Placental abruption US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Placental abruption. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Placental abruption US Medical PG Question 1: A 26-year-old Caucasian G1 presents at 35 weeks gestation with mild vaginal bleeding. She reports no abdominal pain or uterine contractions. She received no prenatal care after 20 weeks gestation because she was traveling. Prior to the current pregnancy, she used oral contraception. At 22 years of age she underwent a cervical polypectomy. She has a 5 pack-year smoking history. The blood pressure is 115/70 mmHg, the heart rate is 88/min, the respiratory rate is 14/min, and the temperature is 36.7℃ (98℉). Abdominal palpation reveals no uterine tenderness or contractions. The fundus is palpable between the umbilicus and the xiphoid process. An ultrasound exam shows placental extension over the internal cervical os. Which of the following factors present in this patient is the risk factor for her condition?
- A. White race
- B. Smoking (Correct Answer)
- C. History of cervical polyp
- D. Intake of oral contraceptives
- E. Nulliparity
Placental abruption Explanation: **Smoking**
- **Smoking** is a well-established risk factor for **placenta previa**, as it impairs placental development and increases the likelihood of abnormal implantation.
- Nicotine and other toxins in cigarette smoke can cause **vasoconstriction** and **ischemia**, leading to placental abnormalities, including a lower implantation site.
*White race*
- While certain ethnicities may have varying rates of obstetrical complications, **white race** is generally not considered an independent or significant risk factor for placenta previa.
- Risk factors for placenta previa are primarily related to uterine health, placental development, and obstetric history.
*History of cervical polyp*
- A history of **cervical polyps** is not a known or significant risk factor for **placenta previa**.
- Cervical polyps are benign growths of the cervix and do not inherently affect the site of placental implantation.
*Intake of oral contraceptives*
- The use of **oral contraceptives** prior to pregnancy is not a risk factor for **placenta previa**.
- Oral contraceptives primarily affect ovarian function and have no direct impact on the subsequent placental implantation site.
*Nulliparity*
- **Nulliparity** (never having given birth) is actually associated with a *lower* risk of placenta previa compared to multiparity.
- The risk of placenta previa generally **increases with the number of previous pregnancies** and deliveries due to changes in the uterine lining.
Placental abruption US Medical PG Question 2: A 38-year-old woman, gravida 2, para 1, at 35 weeks' gestation comes to the emergency department because of an episode of vaginal bleeding that morning. The bleeding has subsided. She has had no prenatal care. Her previous child was delivered with a caesarean section because of a breech presentation. Her temperature is 37.1°C (98.8°F), pulse is 88/min, respirations are 14/min, and blood pressure is 125/85 mm Hg. The abdomen is nontender and the size of the uterus is consistent with a 35-week gestation. No contractions are felt. The fetal heart rate is 145/min. Her hemoglobin concentration is 12 g/dL, leukocyte count is 13,000/mm3, and platelet count is 350,000/mm3. Transvaginal ultrasound shows that the placenta covers the internal os. Which of the following is the most appropriate next step in management?
- A. Schedule elective cesarean delivery (Correct Answer)
- B. Observation only
- C. Perform bimanual pelvic examination
- D. Perform emergency cesarean delivery
- E. Administer oxytocin to induce labor
Placental abruption Explanation: ***Schedule elective cesarean delivery***
- The ultrasound finding of the **placenta covering the internal os** confirms **placenta previa**. Given the patient is at **35 weeks' gestation** and has experienced **vaginal bleeding**, an elective cesarean delivery is the safest management to avoid further bleeding episodes and ensure maternal and fetal well-being.
- An elective cesarean delivery is typically scheduled between **36 and 37 weeks' gestation** for placenta previa to minimize the risk of spontaneous labor and potentially catastrophic hemorrhage.
*Observation only*
- This is inappropriate given the diagnosis of **placenta previa** and the history of **vaginal bleeding**. Observation alone carries a significant risk of recurrent, potentially severe hemorrhage.
- While the bleeding has subsided, the underlying condition remains and warrants active management to prevent future complications.
*Perform bimanual pelvic examination*
- A **bimanual pelvic examination** is **contraindicated** in cases of suspected or confirmed **placenta previa**.
- Performing such an examination can **disrupt the placenta** and precipitate a massive, life-threatening hemorrhage.
*Perform emergency cesarean delivery*
- An emergency cesarean delivery is indicated if the patient presents with **severe, active bleeding** or signs of **fetal distress**.
- In this case, the bleeding has subsided, the patient is hemodynamically stable, and the fetal heart rate is normal, so an immediate emergency delivery is not warranted.
*Administer oxytocin to induce labor*
- **Induction of labor with oxytocin** is **contraindicated** in **placenta previa**.
- Stimulating contractions would lead to **cervical dilation**, causing further placental separation and severe hemorrhage, putting both mother and fetus at extreme risk.
Placental abruption US Medical PG Question 3: A 35-year-old G3P2 woman currently 39 weeks pregnant presents to the emergency department with painful vaginal bleeding shortly after a motor vehicle accident in which she was a passenger. She had her seat belt on and reports that the airbag deployed immediately upon her car's impact against a tree. She admits that she actively smokes cigarettes. Her prenatal workup is unremarkable. Her previous pregnancies were remarkable for one episode of chorioamnionitis that resolved with antibiotics. Her temperature is 98.6°F (37°C), blood pressure is 90/60 mmHg, pulse is 130/min, and respirations are 20/min. The fetal pulse is 110/min. Her uterus is tender and firm. The remainder of her physical exam is unremarkable. What is the most likely diagnosis?
- A. Placental abruption (Correct Answer)
- B. Eclampsia
- C. Vasa previa
- D. Preterm labor
- E. Preeclampsia
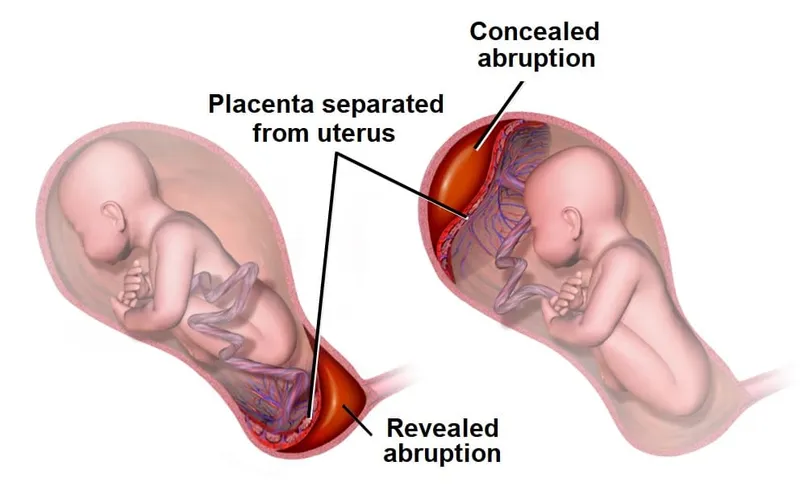
Placental abruption Explanation: ***Placental abruption***
- The patient's presentation with **painful vaginal bleeding** after blunt abdominal trauma (motor vehicle accident), a **tender and firm uterus**, maternal **hypotension** and **tachycardia**, and fetal **bradycardia** is highly characteristic of placental abruption.
- Risk factors like **smoking** and trauma further increase the likelihood of placental abruption.
*Eclampsia*
- Eclampsia is characterized by **new-onset grand mal seizures** in a pregnant woman with preeclampsia, which is not present in this scenario.
- While the patient's low blood pressure and tachycardia are concerning, they do not point to eclampsia.
*Vasa previa*
- Vasa previa involves **fetal blood vessels** running within the fetal membranes over the internal cervical os, risking rupture during labor or membrane rupture, leading to **painless vaginal bleeding** and **fetal distress**.
- The bleeding in this case is described as painful, and the uterine tenderness and firmness are not typical of vasa previa.
*Preterm labor*
- Preterm labor is defined by **regular uterine contractions** causing cervical changes before 37 weeks of gestation, which is not aligned with the patient being 39 weeks pregnant or her symptoms.
- While trauma can initiate labor, the severity of the bleeding and maternal/fetal distress point away from isolated preterm labor.
*Preeclampsia*
- Preeclampsia is characterized by **new-onset hypertension** (blood pressure ≥140/90 mmHg) and **proteinuria** after 20 weeks of gestation.
- This patient presents with hypotension and no mention of hypertension or proteinuria, making preeclampsia unlikely.
Placental abruption US Medical PG Question 4: A clinical diagnosis of abruptio placentae is suspected. Which of the following is the most appropriate next step in the management of this patient?
- A. Vaginal delivery
- B. Administration of intravenous oxytocin
- C. Administration of intramuscular betamethasone
- D. Administration of intravenous fluids (Correct Answer)
- E. Administration of intravenous tranexamic acid
Placental abruption Explanation: ***Administration of intravenous fluids***
- In suspected **abruptio placentae**, significant **blood loss** can occur, leading to maternal **hypotension** and compromise.
- **Intravenous fluids** are crucial for immediate **volume replacement** and maintaining **hemodynamic stability** in both the mother and fetus.
*Vaginal delivery*
- While delivery is often necessary, the **route of delivery** depends on the severity of the abruption, fetal status, and maternal stability; immediate vaginal delivery is not the universal first step before stabilization.
- In cases of severe abruption or fetal distress, an **emergency C-section** might be more appropriate, but **maternal stabilization** with fluids is paramount first.
*Administration of intravenous oxytocin*
- **Oxytocin** is primarily used to **induce labor** or augment contractions, and to prevent or treat **postpartum hemorrhage**.
- It is not indicated as an initial management step for **abruptio placentae**, as it would not address the acute blood loss or fetal compromise.
*Administration of intramuscular betamethasone*
- **Betamethasone** is administered to promote **fetal lung maturity** in cases of preterm delivery.
- While it might be considered if the fetus is preterm and delivery can be delayed for 24-48 hours, **maternal stabilization** and management of acute abruption symptoms take precedence.
*Administration of intravenous tranexamic acid*
- **Tranexamic acid** is an **antifibrinolytic** agent used to reduce bleeding in various settings, including postpartum hemorrhage.
- However, in acute **abruptio placentae**, the immediate concern is **volume resuscitation** rather than directly inhibiting fibrinolysis as the primary first step.
Placental abruption US Medical PG Question 5: A 31-year-old G3P0 is admitted to the hospital with profuse vaginal bleeding and abdominal pain at 34 weeks gestation. She reports passing bright blood with clots and no water in the discharge. She denies recent trauma or medical illnesses. She had no prenatal care. Her previous pregnancies culminated in spontaneous abortions in the second trimester. She has a 6-year history of drug abuse and cocaine smoking 2 hours prior to the onset of her symptoms. Her blood pressure is 160/90 mm Hg, the heart rate is 93/min, the respiratory rate is 19/min, and the temperature is 36.9℃ (98.4℉). The fetal heart rate is 110/min. On examination, the patient is lethargic. Her pupils are constricted, but reactive to light bilaterally. There are no signs of trauma. Abdominal palpation identifies lower abdominal tenderness and strong uterine contractions. The fundus of the uterus is between the xiphoid process and umbilicus. The patient’s perineum is grossly bloody. On pelvic examination, the vaginal canal is without lesions. The cervix is almost completely effaced and 2 cm dilated. Which of the following options is the most likely cause of the patient’s pregnancy-related condition?
- A. Thrombosis of the placental vessels
- B. Dramatic decrease in thrombocytes
- C. Premature rupture of the membranes
- D. Rupture of the placental vessels
- E. Abrupt constriction of maternal and placental vessels (Correct Answer)
Placental abruption Explanation: ***Abrupt constriction of maternal and placental vessels***
- The patient's presentation with **profuse vaginal bleeding**, **abdominal pain**, **strong uterine contractions**, **hypertension**, and a history of **cocaine use** strongly points to **placental abruption**. Cocaine causes abrupt and severe vasoconstriction, leading to placental detachment.
- The **firm and tender uterus**, coupled with **fetal distress** (fetal heart rate of 110/min), is characteristic of placental abruption due to the accumulation of blood behind the placenta and uterine hypertonicity.
*Thrombosis of the placental vessels*
- While thrombosis can affect the placenta, it typically leads to **placental insufficiency** and **fetal growth restriction**, not acute, profuse vaginal bleeding with contractions.
- **Thrombosis** alone does not explain the sudden onset of severe abdominal pain and uterine hypertonicity seen in this case.
*Dramatic decrease in thrombocytes*
- A dramatic decrease in thrombocytes (thrombocytopenia) would cause **generalized bleeding diathesis**, often with petechiae, purpura, or bleeding from other sites, not typically isolated profuse vaginal bleeding with uterine pain and contractions.
- While severe **placental abruption** can lead to **disseminated intravascular coagulation (DIC)** and secondary thrombocytopenia, the primary cause of bleeding here is the placental detachment, not a pre-existing low platelet count.
*Premature rupture of the membranes*
- **Premature rupture of membranes (PROM)** involves the leakage of **amniotic fluid** ("water breaking"), which the patient explicitly denies.
- Although PROM can precede preterm labor, it does not directly cause profuse vaginal bleeding, severe abdominal pain, and uterine hypertonicity in the absence of placental abruption.
*Rupture of the placental vessels*
- **Rupture of placental vessels** without abruption (e.g., vasa previa) typically presents with **painless vaginal bleeding** and rapid **fetal compromise**, but usually without significant maternal abdominal pain or strong uterine contractions.
- The context of **cocaine use** and its known effect on vasoconstriction directly points to placental abruption rather than isolated vessel rupture.
Placental abruption US Medical PG Question 6: A 39-year-old woman, gravida 3, para 2, at 32 weeks' gestation comes to the emergency department 1 hour after the sudden onset of severe abdominal pain and nausea. She has had one episode of nonbloody vomiting. Pregnancy has been uncomplicated, except for a blood pressure measurement of 150/90 mm Hg on her last prenatal visit. Her first child was delivered vaginally; her second child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. She appears anxious and pale. Her temperature is 36.1°C (96°F), pulse is 115/min, and blood pressure is 92/65 mm Hg. Extremities are cool and clammy. Pelvic examination shows a rigid, tender uterus. The cervix is 30% effaced and 1 cm dilated; the vertex is at -1 station. The fetal heart rate is 100/min. Which of the following is the most likely diagnosis?
- A. Ruptured vasa previa
- B. Placenta accreta
- C. Abruptio placentae (Correct Answer)
- D. Ruptured uterus
- E. Placenta previa
Placental abruption Explanation: ***Abruptio placentae***
- The sudden onset of **severe abdominal pain**, **uterine rigidity and tenderness**, maternal hypovolemic shock (tachycardia, hypotension, cool and clammy extremities), and **fetal bradycardia** are classic signs of **abruptio placentae**.
- **Hypertension** (150/90 mm Hg) is a risk factor, and a prior **cesarean section** may slightly increase the risk as well, although the primary risk factor here is hypertension.
*Ruptured vasa previa*
- **Vasa previa** typically presents with **painless vaginal bleeding** when membranes rupture, accompanied by rapid fetal deterioration due to fetal blood loss, and would not cause severe maternal abdominal pain and shock.
- The bleeding in vasa previa originates from fetal vessels, leading to a profound impact on fetal heart rate *before* significant maternal symptoms.
*Placenta accreta*
- **Placenta accreta** is typically diagnosed prenatally via ultrasound or suspected at delivery due to difficulty with placental separation. It does not usually present with acute, severe abdominal pain and hypovolemic shock during pregnancy.
- Patients with placenta accreta are at high risk for significant hemorrhage *after* delivery of the fetus, but before placental delivery.
*Ruptured uterus*
- While a prior **cesarean section** is a risk factor for uterine rupture, the presentation of **rigid and tender uterus** is more characteristic of abruptio placentae. Uterine rupture often involves a **sudden cessation of contractions**, palpable fetal parts outside the uterus, and often severe, sharp pain, but not typically a rigid uterus.
- The fetal heart rate in uterine rupture often shows a **sudden, profound deceleration** or absence, but the specific finding of a rigid, tender uterus with ongoing severe pain points away from frank rupture.
*Placenta previa*
- **Placenta previa** typically presents with **painless vaginal bleeding** in the second or third trimester.
- It does not usually cause severe abdominal pain, uterine tenderness, or maternal hypovolemic shock unless accompanied by abruptio placentae, which is the more dominant and acute finding here.
Placental abruption US Medical PG Question 7: A 28-year-old woman at 30 weeks gestation is rushed to the emergency room with the sudden onset of vaginal bleeding accompanied by intense abdominopelvic pain and uterine contractions. The intensity and frequency of pain have increased in the past 2 hours. This is her 1st pregnancy and she was diagnosed with gestational diabetes several weeks ago. Her vital signs include a blood pressure of 124/68 mm Hg, a pulse of 77/min, a respiratory rate of 22/min, and a temperature of 37.0°C (98.6°F). The abdominal examination is positive for a firm and tender uterus. An immediate cardiotocographic evaluation reveals a fetal heart rate of 150/min with prolonged and repetitive decelerations and high-frequency and low-amplitude uterine contractions. Your attending physician warns you about delaying the vaginal physical examination until a quick sonographic evaluation is completed. Which of the following is the most likely diagnosis in this patient?
- A. Miscarriage
- B. Vasa previa
- C. Placenta abruption (Correct Answer)
- D. Placenta previa
- E. Uterine rupture
Placental abruption Explanation: **Placenta abruption**
- The sudden onset of **vaginal bleeding** with **intense abdominopelvic pain**, **uterine contractions**, and a **firm, tender uterus** strongly suggests **placental abruption**.
- **Fetal decelerations** and the physician's warning against immediate vaginal examination (due to potential for exacerbating hemorrhage if it were placenta previa) further support this diagnosis.
*Miscarriage*
- This patient is at **30 weeks gestation**, whereas a miscarriage is defined as pregnancy loss before **20 weeks of gestation**.
- While bleeding and pain occur, the gestational age rules against a diagnosis of miscarriage.
*Vasa previa*
- **Vasa previa** is characterized by rupture of fetal vessels, leading to **fetal bleeding** and **sudden, painless vaginal bleeding**.
- The patient's presentation includes **intense abdominopelvic pain** and **uterine contractions**, which are not typical of vasa previa.
*Placenta previa*
- **Placenta previa** typically presents with **painless vaginal bleeding** and usually does not involve intense abdominal pain or a **firm, tender uterus**.
- The patient's symptoms of significant pain and uterine contractions are inconsistent with placenta previa.
*Uterine rupture*
- **Uterine rupture** is a catastrophic event, often preceded by a history of **uterine surgery** or trauma, and presents with sudden, severe pain, **fetal distress**, and a **palpable fetal parts** outside the uterus.
- While there is pain and fetal distress, the presence of a **firm, tender uterus** and the absence of a history of uterine surgery make abruption a more likely diagnosis.
Placental abruption US Medical PG Question 8: A 25-year-old G2P1001 at 32 weeks gestation presents to the hospital with painless vaginal bleeding. The patient states that she was taking care of laundry at home when she experienced a sudden sensation of her water breaking and saw that her groin was covered in blood. Her prenatal history is unremarkable according to the clinic records, but she has not seen an obstetrician for the past 14 weeks. Her previous delivery was by urgent cesarean section for placenta previa. Her temperature is 95°F (35°C), blood pressure is 125/75 mmHg, pulse is 79/min, respirations are 18/min, and oxygen saturation is 98% on room air. Cervical exam shows gross blood in the vaginal os. The fetal head is not palpable. Fetal heart rate monitoring demonstrates decelerations and bradycardia. Labs are pending. IV fluids are started. What is the best next step in management?
- A. Cesarean section (Correct Answer)
- B. Betamethasone
- C. Red blood cell transfusion
- D. Vaginal delivery
- E. Lumbar epidural block
Placental abruption Explanation: ***Cesarean section***
- This patient presents with signs highly suggestive of **placenta previa with possible vasa previa or placental abruption**, with life-threatening complications for both mother and fetus. The presence of **painless vaginal bleeding**, a prior **cesarean section for placenta previa**, and **fetal heart rate decelerations/bradycardia** necessitate immediate delivery via cesarean section to prevent **fetal demise** and severe **maternal hemorrhage**.
- The rapid deterioration of the fetal status, indicated by **decelerations and bradycardia**, confirms the urgency. A **cesarean section** is the quickest and safest way to deliver the baby and address the underlying obstetric emergency.
*Betamethasone*
- **Betamethasone** is administered to promote **fetal lung maturity** in cases of preterm delivery. While this patient is preterm at 32 weeks, the critical nature of the fetal distress and bleeding requires immediate delivery, making the delay for betamethasone administration inappropriate.
- The benefits of steroids for lung maturity are outweighed by the **immediate risk of fetal demise** and severe maternal complications if delivery is delayed.
*Red blood cell transfusion*
- While the patient is actively bleeding and may eventually require a **blood transfusion**, starting IV fluids and proceeding with an **immediate cesarean section** are higher priorities to stabilize the mother and rescue the fetus.
- Transfusions are supportive measures once the source of hemorrhage is addressed and vital signs are stabilized during or after surgery.
*Vaginal delivery*
- Given the patient's history of **placenta previa**, current **painless vaginal bleeding**, and signs of **fetal distress**, a vaginal delivery is contraindicated due to the high risk of **exsanguinating hemorrhage** for the mother and severe fetal compromise.
- The prior **cesarean section for placenta previa** also increases the risk of recurrent previa and **placenta accreta spectrum**, further contraindicating vaginal delivery.
*Lumbar epidural block*
- A **lumbar epidural block** is used for pain management during labor, but in this emergent situation with active bleeding and fetal distress, immediate delivery is paramount.
- The time required to safely administer an **epidural**, along with the potential for **hypotension** in a hypovolemic patient, makes it an inappropriate next step.
Placental abruption US Medical PG Question 9: A 32-year-old G2P1 female at 30 weeks gestation presents to the emergency department with complaints of vaginal bleeding and severe abdominal pain. She states that she began feeling poorly yesterday with a stomach-ache, nausea, and vomiting. She first noted a small amount of spotting this morning that progressed to much larger amounts of vaginal bleeding with worsened abdominal pain a few hours later, prompting her to come to the emergency department. Her previous pregnancy was without complications, and the fetus was delivered at 40 weeks by Cesarean section. Fetal heart monitoring shows fetal distress with late decelerations. Which of the following is a risk factor for this patient's presenting condition?
- A. Singleton pregnancy
- B. Hyperlipidemia
- C. Patient age
- D. Hypertension (Correct Answer)
- E. Prior Cesarean section
Placental abruption Explanation: ***Hypertension***
- The presenting symptoms of **vaginal bleeding**, **severe abdominal pain**, and **fetal distress** in a pregnant woman are highly suggestive of **placental abruption**.
- **Chronic hypertension** is a well-established and significant risk factor for placental abruption, increasing the risk by two to three times.
*Singleton pregnancy*
- This is typical for most pregnancies and does not increase the risk of placental abruption.
- **Multiple gestations** (twins, triplets) are actually associated with an increased risk of placental abruption, not singleton pregnancies.
*Hyperlipidemia*
- **Hyperlipidemia** is generally not considered a direct risk factor for placental abruption.
- While it can be associated with other cardiovascular issues, its link to placental abruption is not significant in the way hypertension is.
*Patient age*
- At 32 years old, the patient is not at an extremely advanced maternal age, which typically refers to 35 years or older.
- While **advanced maternal age** can be a slight risk factor for some pregnancy complications, it is not as strong a risk factor for placental abruption as hypertension in this context.
*Prior Cesarean section*
- A **prior Cesarean section** is a risk factor for conditions like **placenta previa** and **placenta accreta**, where the placenta implants abnormally.
- It is not a primary risk factor for **placental abruption**, which involves premature separation of a normally implanted placenta.
Placental abruption US Medical PG Question 10: A 37-year-old woman, gravida 2, para 1, at 35 weeks' gestation is brought to the emergency department for the evaluation of continuous, dark, vaginal bleeding and abdominal pain for one hour. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. The patient has a history of hypertension and has been noncompliant with her hypertensive regimen. Her medications include methyldopa, folic acid, and a multivitamin. Her pulse is 90/min, respirations are 16/min, and blood pressure is 145/90 mm Hg. The abdomen is tender, and hypertonic contractions can be felt. There is blood on the vulva, the introitus, and on the medial aspect of both thighs. The fetus is in a breech presentation. The fetal heart rate is 180/min with recurrent decelerations. Which of the following is the cause of fetal compromise?
- A. Rupture of the uterus
- B. Placental tissue covering the cervical os
- C. Rupture of aberrant fetal vessels
- D. Abnormal position of the fetus
- E. Detachment of the placenta (Correct Answer)
Placental abruption Explanation: ***Detachment of the placenta***
- The presentation of **continuous, dark vaginal bleeding**, **abdominal pain**, and **hypertonic contractions** in a pregnant woman with hypertension strongly indicates **placental abruption**.
- **Fetal compromise**, evidenced by a fetal heart rate of 180/min with recurrent decelerations, results from the compromised oxygen and nutrient exchange due to placental detachment.
*Rupture of the uterus*
- Uterine rupture typically presents with **sudden sharp abdominal pain**, **vaginal bleeding**, and often **cessation of uterine contractions**, which is contradicted by hypertonic contractions.
- A previous C-section scar is a risk factor, but the clinical picture with continuous dark bleeding and hypertonic contractions points more strongly to abruption.
*Placental tissue covering the cervical os*
- This describes **placenta previa**, which typically causes **painless, bright red vaginal bleeding** and usually does not present with abdominal pain or hypertonic contractions.
- The characteristics of pain and dark bleeding make placenta previa less likely.
*Rupture of aberrant fetal vessels*
- This condition, known as **vasa previa**, involves the rupture of fetal blood vessels, leading to **fetal blood loss** and rapid fetal compromise.
- However, the presenting symptoms usually include **sudden onset of bleeding with concurrent fetal bradycardia** or distress, and the vaginal bleeding is typically bright red fetal blood, not dark maternal blood as described.
*Abnormal position of the fetus*
- An abnormal fetal position, such as **breech presentation**, can complicate delivery but does not directly cause dark vaginal bleeding, abdominal pain, or hypertonic uterine contractions.
- While the fetus is breech, this finding does not explain the acute maternal symptoms or the signs of placental compromise.
More Placental abruption US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.