Placenta previa US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Placenta previa. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Placenta previa US Medical PG Question 1: A 26-year-old Caucasian G1 presents at 35 weeks gestation with mild vaginal bleeding. She reports no abdominal pain or uterine contractions. She received no prenatal care after 20 weeks gestation because she was traveling. Prior to the current pregnancy, she used oral contraception. At 22 years of age she underwent a cervical polypectomy. She has a 5 pack-year smoking history. The blood pressure is 115/70 mmHg, the heart rate is 88/min, the respiratory rate is 14/min, and the temperature is 36.7℃ (98℉). Abdominal palpation reveals no uterine tenderness or contractions. The fundus is palpable between the umbilicus and the xiphoid process. An ultrasound exam shows placental extension over the internal cervical os. Which of the following factors present in this patient is the risk factor for her condition?
- A. White race
- B. Smoking (Correct Answer)
- C. History of cervical polyp
- D. Intake of oral contraceptives
- E. Nulliparity
Placenta previa Explanation: **Smoking**
- **Smoking** is a well-established risk factor for **placenta previa**, as it impairs placental development and increases the likelihood of abnormal implantation.
- Nicotine and other toxins in cigarette smoke can cause **vasoconstriction** and **ischemia**, leading to placental abnormalities, including a lower implantation site.
*White race*
- While certain ethnicities may have varying rates of obstetrical complications, **white race** is generally not considered an independent or significant risk factor for placenta previa.
- Risk factors for placenta previa are primarily related to uterine health, placental development, and obstetric history.
*History of cervical polyp*
- A history of **cervical polyps** is not a known or significant risk factor for **placenta previa**.
- Cervical polyps are benign growths of the cervix and do not inherently affect the site of placental implantation.
*Intake of oral contraceptives*
- The use of **oral contraceptives** prior to pregnancy is not a risk factor for **placenta previa**.
- Oral contraceptives primarily affect ovarian function and have no direct impact on the subsequent placental implantation site.
*Nulliparity*
- **Nulliparity** (never having given birth) is actually associated with a *lower* risk of placenta previa compared to multiparity.
- The risk of placenta previa generally **increases with the number of previous pregnancies** and deliveries due to changes in the uterine lining.
Placenta previa US Medical PG Question 2: A 30-year-old woman, gravida 2, para 1, at 12 weeks' gestation comes to the physician for a prenatal visit. She feels well. Pregnancy and vaginal delivery of her first child were uncomplicated. Five years ago, she was diagnosed with hypertension but reports that she has been noncompliant with her hypertension regimen. The patient does not smoke or drink alcohol. She does not use illicit drugs. Medications include methyldopa, folic acid, and a multivitamin. Her temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 145/90 mm Hg. Physical examination shows no abnormalities. Laboratory studies, including serum glucose level, and thyroid-stimulating hormone concentration, are within normal limits. The patient is at increased risk of developing which of the following complications?
- A. Placenta previa
- B. Abruptio placentae (Correct Answer)
- C. Spontaneous abortion
- D. Polyhydramnios
- E. Uterine rupture
Placenta previa Explanation: ***Abruptio placentae***
- The patient's history of **chronic hypertension** (145/90 mmHg) and her noncompliance with antihypertensive medication significantly increase her risk for **abruptio placentae**. Hypertension is a major risk factor for this condition.
- Abruptio placentae involves the **premature separation of the placenta** from the uterine wall, which can lead to severe maternal hemorrhage, fetal distress, and preterm birth.
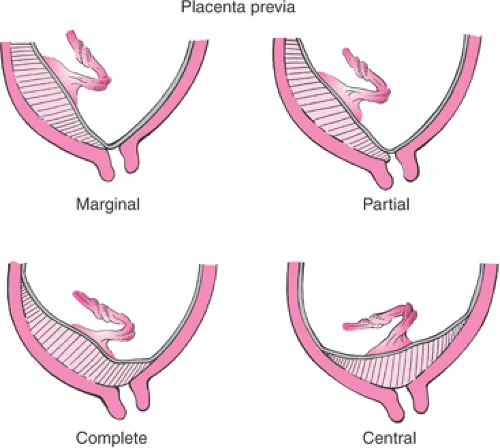
*Placenta previa*
- **Placenta previa** is characterized by the placenta covering the cervical os and is primarily associated with risk factors like **previous C-section**, multiple gestations, or advanced maternal age.
- While a serious complication, it is **not directly linked to chronic hypertension** in the same manner as abruptio placentae.
*Spontaneous abortion*
- **Spontaneous abortion** typically occurs in the **first trimester** and is often due to chromosomal abnormalities, endocrine disorders, or uterine anomalies.
- While hypertension could theoretically contribute to some pregnancy complications, it is **not a primary risk factor** for spontaneous abortion at 12 weeks gestation.
*Polyhydramnios*
- **Polyhydramnios** is an excessive accumulation of amniotic fluid, often associated with **maternal diabetes**, fetal anomalies (e.g., GI obstruction, anencephaly), or multiple gestations.
- Maternal hypertension is **not a direct risk factor** for polyhydramnios.
*Uterine rupture*
- **Uterine rupture** is a rare but catastrophic event, most commonly associated with a **previous uterine scar** (e.g., from a prior C-section or myomectomy).
- The patient's history of a prior vaginal delivery and absence of uterine surgery means she is **not at increased risk** for uterine rupture at this stage.
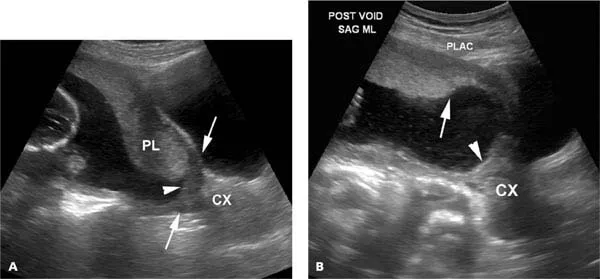
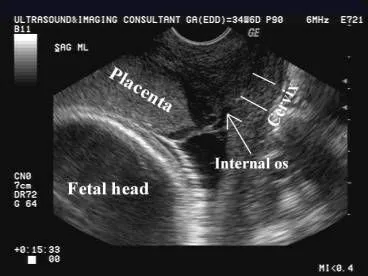
Placenta previa US Medical PG Question 3: A 36-year-old G4P3 is admitted to the obstetrics floor at 35 weeks gestation with painless vaginal spotting for a week. She had 2 cesarean deliveries. An ultrasound examination at 22 weeks gestation showed a partial placenta previa, but she was told not to worry. Today, her vital signs are within normal limits, and a physical examination is unremarkable, except for some blood traces on the perineum. The fetal heart rate is 153/min. The uterine fundus is at the xiphoid process and uterine contractions are absent. Palpation identifies a longitudinal lie. Transvaginal ultrasound shows an anterior placement of the placenta with a placental edge-to-internal os distance of 1.5 cm and a loss of the retroplacental space. Which of the following statements best describes the principle of management for this patient?
- A. Cesarean hysterectomy should be considered for the management of this patient
- B. She can be managed with an unscheduled vaginal delivery with a switch to cesarean delivery if needed
- C. Any decision regarding the mode of delivery in this patient should be taken after an amniocentesis to determine the fetal lung maturity
- D. This patient without a significant prepartum bleeding is unlikely to have an intra- or postpartum bleeding
- E. With such placental position, she should be managed with a scheduled cesarean in the lower uterine segment at 37 weeks’ pregnancy (Correct Answer)
Placenta previa Explanation: ***With such placental position, she should be managed with a scheduled cesarean in the lower uterine segment at 37 weeks’ pregnancy***
- This patient presents with signs highly suggestive of **placenta accreta spectrum (PAS)**, including a history of multiple **cesarean deliveries**, current **partial placenta previa** (placental edge 1.5 cm from internal os), and a **loss of retroplacental space** on ultrasound, all of which increase the risk of massive hemorrhage. A **scheduled cesarean section at 37 weeks** is the standard management for placenta previa and suspected accreta without significant bleeding, as it allows for proper preparation, a multidisciplinary team, and optimized outcomes.
- Delaying delivery until 37 weeks, if the patient remains stable without significant bleeding, helps to ensure **fetal lung maturity** while minimizing maternal risks associated with prolonged pregnancy in the presence of PAS disorders.
*Cesarean hysterectomy should be considered for the management of this patient*
- While **cesarean hysterectomy** might ultimately be necessary in cases of confirmed placenta accreta spectrum with significant invasion, it is typically a **contingency plan** for managing severe hemorrhage or unmanageable placental adherence during a planned cesarean delivery, not the *initial primary management* decision without more extensive bleeding or definitive diagnosis pre-delivery.
- Elective cesarean hysterectomy is associated with **increased morbidity** and is usually reserved for cases where conservative management of the placenta is deemed unsafe or unsuccessful during surgery.
*She can be managed with an unscheduled vaginal delivery with a switch to cesarean delivery if needed*
- The presence of even a **partial placenta previa** and suspected **placenta accreta spectrum** makes vaginal delivery unsafe due to a high risk of **massive hemorrhage** when the cervix dilates or the placenta detaches.
- An unscheduled attempt at vaginal delivery could lead to an **emergency situation**, compromising both maternal and fetal well-being, and is contraindicated with this placental position.
*Any decision regarding the mode of delivery in this patient should be taken after an amniocentesis to determine the fetal lung maturity*
- While fetal lung maturity is a concern for preterm deliveries, the primary concern in this patient is the **maternal risk of hemorrhage** associated with placenta previa and suspected accreta, which dictates the timing and mode of delivery.
- Given the high suspicion for **placenta accreta spectrum**, delaying delivery for amniocentesis adds unnecessary risk without significantly altering the mode of delivery, which will almost certainly be a **cesarean section** regardless of lung maturity results.
*This patient without a significant prepartum bleeding is unlikely to have an intra- or postpartum bleeding*
- This statement is incorrect. The classic presentation of **placenta accreta spectrum** often involves **painless vaginal bleeding** as described, and the absence of *significant* prepartum bleeding does not negate the high risk of **severe intrapartum or postpartum hemorrhage** due to the abnormally adherent placenta.
- The risk of hemorrhage in PAS is primarily associated with the **failure of placental separation** during or after delivery, not necessarily with pre-delivery bleeding patterns.
Placenta previa US Medical PG Question 4: A 24-year-old primigravida presents at 36 weeks gestation with vaginal bleeding, mild abdominal pain, and uterine contractions that appeared after bumping into a handrail. The vital signs are as follows: blood pressure 130/80 mm Hg, heart rate 79/min, respiratory rate 12/min, and temperature 36.5℃ (97.7℉). The fetal heart rate was 145/min. Uterine fundus is at the level of the xiphoid process. Slight uterine tenderness and contractions are noted on palpation. The perineum is bloody. The gynecologic examination shows no vaginal or cervical lesions. The cervix is long and closed. Streaks of bright red blood are passing through the cervix. A transabdominal ultrasound shows the placenta to be attached to the lateral uterine wall with a marginal retroplacental hematoma (an approximate volume of 150 ml). The maternal hematocrit is 36%. What is the next best step in the management of this patient?
- A. Manage as an outpatient with modified rest
- B. Induction of vaginal labor
- C. Corticosteroid administration and schedule a cesarean section after
- D. Admit for maternal and fetal monitoring and observation (Correct Answer)
- E. Urgent cesarean delivery
Placenta previa Explanation: ***Admit for maternal and fetal monitoring and observation***
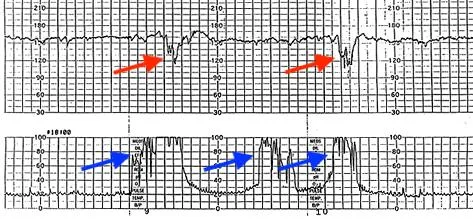
- This patient presents with signs of a **mild placental abruption** (vaginal bleeding, contractions, mild abdominal pain, retroplacental hematoma) after trauma, but her **vital signs are stable**, fetal heart rate is reassuring, and the abruption volume is relatively small.
- Expectant management with **close monitoring** for signs of worsening abruption (increasing pain, vital sign changes, fetal distress) is appropriate for a patient at 36 weeks with a non-catastrophic abruption.
*Manage as an outpatient with modified rest*
- Given the presence of **vaginal bleeding, contractions**, and a **retroplacental hematoma** suggesting placental abruption, outpatient management is not safe.
- There is a risk of the abruption progressing, requiring immediate medical intervention, making **hospital admission for close monitoring** essential.
*Induction of vaginal labor*
- While vaginal delivery might be considered for a stable abruption in some cases, **active induction is not the immediate next step** given the patient's stable status and the need for continuous monitoring.
- The **cervix is long and closed**, indicating that she is not in active labor and immediate induction might not be successful or necessary.
*Corticosteroid administration and schedule a cesarean section after*
- **Corticosteroids** are typically administered for fetal lung maturity when delivery is anticipated before **34 weeks of gestation**; at 36 weeks, this is generally not indicated.
- A scheduled cesarean section is premature as the patient is **stable**, and the immediate goal is to monitor for progression or resolution of the abruption, not immediate delivery.
*Urgent cesarean delivery*
- There are no signs of **maternal or fetal distress** (stable vitals, reassuring fetal heart rate) that would necessitate an urgent cesarean delivery.
- An urgent cesarean is reserved for cases of **severe abruption** with significant bleeding, hemodynamic instability, or fetal compromise.
Placenta previa US Medical PG Question 5: A 28-year-old woman at 30 weeks gestation is rushed to the emergency room with the sudden onset of vaginal bleeding accompanied by intense abdominopelvic pain and uterine contractions. The intensity and frequency of pain have increased in the past 2 hours. This is her 1st pregnancy and she was diagnosed with gestational diabetes several weeks ago. Her vital signs include a blood pressure of 124/68 mm Hg, a pulse of 77/min, a respiratory rate of 22/min, and a temperature of 37.0°C (98.6°F). The abdominal examination is positive for a firm and tender uterus. An immediate cardiotocographic evaluation reveals a fetal heart rate of 150/min with prolonged and repetitive decelerations and high-frequency and low-amplitude uterine contractions. Your attending physician warns you about delaying the vaginal physical examination until a quick sonographic evaluation is completed. Which of the following is the most likely diagnosis in this patient?
- A. Miscarriage
- B. Vasa previa
- C. Placenta abruption (Correct Answer)
- D. Placenta previa
- E. Uterine rupture
Placenta previa Explanation: **Placenta abruption**
- The sudden onset of **vaginal bleeding** with **intense abdominopelvic pain**, **uterine contractions**, and a **firm, tender uterus** strongly suggests **placental abruption**.
- **Fetal decelerations** and the physician's warning against immediate vaginal examination (due to potential for exacerbating hemorrhage if it were placenta previa) further support this diagnosis.
*Miscarriage*
- This patient is at **30 weeks gestation**, whereas a miscarriage is defined as pregnancy loss before **20 weeks of gestation**.
- While bleeding and pain occur, the gestational age rules against a diagnosis of miscarriage.
*Vasa previa*
- **Vasa previa** is characterized by rupture of fetal vessels, leading to **fetal bleeding** and **sudden, painless vaginal bleeding**.
- The patient's presentation includes **intense abdominopelvic pain** and **uterine contractions**, which are not typical of vasa previa.
*Placenta previa*
- **Placenta previa** typically presents with **painless vaginal bleeding** and usually does not involve intense abdominal pain or a **firm, tender uterus**.
- The patient's symptoms of significant pain and uterine contractions are inconsistent with placenta previa.
*Uterine rupture*
- **Uterine rupture** is a catastrophic event, often preceded by a history of **uterine surgery** or trauma, and presents with sudden, severe pain, **fetal distress**, and a **palpable fetal parts** outside the uterus.
- While there is pain and fetal distress, the presence of a **firm, tender uterus** and the absence of a history of uterine surgery make abruption a more likely diagnosis.
Placenta previa US Medical PG Question 6: A 25-year-old G2P1001 at 32 weeks gestation presents to the hospital with painless vaginal bleeding. The patient states that she was taking care of laundry at home when she experienced a sudden sensation of her water breaking and saw that her groin was covered in blood. Her prenatal history is unremarkable according to the clinic records, but she has not seen an obstetrician for the past 14 weeks. Her previous delivery was by urgent cesarean section for placenta previa. Her temperature is 95°F (35°C), blood pressure is 125/75 mmHg, pulse is 79/min, respirations are 18/min, and oxygen saturation is 98% on room air. Cervical exam shows gross blood in the vaginal os. The fetal head is not palpable. Fetal heart rate monitoring demonstrates decelerations and bradycardia. Labs are pending. IV fluids are started. What is the best next step in management?
- A. Cesarean section (Correct Answer)
- B. Betamethasone
- C. Red blood cell transfusion
- D. Vaginal delivery
- E. Lumbar epidural block
Placenta previa Explanation: ***Cesarean section***
- This patient presents with signs highly suggestive of **placenta previa with possible vasa previa or placental abruption**, with life-threatening complications for both mother and fetus. The presence of **painless vaginal bleeding**, a prior **cesarean section for placenta previa**, and **fetal heart rate decelerations/bradycardia** necessitate immediate delivery via cesarean section to prevent **fetal demise** and severe **maternal hemorrhage**.
- The rapid deterioration of the fetal status, indicated by **decelerations and bradycardia**, confirms the urgency. A **cesarean section** is the quickest and safest way to deliver the baby and address the underlying obstetric emergency.
*Betamethasone*
- **Betamethasone** is administered to promote **fetal lung maturity** in cases of preterm delivery. While this patient is preterm at 32 weeks, the critical nature of the fetal distress and bleeding requires immediate delivery, making the delay for betamethasone administration inappropriate.
- The benefits of steroids for lung maturity are outweighed by the **immediate risk of fetal demise** and severe maternal complications if delivery is delayed.
*Red blood cell transfusion*
- While the patient is actively bleeding and may eventually require a **blood transfusion**, starting IV fluids and proceeding with an **immediate cesarean section** are higher priorities to stabilize the mother and rescue the fetus.
- Transfusions are supportive measures once the source of hemorrhage is addressed and vital signs are stabilized during or after surgery.
*Vaginal delivery*
- Given the patient's history of **placenta previa**, current **painless vaginal bleeding**, and signs of **fetal distress**, a vaginal delivery is contraindicated due to the high risk of **exsanguinating hemorrhage** for the mother and severe fetal compromise.
- The prior **cesarean section for placenta previa** also increases the risk of recurrent previa and **placenta accreta spectrum**, further contraindicating vaginal delivery.
*Lumbar epidural block*
- A **lumbar epidural block** is used for pain management during labor, but in this emergent situation with active bleeding and fetal distress, immediate delivery is paramount.
- The time required to safely administer an **epidural**, along with the potential for **hypotension** in a hypovolemic patient, makes it an inappropriate next step.
Placenta previa US Medical PG Question 7: A 36-year-old woman, gravida 4, para 3, at 35 weeks' gestation is brought to the emergency department for the evaluation of a sudden, painless, bright red vaginal bleeding for the last hour. She has had no prenatal care. Her third child was delivered by lower segment transverse cesarean section because of a preterm breech presentation; her first two children were delivered vaginally. The patient's pulse is 100/min, respirations are 15/min, and blood pressure is 105/70 mm Hg. Examination shows a soft, nontender abdomen; no contractions are felt. There is blood on the vulva, the introitus, and on the medial aspect both thighs bilaterally. The fetus is in a cephalic presentation. The fetal heart rate is 140/min. One hour later, the bleeding stops. Which of the following is the most likely diagnosis?
- A. Placenta previa (Correct Answer)
- B. Uterine rupture
- C. Abruptio placentae
- D. Uterine atony
- E. Latent phase of labor
Placenta previa Explanation: **Placenta previa**
- The presentation of **painless, bright red vaginal bleeding** in the third trimester is a hallmark sign of placenta previa.
- A prior **cesarean section** is a significant risk factor for placenta previa due to scarring of the uterine wall.
*Uterine rupture*
- Uterine rupture typically presents with **severe abdominal pain**, maternal **tachycardia**, and fetal **distress** (e.g., decelerations), none of which are noted here.
- The abdomen is described as soft and non-tender, which is inconsistent with uterine rupture.
*Abruptio placentae*
- Abruptio placentae is characterized by **painful vaginal bleeding**, a **tense and tender uterus**, and often fetal distress due to placental detachment.
- The patient's abdomen is soft and non-tender, directly contradictory to the findings in abruptio placentae.
*Uterine atony*
- **Uterine atony** is a cause of **postpartum hemorrhage**, occurring *after* delivery, not during the antenatal period.
- The patient is still pregnant at 35 weeks' gestation, making uterine atony an unlikely diagnosis.
*Latent phase of labor*
- While some bleeding can occur during the latent phase of labor (bloody show), it is usually **minimal** and often mixed with mucus, not the sudden, bright red, profuse bleeding described.
- The absence of regular uterine contractions and a soft, non-tender abdomen further argue against active labor.
Placenta previa US Medical PG Question 8: A 30-year-old woman, gravida 4, para 3, at 39 weeks' gestation comes to the hospital 20 minutes after the onset of vaginal bleeding. She has not received prenatal care. Her third child was delivered by lower segment transverse cesarean section because of a footling breech presentation. Her other two children were delivered vaginally. Her temperature is 37.1°C (98.8°F), pulse is 86/min, respirations are 18/min, and blood pressure is 132/74 mm Hg. The abdomen is nontender, and no contractions are felt. The fetus is in a vertex presentation. The fetal heart rate is 96/min. Per speculum examination reveals ruptured membranes and severe bleeding from the external os. Which of the following is the most likely diagnosis?
- A. Placenta accreta
- B. Threatened abortion
- C. Bloody show
- D. Placenta previa
- E. Ruptured vasa previa (Correct Answer)
Placenta previa Explanation: ***Ruptured vasa previa***
- The sudden onset of painless **vaginal bleeding** at 39 weeks with **fetal heart rate deceleration** (96/min) immediately after membrane rupture is highly indicative of vasa previa rupture.
- In vasa previa, fetal blood vessels lie within the membranes over the cervical os; rupture leads to rapid fetal blood loss.
*Placenta accreta*
- This condition involves abnormal adherence of the **placenta to the uterine wall** and usually presents with hemorrhage during the **third stage of labor** when the placenta fails to separate.
- While a previous cesarean section is a risk factor, the acute scenario with fetal distress following membrane rupture is less typical for placenta accreta as the primary cause of this specific bleeding episode.
*Threatened abortion*
- A threatened abortion occurs **before 20 weeks' gestation** and is characterized by vaginal bleeding with a closed cervix, and would not occur at 39 weeks' gestation.
- The symptoms presented by the patient, including being at term and having severe hemorrhage with fetal heart rate deceleration, are inconsistent with a threatened abortion.
*Bloody show*
- **Bloody show** is typically a small amount of blood-tinged mucus that occurs as the cervix begins to dilate and efface.
- It is not associated with severe, acute hemorrhage or immediate fetal distress, as seen in this case.
*Placenta previa*
- **Placenta previa** typically presents as painless vaginal bleeding in the late second or third trimester but usually does not cause acute, severe fetal heart rate deceleration unless there is significant maternal hypovolemia or placental abruption secondary to the previa.
- The sudden severe bleeding with a rapid drop in fetal heart rate after membrane rupture strongly points away from uncomplicated placenta previa and rather towards fetal vessel rupture.
Placenta previa US Medical PG Question 9: A 29-year-old G1P0 presents to her obstetrician for her first prenatal care visit at 12 weeks gestation by last menstrual period. She states that her breasts are very tender and swollen, and her exercise endurance has declined. She otherwise feels well. She is concerned about preterm birth, as she heard that certain cervical procedures increase the risk. The patient has a gynecologic history of loop electrosurgical excision procedure (LEEP) for cervical dysplasia several years ago and has had negative Pap smears since then. She also has mild intermittent asthma that is well controlled with occasional use of her albuterol inhaler. At this visit, this patient’s temperature is 98.6°F (37.0°C), pulse is 69/min, blood pressure is 119/61 mmHg, and respirations are 13/min. Cardiopulmonary exam is unremarkable, and the uterine fundus is just palpable at the pelvic brim. Pelvic exam reveals normal female external genitalia, a closed and slightly soft cervix, a 12-week-size uterus, and no adnexal masses. Which of the following is the best method for evaluating for possible cervical incompetence in this patient?
- A. Transabdominal ultrasound in the first trimester
- B. Transvaginal ultrasound in the first trimester
- C. Serial transvaginal ultrasounds starting at 16 weeks gestation
- D. Transabdominal ultrasound at 18 weeks gestation
- E. Transvaginal ultrasound at 18 weeks gestation (Correct Answer)
Placenta previa Explanation: ***Transvaginal ultrasound at 18 weeks gestation***
- A history of **LEEP** is a risk factor for **cervical incompetence** and warrants screening with transvaginal ultrasound.
- The optimal timing for **cervical length** screening in women with a history of cervical procedures is typically between **18 and 24 weeks gestation**, as the risk of cervical shortening usually manifests during this period.
*Transabdominal ultrasound in the first trimester*
- **Transabdominal ultrasound** is generally not ideal for precise **cervical length measurement** due to potential shadowing from the fetus or maternal obesity.
- **First-trimester cervical length measurement** is not typically recommended for routine screening of cervical incompetence, as changes are less pronounced early in pregnancy.
*Transvaginal ultrasound in the first trimester*
- While more accurate than transabdominal, **first-trimester transvaginal ultrasound** for cervical length is not standard for predicting cervical incompetence.
- Significant cervical shortening due to incompetence often occurs later in the second trimester, so early screening may miss the condition.
*Serial transvaginal ultrasounds starting at 16 weeks gestation*
- While **serial transvaginal ultrasounds** starting at 16 weeks can be part of a management plan for high-risk patients, the most critical single assessment typically occurs at **18-24 weeks**.
- Starting serial scans too early may not be necessary if the cervix is long and closed at the initial key screening, unless there are other strong indications.
*Transabdominal ultrasound at 18 weeks gestation*
- Similar to first-trimester transabdominal ultrasound, **transabdominal imaging** at 18 weeks is generally **less accurate** than transvaginal for measuring cervical length.
- **Transvaginal ultrasound** offers a clearer and more precise view of the cervix, which is crucial for assessing potential shortening or funneling.
Placenta previa US Medical PG Question 10: A 23-year-old primigravid woman comes to the physician at 36 weeks' gestation for her first prenatal visit. She confirmed the pregnancy with a home urine pregnancy kit a few months ago but has not yet followed up with a physician. She takes no medications. Vital signs are within normal limits. Pelvic examination shows a uterus consistent in size with a 36-week gestation. Laboratory studies show:
Hemoglobin 10.6 g/dL
Serum
Glucose 88 mg/dL
Hepatitis B surface antigen negative
Hepatitis C antibody negative
HIV antibody positive
HIV load 11,000 copies/mL (N < 1000 copies/mL)
Ultrasonography shows an intrauterine fetus consistent in size with a 36-week gestation. Which of the following is the most appropriate next step in management of this patient?
- A. Intrapartum zidovudine and vaginal delivery when labor occurs
- B. Intrapartum zidovudine and cesarean delivery at 38 weeks' gestation
- C. Start cART and prepare for vaginal delivery at 38 weeks' gestation
- D. Conduct cesarean delivery immediately
- E. Start cART and schedule cesarean delivery at 38 weeks' gestation (Correct Answer)
Placenta previa Explanation: ***Start cART and schedule cesarean delivery at 38 weeks' gestation***
- This patient presents at 36 weeks with a **newly diagnosed HIV infection** and a **viral load of 11,000 copies/mL**, which is considered high. Starting **combination antiretroviral therapy (cART)** immediately is crucial to reduce the viral load and the risk of **mother-to-child transmission (MTCT)**.
- For patients with **HIV viral loads > 1,000 copies/mL** near term, a **scheduled cesarean delivery at 38 weeks** is recommended to minimize fetal exposure to maternal blood and secretions during labor, further reducing the risk of MTCT.
*Intrapartum zidovudine and vaginal delivery when labor occurs*
- This approach is appropriate for HIV-positive mothers with a **low viral load (< 1,000 copies/mL)** at or near delivery, as a scheduled cesarean section would not significantly further reduce the risk of transmission.
- Given the patient's **high viral load (11,000 copies/mL)**, **only intrapartum zidovudine** would be insufficient to adequately reduce the risk of MTCT during a vaginal delivery.
*Intrapartum zidovudine and cesarean delivery at 38 weeks' gestation*
- While a **scheduled cesarean delivery at 38 weeks** is indicated for a high viral load, simply administering **intrapartum zidovudine without prior cART** misses the opportunity to significantly reduce viral load before delivery.
- Starting **cART immediately** offers the best chance to lower viral load and optimize outcomes for both mother and child, which is superior to only intrapartum prophylaxis.
*Start cART and prepare for vaginal delivery at 38 weeks' gestation*
- Starting **cART is essential**, but preparing for a vaginal delivery with a **viral load of 11,000 copies/mL** at 36 weeks is inappropriate.
- A **high viral load** necessitates a ** scheduled cesarean delivery** to minimize the risk of MTCT, regardless of cART initiation at this late stage.
*Conduct cesarean delivery immediately*
- While immediate action is needed, an **emergency cesarean delivery** is not indicated at 36 weeks unless there are other obstetric complications or rapid deterioration.
- The primary goal is to **reduce viral load through cART** and then perform a **scheduled cesarean at 38 weeks**, balancing safety for both mother and fetus with the greatest reduction in HIV transmission risk.
More Placenta previa US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.