Thyroid disorders in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thyroid disorders in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thyroid disorders in pregnancy US Medical PG Question 1: A 23-year-old primigravida presents to her physician’s office at 12 weeks gestation complaining of increased sweating and palpitations for the last week. She does not have edema or dyspnea, and had no pre-existing illnesses. The patient says that the symptoms started a few days after several episodes of vomiting. She managed the vomiting at home and yesterday the vomiting stopped, but the symptoms she presents with are persistent. The pre-pregnancy weight was 54 kg (119 lb). The current weight is 55 kg (121 lb). The vital signs are as follows: blood pressure 130/85 mm Hg, heart rate 113/min, respiratory rate 15/min, and temperature 37.0℃ (98.6℉). The physical examination is significant for diaphoresis, an irregular heartbeat, and a fine resting tremor of the hands. The neck is not enlarged and the thyroid gland is not palpable. The ECG shows sinus tachyarrhythmia. The thyroid panel is as follows:
Thyroid stimulating hormone (TSH) < 0.1 mU/L
Total T4 178 nmol/L
Free T4 31 pmol/L
Which of the following is indicated?
- A. Recommend iodine radioablation
- B. Schedule a subtotal thyroidectomy
- C. Prescribe methimazole
- D. Manage with propylthiouracil
- E. Ensure proper hydration and prescribe a beta-blocker (Correct Answer)
Thyroid disorders in pregnancy Explanation: ***Ensure proper hydration and prescribe a beta-blocker***
- The patient's symptoms (sweating, palpitations, irregular heartbeat, tremor, tachycardia, low TSH, high T4) are consistent with **hyperthyroidism**. However, her symptoms started shortly after persistent vomiting (hyperemesis gravidarum), and the thyroid is not enlarged, suggesting **gestational transient thyrotoxicosis (GTT)** rather than Graves' disease. GTT is typically mild and self-limiting, often resolving by mid-gestation.
- Since the patient is pregnant, definitive treatments like **radioiodine ablation** or **thyroidectomy** are contraindicated. Antithyroid medications (methimazole, PTU) are also generally avoided in GTT unless symptoms are severe, due to potential side effects for both mother and fetus. The primary management for mild to moderate GTT involves supportive care, such as ensuring proper hydration and using **beta-blockers** (e.g., propranolol) to alleviate adrenergic symptoms like palpitations and tremors.
*Recommend iodine radioablation*
- **Radioactive iodine (RAI) therapy** for hyperthyroidism is absolutely **contraindicated in pregnancy** because radioactive iodine crosses the placenta and can destroy the fetal thyroid gland, leading to congenital hypothyroidism.
- This treatment is primarily used for definitive treatment of hyperthyroidism in non-pregnant patients, particularly for **Graves' disease** or toxic nodular goiter.
*Schedule a subtotal thyroidectomy*
- **Thyroidectomy** at 12 weeks gestation carries significant risks to both the mother (surgical complications) and the fetus (miscarriage, preterm labor). It is considered only in very rare cases of severe, uncontrolled hyperthyroidism refractory to medical management, typically in the second trimester.
- Given the suspicion of **gestational transient thyrotoxicosis (GTT)**, a self-limiting condition, surgical intervention is highly inappropriate.
*Prescribe methimazole*
- **Methimazole** is an antithyroid drug used to reduce thyroid hormone synthesis. While effective for hyperthyroidism, it is generally **avoided in the first trimester of pregnancy** due to its association with rare but severe fetal abnormalities, such as aplasia cutis.
- For gestational transient thyrotoxicosis, antithyroid drugs are typically not necessary because the condition is usually mild and self-limiting.
*Manage with propylthiouracil*
- **Propylthiouracil (PTU)** is another antithyroid drug that blocks thyroid hormone synthesis. It is typically **preferred over methimazole during the first trimester of pregnancy** when antithyroid medication is absolutely necessary, as it has a lower risk of teratogenicity during this period.
- However, PTU itself carries risks, including rare but severe **hepatotoxicity**, and is generally reserved for cases of severe hyperthyroidism where the benefits outweigh the risks. In mild to moderate gestational transient thyrotoxicosis, medications like PTU are usually not required.
Thyroid disorders in pregnancy US Medical PG Question 2: A 28-year-old gravida-2-para-1 at 12 weeks gestation presents for a prenatal visit. Over the past week, she has felt increasingly tired, even after waking up in the morning. She is vegan and avoids all animal products. She was diagnosed with Graves’ disease 6 months ago. Before conception, methimazole was switched to propylthiouracil (PTU). Other medications include folic acid and a multivitamin. The vital signs include: temperature 37.1℃ (98.8℉), pulse 72/min, respiratory rate 12/min, and blood pressure 110/75 mm Hg. The conjunctivae and nail beds are pale. Petechiae are present over the distal lower extremities. The pelvic examination reveals a uterus consistent in size with a 12-week gestation. Examination of the neck, lungs, heart, and abdomen shows no abnormalities. The laboratory studies show the following:
Laboratory test
Hemoglobin 9.0 g/dL
Mean corpuscular volume 90 μm3
Leukocyte count 4,000/mm3
Segmented neutrophils 55%
Lymphocytes 40%
Platelet count 110,000/mm3
Serum
Thyroid-stimulating hormone 0.1 μU/mL
Thyroxine (T-4) 8 μg/dL
Lactate dehydrogenase 60 U/L
Total bilirubin 0.5 mg/dL
Iron 100 μg/dL
Ferritin 110 ng/mL
Total iron-binding capacity 250 μg/dL
Which of the following best explains these findings?
- A. Excess antithyroid medication
- B. Drug-induced marrow failure (Correct Answer)
- C. Vitamin B12 deficiency
- D. Hemodilution of pregnancy
- E. Autoimmune hemolysis
Thyroid disorders in pregnancy Explanation: **Drug-induced marrow failure**
- The patient's **pancytopenia** (low hemoglobin, leukocytes, and platelets) along with petechiae, in the context of **propylthiouracil (PTU)** use, strongly suggests drug-induced bone marrow suppression. PTU is known to cause agranulocytosis and, less commonly, aplastic anemia.
- The **normal thyroid hormone levels** (TSH 0.1 μU/mL, T4 8 μg/dL) indicate that her Graves' disease is adequately controlled, but the hematological changes are severe enough to point towards a drug-related adverse effect rather than thyroid dysfunction.
*Excess antithyroid medication*
- While excess antithyroid medication like PTU can lead to **hypothyroidism**, the patient's low TSH (though near normal during pregnancy due to hCG effects) and normal T4 indicate she is **not hypothyroid**.
- Hypothyroidism does not directly cause **pancytopenia** or petechiae, which are observed in this case.
*Vitamin B12 deficiency*
- **Vitamin B12 deficiency** typically causes **macrocytic anemia** (high MCV), and sometimes pancytopenia. However, this patient has a **normal MCV (90 μm3)**.
- Although the patient is vegan, she is taking a multivitamin and folic acid, and iron studies are normal, making B12 deficiency less likely given the MCV.
*Hemodilution of pregnancy*
- **Physiologic hemodilution** in pregnancy can cause a *mild drop* in hemoglobin and hematocrit and a *slight decrease* in platelet count but typically does not lead to **leukopenia** or significant thrombocytopenia with petechiae.
- The degree of *pancytopenia* observed here is beyond what would be expected from normal hemodilution.
*Autoimmune hemolysis*
- **Autoimmune hemolysis** would primarily cause **anemia** and potentially elevated bilirubin and LDH due to red blood cell destruction, but it does **not explain the leukopenia or thrombocytopenia** (pancytopenia).
- The patient's bilirubin and LDH are normal, making significant hemolysis unlikely.
Thyroid disorders in pregnancy US Medical PG Question 3: A 28-year-old G1P0 woman comes to the emergency department complaining that her water just broke. She reports irregular prenatal care due to her erratic schedule. She is also unsure of her gestational age but claims that her belly began to show shortly after she received her thyroidectomy for her Graves disease about 9 months ago. She denies any known fevers, chills, abnormal vaginal discharge/bleeding, or sexually transmitted infections. She develops frequent and regular contractions and subsequently goes into active labor. A fetus was later vaginally delivered with a fetal heart rate of 180 bpm. A neonatal physical examination demonstrates a lack of a sagittal cranial suture and an APGAR score of 8 and 8, at 1 and 5 minutes respectively. What findings would you expect in the baby?
- A. Pericardial effusion
- B. Group B streptococcus in blood
- C. Low hemoglobin
- D. High levels of free T4 and total T3 (Correct Answer)
- E. High thyroid-stimulating hormone
Thyroid disorders in pregnancy Explanation: ***High levels of free T4 and total T3***
- This patient likely has **neonatal thyrotoxicosis** due to transplacental passage of **thyroid-stimulating immunoglobulins (TSIs)** from her mother with a history of Graves' disease and thyroidectomy.
- The fetal heart rate of 180 bpm and the lack of a sagittal cranial suture (suggesting **craniosynostosis**, a known complication of neonatal hyperthyroidism) are consistent with severe **hyperthyroidism** and elevated thyroid hormone levels.
*Pericardial effusion*
- While hyperthyroidism can cause **cardiac complications** like high-output cardiac failure, **pericardial effusion** is not a typical or expected finding in neonatal thyrotoxicosis.
- Pericardial effusion is more commonly associated with conditions like **congestive heart failure** of other etiologies, **hypothyroidism**, or infections.
*Group B streptococcus in blood*
- The mother denies any known fevers, chills, abnormal vaginal discharge, or STIs, and there is no indication of **chorioamnionitis** or other risk factors for **Group B Streptococcus (GBS)** infection.
- While GBS can cause neonatal sepsis, the clinical presentation and maternal history strongly point towards an **endocrine disorder** rather than an infection.
*Low hemoglobin*
- **Anemia** is not a characteristic feature of **neonatal thyrotoxicosis**.
- Hyperthyroidism can sometimes be associated with **increased red blood cell turnover** but usually does not lead to clinically significant low hemoglobin levels in neonates.
*High thyroid-stimulating hormone*
- **High TSH** levels would indicate **hypothyroidism**, not hyperthyroidism.
- In neonatal thyrotoxicosis, due to elevated thyroid hormone levels, the **pituitary's TSH secretion is suppressed**, leading to low or undetectable TSH levels.
Thyroid disorders in pregnancy US Medical PG Question 4: A 26-year-old G1P0 presents to her first obstetric visit after having a positive urine pregnancy test at home. Her last menstrual period was 9 weeks ago. She has no past medical history, but her mother has rheumatoid arthritis. The patient states that for several weeks, she has felt especially warm, even when her co-workers do not, and had muscle weakness. She also complains of mood swings and fatigue. At this visit, her temperature is 99.0°F (37.2°C), blood pressure is 140/81 mmHg, pulse is 106/min, and respirations are 17/min. Physical exam is notable for 3+ deep tendon reflexes bilaterally and 4/5 strength in both hips and shoulders. Ultrasound confirms the presence of a heart beat and shows a crown rump length that is consistent with a gestational age of 9 weeks and 3 days. Which of the following is the best therapy for this patient?
- A. Methimazole
- B. Prednisone
- C. Propylthiouracil (Correct Answer)
- D. Intravenous immunoglobulin
- E. Radioactive thyroid ablation (I-131)
Thyroid disorders in pregnancy Explanation: ***Propylthiouracil***
- This patient presents with symptoms of **hyperthyroidism** (warmth, muscle weakness, mood swings, fatigue, tachycardia, hypertension, and hyperreflexia) exacerbated by pregnancy. **Propylthiouracil (PTU)** is the preferred treatment for hyperthyroidism in the **first trimester** of pregnancy due to a lower risk of teratogenicity compared to methimazole.
- PTU works by **inhibiting thyroid hormone synthesis** and also blocks the peripheral conversion of T4 to T3.
*Methimazole*
- While an effective antithyroid drug, methimazole is generally **avoided in the first trimester** of pregnancy due to its association with rare but severe birth defects, such as **aplasia cutis** and choanal atresia.
- It becomes the preferred treatment in the second and third trimesters if antithyroid medication is still required, due to a lower risk of liver toxicity compared to PTU.
*Prednisone*
- **Prednisone** is a corticosteroid used to manage inflammatory conditions and suppress the immune system; it is **not a primary treatment for hyperthyroidism**.
- While it can be used in severe cases of thyroid storm to reduce peripheral conversion of T4 to T3, it is not the initial therapy for uncomplicated gestational hyperthyroidism.
*Intravenous immunoglobulin*
- **Intravenous immunoglobulin (IVIG)** is an immune modulator used in various autoimmune conditions but has **no direct role in the treatment of hyperthyroidism**.
- It works by providing antibodies and modulating the immune response, which is not the primary mechanism needed to control excessive thyroid hormone production.
*Radioactive thyroid ablation (I-131)*
- **Radioactive iodine ablation** is absolutely **contraindicated in pregnancy** as it can cross the placenta and destroy the fetal thyroid gland, leading to **fetal hypothyroidism**.
- This treatment is reserved for non-pregnant individuals with hyperthyroidism who fail antithyroid medications or have recurrent disease.
Thyroid disorders in pregnancy US Medical PG Question 5: A 28-year-old woman, gravida 1, para 0, at 10 weeks gestation comes to the physician for her first prenatal visit. Today, she feels well. She has no history of serious illness. Her pulse is 75/min and blood pressure is 110/74 mm Hg. Examination shows no abnormalities. Ultrasonography shows a pregnancy consistent in size with a 10-week gestation. Serum studies in this patient are most likely to show which of the following sets of laboratory values?
$$$ Thyroid-binding globulin %%% Free Triiodothyronine (T3) %%% Free Thyroxine (T4) %%% Total T3+T4 $$$
- A. Normal ↑ ↑ ↑
- B. ↑ normal normal ↑ (Correct Answer)
- C. Normal normal normal normal
- D. ↓ normal normal ↓
- E. ↓ ↓ normal ↓
Thyroid disorders in pregnancy Explanation: ***↑ normal normal ↑***
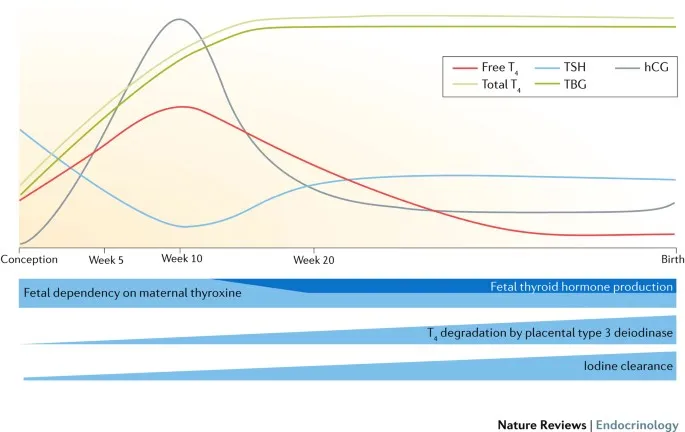
- This option correctly reflects the typical changes in thyroid economy during pregnancy: **increased thyroid-binding globulin (TBG)** due to estrogen, leading to **increased total T3 and T4**, while **free T3 and free T4 remain normal** as the thyroid gland compensates.
- The elevated TBG binds more thyroid hormones, initially decreasing free hormone levels slightly, but the thyroid gland responds by producing more T3 and T4 to maintain **euthyroid** state with normal free hormone levels.
*Normal ↑ ↑ ↑*
- This option incorrectly suggests that **free T3 and free T4 would be elevated** along with total T3 and T4, which is not typical in a healthy pregnant woman.
- While total T3 and T4 increase, the body maintains **euthyroidism** by keeping free thyroid hormone levels within the normal range.
*Normal normal normal normal*
- This option incorrectly suggests that all thyroid parameters remain normal, which is not true for **TBG, total T3, and total T4** in pregnancy.
- The significant physiological changes during pregnancy, particularly the increase in **estrogen**, directly impact TBG levels and subsequently total thyroid hormone levels.
*↓ normal normal ↓*
- This option is incorrect as **TBG and total T3+T4 generally increase** during pregnancy, not decrease.
- A decrease in these values, especially with normal free hormones, is not consistent with the typical **euthyroid state** of a healthy pregnant woman.
*↓ ↓ normal ↓*
- This option incorrectly suggests a decrease in **TBG, free T3, and total T3+T4**, which would indicate a hypothyroid state, inconsistent with the patient's well-being and normal examination findings.
- A healthy pregnant woman maintains **euthyroidism** with normal free thyroid hormone levels.
Thyroid disorders in pregnancy US Medical PG Question 6: A 25-year-old woman presents to her physician with a missed mense and occasional morning nausea. Her menstrual cycles have previously been normal and on time. She has hypothyroidism resulting from Hashimoto thyroiditis diagnosed 2 years ago. She receives levothyroxine (50 mcg daily) and is euthyroid. She does not take any other medications, including birth control pills. At the time of presentation, her vital signs are as follows: blood pressure 120/80 mm Hg, heart rate 68/min, respiratory rate 12/min, and temperature 36.5℃ (97.7℉). The physical examination shows slight breast engorgement and nipple hyperpigmentation. The gynecologic examination reveals cervical softening and increased mobility. The uterus is enlarged. There are no adnexal masses. The thyroid panel is as follows:
Thyroid stimulating hormone (TSH) 3.41 mU/L
Total T4 111 nmol/L
Free T4 20 pmol/L
Which of the following adjustments should be made to the patient’s therapy?
- A. Increase levothyroxine dosage by 20%–30% (Correct Answer)
- B. Decrease levothyroxine dosage by 30%
- C. Discontinue levothyroxine
- D. The patient is euthyroid, so no adjustments should be made
- E. Increase levothyroxine dosage by 5% each week up to 50%
Thyroid disorders in pregnancy Explanation: ***Increase levothyroxine dosage by 20%–30%***
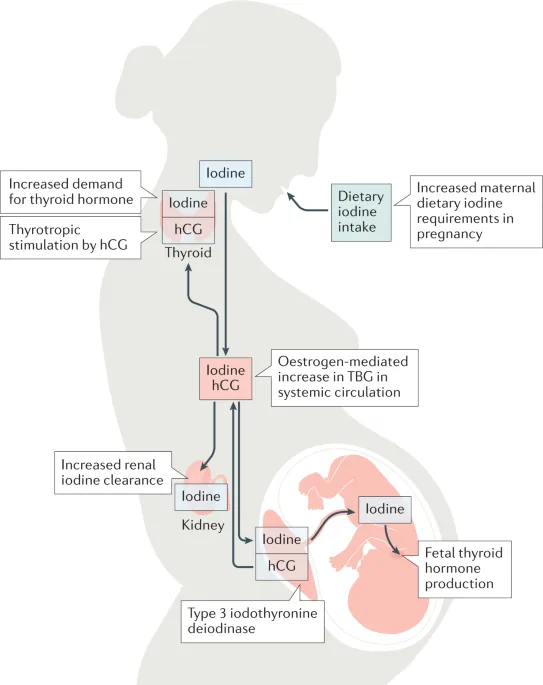
- The patient's symptoms (missed menses, nausea, breast changes, enlarged uterus, cervical changes) are highly suggestive of **pregnancy**. During pregnancy, **thyroid hormone requirements increase significantly** due to increased levels of **thyroid-binding globulin (TBG)** stimulated by estrogen, and the production of **human chorionic gonadotropin (hCG)** which has TSH-like activity.
- The recommended management for pregnant women with hypothyroidism is to **increase the levothyroxine dose by approximately 25-50%** and monitor TSH and free T4 levels every 4-6 weeks to maintain a TSH level within the goal range for pregnancy (typically <2.5 mU/L in the first trimester).
*Decrease levothyroxine dosage by 30%*
- Decreasing levothyroxine would lead to **hypothyroidism**, which is detrimental in pregnancy and associated with adverse outcomes such as **preeclampsia**, **gestational hypertension**, **low birth weight**, and **neurocognitive impairment** in the offspring.
- Thyroid hormone requirements increase, not decrease, during pregnancy.
*Discontinue levothyroxine*
- **Discontinuing levothyroxine** would result in severe hypothyroidism, posing significant risks to both the mother and the developing fetus.
- Hypothyroidism must be treated throughout pregnancy to ensure proper fetal development.
*The patient is euthyroid, so no adjustments should be made*
- While the patient's thyroid panel currently shows euthyroid values (TSH 3.41 mU/L is within normal range but slightly elevated for first-trimester pregnancy goals), the **onset of pregnancy** rapidly increases thyroid hormone demand.
- Failure to adjust the dose can lead to **maternal and fetal hypothyroidism** as pregnancy progresses, even if the patient is currently euthyroid.
*Increase levothyroxine dosage by 5% each week up to 50%*
- A gradual increase of 5% each week may be too slow and insufficient to meet the rapidly increasing thyroid hormone demands of early pregnancy.
- The standard recommendation is to make a more substantial initial adjustment (20-30%) as soon as pregnancy is confirmed, followed by close monitoring and further adjustments.
Thyroid disorders in pregnancy US Medical PG Question 7: A 25-year-old woman, gravida 2, para 1, at 25 weeks' gestation comes to the emergency department because of a 1-day history of fever and right-sided flank pain. During this period, she also had chills, nausea, vomiting, and burning on urination. Her last prenatal visit was 10 weeks ago. Pregnancy and delivery of her first child were uncomplicated. Her temperature is 39°C (102.2°F), pulse is 110/min, respirations are 20/min, and blood pressure is 110/70 mm Hg. Physical examination shows costovertebral angle tenderness on the right. The abdomen is soft and nontender, and no contractions are felt. Pelvic examination shows a uterus consistent in size with a 25-week gestation. Fetal heart rate is 170/min. Laboratory studies show:
Leukocyte count 15,000/mm3
Urine
Nitrite 2+
Protein 1+
Blood 1+
RBC 5/hpf
WBC 500/hpf
Blood and urine samples are obtained for culture and drug sensitivity. Which of the following is the most appropriate next step in management?
- A. Inpatient treatment with intravenous ceftriaxone (Correct Answer)
- B. Perform a renal ultrasound
- C. Outpatient treatment with oral ciprofloxacin
- D. Inpatient treatment with intravenous ampicillin and gentamicin
- E. Admit the patient and request an emergent obstetrical consult
Thyroid disorders in pregnancy Explanation: ***Inpatient treatment with intravenous ceftriaxone***
- The patient presents with classic signs of **pyelonephritis** (fever, flank pain, nausea, vomiting, CVA tenderness) in pregnancy, which warrants **inpatient admission** and **IV antibiotics** to prevent complications such as sepsis, preterm labor, and fetal compromise.
- **Ceftriaxone** is a broad-spectrum cephalosporin that is safe and effective in pregnancy for treating urinary tract infections, including pyelonephritis.
*Perform a renal ultrasound*
- While a **renal ultrasound** may be considered in cases of persistent fever after 48-72 hours of antibiotic therapy or if there's suspicion of obstruction or abscess, it is **not the immediate next step**.
- The priority is to initiate antibiotics promptly to treat the acute infection and prevent further complications.
*Outpatient treatment with oral ciprofloxacin*
- **Outpatient treatment** is inappropriate for **pyelonephritis in pregnancy** due to the high risk of complications for both the mother and the fetus.
- **Ciprofloxacin** (a fluoroquinolone) is generally **contraindicated in pregnancy** because of potential adverse effects on fetal cartilage development.
*Inpatient treatment with intravenous ampicillin and gentamicin*
- Although **ampicillin and gentamicin** are effective for many UTIs and safe in pregnancy, they are often reserved for cases where local resistance patterns favor this combination or as a second-line option.
- **Ceftriaxone** is a preferred first-line empiric choice for pyelonephritis in pregnancy due to its broad coverage and once-daily dosing.
*Admit the patient and request an emergent obstetrical consult*
- While admitting the patient is correct, **immediately requesting an emergent obstetrical consult** is premature as the primary issue is an acute infection requiring medical management.
- Obstetrics consultation is important in managing high-risk pregnancies or complications like preterm labor, but antibiotics for pyelonephritis should be initiated first, and then an obstetrician can be consulted for comanagement.
Thyroid disorders in pregnancy US Medical PG Question 8: A researcher is studying physiologic and hormonal changes that occur during pregnancy. Specifically, they examine the behavior of progesterone over the course of the menstrual cycle and find that it normally decreases over time; however, during pregnancy this decrease does not occur in the usual time frame. The researcher identifies a circulating factor that appears to be responsible for this difference in progesterone behavior. In order to further examine this factor, the researcher denatures the circulating factor and examines the sizes of its components on a western blot as compared to several other hormones. One of the bands the researcher identifies in this circulating factor is identical to that of another known hormone with which of the following sites of action?
- A. Thyroid gland (Correct Answer)
- B. Adrenal gland
- C. Adipocytes
- D. Bones
- E. Kidney tubules
Thyroid disorders in pregnancy Explanation: ***Correct: Thyroid gland***
- The circulating factor described is **human chorionic gonadotropin (hCG)**, which maintains the corpus luteum and progesterone production during early pregnancy
- hCG is a **glycoprotein hormone** composed of an **α subunit** and a **β subunit**
- The **α subunit of hCG is identical** to the α subunits of **TSH (thyroid-stimulating hormone)**, **LH (luteinizing hormone)**, and **FSH (follicle-stimulating hormone)**
- When denatured and examined on Western blot, one of the bands (the α subunit) would be identical to that of **TSH**
- **TSH acts on the thyroid gland** to stimulate thyroid hormone synthesis and release
- This structural similarity explains why very high levels of hCG (as in molar pregnancy or hyperemesis gravidarum) can sometimes cause **thyrotoxicosis** due to cross-reactivity with TSH receptors
*Incorrect: Adrenal gland*
- **ACTH (adrenocorticotropic hormone)** acts on the adrenal cortex to stimulate cortisol production
- ACTH is a **peptide hormone** derived from POMC (pro-opiomelanocortin) and does **NOT share any structural components** with hCG
- There is no identical band between hCG and ACTH on Western blot
*Incorrect: Adipocytes*
- Adipocytes are regulated by hormones like **insulin** and **leptin**
- Neither of these hormones share structural components with hCG
*Incorrect: Bones*
- Bones are primarily regulated by **PTH (parathyroid hormone)**, **calcitonin**, and **vitamin D**
- None of these hormones share structural components with hCG
*Incorrect: Kidney tubules*
- Kidney tubules are regulated by **ADH (antidiuretic hormone/vasopressin)** and **aldosterone**
- Neither shares structural components with hCG
Thyroid disorders in pregnancy US Medical PG Question 9: A 36-year-old primigravida presents to her obstetrician for antenatal care. She is at 24 weeks of gestation and does not have any current complaint except for occasional leg cramps. She does not smoke or drink alcohol. Family history is irrelevant. Her temperature is 36.9°C (98.42°F), blood pressure is 100/60 mm Hg, and pulse of 95/minute. Her body mass index is 21 kg/m² (46 pounds/m²). Physical examination reveals a palpable uterus above the umbilicus with no other abnormalities. Which of the following screening tests is suitable for this patient?
- A. Fasting and random glucose testing for gestational diabetes mellitus
- B. HbA1C for gestational diabetes mellitus
- C. Oral glucose tolerance test for gestational diabetes mellitus (Correct Answer)
- D. Complete blood count for iron deficiency anemia
- E. Wet mount microscopy of vaginal secretions for bacterial vaginosis
Thyroid disorders in pregnancy Explanation: ***Oral glucose tolerance test for gestational diabetes mellitus***
- The **oral glucose tolerance test (OGTT)**, typically performed between **24 and 28 weeks of gestation**, is the gold standard for screening and diagnosing **gestational diabetes mellitus (GDM)**. This patient is at 24 weeks, making it the appropriate time for this screening.
- GDM, if undiagnosed and untreated, can lead to significant maternal and fetal complications, including **macrosomia**, **preeclampsia**, **neonatal hypoglycemia**, and **shoulder dystocia**.
*Fasting and random glucose testing for gestational diabetes mellitus*
- While **fasting** or **random glucose** values can indicate hyperglycemia, they are **not sensitive or specific enough** on their own to reliably screen for or diagnose GDM.
- A single elevated reading might prompt further testing, but it's not the primary or most suitable screening method.
*HbA1C for gestational diabetes mellitus*
- **HbA1c** reflects **average blood glucose levels over the past 2-3 months** and is primarily used for diagnosing and monitoring **pre-existing diabetes** or assessing glycemic control in non-pregnant individuals.
- Due to the **physiological changes in red blood cell turnover during pregnancy** and the acute onset nature of GDM, HbA1c is **not recommended** as a first-line screening tool for GDM.
*Complete blood count for iron deficiency anemia*
- While **complete blood count (CBC)** is a routine prenatal screening test to check for **anemia**, it is typically done earlier in pregnancy and again in the third trimester. There are no specific symptoms in this patient that strongly suggest immediate concern for anemia beyond routine.
- The question specifically asks for the "most suitable" screening test at this gestational age, and the **GDM screening** takes precedence given the timing.
*Wet mount microscopy of vaginal secretions for bacterial vaginosis*
- There are **no symptoms of vaginal infection** (e.g., unusual discharge, itching, odor) mentioned in the patient's presentation that would warrant immediate screening for **bacterial vaginosis (BV)** at this visit.
- While BV can be associated with adverse pregnancy outcomes, routine asymptomatic screening by wet mount is **not universally recommended** at 24 weeks gestation without other indications.
Thyroid disorders in pregnancy US Medical PG Question 10: A 28-year-old primigravid woman comes to the emergency department because of a 12-hour history of lower abdominal pain and vaginal bleeding. She also had nausea and fatigue for the past 3 weeks. Her last menstrual period was 8 weeks ago. Prior to that, her menses occurred regularly at 30-day intervals and lasted for 4 days. There is no history of medical illness, and she takes no medications. Her temperature is 37°C (98.6°F), pulse is 95/min, and blood pressure is 100/70 mm Hg. Pelvic examination is painful and shows a uterus consistent in size with a 13-week gestation. A urine pregnancy test is positive. β-HCG level is 106,000 mIU/mL (N < 5 mIU/mL). Transvaginal ultrasonography shows unclear, amorphous fetal parts and a large placenta with multiple cystic spaces. Which of the following is the most likely cause of this patient's condition?
- A. Placenta implantation into myometrium
- B. Trophoblastic proliferation with chorionic villi distention (Correct Answer)
- C. Embryonic death with cervical dilation
- D. Malpositioned placenta overlying the cervix
- E. Malignant transformation of trophoblastic tissue
Thyroid disorders in pregnancy Explanation: ***Trophoblastic proliferation with chorionic villi distention***
- This description fits a **hydatidiform mole** (molar pregnancy), characterized by abnormal **trophoblastic proliferation** and **swollen, cystic chorionic villi**.
- The ultrasound findings of unclear, amorphous fetal parts and a large placenta with multiple cystic spaces ("snowstorm appearance") are classic for a **partial hydatidiform mole**, consistent with the highly elevated **β-hCG level**.
*Placenta implantation into myometrium*
- This describes **placenta accreta**, where the placenta abnormally adheres to or invades the **myometrium**.
- It is typically diagnosed in the third trimester due to bleeding and is not associated with early, high β-hCG levels or the ultrasound features seen here.
*Embryonic death with cervical dilation*
- This suggests an **incomplete or inevitable abortion**. While it can cause pain and bleeding, the specific ultrasound findings of a **large placenta with multiple cystic spaces** and very high β-hCG are not typical.
- In embryonic death, β-hCG levels would typically fall or plateau, not be excessively high.
*Malpositioned placenta overlying the cervix*
- This refers to **placenta previa**, where the placenta covers the internal cervical os. It primarily causes **painless vaginal bleeding** in the second or third trimester.
- The ultrasound findings and the extremely elevated β-hCG in the first trimester are inconsistent with placenta previa.
*Malignant transformation of trophoblastic tissue*
- While a hydatidiform mole can progress to **gestational trophoblastic neoplasia** (GTN), including choriocarcinoma, this option describes a subsequent complication rather than the initial presentation of the mole itself.
- GTN would typically be diagnosed after evacuation of a mole, or if β-hCG levels persist or rise post-evacuation. The initial diagnosis here is the mole.
More Thyroid disorders in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.