Umbilical cord prolapse US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Umbilical cord prolapse. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
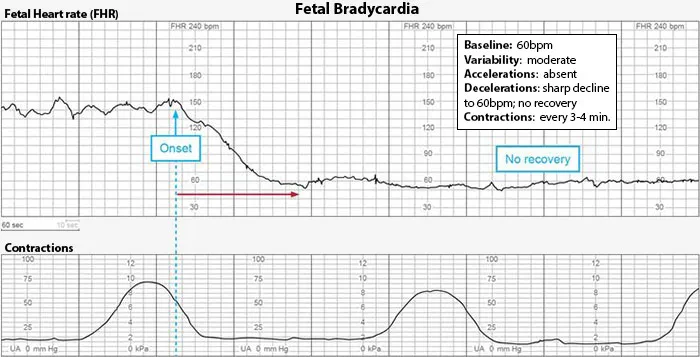
Umbilical cord prolapse US Medical PG Question 1: A 26-year-old primigravid woman at 39 weeks' gestation is admitted to the hospital in active labor. Pregnancy was complicated by mild oligohydramnios detected a week ago, which was managed with hydration. Her pulse is 92/min, respirations are 18/min, and blood pressure is 134/76 mm Hg. Pelvic examination shows 100% cervical effacement and 10 cm cervical dilation; the vertex is at 0 station. Cardiotocography is shown. Which of the following is the most appropriate next step in management?
- A. Maternal repositioning and oxygen administration (Correct Answer)
- B. Emergent cesarean section
- C. Elevation of the fetal head
- D. Reassurance
- E. Rapid amnioinfusion
Umbilical cord prolapse Explanation: ***Maternal repositioning and oxygen administration***
- The cardiotocography shows **variable decelerations**, which are characterized by an abrupt decrease in fetal heart rate, often U, V, or W shaped, and not consistently related to contractions.
- Initial management for variable decelerations, common in cases of **oligohydramnios**, involves conservative measures like **maternal repositioning** (e.g., left lateral, right lateral, hands and knees) to relieve umbilical cord compression and administering **oxygen** to improve fetal oxygenation.
*Emergent cesarean section*
- While severe, unremitting variable decelerations unresponsive to conservative measures may warrant a cesarean section, the current tracing does not indicate an **immediate obstetric emergency** requiring such an invasive procedure as the first step.
- An emergent cesarean section is reserved for situations of **persistent non-reassuring fetal status** despite intervention.
*Elevation of the fetal head*
- Elevating the fetal head is typically done to **relieve umbilical cord prolapse** during a vaginal examination, a condition that might present with sudden, profound decelerations or bradycardia, which is not clearly depicted as the primary issue here.
- This maneuver is an intervention for a specific obstetric emergency and does not address the underlying pathophysiology of variable decelerations due to cord compression.
*Reassurance*
- The presence of **variable decelerations** indicates **umbilical cord compression** and potential fetal compromise, requiring active intervention rather than passive reassurance.
- Reassurance alone is insufficient and inappropriate when there are signs of **fetal distress** on the cardiotocograph.
*Rapid amnioinfusion*
- **Amnioinfusion** can be considered for **recurrent variable decelerations** due to oligohydramnios that are unresponsive to maternal repositioning and oxygen.
- It is generally not the *first* step, as less invasive measures should be attempted first. Moreover, rapid amnioinfusion carries its own risks and should be carefully considered.
Umbilical cord prolapse US Medical PG Question 2: A mother brings her 3-day-old son to the pediatrician with a concern over drops of a clear yellow discharge from the clamped umbilical cord. These drops have formed every few hours every day. The vital signs are within normal limits and a cursory physical shows no abnormalities. On closer examination, the discharge is shown to be urine. The skin around the umbilical cord appears healthy and healing. The umbilical cord is appropriately discolored. An ultrasound shows a fistula tract that connects the urinary bladder and umbilicus. Which of the following structures failed to form in this patient?
- A. Round ligament of the liver
- B. Lateral umbilical ligament
- C. Median umbilical ligament (Correct Answer)
- D. Falciform ligament
- E. Medial umbilical ligament
Umbilical cord prolapse Explanation: ***Median umbilical ligament***
- The discharge of urine from the **umbilical cord stump** is indicative of a **patent urachus**, which occurs when the embryological connection between the bladder and umbilicus (the urachus) fails to close.
- The urachus should normally obliterate and form the **median umbilical ligament** in adults, so its failure to form or close is the underlying cause for the fistula.
*Round ligament of the liver*
- This ligament is the remnant of the **umbilical vein** and is responsible for connecting the umbilicus to the liver.
- A defect in the round ligament of the liver would typically present with symptoms related to hepatic circulation or umbilical hernias, not urinary discharge.
*Lateral umbilical ligament*
- This option likely refers to the **medial umbilical ligaments** (lateral umbilical folds), which are remnants of the **obliterated umbilical arteries**.
- These paired structures carry blood from the internal iliac arteries to the placenta during fetal life and obliterate after birth.
- Failure of these structures to obliterate would typically involve vascular issues, not a urinary fistula from the bladder.
*Falciform ligament*
- The falciform ligament is a **peritoneal fold** that attaches the liver to the anterior abdominal wall and contains the round ligament of the liver in its free edge.
- While it is related to the umbilicus, its primary role is in supporting the liver, and its failure to form would not cause persistent urinary discharge from the umbilicus.
*Medial umbilical ligament*
- The medial umbilical ligaments are remnants of the **umbilical arteries**, which carry deoxygenated blood from the fetus to the placenta.
- Failure of these structures to obliterate would typically involve vascular issues or persistent patent arteries, not a urinary fistula.
Umbilical cord prolapse US Medical PG Question 3: A 30-year-old woman, gravida 1, para 0, at 40 weeks' gestation is admitted to the hospital in active labor. Pregnancy was complicated by iron deficiency anemia treated with iron supplements. At the beginning of the first stage of labor, there are coordinated, regular, rhythmic contractions of high intensity that occur approximately every 10 minutes. Four hours later, the cervix is 100% effaced and 10 cm dilated; the vertex is at -1 station. Over the next two hours, there is minimal change in fetal descent; vertex is still at -1 station. Fetal birth weight is estimated at the 75th percentile. The fetal heart rate is 145/min and is reactive with no decelerations. Contractions occurs approximately every 2 minutes with adequate pressure. Epidural anesthesia was not given, as the patient is coping well with pain. Which of the following is the most appropriate next step in management?
- A. Cesarean section
- B. Observation for another hour (Correct Answer)
- C. Epidural anesthesia
- D. Vacuum-assisted delivery
- E. Administration of terbutaline
Umbilical cord prolapse Explanation: ***Observation for another hour***
- This patient is experiencing a **prolonged second stage of labor**, defined as over 3 hours for nulliparous women with epidural or over 2 hours without. Since she is nulliparous and has not received an epidural, she has breached the initial 2-hour threshold but can labor for up to an additional hour before intervention is necessary.
- The **fetal heart rate (FHR) is reassuring**, and contractions are adequate, indicating no immediate fetal distress or uterine dysfunction, thus allowing for a period of continued observation.
*Cesarean section*
- While a C-section might eventually be indicated if labor fails to progress, it is **premature given the current clinical picture** and lack of fetal distress or clear maternal indication for immediate surgical intervention.
- The criteria for **arrest of descent** in the second stage are not fully met yet, especially considering she is nulliparous and has not received an epidural.
*Epidural anesthesia*
- Epidural anesthesia is used for **pain relief** during labor and can sometimes prolong the second stage, but it is not a management strategy for prolonged second stage itself, especially when the patient is coping well.
- Administering an epidural at this stage might **further compromise efforts** to push effectively and could prolong labor even more.
*Vacuum-assisted delivery*
- Operative vaginal delivery (vacuum or forceps) is considered for a prolonged second stage of labor when there is **arrest of descent** and specific cervical and fetal station criteria are met. However, it is not the first step when the fetus is still at -1 station and there's no immediate distress.
- The **vertex is at -1 station**, which is relatively high for an instrumental delivery unless clear arrest has been established and all other options are exhausted, or there's fetal compromise.
*Administration of terbutaline*
- **Terbutaline is a tocolytic** used to relax the uterus and inhibit contractions, most commonly in cases of preterm labor or uterine tachysystole.
- In this scenario, the patient has **adequate contractions**, and the goal is to facilitate labor progression, not inhibit it.
Umbilical cord prolapse US Medical PG Question 4: Immediately following prolonged delivery of the placenta at 40 weeks gestation, a 32-year-old multiparous woman develops vaginal bleeding. Other than mild asthma, the patient’s pregnancy has been uncomplicated. She has attended many prenatal appointments and followed the physician's advice about screening for diseases, laboratory testing, diet, and exercise. Previous pregnancies were uncomplicated. She has no history of a serious illness. She is currently on intravenous infusion of oxytocin. Her temperature is 37.2°C (99.0°F), blood pressure is 108/60 mm Hg, pulse is 88/min, and respirations are 17/min. Uterine palpation reveals a soft enlarged fundus that extends above the umbilicus. Based on the assessment of the birth canal and placenta, which of the following options is the most appropriate initial step in patient management?
- A. Intramuscular carboprost
- B. Manual exploration of the uterus
- C. Discontinuing oxytocin
- D. Intravenous methylergonovine
- E. Uterine fundal massage (Correct Answer)
Umbilical cord prolapse Explanation: ***Uterine fundal massage***
- The patient presents with **postpartum hemorrhage** indicated by vaginal bleeding and a **soft, enlarged fundus** after placental delivery, suggesting **uterine atony**.
- **Uterine fundal massage** is the **first-line intervention** to encourage uterine contraction and reduce bleeding by expelling clots and compressing vessels.
*Intramuscular carboprost*
- **Carboprost** is a **prostaglandin F2 alpha analog** used to treat **uterine atony** when initial measures like uterine massage and oxytocin are insufficient.
- It is contraindicated in patients with **asthma** due to its bronchoconstrictive effects, which this patient has.
*Manual exploration of the uterus*
- **Manual exploration of the uterus** is indicated when there is suspicion of **retained placental fragments** or **uterine rupture**.
- While these can cause postpartum hemorrhage, the primary finding of a soft, boggy uterus points more strongly to atony, making massage the immediate priority.
*Discontinuing oxytocin*
- The patient is already on an **intravenous oxytocin infusion**, which is a uterotonic agent used to prevent and treat uterine atony.
- Discontinuing it would worsen **uterine atony** and increase blood loss, directly contradicting the goal of management.
*Intravenous methylergonovine*
- **Methylergonovine** is an **ergot alkaloid** used to treat **uterine atony**, but it is contraindicated in patients with **hypertension**, which is not explicitly present here, but it is a potent vasoconstrictor and second-line.
- It is often used as a **second-line agent** if oxytocin and massage are ineffective and there are no contraindications.
Umbilical cord prolapse US Medical PG Question 5: A 29-year-old G2P1 at 35 weeks gestation presents to the obstetric emergency room with vaginal bleeding and severe lower back pain. She reports the acute onset of these symptoms 1 hour ago while she was outside playing with her 4-year-old son. Her prior birthing history is notable for an emergency cesarean section during her first pregnancy. She received appropriate prenatal care during both pregnancies. She has a history of myomectomy for uterine fibroids. Her past medical history is notable for diabetes mellitus. She takes metformin. Her temperature is 99.0°F (37.2°C), blood pressure is 104/68 mmHg, pulse is 120/min, and respirations are 20/min. On physical examination, the patient is in moderate distress. Large blood clots are removed from the vaginal vault. Contractions are occurring every 2 minutes. Delayed decelerations are noted on fetal heart monitoring. Which of the following is the most likely cause of this patient's symptoms?
- A. Premature separation of a normally implanted placenta (Correct Answer)
- B. Amniotic sac rupture prior to the start of uterine contractions
- C. Placental implantation over internal cervical os
- D. Chorionic villi attaching to the myometrium
- E. Chorionic villi attaching to the decidua basalis
Umbilical cord prolapse Explanation: ***Premature separation of a normally implanted placenta***
- The acute onset of **vaginal bleeding**, **severe lower back pain**, frequent uterine contractions, and **fetal decelerations** in a patient with risk factors like a prior cesarean section and diabetes mellitus are highly suggestive of **abruptio placentae**.
- **Uterine tenderness** and a **firm, rigid uterus** (though not explicitly stated, implied by contractions and pain) are also characteristic findings.
*Amniotic sac rupture prior to the start of uterine contractions*
- This condition presents with a gush of fluid from the vagina, often without significant bleeding or severe pain unless associated with other complications.
- While it can lead to preterm labor, it doesn't directly cause the severe back pain, heavy bleeding with clots, and fetal distress seen here.
*Placental implantation over internal cervical os*
- This describes **placenta previa**, which typically presents with **painless vaginal bleeding**, often bright red, without severe abdominal or back pain.
- The presence of severe abdominal pain and uterine contractions makes placenta previa less likely.
*Chorionic villi attaching to the myometrium*
- This describes **placenta accreta**, a condition where the placenta abnormally adheres to the myometrium. It is typically diagnosed postnatally with **difficulty in placental separation** and severe hemorrhage.
- While a prior C-section is a risk factor, the acute presentation of pain and bleeding in the antepartum period is not the classic presentation of accreta alone.
*Chorionic villi attaching to the decidua basalis*
- This describes the **normal implantation** of the placenta into the decidua basalis of the uterus.
- This is the physiological process of pregnancy and would not cause the symptoms of vaginal bleeding, severe pain, and fetal distress described.
Umbilical cord prolapse US Medical PG Question 6: A 22-year-old woman, gravida 2, para 1, at 41 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been uncomplicated. At the beginning of the second stage of labor, the cervix is 100% effaced and 10 cm dilated; the vertex is at -1 station. The fetal heart rate is reactive with no decelerations. As she pushes, it is noted that the fetal heart rate decreases, as seen on cardiotocography (CTG). Which of the following is the most likely cause of this finding?
- A. Fetal myocardial depression
- B. Maternal hypotension
- C. Placental insufficiency
- D. Umbilical cord compression
- E. Fetal head compression (Correct Answer)
Umbilical cord prolapse Explanation: ***Fetal head compression***
- During the second stage of labor, **fetal head compression** commonly occurs with uterine contractions and maternal pushing efforts.
- This compression leads to a reflex vagal response, causing a **decrease in fetal heart rate (early decelerations)**, which is typically benign and resolves after the contraction.
*Fetal myocardial depression*
- **Fetal myocardial depression** can cause a decrease in fetal heart rate, but it is typically associated with **prolonged hypoxia or acidosis** and would likely manifest as late or prolonged decelerations or bradycardia, not just during pushing.
- There are no indications in the scenario of fetal distress or metabolic compromise that would point to myocardial depression.
*Maternal hypotension*
- **Maternal hypotension** would lead to **decreased placental perfusion**, resulting in **late decelerations** due to uteroplacental insufficiency.
- The scenario describes a reactive fetal heart rate with decelerations specifically during pushing, not a pattern consistent with sustained maternal hypotension impacting placental blood flow.
*Placental insufficiency*
- **Placental insufficiency** typically manifests as **late decelerations**, which are gradual decreases in fetal heart rate that begin after the peak of the contraction and return to baseline after the contraction ends.
- The fetal heart rate in the scenario is described as reactive with no decelerations prior to pushing, making placental insufficiency less likely as the primary cause of an acute deceleration during pushing.
*Umbilical cord compression*
- **Umbilical cord compression** causes **variable decelerations**, which are abrupt, often dramatic drops in fetal heart rate.
- While cord compression can occur during labor, the described pattern of deceleration specifically with pushing and the absence of other signs of cord impingement makes head compression a more direct and common cause in this context.
Umbilical cord prolapse US Medical PG Question 7: A 22-year-old primigravid woman at 41 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been uncomplicated. She has asthma treated with theophylline and inhaled corticosteroids. She has had 2 surgeries in the past to repair multiple lower limb and pelvis fractures that were the result of a car accident. She is otherwise healthy. Her temperature is 37.2°C (99°F) and blood pressure is 108/70 mm Hg. Examination shows the cervix is 100% effaced and 10 cm dilated; the vertex is at -4 station, with the occiput in the anterior position. Uterine activity is measured at 275 MVUs. Maternal pushing occurs during the contractions. Fetal heart tracing is 166/min and reactive with no decelerations. Epidural anesthesia is initiated for pain relief. After 4 hours of pushing, the vertex is found to be at -4 station, with increasing strength and rate of uterine contractions; fetal heart tracing shows late decelerations. Which of the following is the most likely cause of this patient's prolonged labor?
- A. Deep transverse arrest
- B. Insufficient uterine contraction
- C. Epidural anesthesia
- D. Cephalopelvic disproportion (Correct Answer)
- E. Inefficient maternal pushing
Umbilical cord prolapse Explanation: ***Cephalopelvic disproportion***
- The history of **multiple lower limb and pelvis fractures** from a car accident suggests a high likelihood of a **contracted or abnormally shaped pelvis**. This can lead to **cephalopelvic disproportion (CPD)**, where the fetal head cannot fit through the maternal pelvis despite adequate uterine contractions (275 MVUs).
- The combination of **prolonged labor** (4 hours of pushing with no descent), **vertex at -4 station** even after full dilation, increasing contraction strength, and new **late decelerations** (indicating fetal distress due to impaired oxygenation from prolonged compression) points towards an obstruction.
*Deep transverse arrest*
- This occurs when the fetal head rotates into the transverse diameter of the pelvis and fails to rotate anteriorly. While it causes **arrest of descent and dilation**, the primary issue is **malposition**, not a fundamental size mismatch.
- The occiput is described as in the **anterior position**, which does not immediately suggest deep transverse arrest.
*Insufficient uterine contraction*
- The uterine activity is measured at **275 MVUs**, which indicates **adequate contraction strength**. Insufficient contractions would typically be below 200 MVUs.
- While weak contractions can cause prolonged labor, the current uterine activity suggests this is not the primary problem.
*Epidural anesthesia*
- Epidural anesthesia can sometimes prolong the second stage of labor by reducing the urge to push or temporarily decreasing the effectiveness of pushing efforts. However, the patient's **strong uterine activity (275 MVUs)** and previous **pelvic fractures** make a mechanical obstruction (CPD) a more specific and likely cause of arrest in this scenario.
- Furthermore, the vertex remaining at -4 station for 4 hours despite strong contractions points to a physical barrier rather than just altered pushing dynamics.
*Inefficient maternal pushing*
- While inefficient maternal pushing can contribute to prolonged labor, the fetus remaining at -4 station for 4 hours with **strong uterine contractions (275 MVUs)** indicates that the issue is likely beyond just inadequate pushing efforts.
- The historical detail of **pelvic fractures** points more strongly to an anatomical obstruction rather than simply ineffective maternal exertion.
Umbilical cord prolapse US Medical PG Question 8: Five minutes after initiating a change of position and oxygen inhalation, the oxytocin infusion is discontinued. A repeat CTG that is done 10 minutes later shows recurrent variable decelerations and a total of 3 uterine contractions in 10 minutes. Which of the following is the most appropriate next step in management?
- A. Restart oxytocin infusion
- B. Emergent Cesarean section
- C. Administer terbutaline
- D. Monitor without intervention
- E. Amnioinfusion (Correct Answer)
Umbilical cord prolapse Explanation: ***Amnioinfusion***
- **Recurrent variable decelerations** persisting after discontinuing oxytocin and changing maternal position often indicate **cord compression**, which can be relieved by amnioinfusion.
- Adding fluid to the amniotic cavity **cushions the umbilical cord**, reducing compression during uterine contractions.
*Restart oxytocin infusion*
- Reinitiating oxytocin would likely **worsen the recurrent variable decelerations** by increasing uterine contraction frequency and intensity, thereby exacerbating cord compression.
- The goal is to alleviate fetal distress, not to intensify uterine activity that is already causing issues.
*Emergent Cesarean section*
- While an emergent Cesarean section is indicated for **unresolved fetal distress**, it's usually considered after less invasive measures, such as amnioinfusion, have failed.
- There is still an opportunity for a simpler intervention to resolve the issue before resorting to surgery.
*Administer terbutaline*
- Terbutaline is a **tocolytic agent** used to reduce uterine contractions, which can be helpful in cases of tachysystole or hyperstimulation.
- In this scenario, the contraction frequency is low (3 in 10 minutes), so reducing contractions is not the primary aim; rather, the focus is on resolving the cord compression causing decelerations.
*Monitor without intervention*
- **Recurrent variable decelerations** are an concerning sign of **fetal distress** and require intervention to prevent potential harm to the fetus.
- Simply monitoring without intervention would be inappropriate and could lead to worsening fetal hypoxemia and acidosis.
Umbilical cord prolapse US Medical PG Question 9: A 7-month-old girl is brought to the hospital by her mother, who complains of a lesion on the infant’s labia for the past 5 days. The lesion is 2 x 2 cm in size and red in color with serosanguinous fluid oozing out of the right labia. The parents note that the girl has had a history of recurrent bacterial skin infections with no pus but delayed healing since birth. She also had delayed sloughing of the umbilical cord at birth. Complete blood count results are as follows:
Neutrophils on admission
Leukocytes 19,000/mm3
Neutrophils 83%
Lymphocytes 10%
Eosinophils 1%
Basophils 1%
Monocytes 5%
Hemoglobin 14 g/dL
Which of the following compounds is most likely to be deficient in this patient?
- A. Selectin
- B. TNF-alpha
- C. Cellular adhesion molecule
- D. Integrin subunit (Correct Answer)
- E. vWF
Umbilical cord prolapse Explanation: **Integrin subunit** ✓
- The patient exhibits features consistent with **Leukocyte Adhesion Deficiency Type 1 (LAD-1)**, characterized by recurrent bacterial infections without pus formation, delayed umbilical cord separation, and **leukocytosis with neutrophil predominance** (due to inability of neutrophils to exit circulation and migrate to tissues).
- LAD-1 is caused by a defect in the **CD18 integrin β2 subunit**, which is essential for the function of β2 integrins (e.g., LFA-1, MAC-1, CR3) involved in firm adhesion and transmigration of leukocytes across the endothelium.
- The absence of pus despite bacterial infections is explained by the inability of neutrophils to migrate to infection sites.
*Selectin*
- **Selectins** (E-selectin, P-selectin, L-selectin) mediate the initial **rolling** phase of leukocyte adhesion to the endothelium.
- Defects in selectins (specifically fucose metabolism) are associated with **LAD-2 (Leukocyte Adhesion Deficiency Type 2)**, which presents with similar infection susceptibility but typically includes additional features like growth retardation, intellectual disability, and the Bombay blood phenotype.
*TNF-alpha*
- **TNF-alpha** is a pro-inflammatory cytokine that upregulates adhesion molecules on endothelial cells and activates immune responses.
- While TNF-alpha deficiency or blockade can increase infection susceptibility, it does not explain the specific constellation of delayed umbilical cord separation, persistent neutrophilic leukocytosis, and infections without pus formation seen in this patient.
*Cellular adhesion molecule*
- This is a broad, non-specific term encompassing multiple adhesion molecule families (integrins, selectins, immunoglobulin superfamily members, cadherins).
- While integrins are indeed cellular adhesion molecules, **"integrin subunit"** is the specific and precise answer for LAD-1, as the defect involves the β2 integrin subunit (CD18).
*vWF*
- **Von Willebrand Factor (vWF)** is crucial for platelet adhesion to damaged endothelium and serves as a carrier protein for factor VIII.
- Deficiency causes **Von Willebrand disease**, presenting with mucocutaneous bleeding (epistaxis, easy bruising, menorrhagia), not recurrent bacterial infections, delayed wound healing, or the immunologic abnormalities observed in this patient.
Umbilical cord prolapse US Medical PG Question 10: A 6-month-old girl presents with recurring skin infections. Past medical history is significant for 3 episodes of acute otitis media since birth. The patient was born at 39 weeks via an uncomplicated, spontaneous transvaginal delivery, but there was delayed umbilical cord separation. She has met all developmental milestones. On physical examination, the skin around her mouth is inflamed and red. Which of the following is most likely responsible for this child’s clinical presentation?
- A. Deficiency in NADPH oxidase
- B. IL-12 receptor deficiency
- C. Absence of CD18 molecule on the surface of leukocytes (Correct Answer)
- D. A microtubule dysfunction
- E. Defect in tyrosine kinase
Umbilical cord prolapse Explanation: ***Absence of CD18 molecule on the surface of leukocytes***
- The combination of **recurrent bacterial skin infections**, **otitis media**, and **delayed umbilical cord separation** is highly characteristic of **leukocyte adhesion deficiency type 1 (LAD-1)**.
- LAD-1 is caused by a defect in the **CD18 subunit of integrins**, leading to impaired leukocyte extravasation to sites of infection.
*Deficiency in NADPH oxidase*
- This defect is associated with **chronic granulomatous disease (CGD)**, which presents with recurrent infections by **catalase-positive organisms** and granuloma formation.
- While recurrent infections occur, **delayed umbilical cord separation** is not a typical feature of CGD.
*IL-12 receptor deficiency*
- This deficiency leads to impaired cellular immunity, particularly against **intracellular bacteria (e.g., mycobacteria)** and **fungi**.
- It does not typically present with the specific combination of **pyogenic infections** and **delayed umbilical cord separation** seen in this patient.
*A microtubule dysfunction*
- Microtubule dysfunction can be seen in conditions like **Chédiak-Higashi syndrome**, which involves impaired lysosomal trafficking and leads to **recurrent pyogenic infections**, **oculocutaneous albinism**, and **neuropathy**.
- **Delayed umbilical cord separation** is not a characteristic feature of Chédiak-Higashi syndrome.
*Defect in tyrosine kinase*
- Defects in tyrosine kinase, such as **Bruton's tyrosine kinase (BTK)**, cause **X-linked agammaglobulinemia**, leading to recurrent infections with **encapsulated bacteria** due to impaired B cell development.
- This condition is characterized by a lack of mature B cells and **low immunoglobulin levels**, but it does not typically present with **delayed umbilical cord separation**.
More Umbilical cord prolapse US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.