Shoulder dystocia management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Shoulder dystocia management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Shoulder dystocia management US Medical PG Question 1: A 29-year-old woman, gravida 1, para 0, at 36 weeks' gestation is brought to the emergency department after an episode of dizziness and vomiting followed by loss of consciousness lasting 1 minute. She reports that her symptoms started after lying down on her back to rest, as she felt tired during yoga class. Her pregnancy has been uncomplicated. On arrival, she is diaphoretic and pale. Her pulse is 115/min and blood pressure is 90/58 mm Hg. On examination, the patient is lying in the supine position with a fundal height of 36 cm. There is a prolonged fetal heart rate deceleration to 80/min. Which of the following is the most appropriate action to reverse this patient's symptoms in the future?
- A. Performing the Muller maneuver
- B. Gentle compression with an abdominal binder
- C. Lying in the supine position and elevating legs
- D. Lying in the left lateral decubitus position (Correct Answer)
- E. Performing the Valsava maneuver
Shoulder dystocia management Explanation: ***Lying in the left lateral decubitus position***
- This position relieves **aortocaval compression** by moving the uterus off the **inferior vena cava (IVC)** and aorta.
- Alleviating IVC compression increases **venous return** to the heart, improving **cardiac output** and blood pressure, thereby resolving the patient's symptoms and improving **fetal oxygenation**.
*Performing the Muller maneuver*
- The **Muller maneuver** involves forced inspiration against a closed glottis, creating **negative intrathoracic pressure**.
- This maneuver is used to evaluate **upper airway compromise** and would not address the underlying issue of aortocaval compression.
*Gentle compression with an abdominal binder*
- An **abdominal binder** would apply external pressure to the abdomen, which could worsen rather than alleviate **aortocaval compression**.
- This would further reduce **venous return** and potentially exacerbate the patient's **hypotension** and fetal distress.
*Lying in the supine position and elevating legs*
- Lying in the **supine position** is the cause of the patient's symptoms due to **aortocaval syndrome**.
- While **elevating the legs** can temporarily increase venous return from the legs, it would not relieve the compression of the IVC by the gravid uterus.
*Performing the Valsava maneuver*
- The **Valsalva maneuver** involves forced exhalation against a closed glottis, which increases **intrathoracic pressure** and decreases **venous return**.
- This would further reduce **cardiac output** and worsen the symptoms of **hypotension** and **fetal compromise**.
Shoulder dystocia management US Medical PG Question 2: A 31-year-old G3P1 woman who is at 37 weeks of gestation is brought into the emergency department by her husband after repeated twitching. According to the husband, they were watching TV when she suddenly became unresponsive and her hands and legs started shaking. The episode lasted about 5 minutes and she “seemed to be sleeping afterwards.” Her past medical history is significant for pregnancy induced hypertension. The patient is tired but responsive and denies urinary incontinence, paresthesia, fever, upper respiratory signs, or new medication changes. She denies a history of seizures. Her temperature is 99°F (37°C), blood pressure is 186/97 mmHg, pulse is 96/min, and respirations are 12/min. Physical examination demonstrates a lethargic patient with moderate right upper quadrant tenderness. What is the most appropriate next step for this patient?
- A. Emergency cesarean section
- B. Expectant management
- C. Intravenous ampicillin and gentamicin
- D. Intravenous infusion of oxytocin
- E. Intravenous magnesium sulfate (Correct Answer)
Shoulder dystocia management Explanation: ***Intravenous magnesium sulfate***
- The patient exhibits classic signs of **eclampsia**: new-onset generalized tonic-clonic seizures in a pregnant woman with a history of **pregnancy-induced hypertension** and **preeclampsia** symptoms (elevated BP, RUQ tenderness, lethargy postpartum).
- **Magnesium sulfate** is the first-line treatment for preventing and managing seizures in eclampsia, reducing seizure recurrence risk and improving maternal outcomes.
*Emergency cesarean section*
- While delivery is the definitive treatment for preeclampsia/eclampsia, the immediate priority after a seizure is to **stabilize the mother** and prevent further complications with anticonvulsant therapy.
- An emergency cesarean section would be considered after **maternal stabilization** but **not as the immediate first step** in an actively seizing or recently seized eclamptic patient.
*Expectant management*
- **Expectant management** is inappropriate given the patient's critical condition with a seizure (eclampsia).
- Eclampsia requires **urgent aggressive intervention** to prevent maternal and fetal morbidity and mortality.
*Intravenous ampicillin and gentamicin*
- **Antibiotics** (ampicillin and gentamicin) are used to treat suspected bacterial infections, particularly in cases of chorioamnionitis or postpartum endometritis.
- There are **no signs of infection** in this patient (no fever, no upper respiratory signs, no urinary incontinence), making antibiotics an inappropriate initial treatment.
*Intravenous infusion of oxytocin*
- **Oxytocin** is used to induce labor or augment uterine contractions and prevent postpartum hemorrhage.
- It is **not indicated** for the acute management of eclampsia or seizures, nor is it the immediate step even if delivery is planned, as maternal stabilization with magnesium sulfate comes first.
Shoulder dystocia management US Medical PG Question 3: A 2-day-old boy is evaluated in the nursery for minimal movement in his left upper limb. He was born at 41 weeks gestation by an assisted forceps-vaginal delivery to a 42-year-old obese woman. Birth weight was 4.4 kg (9.7 lb). The mother had 4 previous vaginal deliveries, all requiring forceps. Examinations of the left upper limb show that the arm hangs by his side and is rotated medially. His forearm is extended and pronated, and his wrist and fingers are flexed. Moro reflex is present only on the right side. Which of the following muscles was spared from the injury sustained during delivery?
- A. Biceps
- B. Supraspinatus
- C. Infraspinatus
- D. Deltoid
- E. Triceps (Correct Answer)
Shoulder dystocia management Explanation: ***Triceps***
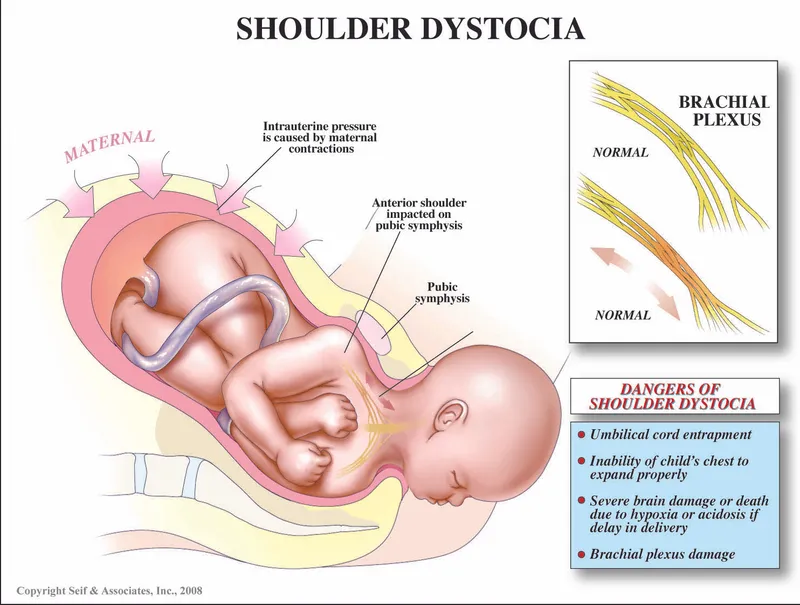
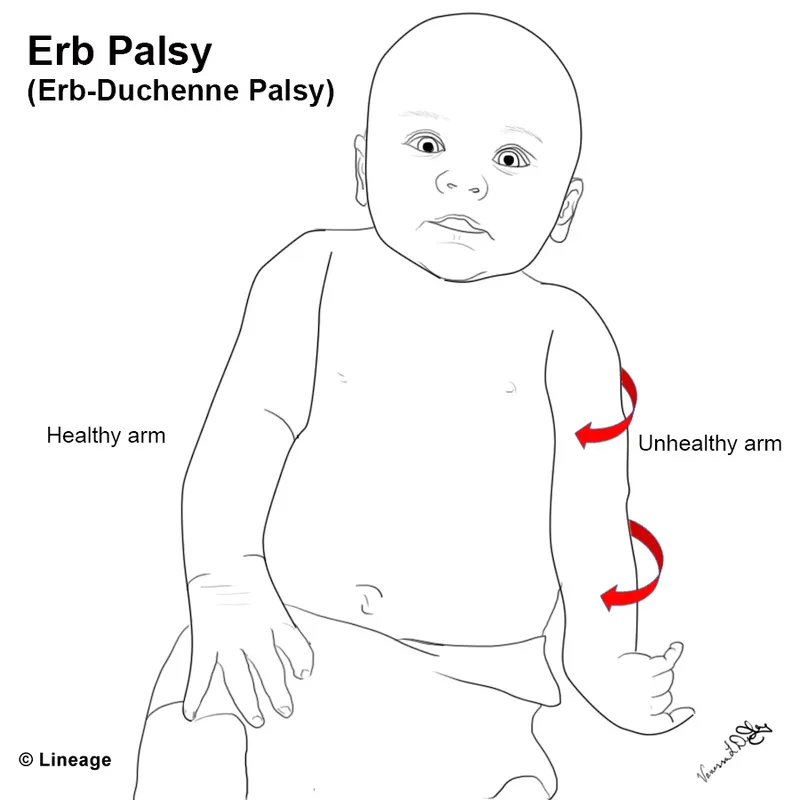
- The patient's presentation is consistent with **Erb-Duchenne palsy**, affecting the **C5-C6 nerve roots** of the brachial plexus.
- The **triceps muscle** is innervated by the **radial nerve** originating from **C6, C7, and C8**, with **C7 and C8 providing the predominant innervation**.
- Since the injury involves primarily **C5-C6**, and the triceps depends mainly on **C7-C8**, it is **functionally spared** in Erb's palsy.
*Biceps*
- The **biceps muscle** is innervated by the **musculocutaneous nerve** (C5-C6) and is responsible for **flexion and supination** of the forearm.
- Its involvement explains the **extended and pronated** forearm observed in Erb's palsy.
*Supraspinatus*
- The **supraspinatus muscle** is innervated by the **suprascapular nerve** (C5-C6) and is crucial for the **initiation of shoulder abduction**.
- Injury to its innervation contributes to the arm hanging by the side.
*Infraspinatus*
- The **infraspinatus muscle** is also innervated by the **suprascapular nerve** (C5-C6) and is responsible for **external rotation** of the humerus.
- Its paralysis leads to the **medially rotated** arm seen in Erb's palsy.
*Deltoid*
- The **deltoid muscle** is innervated by the **axillary nerve** (C5-C6) and primarily functions in **shoulder abduction** and shoulder flexion/extension.
- Damage to this innervation contributes to the inability to abduct the arm.
Shoulder dystocia management US Medical PG Question 4: A 23-year-old woman comes to the emergency department because of increasing abdominal pain with associated nausea and vomiting. The symptoms began suddenly after having intercourse with her partner six hours ago. There is no associated fever, diarrhea, vaginal bleeding, or discharge. Menarche was at the age of 13 years and her last menstrual period was 4 weeks ago. She uses combination contraceptive pills. She had an appendectomy at the age of 12. Her temperature is 37.5°C (99.5°F), pulse is 100/min, respirations are 22/min, and blood pressure is 110/70 mm Hg. Abdominal examination shows severe right lower quadrant tenderness with associated rebound and guarding. Pelvic examination shows scant, clear vaginal discharge and right adnexal tenderness. There is no cervical wall motion tenderness. Her hemoglobin concentration is 10.5 g/dL, leukocyte count is 9,000/mm3, and platelet count is 250,000/mm3. A urine pregnancy test is negative. Which of the following imaging findings is most likely?
- A. Increased ovarian blood flow on doppler
- B. Decreased ovarian blood flow on doppler (Correct Answer)
- C. Complex, echogenic intrauterine mass
- D. Distended fallopian tube with incomplete septations
- E. Echogenic tubal ring
Shoulder dystocia management Explanation: ***Decreased ovarian blood flow on doppler***
- This clinical presentation, particularly the sudden onset of **unilateral abdominal pain** after intercourse, associated nausea/vomiting, and severe right lower quadrant tenderness with rebound/guarding, is highly suggestive of **ovarian torsion**.
- **Ovarian torsion** *is a medical emergency in which the ovary twists on its pedicle, obstructing its blood supply. This causes rapid onset of symptoms and can lead to necrosis of the ovary if not promptly treated.* **Doppler ultrasound** *will show decreased or absent blood flow to the affected ovary, which is key to its diagnosis*.
*Increased ovarian blood flow on doppler*
- **Increased ovarian blood flow** would suggest an inflammatory process or a highly vascularized mass, which is less consistent with the acute, severe ischemic pain described.
- *While some inflammatory conditions or ruptured cysts might present with similar pain, the sudden, severe nature following intercourse points towards a mechanical event like torsion rather than increased flow.*
*Complex, echogenic intrauterine mass*
- A **complex, echogenic intrauterine mass** is indicative of conditions like fibroids, polyps, or retained products of conception, typically presenting with abnormal uterine bleeding or chronic pelvic pain, not acute unilateral abdominal pain after intercourse.
- *The absence of vaginal bleeding and a negative pregnancy test further rule out most intrauterine pregnancy-related issues.*
*Distended fallopian tube with incomplete septations*
- A **distended fallopian tube with incomplete septations** is a hallmark of **hydrosalpinx** or **pyosalpinx**, often associated with pelvic inflammatory disease (PID).
- *While PID can cause adnexal tenderness, the acute onset after intercourse with guarding and rebound in the absence of fever, vaginal discharge (except scant clear), or cervical motion tenderness makes PID less likely.*
*Echogenic tubal ring*
- An **echogenic tubal ring** is a classic sign of an **ectopic pregnancy** within the fallopian tube.
- *The patient's negative urine pregnancy test makes ectopic pregnancy extremely unlikely, despite the adnexal pain.*
Shoulder dystocia management US Medical PG Question 5: A 29-year-old G2P1 at 35 weeks gestation presents to the obstetric emergency room with vaginal bleeding and severe lower back pain. She reports the acute onset of these symptoms 1 hour ago while she was outside playing with her 4-year-old son. Her prior birthing history is notable for an emergency cesarean section during her first pregnancy. She received appropriate prenatal care during both pregnancies. She has a history of myomectomy for uterine fibroids. Her past medical history is notable for diabetes mellitus. She takes metformin. Her temperature is 99.0°F (37.2°C), blood pressure is 104/68 mmHg, pulse is 120/min, and respirations are 20/min. On physical examination, the patient is in moderate distress. Large blood clots are removed from the vaginal vault. Contractions are occurring every 2 minutes. Delayed decelerations are noted on fetal heart monitoring. Which of the following is the most likely cause of this patient's symptoms?
- A. Premature separation of a normally implanted placenta (Correct Answer)
- B. Amniotic sac rupture prior to the start of uterine contractions
- C. Placental implantation over internal cervical os
- D. Chorionic villi attaching to the myometrium
- E. Chorionic villi attaching to the decidua basalis
Shoulder dystocia management Explanation: ***Premature separation of a normally implanted placenta***
- The acute onset of **vaginal bleeding**, **severe lower back pain**, frequent uterine contractions, and **fetal decelerations** in a patient with risk factors like a prior cesarean section and diabetes mellitus are highly suggestive of **abruptio placentae**.
- **Uterine tenderness** and a **firm, rigid uterus** (though not explicitly stated, implied by contractions and pain) are also characteristic findings.
*Amniotic sac rupture prior to the start of uterine contractions*
- This condition presents with a gush of fluid from the vagina, often without significant bleeding or severe pain unless associated with other complications.
- While it can lead to preterm labor, it doesn't directly cause the severe back pain, heavy bleeding with clots, and fetal distress seen here.
*Placental implantation over internal cervical os*
- This describes **placenta previa**, which typically presents with **painless vaginal bleeding**, often bright red, without severe abdominal or back pain.
- The presence of severe abdominal pain and uterine contractions makes placenta previa less likely.
*Chorionic villi attaching to the myometrium*
- This describes **placenta accreta**, a condition where the placenta abnormally adheres to the myometrium. It is typically diagnosed postnatally with **difficulty in placental separation** and severe hemorrhage.
- While a prior C-section is a risk factor, the acute presentation of pain and bleeding in the antepartum period is not the classic presentation of accreta alone.
*Chorionic villi attaching to the decidua basalis*
- This describes the **normal implantation** of the placenta into the decidua basalis of the uterus.
- This is the physiological process of pregnancy and would not cause the symptoms of vaginal bleeding, severe pain, and fetal distress described.
Shoulder dystocia management US Medical PG Question 6: A 25-year-old G2P1001 at 32 weeks gestation presents to the hospital with painless vaginal bleeding. The patient states that she was taking care of laundry at home when she experienced a sudden sensation of her water breaking and saw that her groin was covered in blood. Her prenatal history is unremarkable according to the clinic records, but she has not seen an obstetrician for the past 14 weeks. Her previous delivery was by urgent cesarean section for placenta previa. Her temperature is 95°F (35°C), blood pressure is 125/75 mmHg, pulse is 79/min, respirations are 18/min, and oxygen saturation is 98% on room air. Cervical exam shows gross blood in the vaginal os. The fetal head is not palpable. Fetal heart rate monitoring demonstrates decelerations and bradycardia. Labs are pending. IV fluids are started. What is the best next step in management?
- A. Cesarean section (Correct Answer)
- B. Betamethasone
- C. Red blood cell transfusion
- D. Vaginal delivery
- E. Lumbar epidural block
Shoulder dystocia management Explanation: ***Cesarean section***
- This patient presents with signs highly suggestive of **placenta previa with possible vasa previa or placental abruption**, with life-threatening complications for both mother and fetus. The presence of **painless vaginal bleeding**, a prior **cesarean section for placenta previa**, and **fetal heart rate decelerations/bradycardia** necessitate immediate delivery via cesarean section to prevent **fetal demise** and severe **maternal hemorrhage**.
- The rapid deterioration of the fetal status, indicated by **decelerations and bradycardia**, confirms the urgency. A **cesarean section** is the quickest and safest way to deliver the baby and address the underlying obstetric emergency.
*Betamethasone*
- **Betamethasone** is administered to promote **fetal lung maturity** in cases of preterm delivery. While this patient is preterm at 32 weeks, the critical nature of the fetal distress and bleeding requires immediate delivery, making the delay for betamethasone administration inappropriate.
- The benefits of steroids for lung maturity are outweighed by the **immediate risk of fetal demise** and severe maternal complications if delivery is delayed.
*Red blood cell transfusion*
- While the patient is actively bleeding and may eventually require a **blood transfusion**, starting IV fluids and proceeding with an **immediate cesarean section** are higher priorities to stabilize the mother and rescue the fetus.
- Transfusions are supportive measures once the source of hemorrhage is addressed and vital signs are stabilized during or after surgery.
*Vaginal delivery*
- Given the patient's history of **placenta previa**, current **painless vaginal bleeding**, and signs of **fetal distress**, a vaginal delivery is contraindicated due to the high risk of **exsanguinating hemorrhage** for the mother and severe fetal compromise.
- The prior **cesarean section for placenta previa** also increases the risk of recurrent previa and **placenta accreta spectrum**, further contraindicating vaginal delivery.
*Lumbar epidural block*
- A **lumbar epidural block** is used for pain management during labor, but in this emergent situation with active bleeding and fetal distress, immediate delivery is paramount.
- The time required to safely administer an **epidural**, along with the potential for **hypotension** in a hypovolemic patient, makes it an inappropriate next step.
Shoulder dystocia management US Medical PG Question 7: A newborn infant is born at 41 weeks gestation to a healthy G1P0 mother. The delivery was complicated by shoulder dystocia. The infant is in the 89th and 92nd percentiles for height and weight, respectively. The mother's past medical history is notable for diabetes mellitus and obesity. Immediately after birth, the child's temperature is 99°F (37.2°C), blood pressure is 90/50 mmHg, pulse is 120/min, and respirations are 24/min. The child demonstrates a strong cry and pink upper and lower extremities bilaterally. The left arm is adducted and internally rotated at the shoulder and extended at the elbow. Extension at the elbow and flexion and extension of the wrist appear to be intact in the left upper extremity. The right upper extremity appears to have normal strength and range of motion in all planes. Which of the following sets of nerves or nerve roots is most likely affected in this patient?
- A. Axillary nerve only
- B. Suprascapular nerve only
- C. C5 and C6 nerve roots (Correct Answer)
- D. C5, C6, and C7 nerve roots
- E. Musculocutaneous nerve only
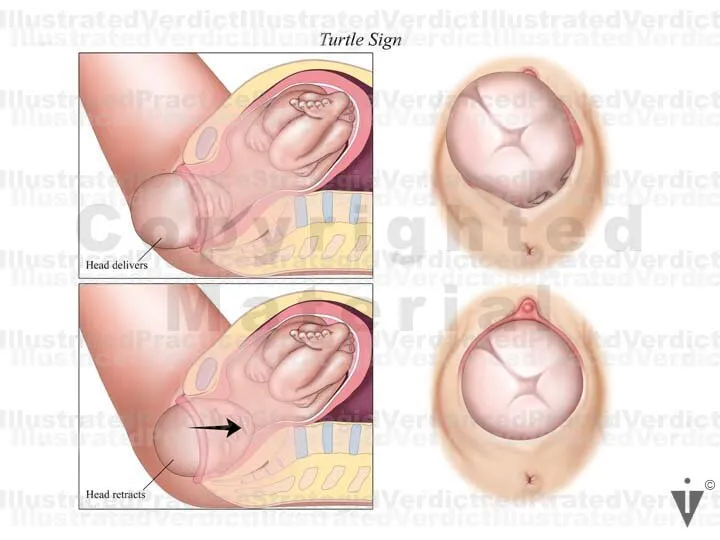
Shoulder dystocia management Explanation: ***C5 and C6 nerve roots***
- The presentation of a newborn with an adducted and internally rotated shoulder, and an extended elbow, is characteristic of **Erb's palsy**, which results from injury to the **upper brachial plexus** (C5-C6 nerve roots). This classic "waiter's tip" position affects muscles innervated by these roots, including the **deltoid**, **supraspinatus**, **infraspinatus**, and **biceps brachii**.
- **Shoulder dystocia** during a complicated delivery is a common cause of Erb's palsy due to excessive lateral traction on the neck, stretching the upper brachial plexus.
*Axillary nerve only*
- Injury to the **axillary nerve** primarily affects **shoulder abduction** (deltoid) and sensation over the lateral shoulder. While abduction is compromised in Erb's palsy, other impairments like **elbow flexion** weakness indicate more widespread nerve involvement than just the axillary nerve.
- The axillary nerve is a terminal branch of the posterior cord, which is formed by the posterior divisions of the upper, middle, and lower trunks of the brachial plexus.
*Suprascapular nerve only*
- The **suprascapular nerve** innervates the **supraspinatus** and **infraspinatus muscles**, responsible for the initial 15 degrees of shoulder abduction and external rotation, respectively. While these movements are affected in Erb's palsy, the presentation also includes **elbow extension** (due to biceps weakness), indicating involvement beyond just the suprascapular nerve.
- This nerve originates directly from the **upper trunk** of the brachial plexus (C5-C6).
*C5, C6, and C7 nerve roots*
- Involvement of the **C7 nerve root** would typically lead to additional weakness in the **wrist extensors** and **finger extensors**, which are noted as intact in the left upper extremity.
- This more extensive injury would suggest a **total brachial plexus palsy** or a more severe form of Erb's palsy that extends into the middle trunk, which is not fully supported by the intact wrist and finger movements.
*Musculocutaneous nerve only*
- The **musculocutaneous nerve** primarily innervates the **biceps brachii**, **brachialis**, and **coracobrachialis muscles**, responsible for **elbow flexion**. While elbow flexion is impaired in this case, the additional **shoulder adduction** and **internal rotation** dysfunction, due to weakness in the deltoid and rotator cuff, points to a broader injury involving the C5-C6 nerve roots rather than an isolated musculocutaneous nerve lesion.
- This nerve is a terminal branch of the lateral cord, formed by the anterior divisions of the upper and middle trunks (C5-C7).
Shoulder dystocia management US Medical PG Question 8: A 31-year-old G6P6 woman with a history of fibroids gives birth to twins via vaginal delivery. Her pregnancy was uneventful, and she reported having good prenatal care. Both placentas are delivered immediately after the birth. The patient continues to bleed significantly over the next 20 minutes. Her temperature is 97.0°F (36.1°C), blood pressure is 124/84 mmHg, pulse is 95/min, respirations are 16/min, and oxygen saturation is 98% on room air. Continued vaginal bleeding is noted. Which of the following is the most appropriate initial step in management?
- A. Oxytocin
- B. Blood product transfusion
- C. Uterine artery embolization
- D. Hysterectomy
- E. Bimanual massage (Correct Answer)
Shoulder dystocia management Explanation: ***Bimanual massage***
- The patient is experiencing **postpartum hemorrhage (PPH)**, indicated by significant bleeding post-delivery. **Uterine atony** is the most common cause of PPH, and bimanual massage helps stimulate uterine contractions to reduce bleeding.
- This is a **first-line, non-pharmacological intervention** that can be rapidly initiated to manage uterine atony.
*Oxytocin*
- While **oxytocin** is a uterotonic agent used to treat PPH, the initial step is typically **bimanual massage** to physically stimulate the uterus while preparing for medication administration.
- Oxytocin infusion would be administered concurrent with or immediately following bimanual massage, but manual compression is often initiated first.
*Blood product transfusion*
- Blood product transfusion is indicated for significant blood loss and hemodynamic instability, but it is a **supportive measure** rather than an initial intervention to stop the bleeding.
- The patient's current **blood pressure (124/84 mmHg)** and **pulse (95/min)** do not immediately suggest severe hypovolemic shock requiring immediate transfusion as the *first* step before attempting to control the source of bleeding.
*Uterine artery embolization*
- **Uterine artery embolization** is a highly invasive procedure typically reserved for cases where conservative measures, including uterotonic agents and bimanual compression, have failed to control PPH.
- It is not an appropriate initial step, as it requires specialized equipment and personnel and would delay immediate management of active bleeding.
*Hysterectomy*
- **Hysterectomy** is a last-resort intervention for intractable PPH that cannot be controlled by all other methods, including uterotonics, uterine massage, and other surgical or interventional radiology techniques.
- It is a highly invasive procedure with significant morbidity and is not considered an initial management step.
Shoulder dystocia management US Medical PG Question 9: A 5-year-old boy presents for a regularly scheduled check-up. The child is wheelchair bound due to lower extremity paralysis and suffers from urinary incontinence. At birth, it was noted that the child had lower limbs of disproportionately small size in relation to the rest of his body. Radiograph imaging at birth also revealed several abnormalities in the spine, pelvis, and lower limbs. Complete history and physical performed on the child's birth mother during her pregnancy would likely have revealed which of the following?
- A. Maternal use of nicotine
- B. Maternal use of tetracyclines
- C. Maternal hyperthyroidism
- D. Maternal use of lithium
- E. Uncontrolled maternal diabetes mellitus (Correct Answer)
Shoulder dystocia management Explanation: ***Uncontrolled maternal diabetes mellitus***
- **Maternal diabetes** is a significant risk factor for **caudal regression syndrome**, which presents with **lower limb paralysis**, **urinary incontinence**, and **spinal/pelvic abnormalities**.
- The combination of disproportionately small lower limbs and the associated neurological and skeletal issues strongly points to a congenital anomaly linked to **poor glycemic control** during pregnancy.
*Maternal use of nicotine*
- Maternal nicotine use is associated with a range of adverse pregnancy outcomes, including **low birth weight**, **premature birth**, and **respiratory problems**, but not typically caudal regression syndrome.
- While concerning, it does not directly explain the specific constellation of skeletal, neurological, and urological abnormalities described.
*Maternal use of tetracyclines*
- **Tetracycline exposure** during pregnancy can lead to **tooth discoloration** and **bone growth inhibition**, particularly in the developing fetus.
- It is not known to cause the severe spinal and lower limb malformations, paralysis, or urinary incontinence seen in this case.
*Maternal hyperthyroidism*
- Uncontrolled maternal hyperthyroidism can lead to complications such as **fetal tachycardia**, **goiter**, and **preterm birth**.
- It is not directly associated with congenital malformations like caudal regression syndrome that affect the lower spine and limbs.
*Maternal use of lithium*
- Maternal lithium use is most notably associated with an increased risk of **Ebstein's anomaly**, a congenital **heart defect**.
- It does not explain the specific musculoskeletal, neurological, and urological abnormalities presented in the case.
Shoulder dystocia management US Medical PG Question 10: A 31-year-old G1P0000 presents to her obstetrician for her first prenatal visit after having a positive home pregnancy test one week ago. She states that her last menstrual period was 8 weeks ago. The patient has a past medical history of type I diabetes mellitus since childhood and is on insulin. Her hemoglobin A1c two weeks ago was 13.7%. At that time, she was also found to have microalbuminuria on routine urinalysis, and her primary care provider prescribed lisinopril but the patient has not yet started taking it. The patient’s brother is autistic, but family history is otherwise unremarkable. At this visit, her temperature is 98.6°F (37.0°C), blood pressure is 124/81 mmHg, pulse is 75/min, and respirations are 14/min. Exam is unremarkable. This fetus is at increased risk for which of the following?
- A. Post-term delivery
- B. Oligohydramnios
- C. Neural tube defect (Correct Answer)
- D. Aneuploidy
- E. Neonatal hyperglycemia
Shoulder dystocia management Explanation: ***Neural tube defect***
- The patient's **poorly controlled type 1 diabetes mellitus** is evidenced by her **HbA1c of 13.7%**. Uncontrolled maternal hyperglycemia during organogenesis significantly increases the risk for fetal malformations, including neural tube defects due to impaired folate metabolism.
- This risk is highest when hyperglycemia occurs during the first 8 weeks of gestation, a period crucial for neural tube closure, which aligns with this patient's presentation at 8 weeks' gestation.
*Post-term delivery*
- **Uncontrolled maternal diabetes** is typically associated with **macrosomia and polyhydramnios**, which can lead to complications such as **shoulder dystocia, premature rupture of membranes (PROM)**, and often precipitates **earlier induction of labor** rather than post-term delivery.
- While exact delivery timing can vary, the direct causal link between uncontrolled diabetes and post-term delivery is not primary; rather, such pregnancies are often managed with earlier interventions.
*Oligohydramnios*
- Poorly controlled maternal diabetes, particularly type 1, is generally associated with **polyhydramnios** due to fetal polyuria caused by hyperglycemia, not oligohydramnios.
- **Oligohydramnios** can be associated with severe **placental insufficiency**, prolonged rupture of membranes, or fetal renal agenesis, none of which are directly indicated by uncontrolled maternal diabetes alone.
*Aneuploidy*
- The primary risk factor for **aneuploidy** (e.g., Down syndrome) is **advanced maternal age**, which is not present in this 31-year-old patient.
- **Maternal diabetes** itself is not a direct risk factor for aneuploidy; genetic factors related to nondisjunction are the main cause.
*Neonatal hyperglycemia*
- Maternal hyperglycemia leads to fetal hyperglycemia, causing **fetal hyperinsulinemia**. After birth, the neonate's elevated insulin levels, in the absence of maternal glucose supply, result in **neonatal hypoglycemia**, not hyperglycemia.
- **Neonatal hyperglycemia** is rare and usually associated with specific genetic defects or administration of excessive glucose postnatally, not maternal diabetes.
More Shoulder dystocia management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.