Trial of labor after cesarean US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Trial of labor after cesarean. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Trial of labor after cesarean US Medical PG Question 1: A 35-year-old G1 is brought to the emergency department because of sharp pains in her abdomen. She is at 30 weeks gestation based on ultrasound. She complains of feeling a little uneasy during the last 3 weeks of her pregnancy. She mentions that her abdomen has not been enlarging as expected and her baby is not moving as much as during the earlier part of the pregnancy. If anything, she noticed her abdomen has decreased in size. While she is giving her history, the emergency medicine physician notices that she is restless and is sweating profusely. An ultrasound is performed and her blood is sent for type and match. The blood pressure is 90/60 mm Hg, the pulse is 120/min, and the respiratory rate is 18/min. The fetal ultrasound is significant for no fetal heart motion or fetal movement. Her blood work shows the following: hemoglobin, 10.3 g/dL; platelet count, 1.1*10(5)/ml; bleeding time, 10 minutes; PT, 25 seconds; and PTT, 45 seconds. Which of the following would be the best immediate course of management for this patient?
- A. Low-molecular-weight heparin
- B. Fresh frozen plasma
- C. Initiation of labor
- D. D-dimer assay
- E. IV fluids (Correct Answer)
Trial of labor after cesarean Explanation: ***IV fluids***
- The patient presents with **hypotension** (90/60 mmHg) and **tachycardia** (120/min), indicating **hypovolemic shock**, likely due to concealed hemorrhage from abruptio placentae.
- **IV fluids** are the immediate priority to restore circulating blood volume and stabilize the patient's hemodynamic status.
*Low-molecular-weight heparin*
- This patient is experiencing signs of **disseminated intravascular coagulation (DIC)**, including thrombocytopenia, prolonged PT/PTT, and increased bleeding time, which makes anticoagulation contraindicated.
- Administering heparin would **exacerbate bleeding** and worsen her condition.
*Fresh frozen plasma*
- While **fresh frozen plasma (FFP)** can replace clotting factors and is indicated for DIC, stabilization of the patient's circulating volume with **IV fluids** is the most immediate life-saving measure in active shock.
- FFP should be given after initial fluid resuscitation and once the decision to deliver is made, to correct coagulopathy.
*Initiation of labor*
- Although the immediate delivery of the fetus is necessary to resolve ongoing placental abruption and DIC, the patient's **hemodynamic instability** must be addressed first.
- Stabilizing her with **IV fluids** is crucial before proceeding with labor induction or C-section.
*D-dimer assay*
- A **D-dimer assay** is a diagnostic test that would likely be elevated in this patient due to DIC, but it does not provide immediate therapeutic benefit.
- The patient's clinical presentation and other lab values (prolonged PT/PTT, thrombocytopenia) already strongly suggest DIC, and immediate intervention is required, not further diagnostic testing.
Trial of labor after cesarean US Medical PG Question 2: A 27-year-old G2P2002 is recovering in the hospital on postpartum day 3 after a low transverse C-section. During morning rounds, she reports a “pus-like” discharge and shaking chills overnight. She also endorses increased uterine cramping compared to the day before, but her postpartum course has otherwise been uneventful with a well-healing incision and normal vaginal bleeding. The patient’s prenatal care was complicated by HIV with a recent viral load of 400 copies/mL, type I diabetes well controlled on insulin, and a history of herpes simplex virus encephalitis in her first child. She did not have any genital lesions during the most recent pregnancy. Four days ago, she presented to the obstetric triage unit after spontaneous rupture of membranes and onset of labor. She made slow cervical change and reached full dilation after 16 hours, but there was limited fetal descent. Cephalopelvic disproportion was felt to be the reason for arrest of descent, so prophylactic ampillicin was administered and C-section was performed. A vaginal hand was required to dislodge the fetus’s head from the pelvis, and a healthy baby boy was delivered. On postpartum day 3, her temperature is 101.5°F (38.6°C), blood pressure is 119/82 mmHg, pulse is 100/min, and respirations are 14/min. Her incision looks clean and dry, there is mild suprapubic tenderness, and a foul yellow discharge tinged with blood is seen on her pad. Which of the following is the most significant risk factor for this patient’s presentation?
- A. HIV positive status
- B. Maternal diabetes
- C. C-section after onset of labor (Correct Answer)
- D. Prolonged rupture of membranes
- E. History of herpes simplex virus in previous pregnancy
Trial of labor after cesarean Explanation: ### **C-section after onset of labor**
* **Intrapartum C-sections**, especially after a prolonged period of labor and ruptured membranes as seen in this patient, significantly increase the risk of **postpartum endometritis** due to increased exposure to vaginal flora and manipulation.
* The clinical picture of fever, chills, uterine tenderness, and foul-smelling lochia is highly consistent with **endometritis**, and the mode of delivery after established labor is the most significant predisposing factor in this case.
### *HIV positive status*
* While HIV can compromise the immune system, the patient's viral load of 400 copies/mL suggests **moderately controlled HIV**, and opportunistic infections of this nature are less common with such a viral load.
* Moreover, **endometritis** is primarily an ascending polymicrobial infection, where the mechanical aspects of delivery often play a more direct role than systemic immunosuppression in its pathogenesis.
### *Maternal diabetes*
* **Diabetes** does increase the risk of infection in general, including postpartum infections, due to impaired immune function and altered microvasculature.
* However, in the context of the detailed obstetric history, the **C-section performed after a prolonged labor** is a more direct and significant risk factor for endometritis than diabetes alone.
### *Prolonged rupture of membranes*
* **Prolonged rupture of membranes (PROM)**, especially combined with prolonged labor, is indeed a risk factor for **chorioamnionitis** and subsequent **endometritis**.
* In this case, the patient had ruptured membranes for four days prior to presentation, but the specific mention of "C-section after onset of labor" encompasses the additional risk conferred by **vaginal examinations** during labor and surgical trauma.
### *History of herpes simplex virus in previous pregnancy*
* A history of **herpes simplex virus (HSV)** in a previous pregnancy is relevant for neonatal infection prevention in subsequent pregnancies if active lesions are present at the time of delivery.
* However, the patient had no genital lesions during this pregnancy, and **HSV is not a direct risk factor for postpartum endometritis**.
Trial of labor after cesarean US Medical PG Question 3: A 25-year-old woman comes to the emergency department one hour after the sudden onset of diffuse abdominal pain and nausea. She has no history of serious illness. Menses occur at regular 27-day intervals and last 4 to 6 days with moderate flow. Her last menstrual period was 6 weeks ago. She is sexually active with two sexual partners and uses oral contraceptive pills inconsistently. She appears pale and diaphoretic. Her temperature is 37.7°C (99.9°F), pulse is 120/min, respirations are 20/min, and blood pressure is 85/70 mm Hg. Abdominal examination shows diffuse abdominal tenderness. Pelvic examination shows a normal appearing vagina, cervix, and uterus, with right adnexal tenderness. Her hemoglobin concentration is 13 g/dL, leukocyte count is 10,000/mm3, and platelet count is 350,000/mm3. Results of a pregnancy test are pending. Which of the following is the most appropriate next step in management?
- A. Perform exploratory laparoscopy
- B. Perform pelvic ultrasound
- C. Perform CT scan of the abdomen and pelvis with contrast
- D. Administer intravenous normal saline fluids (Correct Answer)
- E. Transfuse O negative packed red blood cells
Trial of labor after cesarean Explanation: ***Administer intravenous normal saline fluids***
- The patient presents with classic signs of **hypovolemic shock**: sudden onset of severe abdominal pain, nausea, pallor, diaphoresis, tachycardia (120/min), and hypotension (85/70 mm Hg).
- Immediate administration of **intravenous fluids** is crucial to restore blood volume and stabilize her hemodynamics before further diagnostic or surgical interventions.
*Perform exploratory laparoscopy*
- While exploratory laparoscopy may ultimately be necessary if an **ectopic pregnancy rupture** is suspected, it is not the *immediate* next step before attempting hemodynamic stabilization.
- Performing surgery on a patient in **unresuscitatable shock** significantly increases morbidity and mortality.
*Perform pelvic ultrasound*
- A pelvic ultrasound is a valuable diagnostic tool, especially if an **ectopic pregnancy** is suspected given her missed period, sexual activity, and inconsistent contraception.
- However, in a patient with signs of **hemodynamic instability**, performing an ultrasound before fluid resuscitation wastes critical time and could worsen her condition.
*Perform CT scan of the abdomen and pelvis with contrast*
- A CT scan can provide detailed imaging of the abdomen and pelvis but is **less appropriate** than a pelvic ultrasound for initial evaluation of suspected gynecological causes of acute abdominal pain in a young woman.
- Furthermore, administering contrast to a patient in **shock** could exacerbate her condition and delay immediate life-saving interventions.
*Transfuse O negative packed red blood cells*
- Although the patient's symptoms strongly suggest **internal hemorrhage** (e.g., ruptured ectopic pregnancy), her initial hemoglobin (13 g/dL) is within the normal range.
- While blood products may eventually be needed, initial management of hypovolemic shock prioritizes **crystalloid fluid resuscitation** until blood products can be prepared and cross-matched, unless massive transfusion protocol is activated for severe, ongoing hemorrhage.
Trial of labor after cesarean US Medical PG Question 4: A 36-year-old woman, gravida 3, para 2, at 37 weeks' gestation comes to the emergency department because of sparse vaginal bleeding for 3 hours. She also noticed the bleeding 3 days ago. She has had no prenatal care. Both of her previous children were delivered by lower segment transverse cesarean section. Her temperature is 37.1°C (98.8°F), pulse is 90/min, respirations are 16/min, and blood pressure is 110/80 mm Hg. The abdomen is nontender, and no contractions are felt. Examination shows that the fetus is in a vertex presentation. The fetal heart rate is 160/min and shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Perform cesarean delivery
- B. Perform transvaginal sonography (Correct Answer)
- C. Perform Kleihauer-Betke test
- D. Perform pelvic examination
- E. Conduct contraction stress test
Trial of labor after cesarean Explanation: ***Perform transvaginal sonography***
- The history of **previous cesarean sections** and **painless vaginal bleeding** raises suspicion for **placenta previa**.
- **Transvaginal sonography** is the gold standard for diagnosing placenta previa, as it accurately visualizes the relationship between the placenta and the cervical os without increasing bleeding risk.
*Perform cesarean delivery*
- While a cesarean delivery may eventually be necessary if **placenta previa** is confirmed, it is premature to proceed without a definitive diagnosis.
- An immediate cesarean delivery is indicated only in cases of **heavy, uncontrolled bleeding** or fetal distress, neither of which is present here.
*Perform Kleihauer-Betke test*
- The **Kleihauer-Betke test** measures the amount of fetal hemoglobin transferred into the maternal bloodstream for quantifying **fetomaternal hemorrhage**, which is typically performed after a potential placental abruption or trauma.
- This test is not primarily used for diagnosing the **cause of vaginal bleeding** in this context and would not identify placenta previa.
*Perform pelvic examination*
- A **digital pelvic examination** is **contraindicated** in cases of suspected placenta previa due to the risk of exacerbating bleeding and potentially causing **massive hemorrhage**.
- Even a speculum examination should generally be deferred until a sonogram has ruled out placenta previa to avoid disturbing the placenta.
*Conduct contraction stress test*
- A **contraction stress test** assesses **fetal well-being** in response to uterine contractions and is used to evaluate uteroplacental insufficiency.
- It does not help in diagnosing the cause of **vaginal bleeding** and is not the appropriate first step in a patient with suspected placenta previa.
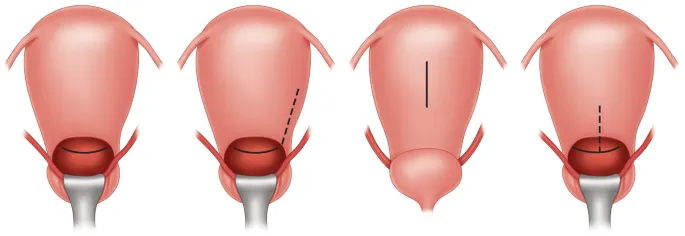
Trial of labor after cesarean US Medical PG Question 5: Three hours after the onset of labor, a 39-year-old woman, gravida 2, para 1, at 40 weeks' gestation has sudden worsening of abdominal pain and vaginal bleeding. 18 months ago her first child was delivered by a lower segment transverse cesarean section because of cephalopelvic disproportion. Her temperature is 37.5°C (99.5°F), pulse is 120/min, respirations are 20/min, and blood pressure is 90/50 mm Hg. Examination shows abdominal tenderness and the absence of uterine contractions. The cervix is 100% effaced and 10 cm dilated; the vertex is at -3 station. An hour before, the vertex was at 0 station. Cardiotocography shows fetal bradycardia, late decelerations, and decreased amplitude of uterine contractions. Which of the following is the most specific feature of this patient's condition?
- A. Loss of fetal station (Correct Answer)
- B. Fetal distress
- C. Abdominal tenderness
- D. Absent uterine contractions
- E. Hemodynamic instability
Trial of labor after cesarean Explanation: ***Loss of fetal station***
- The sudden **retraction of the presenting part** (vertex moving from 0 to -3 station) after a period of labor progression is a classical and highly specific sign of **uterine rupture**.
- This occurs because the uterus tears, allowing the fetus to partially or wholly slip out of the birth canal into the abdominal cavity.
*Fetal distress*
- While fetal bradycardia and late decelerations indicate **fetal distress**, this is a common finding in many obstetric emergencies, including placental abruption and cord prolapse, and is not specific to uterine rupture.
- Fetal distress reflects the immediate impact on the fetus but doesn't pinpoint the exact maternal pathology.
*Abdominal tenderness*
- **Abdominal tenderness** is a general symptom that can be present in various conditions such as placental abruption, chorioamnionitis, or even normal labor with strong contractions, making it non-specific for uterine rupture.
- The type of tenderness and its severity can vary, but by itself, it does not confirm a uterine rupture.
*Absent uterine contractions*
- The cessation of uterine contractions is a significant finding in uterine rupture, as the uterus can no longer effectively contract to expel the fetus.
- However, contractions can also decrease or become absent in cases of maternal exhaustion, failed induction, or excessive analgesia, thus not being entirely specific to rupture.
*Hemodynamic instability*
- The patient's **hypotension** (90/50 mm Hg) and **tachycardia** (120/min) indicate significant blood loss and **hypovolemic shock**, which commonly occur with uterine rupture.
- However, hemodynamic instability can also be seen in other severe obstetric hemorrhages like placental abruption or postpartum hemorrhage from other causes, making it a sensitive but non-specific indicator.
Trial of labor after cesarean US Medical PG Question 6: A 30-year-old woman, gravida 2 para 1, at 39 weeks gestation presents to the hospital with painful contractions and a rupture of membranes. She reports that the contractions started a couple hours ago and are now occurring every 4 minutes. She is accompanied by her husband who states, “her water broke an hour ago before we left for the hospital." The patient denies vaginal bleeding, and fetal movements are normal. The patient has attended all her pre-natal visits without pregnancy complications. She has no chronic medical conditions and takes only pre-natal vitamins. Her blood pressure is 110/75 mm Hg and pulse is 82/min. A fetal heart rate tracing shows a pulse of 140/min with moderate variability and no decelerations. Cervical examination reveals a cervix that is 7 cm dilated and 100% effaced with the fetal head at -1 station. The patient forgoes epidural anesthesia. During which of the following scenarios should a cesarean delivery be considered for this patient?
- A. Cervix is 7 cm dilated and fetal head is at 0 station after 4 hours, with contractions every 2 minutes (Correct Answer)
- B. Cervix is 7 cm dilated and fetal head is at -1 station after 2 hours with contractions every 7 minutes
- C. Cervix is 9 cm dilated and fetal head is at -1 station after 3 hours, with contractions every 3 minutes
- D. Cervix is 10 cm dilated and fetal head is at +1 station after 2 hours, with contractions every 2 minutes
- E. Cervix is 7 cm dilated and fetal head is at 0 station after 1 hour, with contractions every 5 minutes
Trial of labor after cesarean Explanation: ***Cervix is 7 cm dilated and fetal head is at 0 station after 4 hours, with contractions every 2 minutes***
- This scenario describes **arrest of active phase of labor** in a **multiparous woman**, defined as no cervical change for at least 4 hours with adequate contractions (every 2-3 minutes) or at least 6 hours with inadequate contractions.
- The patient started at 7 cm dilation and, after 4 hours of strong contractions, has shown no further cervical change, indicating failed labor progression and warranting C-section.
*Cervix is 7 cm dilated and fetal head is at -1 station after 2 hours with contractions every 7 minutes*
- This still represents the **active phase of labor** (from 6 cm dilation onwards), but the contractions are **inadequate** (every 7 minutes) and the duration of observation is too short to diagnose an arrest (2 hours vs. 4 hours for multiparous).
- The appropriate step would be to **augment labor** (e.g., with oxytocin) rather than proceed directly to C-section.
*Cervix is 9 cm dilated and fetal head is at -1 station after 3 hours, with contractions every 3 minutes*
- The patient has progressed from 7 cm to 9 cm, indicating **cervical change**, and contractions are adequate.
- This is not an arrest of labor; she is nearing full dilation and likely progressing appropriately.
*Cervix is 10 cm dilated and fetal head is at +1 station after 2 hours, with contractions every 2 minutes*
- This scenario describes the **second stage of labor** (complete cervical dilation), where the focus shifts to fetal descent. The fetal head has already descended to +1 station and contractions are adequate.
- While prolonged second stage can lead to C-section, the general threshold for intervention in a multiparous woman with epidural is 3 hours, and without epidural, it's 2 hours. This patient is at 2 hours and progressing, so a C-section is not immediately indicated.
*Cervix is 7 cm dilated and fetal head is at 0 station after 1 hour, with contractions every 5 minutes*
- This is still the **active phase of labor**, but the observation period (1 hour) is too short to diagnose an arrest of labor, even with inadequate contractions (every 5 minutes).
- The first step would be to ensure **adequate uterine activity** and observe for a longer period before considering a C-section.
Trial of labor after cesarean US Medical PG Question 7: A 35-year-old woman, gravida 4, para 3, at 34 weeks' gestation comes to the physician for a prenatal visit. She feels well. She does not note any contractions or fluid from her vagina. Her third child was delivered spontaneously at 35 weeks' gestation; pregnancy and delivery of her other two children were uncomplicated. Vital signs are normal. The abdomen is nontender and no contractions are felt. Pelvic examination shows a uterus consistent in size with a 34-weeks' gestation. Ultrasonography shows the fetus in a breech presentation. The fetal heart rate is 148/min. Which of the following is the most appropriate next step in management?
- A. Internal cephalic version
- B. Intravenous penicillin
- C. Cesarean section
- D. Observation (Correct Answer)
- E. External cephalic version
Trial of labor after cesarean Explanation: ***Observation***
- At 34 weeks' gestation, **spontaneous version** from **breech to cephalic presentation** can still occur, especially in multiparous women.
- Waiting until 37 weeks allows time for the fetus to turn naturally before considering interventions.
*Internal cephalic version*
- This procedure involves a physician inserting a hand into the uterus to manually turn the fetus from inside.
- It is typically performed during **labor** to correct a **malpresentation** once the cervix is dilated sufficiently and is not appropriate for an antepartum breech presentation.
*Intravenous penicillin*
- **Penicillin** is administered to prevent **Group B Streptococcus (GBS) transmission** to the neonate, usually during labor for GBS-positive mothers.
- There is no indication for **GBS prophylaxis** in this case, and GBS status is not provided.
*Cesarean section*
- While breech presentation often necessitates a **cesarean section**, it is generally planned for 39 weeks' gestation or when labor begins if other interventions fail.
- It is premature to schedule a **C-section** at 34 weeks, as the fetus might still undergo spontaneous version.
*External cephalic version*
- This procedure involves manually manipulating the fetus through the maternal abdomen to turn it from breech to cephalic.
- It is usually attempted at **37 weeks' gestation** to maximize success rates and minimize risks, as earlier attempts have lower success and higher re-version rates.
Trial of labor after cesarean US Medical PG Question 8: Five minutes after initiating a change of position and oxygen inhalation, the oxytocin infusion is discontinued. A repeat CTG that is done 10 minutes later shows recurrent variable decelerations and a total of 3 uterine contractions in 10 minutes. Which of the following is the most appropriate next step in management?
- A. Restart oxytocin infusion
- B. Emergent Cesarean section
- C. Administer terbutaline
- D. Monitor without intervention
- E. Amnioinfusion (Correct Answer)
Trial of labor after cesarean Explanation: ***Amnioinfusion***
- **Recurrent variable decelerations** persisting after discontinuing oxytocin and changing maternal position often indicate **cord compression**, which can be relieved by amnioinfusion.
- Adding fluid to the amniotic cavity **cushions the umbilical cord**, reducing compression during uterine contractions.
*Restart oxytocin infusion*
- Reinitiating oxytocin would likely **worsen the recurrent variable decelerations** by increasing uterine contraction frequency and intensity, thereby exacerbating cord compression.
- The goal is to alleviate fetal distress, not to intensify uterine activity that is already causing issues.
*Emergent Cesarean section*
- While an emergent Cesarean section is indicated for **unresolved fetal distress**, it's usually considered after less invasive measures, such as amnioinfusion, have failed.
- There is still an opportunity for a simpler intervention to resolve the issue before resorting to surgery.
*Administer terbutaline*
- Terbutaline is a **tocolytic agent** used to reduce uterine contractions, which can be helpful in cases of tachysystole or hyperstimulation.
- In this scenario, the contraction frequency is low (3 in 10 minutes), so reducing contractions is not the primary aim; rather, the focus is on resolving the cord compression causing decelerations.
*Monitor without intervention*
- **Recurrent variable decelerations** are an concerning sign of **fetal distress** and require intervention to prevent potential harm to the fetus.
- Simply monitoring without intervention would be inappropriate and could lead to worsening fetal hypoxemia and acidosis.
Trial of labor after cesarean US Medical PG Question 9: A 28-year-old woman at 30 weeks gestation is rushed to the emergency room with the sudden onset of vaginal bleeding accompanied by intense abdominopelvic pain and uterine contractions. The intensity and frequency of pain have increased in the past 2 hours. This is her 1st pregnancy and she was diagnosed with gestational diabetes several weeks ago. Her vital signs include a blood pressure of 124/68 mm Hg, a pulse of 77/min, a respiratory rate of 22/min, and a temperature of 37.0°C (98.6°F). The abdominal examination is positive for a firm and tender uterus. An immediate cardiotocographic evaluation reveals a fetal heart rate of 150/min with prolonged and repetitive decelerations and high-frequency and low-amplitude uterine contractions. Your attending physician warns you about delaying the vaginal physical examination until a quick sonographic evaluation is completed. Which of the following is the most likely diagnosis in this patient?
- A. Miscarriage
- B. Vasa previa
- C. Placenta abruption (Correct Answer)
- D. Placenta previa
- E. Uterine rupture
Trial of labor after cesarean Explanation: **Placenta abruption**
- The sudden onset of **vaginal bleeding** with **intense abdominopelvic pain**, **uterine contractions**, and a **firm, tender uterus** strongly suggests **placental abruption**.
- **Fetal decelerations** and the physician's warning against immediate vaginal examination (due to potential for exacerbating hemorrhage if it were placenta previa) further support this diagnosis.
*Miscarriage*
- This patient is at **30 weeks gestation**, whereas a miscarriage is defined as pregnancy loss before **20 weeks of gestation**.
- While bleeding and pain occur, the gestational age rules against a diagnosis of miscarriage.
*Vasa previa*
- **Vasa previa** is characterized by rupture of fetal vessels, leading to **fetal bleeding** and **sudden, painless vaginal bleeding**.
- The patient's presentation includes **intense abdominopelvic pain** and **uterine contractions**, which are not typical of vasa previa.
*Placenta previa*
- **Placenta previa** typically presents with **painless vaginal bleeding** and usually does not involve intense abdominal pain or a **firm, tender uterus**.
- The patient's symptoms of significant pain and uterine contractions are inconsistent with placenta previa.
*Uterine rupture*
- **Uterine rupture** is a catastrophic event, often preceded by a history of **uterine surgery** or trauma, and presents with sudden, severe pain, **fetal distress**, and a **palpable fetal parts** outside the uterus.
- While there is pain and fetal distress, the presence of a **firm, tender uterus** and the absence of a history of uterine surgery make abruption a more likely diagnosis.
Trial of labor after cesarean US Medical PG Question 10: A 30-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the hospital for regular, painful contractions that have been increasing in frequency. Her pregnancy has been complicated by gestational diabetes treated with insulin. Pelvic examination shows the cervix is 50% effaced and 4 cm dilated; the vertex is at -1 station. Ultrasonography shows no abnormalities. A tocometer and Doppler fetal heart monitor are placed on the patient's abdomen. The fetal heart rate monitoring strip shows a baseline heart rate of 145/min with a variability of ≥ 15/min. Within a 20-minute recording, there are 7 uterine contractions, 4 accelerations, and 3 decelerations that have a nadir occurring within half a minute. The decelerations occur at differing intervals relative to the contractions. Which of the following is the most appropriate next step in the management of this patient?
- A. Vibroacoustic stimulation
- B. Routine monitoring (Correct Answer)
- C. Administer tocolytics
- D. Emergent cesarean delivery
- E. Placement of fetal scalp electrode
Trial of labor after cesarean Explanation: ***Routine monitoring***
- The presented FHR tracing exhibits a **normal baseline rate** (145/min), **moderate variability** (≥15/min), and the presence of **accelerations**, indicating a reassuring fetal status.
- The described decelerations are **variable decelerations** due to their sudden onset, nadir within 30 seconds, and variable relationship to contractions, which are generally benign unless prolonged, deep, or repetitive. Given the otherwise reassuring status, continued routine monitoring is appropriate.
*Vibroacoustic stimulation*
- This intervention is used to elicit **fetal accelerations** or movement during non-stress tests (NSTs) when the fetus is quiet or shows a non-reactive pattern.
- In this case, the fetus is already showing **accelerations** and moderate variability, so stimulation is not needed to assess fetal well-being.
*Administer tocolytics*
- **Tocolytics** are used to stop or slow down labor, typically in cases of preterm labor or uterine tachysystole causing fetal distress.
- This patient is at **38 weeks' gestation** and in active labor, and there are no signs of fetal distress warranting the cessation of contractions.
*Emergent cesarean delivery*
- **Emergent cesarean delivery** is indicated for acute fetal distress, such as prolonged decelerations, significant bradycardia, or absent variability in conjunction with other concerning FHR patterns.
- The FHR tracing described is largely reassuring with moderate variability and accelerations, and the variable decelerations are not indicative of immediate threat, making emergent delivery unnecessary.
*Placement of fetal scalp electrode*
- A **fetal scalp electrode** provides a more accurate and continuous measure of the FHR, often used when external monitoring is difficult or when there are concerns about the reliability of the tracing.
- While it can be useful in some situations, the current tracing is **interpretable as reassuring**, making invasive monitoring currently unnecessary.
More Trial of labor after cesarean US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.