Balloon tamponade techniques US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Balloon tamponade techniques. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Balloon tamponade techniques US Medical PG Question 1: A 24-year-old primigravida presents at 36 weeks gestation with vaginal bleeding, mild abdominal pain, and uterine contractions that appeared after bumping into a handrail. The vital signs are as follows: blood pressure 130/80 mm Hg, heart rate 79/min, respiratory rate 12/min, and temperature 36.5℃ (97.7℉). The fetal heart rate was 145/min. Uterine fundus is at the level of the xiphoid process. Slight uterine tenderness and contractions are noted on palpation. The perineum is bloody. The gynecologic examination shows no vaginal or cervical lesions. The cervix is long and closed. Streaks of bright red blood are passing through the cervix. A transabdominal ultrasound shows the placenta to be attached to the lateral uterine wall with a marginal retroplacental hematoma (an approximate volume of 150 ml). The maternal hematocrit is 36%. What is the next best step in the management of this patient?
- A. Manage as an outpatient with modified rest
- B. Induction of vaginal labor
- C. Corticosteroid administration and schedule a cesarean section after
- D. Admit for maternal and fetal monitoring and observation (Correct Answer)
- E. Urgent cesarean delivery
Balloon tamponade techniques Explanation: ***Admit for maternal and fetal monitoring and observation***
- This patient presents with signs of a **mild placental abruption** (vaginal bleeding, contractions, mild abdominal pain, retroplacental hematoma) after trauma, but her **vital signs are stable**, fetal heart rate is reassuring, and the abruption volume is relatively small.
- Expectant management with **close monitoring** for signs of worsening abruption (increasing pain, vital sign changes, fetal distress) is appropriate for a patient at 36 weeks with a non-catastrophic abruption.
*Manage as an outpatient with modified rest*
- Given the presence of **vaginal bleeding, contractions**, and a **retroplacental hematoma** suggesting placental abruption, outpatient management is not safe.
- There is a risk of the abruption progressing, requiring immediate medical intervention, making **hospital admission for close monitoring** essential.
*Induction of vaginal labor*
- While vaginal delivery might be considered for a stable abruption in some cases, **active induction is not the immediate next step** given the patient's stable status and the need for continuous monitoring.
- The **cervix is long and closed**, indicating that she is not in active labor and immediate induction might not be successful or necessary.
*Corticosteroid administration and schedule a cesarean section after*
- **Corticosteroids** are typically administered for fetal lung maturity when delivery is anticipated before **34 weeks of gestation**; at 36 weeks, this is generally not indicated.
- A scheduled cesarean section is premature as the patient is **stable**, and the immediate goal is to monitor for progression or resolution of the abruption, not immediate delivery.
*Urgent cesarean delivery*
- There are no signs of **maternal or fetal distress** (stable vitals, reassuring fetal heart rate) that would necessitate an urgent cesarean delivery.
- An urgent cesarean is reserved for cases of **severe abruption** with significant bleeding, hemodynamic instability, or fetal compromise.
Balloon tamponade techniques US Medical PG Question 2: A 30-year-old woman, gravida 2, para 1, at 42 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been complicated by gestational diabetes, for which she has been receiving insulin injections. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 90/min, respirations are 18/min, and blood pressure is 135/80 mm Hg. The fetal heart rate tracing shows a baseline heart rate of 145/min and moderate variation with frequent accelerations and occasional early decelerations. She undergoes an elective repeat lower segment transverse cesarean section with complete removal of the placenta. Shortly after the operation, she starts having heavy uterine bleeding with passage of clots. Examination shows a soft uterus on palpation. Her bleeding continues despite fundal massage and the use of packing, oxytocin, misoprostol, and carboprost. Her pulse rate is now 120/min, respirations are 20/min, and blood pressure is 90/70 mm Hg. Her hemoglobin is 8 g/dL, hematocrit is 24%, platelet count is 120,000 mm3, prothrombin time is 11 seconds, and partial thromboplastin time is 30 seconds. Mass transfusion protocol is activated and a B-Lynch uterine compression suture is placed to control her bleeding. Which of the following is the mostly likely cause of her postpartum complication?
- A. Adherent placenta to myometrium
- B. Uterine inversion
- C. Infection of the endometrial lining of the uterus
- D. Uterine rupture
- E. Lack of uterine muscle contraction (Correct Answer)
Balloon tamponade techniques Explanation: ***Lack of uterine muscle contraction***
- The presentation of a **soft uterus** on palpation and continued severe bleeding despite fundal massage and uterotonics (**oxytocin, misoprostol, carboprost**) is highly indicative of **uterine atony**, which is a lack of effective uterine muscle contraction.
- Uterine atony is the most common cause of **postpartum hemorrhage**, and risk factors include **macrosomia** (due to gestational diabetes), **multiparity**, and a prolonged labor or rapid delivery, though the latter two are less clear here.
*Adherent placenta to myometrium*
- While a history of prior C-section and **macrosomia** (due to gestational diabetes) could increase the risk of an **abnormally adherent placenta** (accreta, increta, percreta), the description notes **complete removal of the placenta**.
- If the placenta were morbidly adherent and not completely removed, bleeding would likely stem from retained placental tissue, and this would typically be explicitly noted or suspected due to difficulty with manual removal.
*Uterine inversion*
- **Uterine inversion** involves the uterus turning inside out, which would present with a **mass protruding from the vagina** or a visible inversion of the fundus upon examination, along with sudden onset of severe pain and shock.
- The description of a **soft uterus** and an absence of a physical description of uterine inversion makes this diagnosis less likely.
*Infection of the endometrial lining of the uterus*
- **Endometritis** (infection of the endometrial lining) typically presents with fever, foul-smelling lochia, uterine tenderness, and prolonged postpartum bleeding, usually occurring a few days postpartum rather than immediately following delivery.
- The acute, massive hemorrhage immediately following delivery, coupled with a normal initial temperature, does not align with the typical presentation of endometritis.
*Uterine rupture*
- **Uterine rupture** is a serious complication, especially with a history of prior C-section, but it typically presents with **sudden severe abdominal pain**, fetal heart rate abnormalities (if it occurs before delivery), and **hemodynamic instability**, often with cessation of contractions.
- While the patient is hemodynamically unstable, the primary issue described is heavy uterine bleeding with a soft uterus, and no mention of severe abdominal pain or clear signs of rupture during the C-section make uterine atony a more direct explanation for the described symptoms.
Balloon tamponade techniques US Medical PG Question 3: Five minutes after initiating a change of position and oxygen inhalation, the oxytocin infusion is discontinued. A repeat CTG that is done 10 minutes later shows recurrent variable decelerations and a total of 3 uterine contractions in 10 minutes. Which of the following is the most appropriate next step in management?
- A. Restart oxytocin infusion
- B. Emergent Cesarean section
- C. Administer terbutaline
- D. Monitor without intervention
- E. Amnioinfusion (Correct Answer)
Balloon tamponade techniques Explanation: ***Amnioinfusion***
- **Recurrent variable decelerations** persisting after discontinuing oxytocin and changing maternal position often indicate **cord compression**, which can be relieved by amnioinfusion.
- Adding fluid to the amniotic cavity **cushions the umbilical cord**, reducing compression during uterine contractions.
*Restart oxytocin infusion*
- Reinitiating oxytocin would likely **worsen the recurrent variable decelerations** by increasing uterine contraction frequency and intensity, thereby exacerbating cord compression.
- The goal is to alleviate fetal distress, not to intensify uterine activity that is already causing issues.
*Emergent Cesarean section*
- While an emergent Cesarean section is indicated for **unresolved fetal distress**, it's usually considered after less invasive measures, such as amnioinfusion, have failed.
- There is still an opportunity for a simpler intervention to resolve the issue before resorting to surgery.
*Administer terbutaline*
- Terbutaline is a **tocolytic agent** used to reduce uterine contractions, which can be helpful in cases of tachysystole or hyperstimulation.
- In this scenario, the contraction frequency is low (3 in 10 minutes), so reducing contractions is not the primary aim; rather, the focus is on resolving the cord compression causing decelerations.
*Monitor without intervention*
- **Recurrent variable decelerations** are an concerning sign of **fetal distress** and require intervention to prevent potential harm to the fetus.
- Simply monitoring without intervention would be inappropriate and could lead to worsening fetal hypoxemia and acidosis.
Balloon tamponade techniques US Medical PG Question 4: Thirty minutes after vaginal delivery of a 2780-g (6-lb 2-oz) newborn at term, a 25-year-old woman, gravida 1, para 1, has heavy vaginal bleeding. Her pregnancy was complicated by pre-eclampsia. Her pulse is 111/min and blood pressure is 95/65 mm Hg. Physical examination shows a fundal height 2 inches below the xiphoid process of the sternum. A drug with which of the following mechanisms of action is most appropriate for this patient?
- A. Activation of phospholipase C (Correct Answer)
- B. Depolarization of the motor end plate
- C. Increased synthesis of cyclic AMP
- D. Inhibition of norepinephrine reuptake
- E. Binding to prostaglandin I2 receptors
Balloon tamponade techniques Explanation: ***Activation of phospholipase C***
- This patient presents with **postpartum hemorrhage (PPH)**, characterized by heavy vaginal bleeding, tachycardia, hypotension, and a poorly contracted uterus (normal fundal height is at the umbilicus immediately after delivery; 2 inches below the xiphoid is high indicating uterine atony).
- The most appropriate first-line treatment for uterine atony is **oxytocin**, which acts by binding to G protein-coupled receptors, leading to the **activation of phospholipase C** and an increase in intracellular calcium, causing uterine muscle contraction.
*Depolarization of the motor end plate*
- This mechanism describes the action of **neuromuscular blocking agents** or agonists at the nicotinic acetylcholine receptor, which are not used for treating postpartum hemorrhage.
- The motor end plate is involved in skeletal muscle contraction, not smooth muscle contraction of the uterus.
*Increased synthesis of cyclic AMP*
- **Increased cyclic AMP** generally leads to smooth muscle relaxation (e.g., beta-2 agonists like terbutaline), which would worsen uterine atony and postpartum hemorrhage.
- Tocolytic agents that would cause uterine relaxation would be contraindicated in this scenario.
*Inhibition of norepinephrine reuptake*
- This mechanism describes the action of certain **antidepressants** (e.g., tricyclic antidepressants, SNRIs) or **stimulants**, which primarily affect the central nervous system and are not used to manage postpartum hemorrhage.
- This action does not directly cause uterine contraction.
*Binding to prostaglandin I2 receptors*
- **Prostaglandin I2 (PGI2)**, also known as prostacyclin, is a potent vasodilator and inhibitor of platelet aggregation. Binding to its receptors would lead to smooth muscle relaxation and would increase bleeding, directly worsening postpartum hemorrhage.
- Uterotonic agents like carboprost (PGF2α analog) act on different prostaglandin receptors to induce uterine contraction.
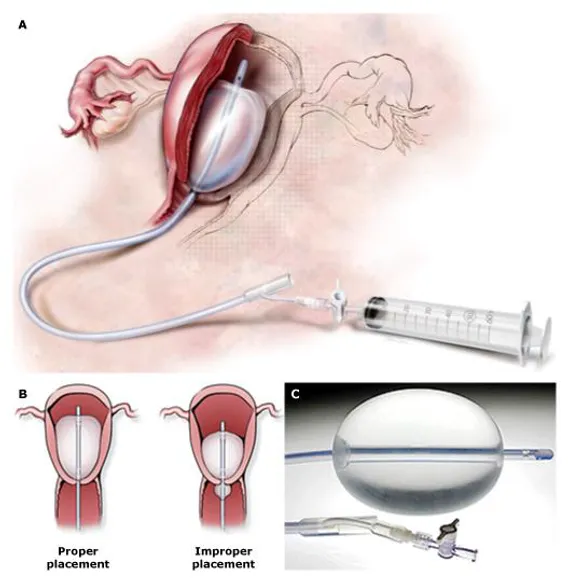
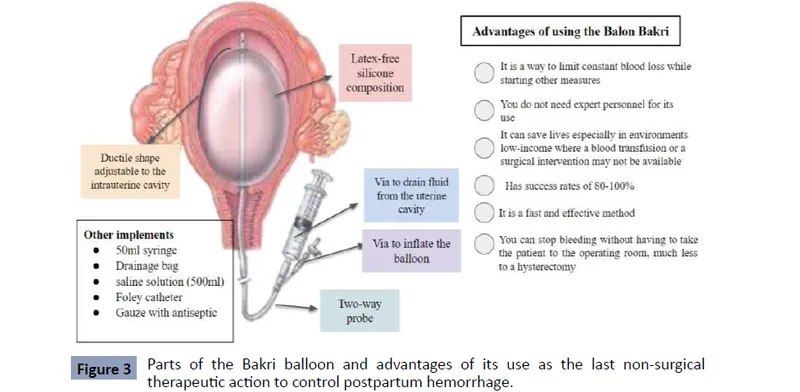
Balloon tamponade techniques US Medical PG Question 5: Thirty minutes after normal vaginal delivery of twins, a 35-year-old woman, gravida 5, para 4, has heavy vaginal bleeding with clots. Physical examination shows a soft, enlarged, and boggy uterus. Despite bimanual uterine massage, administration of uterotonic drugs, and placement of an intrauterine balloon for tamponade, the bleeding continues. A hysterectomy is performed. Vessels running through which of the following structures must be ligated during the surgery to achieve hemostasis?
- A. Suspensory ligament
- B. Round ligament
- C. Ovarian ligament
- D. Uterosacral ligament
- E. Cardinal ligament (Correct Answer)
Balloon tamponade techniques Explanation: ***Cardinal ligament***
- The **uterine artery** and **uterine vein**, which supply the uterus, run through the **cardinal ligament** (also known as the transverse cervical ligament).
- Ligation of these vessels is crucial during a hysterectomy to control bleeding from the uterus.
*Suspensory ligament*
- The **suspensory ligament of the ovary** contains the **ovarian artery** and vein, which primarily supply the ovaries and fallopian tubes.
- While these may be ligated during a hysterectomy if the ovaries are removed, they are not the primary vessels causing uterine bleeding in postpartum hemorrhage.
*Round ligament*
- The **round ligament of the uterus** extends from the uterus to the labia majora and contains relatively small vessels, primarily contributing to uterine support.
- Ligation of this ligament alone would not effectively control heavy uterine bleeding.
*Ovarian ligament*
- The **ovarian ligament** connects the ovary to the uterus and contains small vessels that mainly supply the ovary.
- It does not house the major blood supply to the uterus itself.
*Uterosacral ligament*
- The **uterosacral ligaments** primarily provide support to the uterus by connecting it to the sacrum and contain small nerves and vessels.
- Ligation of these ligaments would not control the main arterial supply to the uterus.
Balloon tamponade techniques US Medical PG Question 6: A 57-year-old man is brought to the emergency department by his family because of several episodes of vomiting of blood in the past 24 hours. He has a history of alcoholic cirrhosis and is being treated for ascites with diuretics and for encephalopathy with lactulose. His vital signs include a temperature of 36.9°C (98.4°F), pulse of 85/min, and blood pressure of 80/52 mm Hg. On examination, he is confused and unable to give a complete history. He is noted to have jaundice, splenomegaly, and multiple spider angiomas over his chest. Which of the following is the best initial management of this patient?
- A. Endoscopic surveillance
- B. Non-selective beta-blockers
- C. Combined vasoactive and endoscopic therapy (Correct Answer)
- D. Balloon tamponade
- E. Transjugular intrahepatic portosystemic shunt (TIPS)
Balloon tamponade techniques Explanation: ***Combined vasoactive and endoscopic therapy***
- The patient presents with **hematemesis**, **hypotension**, and signs of decompensated **alcoholic cirrhosis** (jaundice, splenomegaly, spider angiomas). This clinical picture is highly suggestive of **esophageal variceal bleeding**, a life-threatening emergency.
- **Combined vasoactive drug therapy** (e.g., octreotide to reduce splanchnic blood flow) and **endoscopic therapy** (e.g., variceal ligation or sclerotherapy) are the recommended initial management for **active variceal bleeding** to control hemorrhage and prevent rebleeding.
*Endoscopic surveillance*
- **Endoscopic surveillance** is performed for patients with known varices who are **not actively bleeding** to identify varices at high risk of rupture and to initiate primary prophylaxis.
- This patient is actively bleeding, making surveillance an inappropriate initial step.
*Non-selective beta-blockers*
- **Non-selective beta-blockers** (e.g., propranolol, carvedilol) are used for **primary and secondary prophylaxis** of variceal bleeding by reducing portal pressure.
- They are **not appropriate for acute bleeding management**, as their onset of action is too slow to control active hemorrhage.
*Balloon tamponade*
- **Balloon tamponade** (e.g., with a Sengstaken-Blakemore tube) is a **temporary measure** used to control massive, refractory variceal bleeding when endoscopic therapy is unsuccessful or immediately unavailable.
- It is a **bridge to definitive management** and carries significant risks, such as **esophageal rupture** or **aspiration**, so it is not the first-line initial treatment.
*Transjugular intrahepatic portosystemic shunt (TIPS)*
- **TIPS** is typically reserved for patients with **refractory variceal bleeding** that cannot be controlled by endoscopic and pharmacologic therapy, or for those with **recurrent bleeding despite optimal secondary prophylaxis**.
- It is an **invasive procedure** and not the immediate initial intervention for acute variceal hemorrhage.
Balloon tamponade techniques US Medical PG Question 7: A 29-year-old G1P0 presents to her obstetrician for her first prenatal care visit at 12 weeks gestation by last menstrual period. She states that her breasts are very tender and swollen, and her exercise endurance has declined. She otherwise feels well. She is concerned about preterm birth, as she heard that certain cervical procedures increase the risk. The patient has a gynecologic history of loop electrosurgical excision procedure (LEEP) for cervical dysplasia several years ago and has had negative Pap smears since then. She also has mild intermittent asthma that is well controlled with occasional use of her albuterol inhaler. At this visit, this patient’s temperature is 98.6°F (37.0°C), pulse is 69/min, blood pressure is 119/61 mmHg, and respirations are 13/min. Cardiopulmonary exam is unremarkable, and the uterine fundus is just palpable at the pelvic brim. Pelvic exam reveals normal female external genitalia, a closed and slightly soft cervix, a 12-week-size uterus, and no adnexal masses. Which of the following is the best method for evaluating for possible cervical incompetence in this patient?
- A. Transabdominal ultrasound in the first trimester
- B. Transvaginal ultrasound in the first trimester
- C. Serial transvaginal ultrasounds starting at 16 weeks gestation
- D. Transabdominal ultrasound at 18 weeks gestation
- E. Transvaginal ultrasound at 18 weeks gestation (Correct Answer)
Balloon tamponade techniques Explanation: ***Transvaginal ultrasound at 18 weeks gestation***
- A history of **LEEP** is a risk factor for **cervical incompetence** and warrants screening with transvaginal ultrasound.
- The optimal timing for **cervical length** screening in women with a history of cervical procedures is typically between **18 and 24 weeks gestation**, as the risk of cervical shortening usually manifests during this period.
*Transabdominal ultrasound in the first trimester*
- **Transabdominal ultrasound** is generally not ideal for precise **cervical length measurement** due to potential shadowing from the fetus or maternal obesity.
- **First-trimester cervical length measurement** is not typically recommended for routine screening of cervical incompetence, as changes are less pronounced early in pregnancy.
*Transvaginal ultrasound in the first trimester*
- While more accurate than transabdominal, **first-trimester transvaginal ultrasound** for cervical length is not standard for predicting cervical incompetence.
- Significant cervical shortening due to incompetence often occurs later in the second trimester, so early screening may miss the condition.
*Serial transvaginal ultrasounds starting at 16 weeks gestation*
- While **serial transvaginal ultrasounds** starting at 16 weeks can be part of a management plan for high-risk patients, the most critical single assessment typically occurs at **18-24 weeks**.
- Starting serial scans too early may not be necessary if the cervix is long and closed at the initial key screening, unless there are other strong indications.
*Transabdominal ultrasound at 18 weeks gestation*
- Similar to first-trimester transabdominal ultrasound, **transabdominal imaging** at 18 weeks is generally **less accurate** than transvaginal for measuring cervical length.
- **Transvaginal ultrasound** offers a clearer and more precise view of the cervix, which is crucial for assessing potential shortening or funneling.
Balloon tamponade techniques US Medical PG Question 8: A 27-year-old woman, gravida 2, para 1, at 36 weeks' gestation comes to the physician for a prenatal visit. She feels well. Fetal movements are adequate. This is her 7th prenatal visit. She had an ultrasound scan performed 1 month ago that showed a live intrauterine pregnancy consistent with a 32-week gestation with no anomalies. She had a Pap smear performed 1 year ago, which was normal. Vital signs are within normal limits. Pelvic examination shows a uterus consistent in size with a 36-week gestation. Her blood group and type is A negative. Which of the following is the most appropriate next step in management?
- A. Transabdominal doppler ultrasonography
- B. Rh antibody testing
- C. Swab for GBS culture (Correct Answer)
- D. Serum PAPP-A and HCG levels
- E. Complete blood count
Balloon tamponade techniques Explanation: ***Swab for GBS culture***
- All pregnant women should be screened for **Group B Streptococcus (GBS)** between **36 weeks 0 days and 37 weeks 6 days** of gestation.
- A positive GBS culture requires **intrapartum antibiotic prophylaxis** to prevent early-onset neonatal GBS disease.
*Transabdominal doppler ultrasonography*
- **Doppler ultrasonography** is primarily used to assess **fetal well-being** in cases of **fetal growth restriction**, preeclampsia, or other high-risk conditions.
- This patient has a **normal-sized uterus** and **adequate fetal movements**, indicating no immediate need for fetal Doppler assessment.
*Rh antibody testing*
- **Rh antibody testing** (indirect Coombs test) is performed early in pregnancy for Rh-negative women and typically repeated at **28 weeks' gestation** before anti-D immune globulin administration.
- Repeating this test at 36 weeks is not the most appropriate *next* step as the routine schedule for Rh immune globulin would typically be managed prior to this point.
*Serum PAPP-A and HCG levels*
- **Serum PAPP-A and HCG levels** are components of **first-trimester screening** for chromosomal abnormalities, performed between 11 and 14 weeks of gestation.
- At 36 weeks' gestation, these markers are not relevant for current fetal assessment.
*Complete blood count*
- A **complete blood count (CBC)** is routinely performed in the first trimester and often repeated in the **late second or early third trimester** (around 28 weeks) to check for anemia.
- While a CBC might be done as part of general prenatal care, it is not the most urgent or specifically indicated test at 36 weeks in the absence of symptoms.
Balloon tamponade techniques US Medical PG Question 9: A 30-year-old woman comes to the primary care physician because she has felt nauseous and fatigued for 3 weeks. Menses occur at irregular 24- to 33-day intervals and last for 4–6 days. Her last menstrual period was 7 weeks ago. Her temperature is 37°C (98.6°F), pulse is 95/min, and blood pressure is 100/70 mm Hg. Pelvic examination shows an enlarged uterus. Her serum β-hCG concentration is 96,000 mIU/mL (N < 5). An abdominal ultrasound is shown. Which of the following is the most likely diagnosis?
- A. Partial hydatidiform mole
- B. Bicornuate uterus pregnancy
- C. Abdominal pregnancy
- D. Complete hydatid mole (Correct Answer)
- E. Dichorionic-diamniotic twins
Balloon tamponade techniques Explanation: ***Complete hydatid mole***
- The ultrasound image shows a **\"snowstorm\" appearance** with multiple anechoic cysts, typical of a complete hydatidiform mole, consistent with **grape-like vesicles**.
- The significantly elevated **β-hCG level (96,000 mIU/mL)** and symptoms like nausea in conjunction with an enlarged uterus and irregular menses, are highly indicative of gestational trophoblastic disease.
*Partial hydatidiform mole*
- A partial mole typically shows evidence of **fetal tissue** or a **fetus** with associated placental changes, which is absent in this image and clinical presentation.
- While β-hCG levels can be elevated, they are often lower than in complete moles and less likely to show the classic **\"snowstorm\" appearance** in the absence of fetal parts.
*Bicornuate uterus pregnancy*
- A bicornuate uterus is a **uterine anomaly** where the uterus has two horns, and pregnancy would typically occur in one of these horns, appearing as a normal or atypical intrauterine pregnancy on ultrasound.
- The ultrasound image does not show a normally developing pregnancy within a horn of a bicornuate uterus, but rather a characteristic vesicular pattern within the uterus.
*Abdominal pregnancy*
- Abdominal pregnancy involves an **ectopic implantation** outside the uterus, in the abdominal cavity, often showing abnormal fetal presentation and placental attachment to abdominal organs.
- The ultrasound clearly shows an **intrauterine mass** with the characteristic vesicular pattern, ruling out an abdominal pregnancy.
*Dichorionic-diamniotic twins*
- This refers to a **twin pregnancy** with two separate placentas and two separate amniotic sacs, which would be visible as two distinct gestational sacs and two fetuses on ultrasound.
- The image shows a **single mass** with a vesicular pattern, not two separate gestational sacs or fetuses, nor two distinct placentas.
Balloon tamponade techniques US Medical PG Question 10: 29-year-old G2P2002 presents with foul-smelling lochia and fever. She is post-partum day three status-post cesarean section due to eclampsia. Her temperature is 101 F, and heart rate is 103. She denies chills. On physical exam, lower abdominal and uterine tenderness is present. Leukocytosis with left shift is seen in labs. Which of the following is the next best step in management?
- A. Endometrial culture
- B. Intravenous clindamycin and gentamicin treatment (Correct Answer)
- C. Prophylactic intravenous cefazolin treatment
- D. Intramuscular cefotetan treatment
- E. Blood culture
Balloon tamponade techniques Explanation: **Intravenous clindamycin and gentamicin treatment**
* This patient presents with **fever**, **foul-smelling lochia**, **uterine tenderness**, and **leukocytosis with left shift** on postpartum day three after a cesarean section, which are classic signs of **postpartum endometritis**.
* The recommended first-line treatment for **postpartum endometritis** is **broad-spectrum intravenous antibiotics**, typically a combination of **clindamycin** and **gentamicin**, which covers the polymicrobial nature of the infection, including anaerobes and gram-negative rods.
*Endometrial culture*
* While useful for identifying specific pathogens, **endometrial cultures** are generally **not recommended prior to initiating treatment for postpartum endometritis** as the infection is typically polymicrobial, and treatment should be started empirically.
* **Contamination with normal vaginal flora** is a significant concern, making interpretation of cultures difficult and potentially delaying appropriate treatment.
*Prophylactic intravenous cefazolin treatment*
* **Cefazolin** is a first-generation cephalosporin often used for **surgical prophylaxis** before a cesarean section to prevent infection.
* This patient already has clear signs of an established **postpartum infection (endometritis)**, so prophylactic antibiotics are no longer appropriate; she requires therapeutic treatment.
*Intramuscular cefotetan treatment*
* **Cefotetan** is a second-generation cephalosporin with good coverage against some anaerobes and gram-negative bacteria.
* However, for established **postpartum endometritis**, especially after a cesarean section, **intravenous administration** of broad-spectrum antibiotics is preferred for faster therapeutic levels and better efficacy than intramuscular delivery.
*Blood culture*
* **Blood cultures** are important to rule out **bacteremia** or **sepsis**, especially in patients with high fever or signs of systemic illness.
* While an important diagnostic step, it is **not the *next best step in management*** for a patient with clear signs of endometritis; empirical antibiotic therapy should be initiated promptly while awaiting culture results.
More Balloon tamponade techniques US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.