Prior cesarean delivery management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Prior cesarean delivery management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Prior cesarean delivery management US Medical PG Question 1: A 27-year old primigravid woman at 37 weeks' gestation comes to the emergency department because of frequent contractions for 4 hours. Her pregnancy has been complicated by hyperemesis gravidarum which subsided in the second trimester. The contractions occur every 10–15 minutes and have been increasing in intensity and duration since onset. Her temperature is 37.1°C (98.8°F), pulse is 110/min, and blood pressure is 140/85 mm Hg. Uterine contractions are felt on palpation. Pelvic examination shows clear fluid in the vagina. The cervix is 50% effaced and 3 cm dilated. After 4 hours the cervix is 80% effaced and 6 cm dilated. Pelvic examination is inconclusive for the position of the fetal head. The fetal heart rate is reassuring. Which of the following is the most appropriate next step?
- A. Administer oxytocin
- B. Perform external cephalic version
- C. Administer misoprostol
- D. Perform Mauriceau-Smellie-Veit maneuver
- E. Perform ultrasonography (Correct Answer)
Prior cesarean delivery management Explanation: ***Perform ultrasonography***
- The examination notes that the **pelvic examination is inconclusive for the position of the fetal head**, which is a critical piece of information needed for safe delivery. **Ultrasonography** is the most appropriate next step to ascertain the fetal presentation and position, especially given the dilated cervix.
- Determining fetal position is essential to rule out **malpresentation**, such as **breech** or **transverse lie**, which would significantly impact the delivery plan and potentially necessitate a **cesarean section**.
*Administer oxytocin*
- **Oxytocin** is used to induce or augment labor when contractions are insufficient or labor is prolonged, but in this case, the cervix is progressing well (from 3 cm to 6 cm dilation in 4 hours), indicating **active labor**.
- Without knowing the fetal presentation, administering oxytocin could exacerbate issues if there's a **malpresentation**, potentially leading to **fetal distress** or **uterine rupture**.
*Perform external cephalic version*
- **External cephalic version (ECV)** is performed to change a **breech presentation** to a **cephalic presentation** by external manipulation, typically done before labor onset or early in labor at term.
- This patient is already in **active labor** with significant cervical dilation (6 cm), making ECV less likely to be successful and potentially increasing risks like **placental abruption** or **umbilical cord compression**.
*Administer misoprostol*
- **Misoprostol** is a prostaglandin analog used for **cervical ripening** and **labor induction** in cases where the cervix is unfavorable or labor needs to be initiated.
- This patient is already in **active labor** with progressive cervical dilation, making misoprostol unnecessary and potentially harmful due to the risk of **uterine hyperstimulation**.
*Perform Mauriceau-Smellie-Veit maneuver*
- The **Mauriceau-Smellie-Veit maneuver** is a technique used during a **vaginal breech delivery** to deliver the fetal head, specifically in cases of **frank or complete breech** that are being delivered vaginally.
- This maneuver is only performed *during* delivery of a breech baby, and the fetal position is currently unknown. It would be premature and inappropriate to consider this maneuver without first confirming a **breech presentation** and the decision for vaginal delivery.
Prior cesarean delivery management US Medical PG Question 2: Immediately following prolonged delivery of the placenta at 40 weeks gestation, a 32-year-old multiparous woman develops vaginal bleeding. Other than mild asthma, the patient’s pregnancy has been uncomplicated. She has attended many prenatal appointments and followed the physician's advice about screening for diseases, laboratory testing, diet, and exercise. Previous pregnancies were uncomplicated. She has no history of a serious illness. She is currently on intravenous infusion of oxytocin. Her temperature is 37.2°C (99.0°F), blood pressure is 108/60 mm Hg, pulse is 88/min, and respirations are 17/min. Uterine palpation reveals a soft enlarged fundus that extends above the umbilicus. Based on the assessment of the birth canal and placenta, which of the following options is the most appropriate initial step in patient management?
- A. Intramuscular carboprost
- B. Manual exploration of the uterus
- C. Discontinuing oxytocin
- D. Intravenous methylergonovine
- E. Uterine fundal massage (Correct Answer)
Prior cesarean delivery management Explanation: ***Uterine fundal massage***
- The patient presents with **postpartum hemorrhage** indicated by vaginal bleeding and a **soft, enlarged fundus** after placental delivery, suggesting **uterine atony**.
- **Uterine fundal massage** is the **first-line intervention** to encourage uterine contraction and reduce bleeding by expelling clots and compressing vessels.
*Intramuscular carboprost*
- **Carboprost** is a **prostaglandin F2 alpha analog** used to treat **uterine atony** when initial measures like uterine massage and oxytocin are insufficient.
- It is contraindicated in patients with **asthma** due to its bronchoconstrictive effects, which this patient has.
*Manual exploration of the uterus*
- **Manual exploration of the uterus** is indicated when there is suspicion of **retained placental fragments** or **uterine rupture**.
- While these can cause postpartum hemorrhage, the primary finding of a soft, boggy uterus points more strongly to atony, making massage the immediate priority.
*Discontinuing oxytocin*
- The patient is already on an **intravenous oxytocin infusion**, which is a uterotonic agent used to prevent and treat uterine atony.
- Discontinuing it would worsen **uterine atony** and increase blood loss, directly contradicting the goal of management.
*Intravenous methylergonovine*
- **Methylergonovine** is an **ergot alkaloid** used to treat **uterine atony**, but it is contraindicated in patients with **hypertension**, which is not explicitly present here, but it is a potent vasoconstrictor and second-line.
- It is often used as a **second-line agent** if oxytocin and massage are ineffective and there are no contraindications.
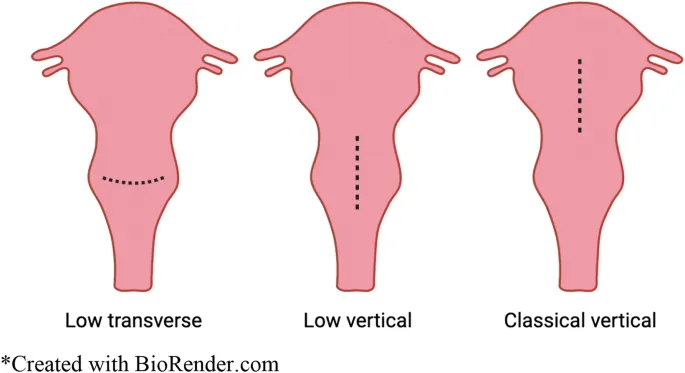
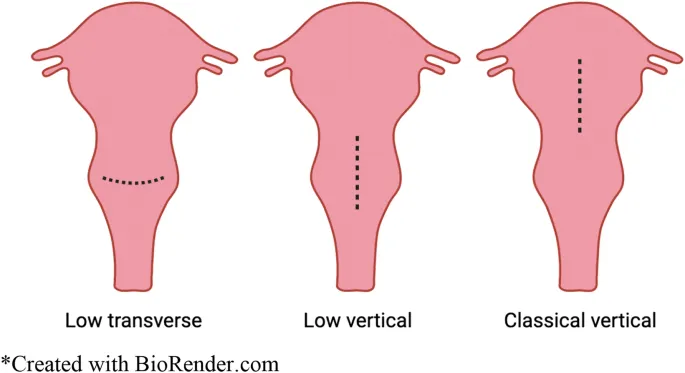
Prior cesarean delivery management US Medical PG Question 3: A 30-year-old woman, gravida 2, para 1, at 42 weeks' gestation is admitted to the hospital in active labor. Pregnancy has been complicated by gestational diabetes, for which she has been receiving insulin injections. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 90/min, respirations are 18/min, and blood pressure is 135/80 mm Hg. The fetal heart rate tracing shows a baseline heart rate of 145/min and moderate variation with frequent accelerations and occasional early decelerations. She undergoes an elective repeat lower segment transverse cesarean section with complete removal of the placenta. Shortly after the operation, she starts having heavy uterine bleeding with passage of clots. Examination shows a soft uterus on palpation. Her bleeding continues despite fundal massage and the use of packing, oxytocin, misoprostol, and carboprost. Her pulse rate is now 120/min, respirations are 20/min, and blood pressure is 90/70 mm Hg. Her hemoglobin is 8 g/dL, hematocrit is 24%, platelet count is 120,000 mm3, prothrombin time is 11 seconds, and partial thromboplastin time is 30 seconds. Mass transfusion protocol is activated and a B-Lynch uterine compression suture is placed to control her bleeding. Which of the following is the mostly likely cause of her postpartum complication?
- A. Adherent placenta to myometrium
- B. Uterine inversion
- C. Infection of the endometrial lining of the uterus
- D. Uterine rupture
- E. Lack of uterine muscle contraction (Correct Answer)
Prior cesarean delivery management Explanation: ***Lack of uterine muscle contraction***
- The presentation of a **soft uterus** on palpation and continued severe bleeding despite fundal massage and uterotonics (**oxytocin, misoprostol, carboprost**) is highly indicative of **uterine atony**, which is a lack of effective uterine muscle contraction.
- Uterine atony is the most common cause of **postpartum hemorrhage**, and risk factors include **macrosomia** (due to gestational diabetes), **multiparity**, and a prolonged labor or rapid delivery, though the latter two are less clear here.
*Adherent placenta to myometrium*
- While a history of prior C-section and **macrosomia** (due to gestational diabetes) could increase the risk of an **abnormally adherent placenta** (accreta, increta, percreta), the description notes **complete removal of the placenta**.
- If the placenta were morbidly adherent and not completely removed, bleeding would likely stem from retained placental tissue, and this would typically be explicitly noted or suspected due to difficulty with manual removal.
*Uterine inversion*
- **Uterine inversion** involves the uterus turning inside out, which would present with a **mass protruding from the vagina** or a visible inversion of the fundus upon examination, along with sudden onset of severe pain and shock.
- The description of a **soft uterus** and an absence of a physical description of uterine inversion makes this diagnosis less likely.
*Infection of the endometrial lining of the uterus*
- **Endometritis** (infection of the endometrial lining) typically presents with fever, foul-smelling lochia, uterine tenderness, and prolonged postpartum bleeding, usually occurring a few days postpartum rather than immediately following delivery.
- The acute, massive hemorrhage immediately following delivery, coupled with a normal initial temperature, does not align with the typical presentation of endometritis.
*Uterine rupture*
- **Uterine rupture** is a serious complication, especially with a history of prior C-section, but it typically presents with **sudden severe abdominal pain**, fetal heart rate abnormalities (if it occurs before delivery), and **hemodynamic instability**, often with cessation of contractions.
- While the patient is hemodynamically unstable, the primary issue described is heavy uterine bleeding with a soft uterus, and no mention of severe abdominal pain or clear signs of rupture during the C-section make uterine atony a more direct explanation for the described symptoms.
Prior cesarean delivery management US Medical PG Question 4: A 32-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the emergency department because of vaginal bleeding for the past hour. The patient reports that she felt contractions prior to the onset of the bleeding, but the contractions stopped after the bleeding started. She also has severe abdominal pain. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her pulse is 110/min, respirations are 17/min, and blood pressure is 90/60 mm Hg. Examination shows diffuse abdominal tenderness with no rebound or guarding; no contractions are felt. The fetal heart rate shows recurrent variable decelerations. Which of the following is the most likely diagnosis?
- A. Uterine inertia
- B. Amniotic fluid embolism
- C. Uterine rupture (Correct Answer)
- D. Vasa previa
- E. Abruptio placentae
Prior cesarean delivery management Explanation: ***Uterine rupture***
- The patient's history of a prior **cesarean section**, sudden onset of **vaginal bleeding** and **severe abdominal pain**, resolution of contractions, and signs of **hypovolemic shock** (tachycardia, hypotension) coupled with fetal distress (variable decelerations) are highly indicative of uterine rupture.
- Diffuse abdominal tenderness without rebound or guarding, and no palpable contractions, are also consistent with rupture.
*Uterine inertia*
- This condition is characterized by **weak or uncoordinated uterine contractions** leading to prolonged labor, but it does not typically present with acute vaginal bleeding, sudden severe abdominal pain, or hypovolemic shock.
- Fetal distress in uterine inertia would more likely be due to prolonged labor rather than acute compromise following a sudden event.
*Amniotic fluid embolism*
- This is a rare, life-threatening obstetric emergency characterized by sudden **cardiovascular collapse, respiratory distress**, and **coagulopathy**, often occurring during labor or immediately postpartum.
- While it can cause fetal distress, vaginal bleeding and severe abdominal pain are not primary presenting symptoms.
*Vasa previa*
- Characterized by **painless vaginal bleeding** when fetal vessels within the membranes cross the internal cervical os, making them vulnerable to rupture during cervical dilation or amniotomy.
- The bleeding is typically fetal blood, and fetal distress occurs rapidly, but the mother would not experience severe abdominal pain or signs of hypovolemic shock unless the bleeding is substantial and prolonged.
*Abruptio placentae*
- This involves the **premature separation of the placenta**, causing painful vaginal bleeding, uterine tenderness, and frequent, strong contractions.
- While it can cause hypovolemic shock and fetal distress, the description of contractions stopping after bleeding started, along with a previous C-section scar, points more specifically to uterine rupture rather than an abruption.
Prior cesarean delivery management US Medical PG Question 5: A 34-year-old G5P5 woman gave birth to a healthy infant 30 minutes ago by vacuum-assisted vaginal delivery and is now experiencing vaginal bleeding. The placenta was delivered spontaneously and was intact upon examination. The infant weighed 5.2 kg and had Apgar scores of 8 and 9. No perineal tear or intentional episiotomy occurred. The patient has type 1 diabetes. She had good glycemic control throughout her pregnancy. She took a prenatal vitamin daily. Blood pressure is 135/72 mmHg, pulse is 102/min, and respirations are 18/min. Upon physical examination, the uterine fundus is soft and palpated 4 cm above the umbilicus. There are 3-cm blood clots on the patient’s bed pad. Which of the following is the next best step in management for the patient’s bleeding?
- A. Administer misoprostol
- B. Manually remove retained placental fragments
- C. Perform uterine massage and administer oxytocin (Correct Answer)
- D. Perform uterine artery embolization
- E. Perform hysterectomy
Prior cesarean delivery management Explanation: ***Perform uterine massage and administer oxytocin***
- The patient's presentation of a **soft, boggy uterus** palpated 4 cm above the umbilicus after delivery, along with significant vaginal bleeding and clots, is highly indicative of **uterine atony**.
- **Uterine massage** and administration of **oxytocin** are the first-line interventions to stimulate uterine contractions and reduce bleeding by compressing placental site blood vessels.
*Administer misoprostol*
- **Misoprostol** is a prostaglandin analog that can be used for uterine atony when oxytocin is insufficient or contraindicated, but it is not the *first-line* treatment.
- Its onset of action may be slower than immediate uterine massage and IV oxytocin, which are preferred for initial management of acute uterine atony.
*Manually remove retained placental fragments*
- The question states that the **placenta was delivered spontaneously and was intact upon examination**, which makes retained placental fragments less likely as the primary cause of bleeding.
- While retained fragments can cause postpartum hemorrhage, the boggy uterus points more strongly to atony, and manual removal is indicated *after* confirming retained placental tissue.
*Perform uterine artery embolization*
- **Uterine artery embolization** is an interventional radiology procedure typically reserved for cases of postpartum hemorrhage that are refractory to conventional medical and surgical management.
- It is an invasive procedure and not the appropriate *next best step* for initial management of suspected uterine atony.
*Perform hysterectomy*
- **Hysterectomy** is a last-resort, life-saving measure for intractable postpartum hemorrhage when all other medical and surgical options have failed.
- It is a highly invasive and irreversible procedure, certainly not the *next best step* in a patient who has just begun to bleed.
Prior cesarean delivery management US Medical PG Question 6: A 33-year-old woman, gravida 2, para 1, at 26 weeks' gestation comes to the emergency department because of frequent contractions. The contractions are 40 seconds each, occurring every 2 minutes, and increasing in intensity. Her first child was delivered by lower segment transverse cesarean section because of a nonreassuring fetal heart rate. Her current medications include folic acid and a multivitamin. Her temperature is 36.9°C (98.4°F), heart rate is 88/min, and blood pressure is 126/76 mm Hg. Contractions are felt on the abdomen. There is clear fluid in the vulva and the introitus. The cervix is dilated to 5 cm, 70% effaced, and station of the head is -2. A fetal ultrasound shows polyhydramnios, a median cleft lip, and fused thalami. The corpus callosum, 3rd ventricle, and lateral ventricles are absent. The spine shows no abnormalities and there is a four chamber heart. Which of the following is the most appropriate next step in management?
- A. Initiate misoprostol therapy
- B. Allow vaginal delivery (Correct Answer)
- C. Perform dilation and evacuation
- D. Initiate nifedipine therapy
- E. Perform cesarean delivery
Prior cesarean delivery management Explanation: ***Allow vaginal delivery***
- The presence of severe fetal anomalies, including **holoprosencephaly** (median cleft lip, fused thalami, absent corpus callosum, 3rd and lateral ventricles), indicates that the fetus is **incompatible with life**.
- Given the prognosis, the most appropriate and safest approach for the mother is to **allow vaginal delivery**, as there is no benefit to delaying delivery or attempting a surgical intervention that might pose more risks to the mother.
*Initiate misoprostol therapy*
- **Misoprostol** is a prostaglandin analog used to induce labor or abortion, particularly in cases of uterine atony or to ripen the cervix.
- While it aids in cervical ripening and uterine contractions, the cervix is already 5 cm dilated and 70% effaced, indicating a **rapidly progressing labor** not requiring additional induction.
*Perform dilation and evacuation*
- **Dilation and evacuation (D&E)** is typically performed in the second trimester for fetal demise or termination of pregnancy, usually before 24 weeks' gestation.
- At 26 weeks' gestation with advanced labor and significant cervical dilation, D&E is a **high-risk procedure** for the mother and less appropriate than vaginal delivery.
*Initiate nifedipine therapy*
- **Nifedipine is a tocolytic** used to suppress preterm labor by relaxing the uterine muscles.
- Given the **lethal fetal anomalies** and the advanced stage of labor (5 cm dilated, 70% effaced, intense contractions), stopping labor would only prolong a non-viable pregnancy and increase maternal risk.
*Perform cesarean delivery*
- **Cesarean delivery** would expose the mother to surgical risks (e.g., infection, hemorrhage, future pregnancy complications) without any benefit to the fetus, who has anomalies **incompatible with survival**.
- A previous cesarean section does not preclude a vaginal delivery in this context, especially when **fetal viability is not a concern**.
Prior cesarean delivery management US Medical PG Question 7: A 30-year-old woman, gravida 2, para 1, at 38 weeks' gestation comes to the hospital for regular, painful contractions that have been increasing in frequency. Her pregnancy has been complicated by gestational diabetes treated with insulin. Pelvic examination shows the cervix is 50% effaced and 4 cm dilated; the vertex is at -1 station. Ultrasonography shows no abnormalities. A tocometer and Doppler fetal heart monitor are placed on the patient's abdomen. The fetal heart rate monitoring strip shows a baseline heart rate of 145/min with a variability of ≥ 15/min. Within a 20-minute recording, there are 7 uterine contractions, 4 accelerations, and 3 decelerations that have a nadir occurring within half a minute. The decelerations occur at differing intervals relative to the contractions. Which of the following is the most appropriate next step in the management of this patient?
- A. Vibroacoustic stimulation
- B. Routine monitoring (Correct Answer)
- C. Administer tocolytics
- D. Emergent cesarean delivery
- E. Placement of fetal scalp electrode
Prior cesarean delivery management Explanation: ***Routine monitoring***
- The presented FHR tracing exhibits a **normal baseline rate** (145/min), **moderate variability** (≥15/min), and the presence of **accelerations**, indicating a reassuring fetal status.
- The described decelerations are **variable decelerations** due to their sudden onset, nadir within 30 seconds, and variable relationship to contractions, which are generally benign unless prolonged, deep, or repetitive. Given the otherwise reassuring status, continued routine monitoring is appropriate.
*Vibroacoustic stimulation*
- This intervention is used to elicit **fetal accelerations** or movement during non-stress tests (NSTs) when the fetus is quiet or shows a non-reactive pattern.
- In this case, the fetus is already showing **accelerations** and moderate variability, so stimulation is not needed to assess fetal well-being.
*Administer tocolytics*
- **Tocolytics** are used to stop or slow down labor, typically in cases of preterm labor or uterine tachysystole causing fetal distress.
- This patient is at **38 weeks' gestation** and in active labor, and there are no signs of fetal distress warranting the cessation of contractions.
*Emergent cesarean delivery*
- **Emergent cesarean delivery** is indicated for acute fetal distress, such as prolonged decelerations, significant bradycardia, or absent variability in conjunction with other concerning FHR patterns.
- The FHR tracing described is largely reassuring with moderate variability and accelerations, and the variable decelerations are not indicative of immediate threat, making emergent delivery unnecessary.
*Placement of fetal scalp electrode*
- A **fetal scalp electrode** provides a more accurate and continuous measure of the FHR, often used when external monitoring is difficult or when there are concerns about the reliability of the tracing.
- While it can be useful in some situations, the current tracing is **interpretable as reassuring**, making invasive monitoring currently unnecessary.
Prior cesarean delivery management US Medical PG Question 8: A 24-year-old primigravid woman at 38 weeks' gestation comes to the physician for a prenatal visit. At the last two prenatal visits, transabdominal ultrasound showed the fetus in breech presentation. She has no medical conditions and only takes prenatal vitamins. Her pulse is 95/min, respirations are 16/min, and blood pressure is 130/76 mm Hg. The abdomen is soft and nontender; no contractions are felt. Pelvic examination shows a closed cervical os and a uterus consistent with 38 weeks' gestation. The fetal rate tracing shows a baseline heart rate of 152/min and 2 accelerations over 10 minutes. Repeat ultrasound today shows a persistent breech presentation. The patient states that she would like to attempt a vaginal delivery. Which of the following is the most appropriate next step in management?
- A. Offer internal podalic version
- B. Offer external cephalic version (Correct Answer)
- C. Repeat ultrasound in one week
- D. Observe until spontaneous labor
- E. Recommend cesarean section
Prior cesarean delivery management Explanation: ***Offer external cephalic version***
- External cephalic version (ECV) is the most appropriate next step for a **term pregnancy with persistent breech presentation** in a woman who desires a vaginal delivery, given there are no contraindications.
- It is a procedure performed to manually turn the fetus from a breech to a cephalic presentation, potentially allowing for a **vaginal birth** and avoiding a cesarean section.
*Offer internal podalic version*
- Internal podalic version is a procedure primarily used for the **second twin during a vaginal delivery** or in specific cases of significant fetal distress during labor, not as an initial attempt for a singleton breech presentation at term.
- It involves inserting a hand into the uterus to grasp the fetal feet and turn the fetus, carrying **higher risks** than ECV.
*Repeat ultrasound in one week*
- Repeating an ultrasound in one week is unlikely to change the fetal presentation as the woman is already at **38 weeks' gestation**, and spontaneous version is rare at this stage.
- This delay would **prolong the breech presentation** and reduce the window of opportunity for a successful ECV.
*Observe until spontaneous labor*
- Observing until spontaneous labor would mean the baby would likely remain in a **breech presentation**, necessitating either a planned cesarean section or a complicated breech vaginal delivery with increased risks.
- Allowing labor to begin with a breech presentation **limits options** and increases the likelihood of a C-section or potential complications.
*Recommend cesarean section*
- While a cesarean section is an option for breech presentation, it is generally reserved for cases where ECV is unsuccessful or contraindicated, or if the woman prefers it.
- Given the patient's desire to attempt a vaginal delivery and no contraindications, ECV should be **offered first** before recommending a C-section.
Prior cesarean delivery management US Medical PG Question 9: A 23-year-old primigravid woman comes to the physician at 36 weeks' gestation for her first prenatal visit. She confirmed the pregnancy with a home urine pregnancy kit a few months ago but has not yet followed up with a physician. She takes no medications. Vital signs are within normal limits. Pelvic examination shows a uterus consistent in size with a 36-week gestation. Laboratory studies show:
Hemoglobin 10.6 g/dL
Serum
Glucose 88 mg/dL
Hepatitis B surface antigen negative
Hepatitis C antibody negative
HIV antibody positive
HIV load 11,000 copies/mL (N < 1000 copies/mL)
Ultrasonography shows an intrauterine fetus consistent in size with a 36-week gestation. Which of the following is the most appropriate next step in management of this patient?
- A. Intrapartum zidovudine and vaginal delivery when labor occurs
- B. Intrapartum zidovudine and cesarean delivery at 38 weeks' gestation
- C. Start cART and prepare for vaginal delivery at 38 weeks' gestation
- D. Conduct cesarean delivery immediately
- E. Start cART and schedule cesarean delivery at 38 weeks' gestation (Correct Answer)
Prior cesarean delivery management Explanation: ***Start cART and schedule cesarean delivery at 38 weeks' gestation***
- This patient presents at 36 weeks with a **newly diagnosed HIV infection** and a **viral load of 11,000 copies/mL**, which is considered high. Starting **combination antiretroviral therapy (cART)** immediately is crucial to reduce the viral load and the risk of **mother-to-child transmission (MTCT)**.
- For patients with **HIV viral loads > 1,000 copies/mL** near term, a **scheduled cesarean delivery at 38 weeks** is recommended to minimize fetal exposure to maternal blood and secretions during labor, further reducing the risk of MTCT.
*Intrapartum zidovudine and vaginal delivery when labor occurs*
- This approach is appropriate for HIV-positive mothers with a **low viral load (< 1,000 copies/mL)** at or near delivery, as a scheduled cesarean section would not significantly further reduce the risk of transmission.
- Given the patient's **high viral load (11,000 copies/mL)**, **only intrapartum zidovudine** would be insufficient to adequately reduce the risk of MTCT during a vaginal delivery.
*Intrapartum zidovudine and cesarean delivery at 38 weeks' gestation*
- While a **scheduled cesarean delivery at 38 weeks** is indicated for a high viral load, simply administering **intrapartum zidovudine without prior cART** misses the opportunity to significantly reduce viral load before delivery.
- Starting **cART immediately** offers the best chance to lower viral load and optimize outcomes for both mother and child, which is superior to only intrapartum prophylaxis.
*Start cART and prepare for vaginal delivery at 38 weeks' gestation*
- Starting **cART is essential**, but preparing for a vaginal delivery with a **viral load of 11,000 copies/mL** at 36 weeks is inappropriate.
- A **high viral load** necessitates a ** scheduled cesarean delivery** to minimize the risk of MTCT, regardless of cART initiation at this late stage.
*Conduct cesarean delivery immediately*
- While immediate action is needed, an **emergency cesarean delivery** is not indicated at 36 weeks unless there are other obstetric complications or rapid deterioration.
- The primary goal is to **reduce viral load through cART** and then perform a **scheduled cesarean at 38 weeks**, balancing safety for both mother and fetus with the greatest reduction in HIV transmission risk.
Prior cesarean delivery management US Medical PG Question 10: A 36-year-old woman, gravida 1, para 1, has back pain and numbness in her lower extremities after an emergency cesarean delivery of a healthy 3856-g (8-lb, 8-oz) newborn male. She had a placental abruption and lost approximately 2000 ml of blood. During the procedure, she received two units of packed red blood cells and intravenous fluids. She has no history of serious illness and takes no medications. She is sexually active with one male partner, and they use condoms inconsistently. She is alert and oriented to person, place, and time. Her temperature is 37.2°C (98.9°F), pulse is 90/min, respirations are 15/min, and blood pressure is 94/58 mm Hg. Examination shows decreased sensation to temperature and pinprick below her waist and 0/5 muscle strength in her lower extremities. She feels the vibrations of a tuning fork placed on both of her great toes. Deep tendon reflexes are absent in the lower extremities and 2+ in the upper extremities. Which of the following is the most likely diagnosis?
- A. Posterior spinal artery syndrome
- B. Brown-Séquard syndrome
- C. Anterior spinal artery syndrome (Correct Answer)
- D. Guillain-Barré Syndrome
- E. Tabes dorsalis
Prior cesarean delivery management Explanation: ***Anterior spinal artery syndrome***
- This syndrome is characterized by the sudden onset of **bilateral motor paralysis** below the level of the lesion, accompanied by a dissociated sensory loss (**loss of pain and temperature sensation**) while **proprioception and vibratory sensation are preserved**.
- The patient's history of **significant blood loss** and hypotension during delivery makes her susceptible to spinal cord ischemia, particularly in the anterior spinal artery territory, which supplies the anterior two-thirds of the spinal cord.
*Posterior spinal artery syndrome*
- This syndrome primarily affects the **dorsal columns**, leading to a loss of **proprioception and vibratory sensation**, with preservation of motor function and pain/temperature sensation.
- The patient's preserved vibratory sensation and significant motor deficits rule out posterior spinal artery syndrome.
*Brown-Séquard syndrome*
- This syndrome results from **hemitransverse lesion of the spinal cord**, causing **ipsilateral motor paralysis** and loss of proprioception/vibration below the lesion, and **contralateral loss of pain and temperature sensation**.
- The patient's **bilateral motor and sensory deficits** are inconsistent with the unilateral presentation of Brown-Séquard syndrome.
*Guillain-Barré Syndrome*
- GBS typically presents as an **ascending paralysis** with **areflexia**, but sensory loss is usually stocking-glove distribution and often involves proprioception, and it is a **peripheral neuropathy** not a spinal cord infarction.
- The acute, localized nature of the sensory and motor loss below the waist, along with preserved vibratory sensation, differentiates it from the more diffuse presentation of GBS.
*Tabes dorsalis*
- This is a late manifestation of **syphilis** affecting the **dorsal columns** and dorsal roots, characterized by ataxia, lancinating pains, and loss of proprioception and vibration sense.
- The acute onset of symptoms following a hypotensive episode, along with motor paralysis and preserved vibratory sensation, does not fit the chronic, dorsal column pathology of tabes dorsalis.
More Prior cesarean delivery management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.