Premature rupture of membranes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Premature rupture of membranes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Premature rupture of membranes US Medical PG Question 1: A 35-year-old G3P2 woman currently 39 weeks pregnant presents to the emergency department with painful vaginal bleeding shortly after a motor vehicle accident in which she was a passenger. She had her seat belt on and reports that the airbag deployed immediately upon her car's impact against a tree. She admits that she actively smokes cigarettes. Her prenatal workup is unremarkable. Her previous pregnancies were remarkable for one episode of chorioamnionitis that resolved with antibiotics. Her temperature is 98.6°F (37°C), blood pressure is 90/60 mmHg, pulse is 130/min, and respirations are 20/min. The fetal pulse is 110/min. Her uterus is tender and firm. The remainder of her physical exam is unremarkable. What is the most likely diagnosis?
- A. Placental abruption (Correct Answer)
- B. Eclampsia
- C. Vasa previa
- D. Preterm labor
- E. Preeclampsia
Premature rupture of membranes Explanation: ***Placental abruption***
- The patient's presentation with **painful vaginal bleeding** after blunt abdominal trauma (motor vehicle accident), a **tender and firm uterus**, maternal **hypotension** and **tachycardia**, and fetal **bradycardia** is highly characteristic of placental abruption.
- Risk factors like **smoking** and trauma further increase the likelihood of placental abruption.
*Eclampsia*
- Eclampsia is characterized by **new-onset grand mal seizures** in a pregnant woman with preeclampsia, which is not present in this scenario.
- While the patient's low blood pressure and tachycardia are concerning, they do not point to eclampsia.
*Vasa previa*
- Vasa previa involves **fetal blood vessels** running within the fetal membranes over the internal cervical os, risking rupture during labor or membrane rupture, leading to **painless vaginal bleeding** and **fetal distress**.
- The bleeding in this case is described as painful, and the uterine tenderness and firmness are not typical of vasa previa.
*Preterm labor*
- Preterm labor is defined by **regular uterine contractions** causing cervical changes before 37 weeks of gestation, which is not aligned with the patient being 39 weeks pregnant or her symptoms.
- While trauma can initiate labor, the severity of the bleeding and maternal/fetal distress point away from isolated preterm labor.
*Preeclampsia*
- Preeclampsia is characterized by **new-onset hypertension** (blood pressure ≥140/90 mmHg) and **proteinuria** after 20 weeks of gestation.
- This patient presents with hypotension and no mention of hypertension or proteinuria, making preeclampsia unlikely.
Premature rupture of membranes US Medical PG Question 2: A 27-year-old woman, gravida 2, para 1, at 37 weeks' gestation is admitted to the hospital in active labor. She has received routine prenatal care, but she has not been tested for group B streptococcal (GBS) colonization. Pregnancy and delivery of her first child were complicated by an infection with GBS that resulted in sepsis in the newborn. Current medications include folic acid and a multivitamin. Vital signs are within normal limits. The abdomen is nontender and contractions are felt every 4 minutes. There is clear amniotic fluid pooling in the vagina. The fetus is in a cephalic presentation. The fetal heart rate is 140/min. Which of the following is the most appropriate next step in management?
- A. Obtain vaginal-rectal swab for nucleic acid amplification testing
- B. Obtain vaginal-rectal swab for GBS culture
- C. Administer intrapartum intravenous penicillin (Correct Answer)
- D. Reassurance
- E. Obtain vaginal-rectal swab for GBS culture and nucleic acid amplification testing
Premature rupture of membranes Explanation: ***Administer intrapartum intravenous penicillin***
- This patient has a **previous infant with invasive GBS disease**, which is a strong indication for **intrapartum antibiotic prophylaxis (IAP)** regardless of current GBS colonization status.
- Penicillin is the **first-line agent** for GBS prophylaxis during labor to prevent vertical transmission to the newborn.
*Obtain vaginal-rectal swab for nucleic acid amplification testing*
- While **NAAT** can provide rapid results, the presence of a prior infant with invasive GBS disease is an **absolute indication** for IAP, making testing unnecessary.
- Waiting for NAAT results would **delay necessary antibiotic administration**, increasing the risk of GBS transmission.
*Obtain vaginal-rectal swab for GBS culture*
- A **GBS culture** typically takes 24-48 hours for results, which is too long given the patient is in active labor and requires immediate management.
- As with NAAT, a prior affected infant means that **IAP is indicated regardless of current culture results**.
*Reassurance*
- Reassurance alone is **insufficient** given the patient's history of a previous infant with GBS sepsis, which places her current fetus at high risk.
- **Active intervention** with antibiotics is crucial to prevent recurrence of GBS disease in the newborn.
*Obtain vaginal-rectal swab for GBS culture and nucleic acid amplification testing*
- Performing both tests is **unnecessary and delays treatment** in a patient with a clear indication for intrapartum antibiotics.
- The patient's history of a prior infant with GBS sepsis is classified as a **high-risk factor, necessitating immediate antibiotic prophylaxis** without waiting for test results.
Premature rupture of membranes US Medical PG Question 3: A 30-year-old woman, gravida 2, para 1, at 31 weeks' gestation is admitted to the hospital because her water broke one hour ago. Pregnancy has been complicated by iron deficiency anemia and hypothyroidism treated with iron supplements and L-thyroxine, respectively. The patient followed-up with her gynecologist on a regular basis throughout the pregnancy. Pregnancy and delivery of her first child were uncomplicated. Pulse is 90/min, respirations are 17/min, and blood pressure is 130/80 mm Hg. The abdomen is nontender. She has had 8 contractions within the last hour. Pelvic examination shows cervical dilation of 3 cm. The fetal heart rate is 140/min with no decelerations. In addition to administration of dexamethasone and terbutaline, which of the following is the most appropriate next step in the management of this patient?
- A. Administer prophylactic azithromycin
- B. Emergency cesarean delivery
- C. Administration of anti-RhD immunoglobulin
- D. Cervical cerclage
- E. Administration of magnesium sulfate (Correct Answer)
Premature rupture of membranes Explanation: ***Administration of magnesium sulfate***
- This patient is experiencing **preterm premature rupture of membranes (PPROM)** at 31 weeks and is in **preterm labor** (contractions with cervical changes).
- **Magnesium sulfate** is administered for **fetal neuroprotection** in cases of anticipated preterm birth before 32 weeks' gestation, reducing the risk of cerebral palsy.
*Administer prophylactic azithromycin*
- **Prophylactic antibiotics** are indicated in PPROM to prolong latency and prevent infection, but **broad-spectrum antibiotics** (e.g., ampicillin and erythromycin) are typically used, not solely azithromycin.
- While azithromycin might be part of an antibiotic regimen for PPROM, it is not the *most appropriate next single step* given the immediate need for neuroprotection and labor inhibition.
*Emergency cesarean delivery*
- An emergency cesarean delivery is not indicated at this time as the **fetal heart rate is reassuring** (140/min with no decelerations) and there are no signs of fetal distress or maternal compromise.
- The primary goal is to **delay delivery** to allow for fetal lung maturity and neuroprotection, rather than immediate delivery.
*Administration of anti-RhD immunoglobulin*
- **Anti-RhD immunoglobulin** is administered to Rh-negative mothers to prevent alloimmunization, typically at 28 weeks' gestation and postpartum.
- While administration may be due at this stage for an Rh-negative patient, it is not the **most critical next step** in the *acute management* of preterm labor and PPROM.
*Cervical cerclage*
- **Cervical cerclage** is a procedure to reinforce the cervix and is performed to prevent preterm birth in patients with **cervical insufficiency**, usually in the late first or early second trimester.
- It is **contraindicated** once membranes have ruptured and the patient is in active labor due to the risk of infection and uterine rupture.
Premature rupture of membranes US Medical PG Question 4: A 28-year-old primigravid woman at 36 weeks' gestation comes to the emergency department because of worsening pelvic pain for 2 hours. Three days ago, she had a burning sensation with urination that resolved spontaneously. She has nausea and has vomited fluid twice on her way to the hospital. She appears ill. Her temperature is 39.7°C (103.5°F), pulse is 125/min, respirations are 33/min, and blood pressure is 130/70 mm Hg. Abdominal examination shows diffuse tenderness. No contractions are felt. Speculum examination shows pooling of nonbloody, malodorous fluid in the vaginal vault. The cervix is not effaced or dilated. Laboratory studies show a hemoglobin concentration of 14 g/dL, a leukocyte count of 16,000/mm3, and a platelet count of 250,000/mm3. Fetal heart rate is 148/min and reactive with no decelerations. Which of the following is the most appropriate next step in management?
- A. Administer oral azithromycin and induce labor
- B. Administer intravenous ampicillin and gentamicin and perform C-section
- C. Administer intravenous ampicillin and gentamicin and induce labor (Correct Answer)
- D. Perform C-section
- E. Expectant management
Premature rupture of membranes Explanation: ***Administer intravenous ampicillin and gentamicin and induce labor***
- This patient presents with signs of **chorioamnionitis** (fever, maternal tachycardia, uterine tenderness, malodorous amniotic fluid with ruptured membranes), necessitating immediate broad-spectrum antibiotics and delivery.
- **Induction of labor** is generally preferred over C-section for chorioamnionitis unless there are other obstetric indications for C-section, to minimize maternal morbidity and reduce overall fetal exposure to infection.
*Administer oral azithromycin and induce labor*
- **Oral azithromycin** is not appropriate for the acute management of chorioamnionitis, which requires broad-spectrum intravenous antibiotics due to the potential for severe maternal and fetal infection.
- While **induction of labor** is correct, the choice of antibiotic is inadequate for this severe infection
*Administer intravenous ampicillin and gentamicin and perform C-section*
- While **intravenous ampicillin and gentamicin** are appropriate antibiotics for chorioamnionitis, a **C-section** is not the standard primary management unless there's a specific obstetric indication (e.g., failed induction, fetal distress).
- Vaginal delivery is generally safer for the mother in cases of chorioamnionitis, as C-section increases the risk of **postpartum endometritis** and wound infection.
*Perform C-section*
- **C-section** alone without immediate antibiotic treatment would be inappropriate and dangerous given the active infection.
- A C-section is also not the first-line delivery method for chorioamnionitis unless other complications necessitate it.
*Expectant management*
- **Expectant management** is contraindicated in chorioamnionitis due to the high risk of severe maternal and neonatal morbidity and mortality, including **sepsis**.
- Immediate intervention with antibiotics and delivery is crucial to prevent further progression of the infection.
Premature rupture of membranes US Medical PG Question 5: A 34-year-old gravida 2 para 1 woman at 16 weeks gestation presents for prenatal care. Her prenatal course has been uncomplicated. She takes no medications besides her prenatal vitamin which she takes every day, and she has been compliant with routine prenatal care. She has a 7-year-old daughter who is healthy. The results of her recent quadruple screen are listed below:
AFP: Low
hCG: Low
Estriol: Low
Inhibin-A: Normal
Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Chorionic villus sampling
- B. Amniocentesis (Correct Answer)
- C. Ultrasound for nuchal translucency
- D. Folic acid supplementation
- E. Return to clinic in 4 weeks
Premature rupture of membranes Explanation: ***Amniocentesis***
- The presented quad screen results (low AFP, low hCG, low estriol, normal Inhibin-A) are highly suggestive of **trisomy 18 (Edwards syndrome)**. Amniocentesis is a **definitive diagnostic test** that can confirm aneuploidy by providing a fetal karyotype.
- While typically performed between **15 and 20 weeks gestation**, it can differentiate between trisomy 18 and trisomy 21 (Down syndrome), which usually presents with high hCG and high Inhibin-A.
*Chorionic villus sampling (CVS)*
- **CVS** is typically performed earlier in pregnancy, between **10 and 13 weeks gestation**, meaning it is too late to perform at 16 weeks gestation.
- While it can provide a fetal karyotype for genetic diagnosis, the gestational age presented in the vignette makes this option currently inappropriate.
*Ultrasound for nuchal translucency*
- **Nuchal translucency (NT)** is part of the first-trimester screening, usually measured between **11 and 14 weeks gestation**.
- At 16 weeks gestation, measuring NT would be **outside the appropriate timeframe**, and the second-trimester quad screen has already been completed, making further screening rather than diagnosis less useful.
*Folic acid supplementation*
- **Folic acid supplementation** is crucial before and during early pregnancy to prevent neural tube defects, which would be associated with high AFP.
- The patient is already taking prenatal vitamins (which contain folic acid), and her quad screen results are not indicative of a neural tube defect but rather a chromosomal abnormality.
*Return to clinic in 4 weeks*
- The abnormal quad screen results indicate a **high risk for aneuploidy**, specifically trisomy 18, which requires immediate follow-up and definitive diagnosis.
- Delaying further assessment for 4 weeks would be clinically inappropriate and could increase patient anxiety and potentially reduce options for further management.
Premature rupture of membranes US Medical PG Question 6: A 32-year-old G2P1 female at 30 weeks gestation presents to the emergency department with complaints of vaginal bleeding and severe abdominal pain. She states that she began feeling poorly yesterday with a stomach-ache, nausea, and vomiting. She first noted a small amount of spotting this morning that progressed to much larger amounts of vaginal bleeding with worsened abdominal pain a few hours later, prompting her to come to the emergency department. Her previous pregnancy was without complications, and the fetus was delivered at 40 weeks by Cesarean section. Fetal heart monitoring shows fetal distress with late decelerations. Which of the following is a risk factor for this patient's presenting condition?
- A. Singleton pregnancy
- B. Hyperlipidemia
- C. Patient age
- D. Hypertension (Correct Answer)
- E. Prior Cesarean section
Premature rupture of membranes Explanation: ***Hypertension***
- The presenting symptoms of **vaginal bleeding**, **severe abdominal pain**, and **fetal distress** in a pregnant woman are highly suggestive of **placental abruption**.
- **Chronic hypertension** is a well-established and significant risk factor for placental abruption, increasing the risk by two to three times.
*Singleton pregnancy*
- This is typical for most pregnancies and does not increase the risk of placental abruption.
- **Multiple gestations** (twins, triplets) are actually associated with an increased risk of placental abruption, not singleton pregnancies.
*Hyperlipidemia*
- **Hyperlipidemia** is generally not considered a direct risk factor for placental abruption.
- While it can be associated with other cardiovascular issues, its link to placental abruption is not significant in the way hypertension is.
*Patient age*
- At 32 years old, the patient is not at an extremely advanced maternal age, which typically refers to 35 years or older.
- While **advanced maternal age** can be a slight risk factor for some pregnancy complications, it is not as strong a risk factor for placental abruption as hypertension in this context.
*Prior Cesarean section*
- A **prior Cesarean section** is a risk factor for conditions like **placenta previa** and **placenta accreta**, where the placenta implants abnormally.
- It is not a primary risk factor for **placental abruption**, which involves premature separation of a normally implanted placenta.
Premature rupture of membranes US Medical PG Question 7: A 26-year-old gravida 1 at 36 weeks gestation is brought to the emergency department by her husband complaining of contractions lasting up to 2 minutes. The contractions are mostly in the front of her abdomen and do not radiate. The frequency and intensity of contractions have not changed since the onset. The patient worries that she is in labor. The blood pressure is 125/80 mm Hg, the heart rate is 96/min, the respiratory rate is 15/min, and the temperature 36.8°C (98.2℉). The physical examination is unremarkable. The estimated fetal weight is 3200 g (6.6 lb). The fetal heart rate is 146/min. The cervix is not dilated. The vertex is at the -4 station. Which of the following would be proper short-term management of this woman?
- A. Reassurance, hydration, and ambulation (Correct Answer)
- B. Admit to the Obstetrics Department for observation
- C. Manage with terbutaline
- D. Admit to the Obstetrics Department in preparation for labor induction
- E. Perform an ultrasound examination
Premature rupture of membranes Explanation: ***Reassurance, hydration, and ambulation***
- This patient is experiencing **Braxton-Hicks contractions**, which are irregular, do not cause cervical change, and often resolve with hydration and rest or light activity.
- Given her stable vital signs, normal fetal heart rate, and undilated cervix, these interventions are appropriate to differentiate from true labor and provide comfort.
*Admit to the Obstetrics Department for observation*
- Admission for observation is unnecessary as there are no signs of **true labor** (cervical dilation or effacement) or fetal distress.
- The contractions are described as not changing in frequency or intensity and are localized to the anterior abdomen, consistent with **false labor**.
*Manage with terbutaline*
- **Terbutaline** is a tocolytic used to stop or prevent premature labor, but this patient is at 36 weeks gestation, which is near term, and not in true labor.
- Using a tocolytic for **Braxton-Hicks contractions** is not indicated and can have adverse effects.
*Admit to the Obstetrics Department in preparation for labor induction*
- There is no indication for **labor induction** as the patient is not in active labor and has not reached her due date.
- Labor induction is reserved for medical or obstetric indications, which are not present here.
*Perform an ultrasound examination*
- An ultrasound has already provided an estimated fetal weight and the fetal heart rate is normal, suggesting no immediate need for further **ultrasound evaluation**.
- There are no clinical signs to suggest fetal distress or other complications that would warrant an **urgent ultrasound**.
Premature rupture of membranes US Medical PG Question 8: A 30-year-old woman, gravida 4, para 3, at 39 weeks' gestation comes to the hospital 20 minutes after the onset of vaginal bleeding. She has not received prenatal care. Her third child was delivered by lower segment transverse cesarean section because of a footling breech presentation. Her other two children were delivered vaginally. Her temperature is 37.1°C (98.8°F), pulse is 86/min, respirations are 18/min, and blood pressure is 132/74 mm Hg. The abdomen is nontender, and no contractions are felt. The fetus is in a vertex presentation. The fetal heart rate is 96/min. Per speculum examination reveals ruptured membranes and severe bleeding from the external os. Which of the following is the most likely diagnosis?
- A. Placenta accreta
- B. Threatened abortion
- C. Bloody show
- D. Placenta previa
- E. Ruptured vasa previa (Correct Answer)
Premature rupture of membranes Explanation: ***Ruptured vasa previa***
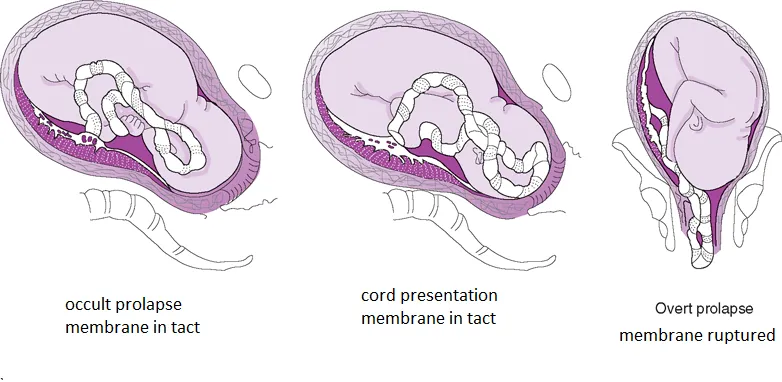
- The sudden onset of painless **vaginal bleeding** at 39 weeks with **fetal heart rate deceleration** (96/min) immediately after membrane rupture is highly indicative of vasa previa rupture.
- In vasa previa, fetal blood vessels lie within the membranes over the cervical os; rupture leads to rapid fetal blood loss.
*Placenta accreta*
- This condition involves abnormal adherence of the **placenta to the uterine wall** and usually presents with hemorrhage during the **third stage of labor** when the placenta fails to separate.
- While a previous cesarean section is a risk factor, the acute scenario with fetal distress following membrane rupture is less typical for placenta accreta as the primary cause of this specific bleeding episode.
*Threatened abortion*
- A threatened abortion occurs **before 20 weeks' gestation** and is characterized by vaginal bleeding with a closed cervix, and would not occur at 39 weeks' gestation.
- The symptoms presented by the patient, including being at term and having severe hemorrhage with fetal heart rate deceleration, are inconsistent with a threatened abortion.
*Bloody show*
- **Bloody show** is typically a small amount of blood-tinged mucus that occurs as the cervix begins to dilate and efface.
- It is not associated with severe, acute hemorrhage or immediate fetal distress, as seen in this case.
*Placenta previa*
- **Placenta previa** typically presents as painless vaginal bleeding in the late second or third trimester but usually does not cause acute, severe fetal heart rate deceleration unless there is significant maternal hypovolemia or placental abruption secondary to the previa.
- The sudden severe bleeding with a rapid drop in fetal heart rate after membrane rupture strongly points away from uncomplicated placenta previa and rather towards fetal vessel rupture.
Premature rupture of membranes US Medical PG Question 9: A 32-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the emergency department because of vaginal bleeding for the past hour. The patient reports that she felt contractions prior to the onset of the bleeding, but the contractions stopped after the bleeding started. She also has severe abdominal pain. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 110/min, respirations are 17/min, and blood pressure is 90/60 mm Hg. Examination shows diffuse abdominal tenderness with no rebound or guarding; no contractions are felt. The fetal heart rate shows recurrent variable decelerations. Which of the following is the most likely diagnosis?
- A. Uterine inertia
- B. Amniotic fluid embolism
- C. Uterine rupture (Correct Answer)
- D. Vasa previa
- E. Abruptio placentae
Premature rupture of membranes Explanation: ***Uterine rupture***
- The patient's history of a prior **cesarean section**, sudden onset of **vaginal bleeding** and **severe abdominal pain**, resolution of contractions, and signs of **hypovolemic shock** (tachycardia, hypotension) coupled with fetal distress (variable decelerations) are highly indicative of uterine rupture.
- Diffuse abdominal tenderness without rebound or guarding, and no palpable contractions, are also consistent with rupture.
*Uterine inertia*
- This condition is characterized by **weak or uncoordinated uterine contractions** leading to prolonged labor, but it does not typically present with acute vaginal bleeding, sudden severe abdominal pain, or hypovolemic shock.
- Fetal distress in uterine inertia would more likely be due to prolonged labor rather than acute compromise following a sudden event.
*Amniotic fluid embolism*
- This is a rare, life-threatening obstetric emergency characterized by sudden **cardiovascular collapse, respiratory distress**, and **coagulopathy**, often occurring during labor or immediately postpartum.
- While it can cause fetal distress, vaginal bleeding and severe abdominal pain are not primary presenting symptoms.
*Vasa previa*
- Characterized by **painless vaginal bleeding** when fetal vessels within the membranes cross the internal cervical os, making them vulnerable to rupture during cervical dilation or amniotomy.
- The bleeding is typically fetal blood, and fetal distress occurs rapidly, but the mother would not experience severe abdominal pain or signs of hypovolemic shock unless the bleeding is substantial and prolonged.
*Abruptio placentae*
- This involves the **premature separation of the placenta**, causing painful vaginal bleeding, uterine tenderness, and frequent, strong contractions.
- While it can cause hypovolemic shock and fetal distress, the description of contractions stopping after bleeding started, along with a previous C-section scar, points more specifically to uterine rupture rather than an abruption.
Premature rupture of membranes US Medical PG Question 10: A 29-year-old G2P1 at 35 weeks gestation presents to the obstetric emergency room with vaginal bleeding and severe lower back pain. She reports the acute onset of these symptoms 1 hour ago while she was outside playing with her 4-year-old son. Her prior birthing history is notable for an emergency cesarean section during her first pregnancy. She received appropriate prenatal care during both pregnancies. She has a history of myomectomy for uterine fibroids. Her past medical history is notable for diabetes mellitus. She takes metformin. Her temperature is 99.0°F (37.2°C), blood pressure is 104/68 mmHg, pulse is 120/min, and respirations are 20/min. On physical examination, the patient is in moderate distress. Large blood clots are removed from the vaginal vault. Contractions are occurring every 2 minutes. Delayed decelerations are noted on fetal heart monitoring. Which of the following is the most likely cause of this patient's symptoms?
- A. Premature separation of a normally implanted placenta (Correct Answer)
- B. Amniotic sac rupture prior to the start of uterine contractions
- C. Placental implantation over internal cervical os
- D. Chorionic villi attaching to the myometrium
- E. Chorionic villi attaching to the decidua basalis
Premature rupture of membranes Explanation: ***Premature separation of a normally implanted placenta***
- The acute onset of **vaginal bleeding**, **severe lower back pain**, frequent uterine contractions, and **fetal decelerations** in a patient with risk factors like a prior cesarean section and diabetes mellitus are highly suggestive of **abruptio placentae**.
- **Uterine tenderness** and a **firm, rigid uterus** (though not explicitly stated, implied by contractions and pain) are also characteristic findings.
*Amniotic sac rupture prior to the start of uterine contractions*
- This condition presents with a gush of fluid from the vagina, often without significant bleeding or severe pain unless associated with other complications.
- While it can lead to preterm labor, it doesn't directly cause the severe back pain, heavy bleeding with clots, and fetal distress seen here.
*Placental implantation over internal cervical os*
- This describes **placenta previa**, which typically presents with **painless vaginal bleeding**, often bright red, without severe abdominal or back pain.
- The presence of severe abdominal pain and uterine contractions makes placenta previa less likely.
*Chorionic villi attaching to the myometrium*
- This describes **placenta accreta**, a condition where the placenta abnormally adheres to the myometrium. It is typically diagnosed postnatally with **difficulty in placental separation** and severe hemorrhage.
- While a prior C-section is a risk factor, the acute presentation of pain and bleeding in the antepartum period is not the classic presentation of accreta alone.
*Chorionic villi attaching to the decidua basalis*
- This describes the **normal implantation** of the placenta into the decidua basalis of the uterus.
- This is the physiological process of pregnancy and would not cause the symptoms of vaginal bleeding, severe pain, and fetal distress described.
More Premature rupture of membranes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.