Labor Complications

On this page
🚨 The Obstetric Emergency Arsenal: When Delivery Goes Critical
Labor complications transform routine deliveries into high-stakes emergencies where your recognition speed and intervention precision directly determine maternal and fetal survival. You'll master the pathophysiology driving obstetric crises, sharpen your clinical radar to catch warning signs before catastrophe strikes, and build a systematic approach to differentiate mimics from true threats. Through evidence-based protocols and multi-system thinking, you'll develop the rapid decision-making framework that defines expert emergency obstetric care when seconds matter most.
📌 Remember: ABCDE of Obstetric Emergencies - Abruption, Breech, Cord prolapse, Dystocia, Embolism - The 5 scenarios that demand immediate recognition and action
Labor complications affect 15-20% of all deliveries, with 5-8% requiring emergency intervention within 30 minutes of recognition. These emergencies cluster into predictable patterns, each with distinct warning signs and management protocols.
- Hemorrhagic Emergencies (40% of complications)
- Placental abruption: 1 in 150 deliveries, 15% mortality risk
- Uterine rupture: 1 in 2,000 deliveries, 6% maternal mortality
- Complete rupture: 90% require hysterectomy
- Incomplete rupture: 60% salvageable with repair
- Mechanical Emergencies (35% of complications)
- Shoulder dystocia: 0.6-1.4% of vaginal deliveries
- Cord prolapse: 0.1-0.6% of deliveries, 91% emergency cesarean rate
- Infectious Emergencies (15% of complications)
- Chorioamnionitis: 1-5% of term deliveries, 13-20% preterm
- Systemic Emergencies (10% of complications)
- Amniotic fluid embolism: 1 in 40,000 deliveries, 60-80% mortality
| Emergency Type | Incidence | Time to Intervention | Maternal Risk | Fetal Risk | Key Diagnostic Sign |
|---|---|---|---|---|---|
| Placental Abruption | 1:150 | <30 minutes | 15% mortality | 25% mortality | Painful bleeding |
| Uterine Rupture | 1:2,000 | <15 minutes | 6% mortality | 35% mortality | Sudden pain cessation |
| Shoulder Dystocia | 1:150 | <5 minutes | <1% morbidity | 10% brachial plexus | Turtle sign |
| Cord Prolapse | 1:500 | <10 minutes | <1% mortality | 15% mortality | Visible/palpable cord |
| Amniotic Embolism | 1:40,000 | <5 minutes | 70% mortality | 85% mortality | Sudden collapse |
💡 Master This: Every labor complication follows the "3-Phase Pattern" - Recognition (clinical signs), Stabilization (immediate interventions), Resolution (definitive management). Master this sequence, and you control any obstetric emergency.
Understanding labor complications requires recognizing that 85% of emergencies present with predictable warning patterns occurring 2-6 hours before crisis. The key lies in pattern recognition rather than waiting for obvious signs.
🚨 The Obstetric Emergency Arsenal: When Delivery Goes Critical
⚡ The Pathophysiology Powerhouse: When Normal Labor Breaks Down
📌 Remember: STOP the Bleeding - Source control, Tone restoration, Oxytocin/uterotonics, Products of conception removal - The 4-step hemorrhage protocol that saves lives in <10 minutes
Hemorrhagic Complications represent 60% of maternal mortality, with 3 primary mechanisms:
- Placental Separation Disorders
- Abruption: Premature separation with retroplacental hematoma
- Previa: Abnormal implantation over cervical os
- Complete previa: 100% cesarean delivery required
- Marginal previa: 70% vaginal delivery possible
- Uterine Integrity Failure
- Rupture: Full-thickness separation of uterine wall
- Atony: Failure of myometrial contraction post-delivery
- Primary atony: 80% respond to first-line uterotonics
- Secondary atony: 40% require surgical intervention
- Coagulation System Breakdown
- DIC: Consumption coagulopathy with fibrinogen <150 mg/dL
- Dilutional coagulopathy: Massive transfusion with >10 units PRBC
| Complication | Pathophysiology | Time Course | Blood Loss | Intervention Window |
|---|---|---|---|---|
| Placental Abruption | Decidual hemorrhage | Minutes to hours | 500-2000 mL | <30 minutes |
| Uterine Rupture | Myometrial separation | Sudden onset | 1000-3000 mL | <15 minutes |
| Uterine Atony | Contraction failure | Post-delivery | 500-1500 mL | <20 minutes |
| Placenta Previa | Cervical dilation | Progressive | 200-1000 mL | <45 minutes |
| DIC | Coagulation consumption | Hours | Variable | <60 minutes |
Mechanical Complications disrupt the cardinal movements of labor through 3 primary mechanisms:
- Fetal Factors (45% of dystocia)
- Macrosomia: >4500g increases dystocia risk 3-fold
- Malpresentation: Breech 3-4%, face 0.2%, brow 0.1%
- Maternal Factors (35% of dystocia)
- Pelvic architecture: Android pelvis increases cesarean risk 2.5-fold
- Soft tissue: Cervical dystocia in 2-5% of nulliparous women
- Power Factors (20% of dystocia)
- Inadequate contractions: <200 Montevideo units
- Precipitous labor: >5 cm/hour cervical dilation
💡 Master This: The "Power-Passenger-Passage" triad governs all mechanical complications. Identify the primary dysfunction, and you predict both the complication pattern and optimal intervention strategy.
Understanding these pathophysiologic foundations enables predictive recognition rather than reactive management, transforming obstetric emergencies from chaotic crises into systematic challenges with clear solutions.
⚡ The Pathophysiology Powerhouse: When Normal Labor Breaks Down
🎯 The Recognition Radar: Spotting Trouble Before Crisis
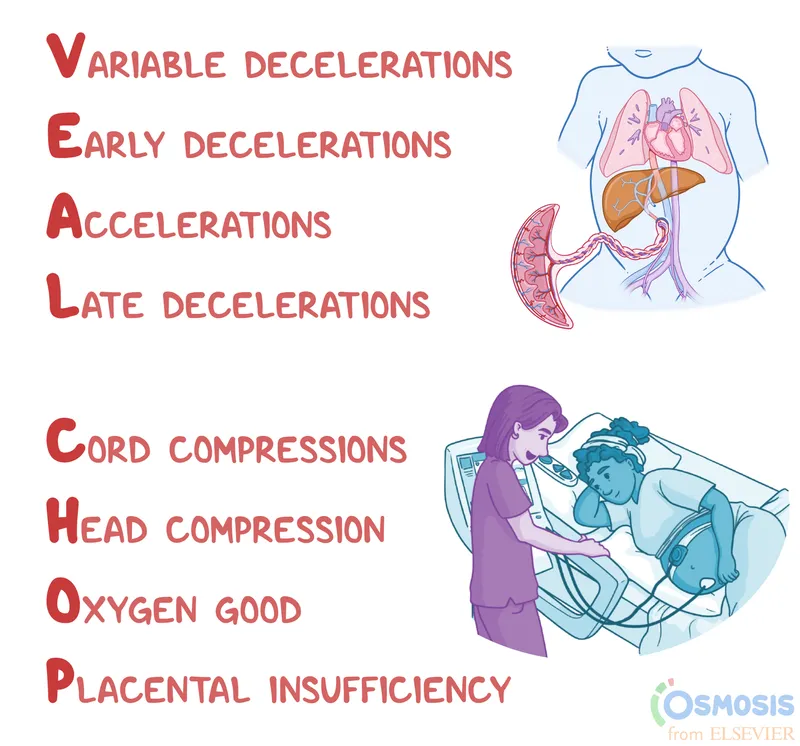
📌 Remember: VEAL CHOP - Variable = Cord compression, Early = Head compression, Acceleration = OK, Late = Placental insufficiency - The FHR pattern decoder that predicts fetal compromise
Early Warning Pattern Recognition follows predictable sequences:
- Hemorrhagic Warning Signs (2-6 hours before crisis)
- Vital sign trends: HR ↑ >20 bpm, SBP ↓ >15 mmHg
- Fetal changes: Late decelerations in >50% of contractions
- Laboratory shifts: Hgb ↓ >2 g/dL, Plt ↓ >50,000
- Abruption pattern: Painful bleeding + rigid uterus
- Previa pattern: Painless bleeding + soft uterus
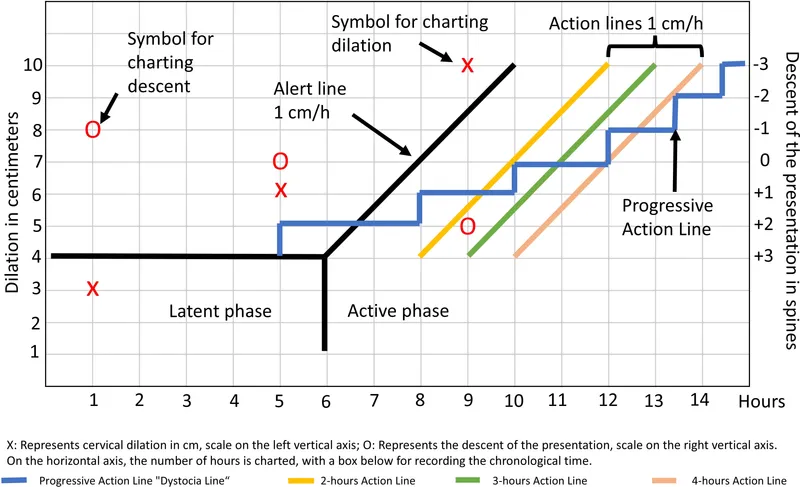
- Mechanical Warning Signs (1-3 hours before dystocia)
- Labor progress: <1 cm/hour cervical change in active phase
- Station arrest: No descent for >2 hours with adequate contractions
- Contraction pattern: <200 Montevideo units despite augmentation
- Shoulder dystocia risk: Fetal weight >4000g + diabetes
- Malpresentation clues: Irregular fetal heart tones + palpable extremities
| Warning Pattern | Sensitivity | Specificity | Positive Predictive Value | Time to Crisis | Intervention Success |
|---|---|---|---|---|---|
| Late FHR decelerations | 85% | 70% | 45% | 2-4 hours | 90% if <2 hours |
| Shock index >0.9 | 75% | 85% | 65% | 1-2 hours | 95% if <1 hour |
| Labor arrest pattern | 80% | 60% | 55% | 2-6 hours | 85% if <4 hours |
| Rigid uterus + pain | 90% | 95% | 85% | 30-60 minutes | 80% if <30 min |
| Turtle sign | 100% | 100% | 100% | <5 minutes | 95% if <2 minutes |
Advanced Pattern Integration combines multiple data streams:
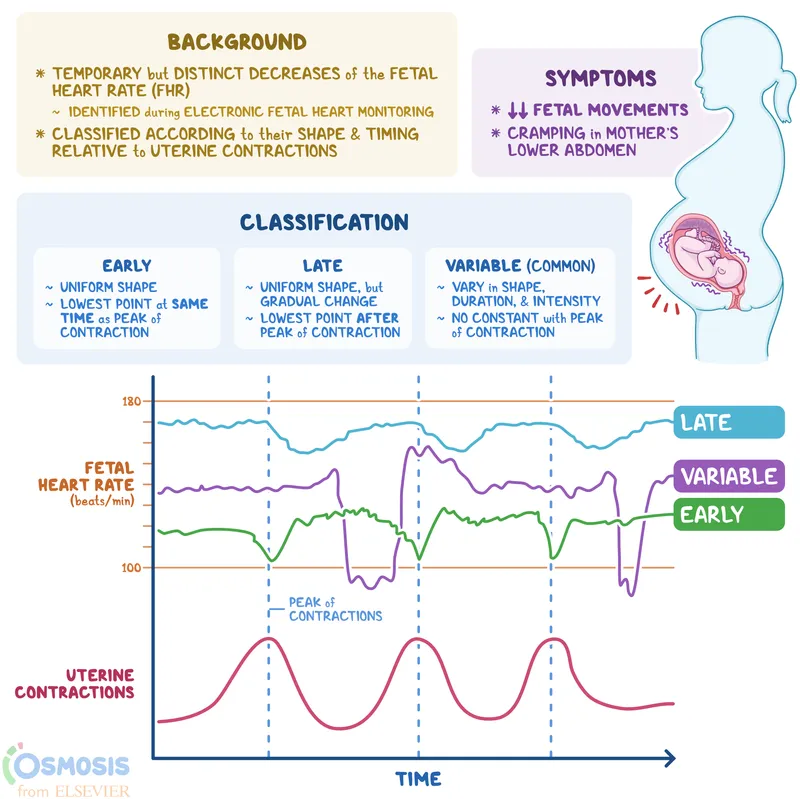
- Fetal Heart Rate Patterns
- Category I: Normal baseline (110-160 bpm), moderate variability (6-25 bpm)
- Category II: Indeterminate - requires continuous monitoring and intervention consideration
- Category III: Abnormal - demands immediate delivery within 30 minutes
- Absent variability + recurrent late decelerations = 95% acidemia risk
- Sinusoidal pattern = 85% severe anemia or hypoxia
- Maternal Monitoring Integration
- Contraction strength: >50 mmHg intensity, >200 MVU adequacy
- Cervical change: >1.2 cm/hour in nulliparous, >1.5 cm/hour multiparous
- Descent pattern: >1 station/hour in second stage
- Arrest of dilation: No change >4 hours with adequate contractions
- Arrest of descent: No progress >3 hours nulliparous, >2 hours multiparous
💡 Master This: "Triple Assessment" - Fetal status (FHR patterns), Maternal status (vital signs/bleeding), Labor progress (cervix/descent). When any 2 of 3 show concerning trends, intervention within 1 hour prevents 90% of emergency complications.
Recognition mastery transforms unpredictable emergencies into manageable clinical scenarios with clear decision points and optimal timing for intervention.
🎯 The Recognition Radar: Spotting Trouble Before Crisis
⚔️ The Differential Decoder: Separating Look-Alikes from Life-Threats
📌 Remember: PAINFUL vs PAINLESS - Abruption = Painful bleeding with rigid uterus, Previa = Painless bleeding with soft uterus - The cardinal distinction that determines immediate management
Hemorrhagic Emergency Differentiation requires systematic comparison:
- Placental Abruption vs Placenta Previa
- Pain pattern: Abruption = severe, constant; Previa = absent
- Uterine tone: Abruption = rigid, tender; Previa = soft, non-tender
- Bleeding onset: Abruption = sudden, severe; Previa = gradual, recurrent
- Abruption: Dark red blood with clots
- Previa: Bright red blood without clots
- Uterine Rupture vs Abruption
- Pain character: Rupture = sudden cessation; Abruption = persistent severe
- Fetal station: Rupture = loss of engagement; Abruption = unchanged
- Maternal shock: Rupture = immediate, profound; Abruption = progressive
| Feature | Abruption | Previa | Uterine Rupture | Vasa Previa | Uterine Atony |
|---|---|---|---|---|---|
| Pain | Severe, constant | Absent | Sudden cessation | Absent | Cramping |
| Bleeding | Dark, clotted | Bright, liquid | Variable | Bright, minimal | Bright, heavy |
| Uterine tone | Rigid, tender | Soft | Loss of contour | Normal | Boggy, soft |
| Fetal status | Distressed (80%) | Normal (60%) | Bradycardia (90%) | Severe distress | Usually normal |
| Shock severity | Moderate-severe | Mild-moderate | Severe, immediate | Mild maternal | Moderate-severe |
Mechanical Emergency Differentiation focuses on anatomical patterns:
- Shoulder Dystocia vs Normal Delivery Pause
- Turtle sign: Dystocia = head retracts; Normal = head remains extended
- Time factor: Dystocia = >60 seconds; Normal = <30 seconds
- Traction response: Dystocia = no descent; Normal = progressive descent
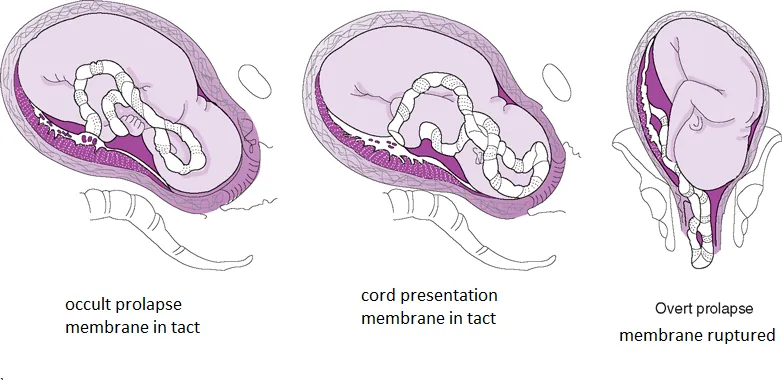
- Cord Prolapse vs Cord Presentation
- Membrane status: Prolapse = ruptured membranes; Presentation = intact membranes
- Pulsation: Prolapse = palpable pulsation; Presentation = may be absent
- Urgency: Prolapse = immediate delivery; Presentation = close monitoring
Infectious vs Non-infectious Fever in labor:
- Chorioamnionitis Criteria (≥2 required)
- Maternal fever: >38°C (100.4°F)
- Maternal tachycardia: >100 bpm
- Fetal tachycardia: >160 bpm
- Uterine tenderness: Fundal or lower segment
- Purulent/foul amniotic fluid: Visual or olfactory
- Epidural-related fever: 38-39°C, no other signs, normal WBC
- Dehydration fever: Low-grade, concentrated urine, responds to hydration
💡 Master This: The "ABCDE Rule" for emergency differentiation - Assess pain pattern, Bleeding characteristics, Contraction quality, Descent progression, Electronic fetal monitoring. Systematic evaluation of all 5 parameters achieves >95% diagnostic accuracy.
Differential mastery eliminates diagnostic uncertainty, enabling confident decision-making even in complex presentations with overlapping symptoms.
⚔️ The Differential Decoder: Separating Look-Alikes from Life-Threats
⚡ The Intervention Engine: Evidence-Based Emergency Protocols
📌 Remember: HELPERR for Shoulder Dystocia - Help (call for assistance), Evaluate for episiotomy, Legs (McRoberts), Pressure (suprapubic), Enter maneuvers (internal), Remove posterior arm, Roll patient - 7-step protocol with 95% success rate
Hemorrhage Management Protocol (4-Tier Approach):
- Tier 1: Immediate Stabilization (0-5 minutes)
- IV access: 2 large-bore IVs (16-18 gauge)
- Fluid resuscitation: Crystalloid 1-2L rapid infusion
- Laboratory: Type/crossmatch 4-6 units, CBC, coagulation studies
- Monitoring: Continuous vital signs, Foley catheter, pulse oximetry
- Tier 2: Source Control (5-15 minutes)
- Uterine massage: Bimanual compression for atony
- Medications: Oxytocin 40 units/L, Methergine 0.2mg IM, Hemabate 250mcg IM
- Examination: Cervical/vaginal lacerations, retained products
- Tier 3: Advanced Interventions (15-30 minutes)
- Balloon tamponade: Bakri balloon with 300-500mL saline
- Compression sutures: B-Lynch or Cho technique
- Arterial ligation: Uterine or hypogastric arteries
- Tier 4: Definitive Surgery (30-45 minutes)
- Hysterectomy: Peripartum with ovarian preservation
- Interventional radiology: Arterial embolization if stable
| Intervention | Success Rate | Time to Effect | Complications | Cost Effectiveness |
|---|---|---|---|---|
| Oxytocin | 85% | 2-5 minutes | Minimal | High |
| Methergine | 75% | 5-10 minutes | Hypertension (15%) | High |
| Hemabate | 80% | 10-15 minutes | Bronchospasm (5%) | Moderate |
| Bakri balloon | 90% | 15-30 minutes | Infection (2%) | High |
| B-Lynch suture | 85% | 30-45 minutes | Uterine necrosis (1%) | Moderate |
| Hysterectomy | 100% | 45-90 minutes | Major surgery risks | Low |
Shoulder Dystocia Management (HELPERR Protocol):
- Help: Call for assistance - anesthesia, pediatrics, additional nursing
- Evaluate: Episiotomy if restrictive perineum (not routine)
- Legs: McRoberts maneuver - hip flexion >90°, success rate 42%
- Pressure: Suprapubic pressure - downward/lateral, avoid fundal pressure
- Enter: Internal maneuvers - Woods screw or Rubin maneuver
- Remove: Posterior arm delivery - flex elbow, sweep across chest
- Roll: All-fours position (Gaskin maneuver) - success rate 83%
Cord Prolapse Management (<10 minutes to delivery):
- Immediate actions (<2 minutes)
- Elevate presenting part - manual displacement of fetal head
- Knee-chest or Trendelenburg position
- Avoid cord manipulation - maintain warmth and moisture
- Delivery preparation (2-10 minutes)
- Emergency cesarean if not fully dilated
- Operative vaginal delivery if fully dilated and low station
- Continuous fetal monitoring until delivery
💡 Master This: "Time-Critical Interventions" follow the "3-30-300 Rule" - 3 minutes for cord prolapse, 30 minutes for abruption, 300 minutes (5 hours) for dystocia. Exceed these timeframes, and morbidity increases exponentially.
Evidence-based protocols eliminate decision paralysis during emergencies, providing clear pathways from recognition to resolution with optimal outcomes.
⚡ The Intervention Engine: Evidence-Based Emergency Protocols
🌐 The Integration Matrix: Multi-System Mastery
📌 Remember: MODS - Maternal Organ Dysfunction Syndrome follows predictable patterns: Cardiovascular → Renal → Hepatic → Pulmonary → Neurologic - The 5-system cascade that determines maternal survival
Hemorrhage-Induced System Integration:
- Cardiovascular Compensation (Stage 1: 15-30% blood loss)
- Heart rate: ↑ 15-20 bpm (normal 60-100 bpm)
- Blood pressure: Maintained through vasoconstriction
- Cardiac output: ↑ 10-15% through increased contractility
- Renal-Endocrine Response (Stage 2: 30-40% blood loss)
- Urine output: ↓ to 0.5-1.0 mL/kg/hr (normal >1.0 mL/kg/hr)
- Antidiuretic hormone: ↑ 5-10 fold baseline levels
- Aldosterone: ↑ 3-5 fold for sodium retention
- Coagulation Activation (Stage 3: >40% blood loss)
- Fibrinogen: ↓ <150 mg/dL (normal 200-400 mg/dL)
- D-dimer: ↑ >4000 ng/mL (normal <500 ng/mL)
- Platelet count: ↓ <100,000 (normal 150,000-400,000)
| System | Early Changes (15-30% loss) | Moderate Changes (30-40% loss) | Severe Changes (>40% loss) | Recovery Time |
|---|---|---|---|---|
| Cardiovascular | HR ↑20%, BP stable | HR ↑40%, SBP ↓15% | HR ↑60%, SBP ↓30% | 24-48 hours |
| Renal | UOP ↓25% | UOP ↓50% | UOP ↓75% | 48-72 hours |
| Hematologic | Hct ↓10% | Hct ↓25% | Hct ↓40% | 4-6 weeks |
| Coagulation | Normal | Fibrinogen ↓25% | DIC pattern | 72-96 hours |
| Neurologic | Anxiety | Confusion | Altered consciousness | Variable |
Infection-Inflammation Integration (Chorioamnionitis cascade):
- Local Inflammatory Response (0-6 hours)
- Cytokine release: IL-1β, TNF-α ↑ 10-50 fold
- Prostaglandin production: PGE2 ↑ 5-10 fold → cervical ripening
- Neutrophil infiltration: WBC ↑ >15,000 with >80% neutrophils
- Systemic Inflammatory Response (6-24 hours)
- Fever: >38.5°C in 90% of cases
- Tachycardia: Maternal >100 bpm, Fetal >160 bpm
- Metabolic acidosis: Base deficit >-5 mEq/L
- Fetal Inflammatory Response (12-48 hours)
- Fetal inflammatory response syndrome: IL-6 >11 pg/mL
- Cerebral palsy risk: ↑ 4-fold with severe chorioamnionitis
- Neonatal sepsis: 15-25% incidence with positive cultures
Mechanical-Vascular Integration (Prolonged labor effects):
- Uterine Overdistention (>12 hours active labor)
- Myometrial blood flow: ↓ 30-50% during strong contractions
- Lactic acid accumulation: ↑ 2-3 fold in uterine muscle
- Atony risk: ↑ 3-fold after prolonged labor
- Fetal Compromise Progression
- Umbilical cord compression: Variable decelerations in 60%
- Placental insufficiency: Late decelerations in 40%
- Metabolic acidosis: pH <7.20 in 25% after >18 hours labor
💡 Master This: "System Integration Monitoring" requires simultaneous assessment of cardiovascular (vital signs), renal (urine output), hematologic (bleeding), neurologic (mental status), and fetal (FHR patterns) parameters. Any 2 systems showing deterioration predicts cascade failure within 2-6 hours.
Multi-system integration transforms single-problem thinking into comprehensive care that prevents cascade complications and optimizes maternal-fetal outcomes.
🌐 The Integration Matrix: Multi-System Mastery
🎯 The Mastery Arsenal: Rapid-Fire Clinical Command
📌 Remember: CRASH Cart Obstetrics - Cord prolapse (<3 min), Rupture (<15 min), Abruption (<30 min), Shoulder dystocia (<5 min), Hemorrhage (<20 min) - Time-critical windows that determine survival outcomes
Essential Clinical Arsenal (Memorize These Numbers):
- Critical Timeframes
- Cord prolapse to delivery: <10 minutes (optimal <5 minutes)
- Uterine rupture recognition to delivery: <15 minutes
- Placental abruption to delivery: <30 minutes
- Shoulder dystocia resolution: <5 minutes (each minute ↑ 16% morbidity)
- Postpartum hemorrhage control: <20 minutes for optimal outcomes
- Vital Thresholds
- Shock index: >1.0 = significant hemorrhage, >1.5 = massive transfusion
- Blood loss: >500 mL vaginal, >1000 mL cesarean = hemorrhage
- Fetal bradycardia: <110 bpm >10 minutes = immediate delivery
- Maternal fever: >38°C + 2 other signs = chorioamnionitis
| Emergency | Recognition Time | Intervention Window | Success Rate | Key Decision Point |
|---|---|---|---|---|
| Cord Prolapse | <2 minutes | <10 minutes | 95% if <5 min | Cervical dilation |
| Shoulder Dystocia | Immediate | <5 minutes | 90% with HELPERR | McRoberts failure |
| Uterine Rupture | <5 minutes | <15 minutes | 85% if <10 min | Pain pattern change |
| Placental Abruption | <10 minutes | <30 minutes | 80% if <20 min | Fetal status |
| Amniotic Embolism | <1 minute | <5 minutes | 30% overall | Cardiac arrest |
Rapid Assessment Protocol (<3 minutes):
- Primary Survey (60 seconds)
- Airway/Breathing: Oxygen saturation >95%
- Circulation: Pulse, blood pressure, capillary refill <2 seconds
- Disability: Mental status, neurologic function
- Exposure: Visual inspection for bleeding, uterine contour
- Obstetric Survey (90 seconds)
- Fetal status: FHR pattern, variability, decelerations
- Uterine assessment: Tone, tenderness, bleeding
- Cervical examination: Dilation, effacement, station
- Membrane status: Intact, ruptured, cord prolapse
- Decision Point (30 seconds)
- Immediate delivery vs stabilization vs expectant management
- Route of delivery: Vaginal vs cesarean vs operative vaginal
Master Clinician Mindset:
- Pattern Recognition: "I've seen this before" - instant categorization
- Protocol Activation: "I know exactly what to do" - automatic responses
- Team Leadership: "Everyone knows their role" - coordinated execution
- Outcome Focus: "We will achieve the best possible result" - relentless optimization
💡 Master This: "The 3-Second Rule" - Within 3 seconds of entering any obstetric emergency, you should know: 1) What type of emergency, 2) What immediate action is needed, 3) What the optimal outcome looks like. Master this instant assessment, and you control any obstetric crisis.
Clinical Excellence Metrics:
- Recognition speed: <2 minutes for any emergency pattern
- Protocol initiation: <5 minutes from recognition to first intervention
- Team coordination: <10 minutes to full emergency response
- Outcome achievement: >90% optimal outcomes with systematic approach
The mastery arsenal transforms knowledge into action, protocols into results, and emergencies into controlled challenges with predictable success patterns.
🎯 The Mastery Arsenal: Rapid-Fire Clinical Command
Practice Questions: Labor Complications
Test your understanding with these related questions
A 30-year-old woman, gravida 2, para 1, at 12 weeks' gestation comes to the physician for a prenatal visit. She feels well. Pregnancy and vaginal delivery of her first child were uncomplicated. Five years ago, she was diagnosed with hypertension but reports that she has been noncompliant with her hypertension regimen. The patient does not smoke or drink alcohol. She does not use illicit drugs. Medications include methyldopa, folic acid, and a multivitamin. Her temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 145/90 mm Hg. Physical examination shows no abnormalities. Laboratory studies, including serum glucose level, and thyroid-stimulating hormone concentration, are within normal limits. The patient is at increased risk of developing which of the following complications?













