery for imaging risks **exsanguination** and worsening patient outcomes, especially with a blood pressure of **100/50 mmHg** and a heart rate of **110 bpm**, indicating early shock.
*Radiograph lower extremities*
- A radiograph would primarily visualize bone structures and foreign bodies but would not provide adequate information regarding the **vascular injury** and active bleeding.
- It would not change the urgent need for **surgical exploration** to address the pulsatile hemorrhage.
*Coagulation studies and blood typing/crossmatch*
- These are important preparatory steps for major surgery involving significant blood loss, but they should be carried out **concurrently with preparations for emergent surgery**, not instead of it.
- Delaying surgery to await these results would be inappropriate when facing **active arterial bleeding**.
*Tourniquet of proximal lower extremity*
- While a tourniquet can be used for temporary hemorrhage control, especially in an uncontrolled external hemorrhage, the current bleeding is being controlled by **direct pressure**.
- Applying a tourniquet could cause **ischemic damage** to the extremity if applied for too long, and for a deep stab wound, direct compression is often effective until surgical control can be achieved.
Blood product replacement strategies US Medical PG Question 6: A 22-year-old woman in the intensive care unit has had persistent oozing from the margins of wounds for 2 hours that is not controlled by pressure bandages. She was admitted to the hospital 13 hours ago following a high-speed motor vehicle collision. Initial focused assessment with sonography for trauma was negative. An x-ray survey showed opacification of the right lung field and fractures of multiple ribs, the tibia, fibula, calcaneus, right acetabulum, and bilateral pubic rami. Laboratory studies showed a hemoglobin concentration of 14.8 g/dL, leukocyte count of 10,300/mm3, platelet count of 175,000/mm3, and blood glucose concentration of 77 mg/dL. Infusion of 0.9% saline was begun. Multiple lacerations on the forehead and extremities were sutured, and fractures were stabilized. Repeat laboratory studies now show a hemoglobin concentration of 12.4 g/dL, platelet count of 102,000/mm3, prothrombin time of 26 seconds (INR=1.8), and activated partial thromboplastin time of 63 seconds. Which of the following is the next best step in management?
- A. Transfuse packed RBC
- B. Transfuse packed RBC and fresh frozen plasma in a 1:1 ratio
- C. Transfuse fresh frozen plasma and platelet concentrate in a 1:1 ratio
- D. Transfuse whole blood and administer vitamin K
- E. Transfuse packed RBC, fresh frozen plasma, and platelet concentrate in a 1:1:1 ratio (Correct Answer)
Blood product replacement strategies Explanation: ***Transfuse packed RBC, fresh frozen plasma, and platelet concentrate in a 1:1:1 ratio***
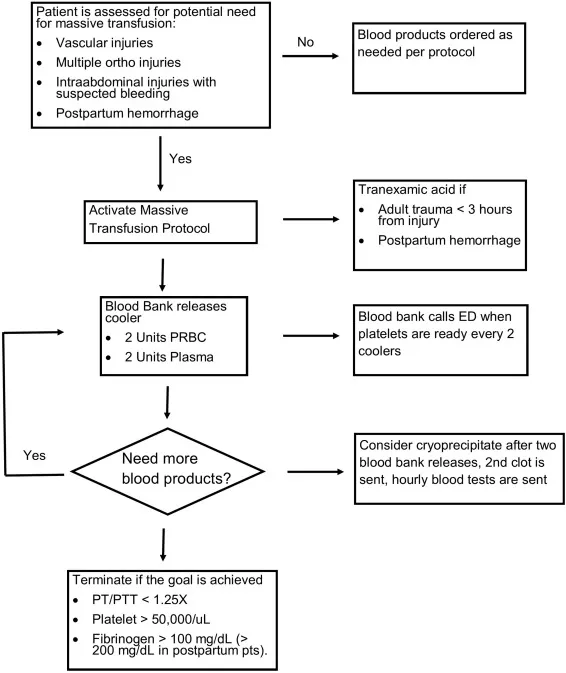
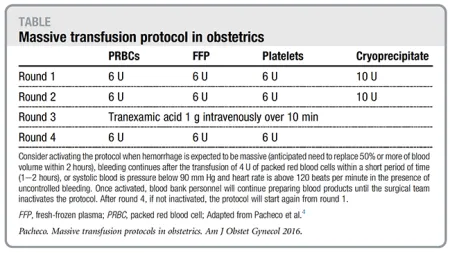
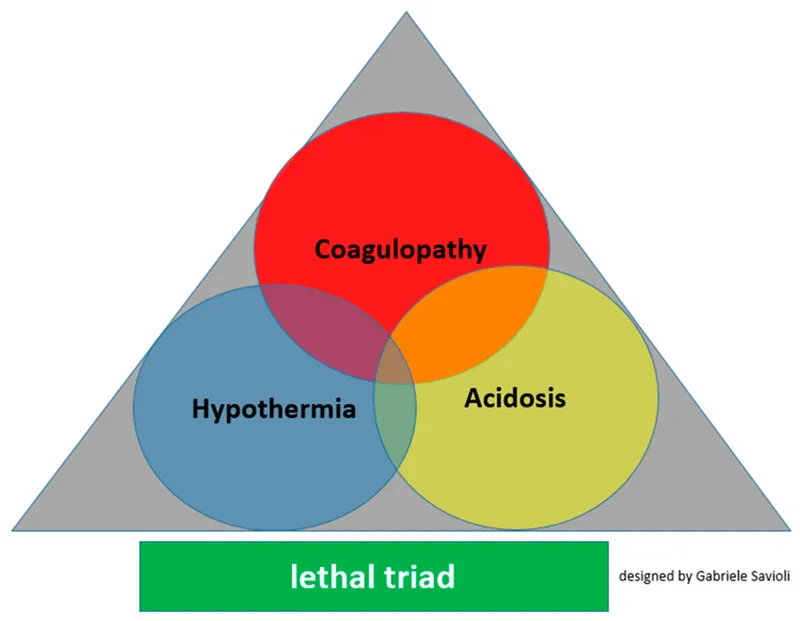
- The patient exhibits signs of **massive hemorrhage and coagulopathy** (persistent oozing, decreasing hemoglobin, prolonged PT and aPTT, decreasing platelets) following severe trauma.
- A **1:1:1 ratio transfusion** of packed red blood cells (RBCs), fresh frozen plasma (FFP), and platelet concentrate is the recommended **massive transfusion protocol** to address hypovolemia, anemia, and consumptive coagulopathy simultaneously.
*Transfuse packed RBC*
- While the patient is anemic (Hb dropped from 14.8 to 12.4 g/dL), transfusing only RBCs would not address the significant **coagulopathy** evidenced by prolonged PT/aPTT and decreasing platelets.
- This option would correct **hypovolemia and oxygen-carrying capacity** but fail to resolve the underlying bleeding disorder, potentially worsening hemorrhage.
*Transfuse packed RBC and fresh frozen plasma in a 1:1 ratio*
- This approach addresses **anemia and coagulopathy** by providing clotting factors, but it neglects the patient's **thrombocytopenia** (platelets dropped from 175,000 to 102,000/mm3 with ongoing bleeding).
- Platelet transfusion is crucial for **hemostasis**, especially in uncontrolled traumatic bleeding.
*Transfuse fresh frozen plasma and platelet concentrate in a 1:1 ratio*
- This option targets **coagulopathy and thrombocytopenia** but completely ignores the significant **anemia and hypovolemia** (Hb 12.4 g/dL with ongoing bleeding) that is likely contributing to hypoperfusion.
- **RBCs** are essential to restore oxygen delivery to tissues and manage hemorrhagic shock.
*Transfuse whole blood and administer vitamin K*
- **Whole blood** is rarely used in civilian trauma settings due to practical limitations, and its components can be provided separately.
- **Vitamin K** is primarily used for warfarin reversal or vitamin K deficiency, which is not the acute cause of coagulopathy in severe trauma; the issue is **dilutional and consumptive coagulopathy**.
Blood product replacement strategies US Medical PG Question 7: A 74-year-old man presents to the emergency department by paramedics for slurred speech and weakness in the left arm and leg for 1 hour. The patient was playing with his grandson when the symptoms started and his wife immediately called an ambulance. There is no history of head trauma or recent surgery. The patient takes captopril for hypertension. The vital signs include: pulse 110/min, respiratory rate 22/min, and blood pressure 200/105 mm Hg. The physical examination shows that the patient is alert and conscious, but speech is impaired. Muscle strength is 0/5 in the left arm and leg and 5/5 in the right arm and leg. A non-contrast CT of the head shows no evidence of intracranial bleeding. The lab results are as follows:
Serum glucose 90 mg/dL
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Serum creatinine 1.3 mg/dL
Blood urea nitrogen 20 mg/dL
Cholesterol, total 240 mg/dL
HDL-cholesterol 38 mg/dL
LDL-cholesterol 100 mg/dL
Triglycerides 190 mg/dL
Hemoglobin (Hb%) 15.3 g/dL
Mean corpuscular volume (MCV) 83 fL
Reticulocyte count 0.8%
Erythrocyte count 5.3 million/mm3
Platelet count 130,000/mm3
Partial thromboplastin time (aPTT) 30 sec
Prothrombin time (PT) 12 sec
Although he is within the time frame for the standard therapy of the most likely condition, the treatment cannot be started because of which of the following contraindications?
- A. A platelet count of 130,000/mm3
- B. Age of 74 years
- C. Cholesterol level of 240 mg/dL
- D. Creatinine level of 1.3 mg/dL
- E. Systolic blood pressure of 200 mm Hg (Correct Answer)
Blood product replacement strategies Explanation: ***Systolic blood pressure of 200 mm Hg***
- The patient presents with symptoms highly suggestive of an **acute ischemic stroke**, including **slurred speech** and **left-sided weakness**.
- For patients with acute ischemic stroke who are candidates for **thrombolytic therapy (e.g., alteplase)**, a **systolic blood pressure consistently >185 mm Hg or diastolic >110 mm Hg is a contraindication** due to increased risk of hemorrhagic transformation.
*A platelet count of 130,000/mm3*
- A platelet count of 130,000/mm³ is above the **contraindication threshold for thrombolytic therapy**, which is typically <100,000/mm³.
- Therefore, this platelet count would **not prevent** the initiation of tPA.
*Age of 74 years*
- While older age was once considered a relative contraindication, current guidelines **do not consider age alone (including 74 years old) as an absolute contraindication** for thrombolytic therapy in acute ischemic stroke.
- Eligibility is determined by a comprehensive risk-benefit assessment, not solely by age.
*Cholesterol level of 240 mg/dL*
- An elevated **cholesterol level** is a **risk factor for atherosclerosis** and ischemic stroke, but it is **not a contraindication for acute thrombolytic therapy**.
- It relates to the underlying cause of the stroke rather than the immediate treatment decision.
*Creatinine level of 1.3 mg/dL*
- A **creatinine level of 1.3 mg/dL** indicates **mild renal impairment**, but it is **not a contraindication for thrombolytic therapy**.
- Renal function more significantly impacts the use of certain anticoagulants, but not typically alteplase in the acute setting.
Blood product replacement strategies US Medical PG Question 8: A 23-year-old male presents to the emergency room following a gunshot wound to the leg. On arrival his temperature is 99°F (37.2°C), blood pressure is 90/60 mmHg, pulse is 112/min, respirations are 21/min, and pulse oximetry is 99% on room air. Two large bore IVs are placed and he receives crystalloid fluid replacement followed by 2 units of crossmatched packed red blood cells. Immediately following transfusion, his temperature is 102.2°F (39°C), blood pressure is 93/64 mmHg, pulse is 112/min, respirations are 21/min, and pulse oximetry is 99% on room air. There is oozing from his IV sites. You check the records and realize there was a clerical error with the blood bank. What is the mechanism for his current condition?
- A. IgE mediated reaction
- B. Deposition of immune complexes
- C. Production of leukotrienes
- D. Preformed antibodies (Correct Answer)
- E. T lymphocyte reaction
Blood product replacement strategies Explanation: ***Preformed antibodies***
- The patient's symptoms, including **fever**, persistent **hypotension**, and **oozing from IV sites** (which suggests **DIC**), immediately following a transfusion due to a clerical error, are classic signs of an **acute hemolytic transfusion reaction (AHTR)**.
- AHTRs are caused by the recipient's **preformed antibodies** (e.g., anti-A, anti-B) reacting with donor red blood cell antigens, leading to rapid **intravascular hemolysis**, cytokine release, and activation of the coagulation cascade.
*IgE mediated reaction*
- An **IgE-mediated reaction** (Type I hypersensitivity) typically presents with symptoms like **hives, angioedema, bronchospasm, or anaphylaxis**.
- While transfusion reactions can involve allergic components, the clinical picture of severe hemolysis and DIC points away from a primary IgE-mediated anaphylactic response.
*Deposition of immune complexes*
- **Immune complex deposition** (Type III hypersensitivity) is characteristic of conditions like **serum sickness** or **lupus**.
- These reactions usually manifest hours to days after exposure and typically involve features like **arthritis** or **glomerulonephritis**, which are not seen in this acute scenario.
*Production of leukotrienes*
- **Leukotrienes** are mediators of inflammation and bronchoconstriction, prominently involved in **asthma** and some allergic reactions.
- While they may play a secondary role in the inflammatory response, they are not the primary mechanism initiating an **acute hemolytic transfusion reaction**.
*T lymphocyte reaction*
- **T lymphocyte reactions** are central to **delayed-type hypersensitivity** (Type IV) and **graft-versus-host disease (GVHD)**.
- These reactions have a delayed onset (**days to weeks**) and primarily involve cellular immunity, which does not explain the immediate and severe hemolytic reaction observed.
Blood product replacement strategies US Medical PG Question 9: A 68-year-old man is brought to the emergency department because of a severe headache, nausea, and vomiting for 30 minutes. Forty-five minutes ago, he fell and struck his head, resulting in loss of consciousness for 1 minute. After regaining consciousness, he felt well for 15 minutes before the headache began. On arrival, the patient becomes rigid and his eyes deviate to the right; he is incontinent of urine. Intravenous lorazepam is administered and the rigidity resolves. Which of the following is the most likely cause of the patient's condition?
- A. Rupture of bridging veins
- B. Cerebrospinal fluid production/absorption mismatch
- C. Acute insufficiency of cerebral blood flow
- D. Bleeding between dura mater and skull (Correct Answer)
- E. Intracerebral hemorrhage
Blood product replacement strategies Explanation: ***Bleeding between dura mater and skull***
- The classic presentation of an **epidural hematoma** includes a brief **loss of consciousness** followed by a **lucent interval** (patient feeling well) and then rapid neurological deterioration with symptoms like **severe headache**, **nausea**, **vomiting**, and **seizures** due to increasing intracranial pressure.
- This type of bleeding is typically arterial, usually from the **middle meningeal artery**, and occurs between the dura mater and the inner table of the skull.
*Rupture of bridging veins*
- This describes a **subdural hematoma**, which usually results in a more gradual onset of symptoms due to slower venous bleeding, often over days to weeks.
- While a fall can cause it, the rapid deterioration after a lucid interval is less typical for a subdural hematoma.
*Cerebrospinal fluid production/absorption mismatch*
- This mechanism is associated with conditions like **hydrocephalus** or **idiopathic intracranial hypertension**, which typically present with a more gradual onset of symptoms such as chronic headache, visual changes, or gait disturbances.
- It does not account for an acute traumatic event, loss of consciousness, and rapid deterioration seen in this patient.
*Acute insufficiency of cerebral blood flow*
- This typically refers to an **ischemic stroke** or **transient ischemic attack (TIA)**, where symptoms arise from a lack of oxygenated blood to brain regions.
- While it can cause neurological deficits, the history of head trauma, lucid interval, and rapid progression to severe symptoms and seizures points away from a primary ischemic event.
*Intracerebral hemorrhage*
- This involves bleeding within the **brain parenchyma** itself, which can present acutely with headache, vomiting, and neurological deficits.
- However, the distinct **lucid interval** following initial loss of consciousness, as described, is much more characteristic of an **epidural hematoma** rather than bleeding directly into the brain tissue.
Blood product replacement strategies US Medical PG Question 10: A 27-year-old man presents to the emergency department with his family because of abdominal pain, excessive urination, and drowsiness since the day before. He has had type 1 diabetes mellitus for 2 years. He ran out of insulin 2 days ago. The vital signs at admission include: temperature 36.8°C (98.2°F), blood pressure 102/69 mm Hg, and pulse 121/min. On physical examination, he is lethargic and his breathing is rapid and deep. There is a mild generalized abdominal tenderness without rebound tenderness or guarding. His serum glucose is 480 mg/dL. Arterial blood gas of this patient will most likely show which of the following?
- A. ↑ pH, ↑ bicarbonate, and normal pCO2
- B. ↓ pH, ↓ bicarbonate and ↑ anion gap (Correct Answer)
- C. ↑ pH, normal bicarbonate and ↓ pCO2
- D. ↓ pH, ↓ bicarbonate and normal anion gap
- E. ↓ pH, normal bicarbonate and ↑ pCO2
Blood product replacement strategies Explanation: ***↓ pH, ↓ bicarbonate and ↑ anion gap***
- The patient's symptoms (abdominal pain, excessive urination, drowsiness, rapid and deep breathing, hyperglycemia) and history of Type 1 diabetes with missed insulin are highly suggestive of **diabetic ketoacidosis (DKA)**.
- DKA is characterized by **metabolic acidosis** due to the accumulation of ketone bodies, leading to a **decreased pH**, consumption of bicarbonate and thus a **decreased bicarbonate level**, and an **increased anion gap**.
*↑ pH, ↑ bicarbonate, and normal pCO2*
- This pattern suggests a **metabolic alkalosis**, which is inconsistent with the patient's presentation of DKA.
- Metabolic alkalosis is typically seen in conditions like severe vomiting or diuretic use, not uncontrolled diabetes.
*↑ pH, normal bicarbonate and ↓ pCO2*
- This profile describes **respiratory alkalosis**, often caused by primary hyperventilation.
- While the patient has rapid and deep breathing (Kussmaul respiration), this is a compensatory mechanism for metabolic acidosis, not a primary respiratory alkalosis.
*↓ pH, ↓ bicarbonate and normal anion gap*
- This indicates a **normal anion gap metabolic acidosis**, also known as hyperchloremic acidosis.
- This is typically seen in conditions like renal tubular acidosis or severe diarrhea, where bicarbonate is lost or chloride is retained, which is not the case for DKA.
*↓ pH, normal bicarbonate and ↑ pCO2*
- This presentation indicates **respiratory acidosis**, which is caused by hypoventilation and retention of CO2.
- The patient's rapid and deep breathing (Kussmaul breathing) is a compensatory mechanism to blow off CO2 and would decrease pCO2, not increase it.
More Blood product replacement strategies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.