Pregestational diabetes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pregestational diabetes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pregestational diabetes US Medical PG Question 1: A 31-year-old G1P0000 presents to her obstetrician for her first prenatal visit after having a positive home pregnancy test one week ago. She states that her last menstrual period was 8 weeks ago. The patient has a past medical history of type I diabetes mellitus since childhood and is on insulin. Her hemoglobin A1c two weeks ago was 13.7%. At that time, she was also found to have microalbuminuria on routine urinalysis, and her primary care provider prescribed lisinopril but the patient has not yet started taking it. The patient’s brother is autistic, but family history is otherwise unremarkable. At this visit, her temperature is 98.6°F (37.0°C), blood pressure is 124/81 mmHg, pulse is 75/min, and respirations are 14/min. Exam is unremarkable. This fetus is at increased risk for which of the following?
- A. Post-term delivery
- B. Oligohydramnios
- C. Neural tube defect (Correct Answer)
- D. Aneuploidy
- E. Neonatal hyperglycemia
Pregestational diabetes Explanation: ***Neural tube defect***
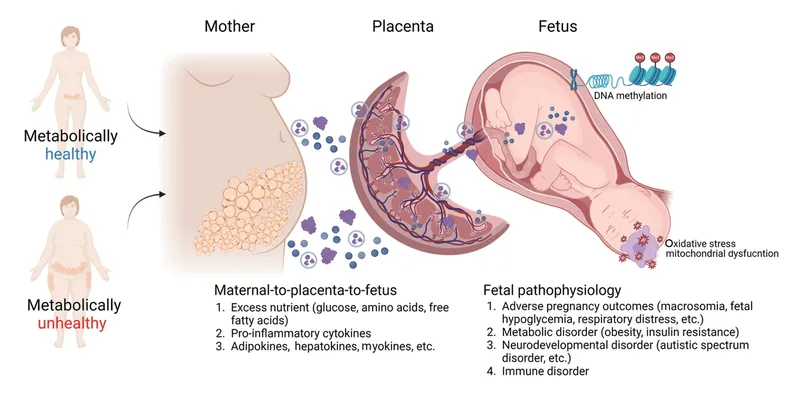
- The patient's **poorly controlled type 1 diabetes mellitus** is evidenced by her **HbA1c of 13.7%**. Uncontrolled maternal hyperglycemia during organogenesis significantly increases the risk for fetal malformations, including neural tube defects due to impaired folate metabolism.
- This risk is highest when hyperglycemia occurs during the first 8 weeks of gestation, a period crucial for neural tube closure, which aligns with this patient's presentation at 8 weeks' gestation.
*Post-term delivery*
- **Uncontrolled maternal diabetes** is typically associated with **macrosomia and polyhydramnios**, which can lead to complications such as **shoulder dystocia, premature rupture of membranes (PROM)**, and often precipitates **earlier induction of labor** rather than post-term delivery.
- While exact delivery timing can vary, the direct causal link between uncontrolled diabetes and post-term delivery is not primary; rather, such pregnancies are often managed with earlier interventions.
*Oligohydramnios*
- Poorly controlled maternal diabetes, particularly type 1, is generally associated with **polyhydramnios** due to fetal polyuria caused by hyperglycemia, not oligohydramnios.
- **Oligohydramnios** can be associated with severe **placental insufficiency**, prolonged rupture of membranes, or fetal renal agenesis, none of which are directly indicated by uncontrolled maternal diabetes alone.
*Aneuploidy*
- The primary risk factor for **aneuploidy** (e.g., Down syndrome) is **advanced maternal age**, which is not present in this 31-year-old patient.
- **Maternal diabetes** itself is not a direct risk factor for aneuploidy; genetic factors related to nondisjunction are the main cause.
*Neonatal hyperglycemia*
- Maternal hyperglycemia leads to fetal hyperglycemia, causing **fetal hyperinsulinemia**. After birth, the neonate's elevated insulin levels, in the absence of maternal glucose supply, result in **neonatal hypoglycemia**, not hyperglycemia.
- **Neonatal hyperglycemia** is rare and usually associated with specific genetic defects or administration of excessive glucose postnatally, not maternal diabetes.
Pregestational diabetes US Medical PG Question 2: A 21-year-old gravida 1, para 0 woman presents to the family medicine clinic for her first prenatal appointment. She states that she has been taking folic acid supplements daily as directed by her mother. She smokes a few cigarettes a day and has done so for the last 5 years. Pediatric records indicate the patient is measles, mumps, and rubella non-immune. Her heart rate is 78/min, respiratory rate is 14/min, temperature is 36.5°C (97.7°F), and blood pressure is 112/70 mm Hg. Her calculated BMI is approximately 26 kg/m2. Her heart is without murmurs and lung sounds are clear bilaterally. Standard prenatal testing is ordered. Which of the following is the next best step for this patient’s prenatal care?
- A. MMR vaccine during pregnancy
- B. Serology, then vaccine postpartum
- C. MMR vaccine postpartum (Correct Answer)
- D. Serology, then vaccine during pregnancy
- E. MMR vaccine and immune globulin postpartum
Pregestational diabetes Explanation: ***MMR vaccine postpartum***
- The **MMR vaccine is a live attenuated vaccine** and therefore **contraindicated during pregnancy** due to the theoretical risk of fetal infection and congenital rubella syndrome.
- Vaccinating postpartum ensures the mother develops immunity without any risk to the current pregnancy, and it's also safe for breastfeeding.
*MMR vaccine during pregnancy*
- Administering a **live attenuated vaccine** like MMR during pregnancy is generally avoided due to the **theoretical risk of teratogenicity**.
- While documented cases of congenital rubella syndrome from the vaccine are rare, the risk is not zero, making it unsafe for routine administration during gestation.
*Serology, then vaccine postpartum*
- The patient's records already indicate she is **MMR non-immune**, rendering additional serology unnecessary to determine her immune status.
- The crucial step is the timing of vaccination, which should be postpartum, regardless of repeat serology findings.
*Serology, then vaccine during pregnancy*
- As explained, **MMR vaccination is contraindicated during pregnancy**, making immediate vaccination during gestation an inappropriate course of action.
- While serology can confirm non-immunity, it doesn't change the recommendation to delay vaccination until after delivery.
*MMR vaccine and immune globulin postpartum*
- **Immune globulin** is typically given for passive immunity following exposure to certain diseases if the patient is non-immune (e.g., RhoGAM for Rh-negative mothers).
- It is **not routinely administered with the MMR vaccine postpartum** for healthy, non-immune individuals, as the vaccine itself stimulates active immunity.
Pregestational diabetes US Medical PG Question 3: A 31-year-old G1P0 woman at 26 weeks gestation presents to the clinic for evaluation of an abnormal glucose tolerance test. She denies any symptoms, but states that she was given 50 g of oral glucose 1 week earlier and demonstrated a subsequent venous plasma glucose level of 156 mg/dL 1 hour later. The vital signs are: blood pressure, 112/78 mm Hg; pulse, 81/min; and respiratory rate, 16/min. Physical examination is within normal limits. Which of the following is the most appropriate next step in management?
- A. Administer an oral, 3-hour 100 g glucose dose (Correct Answer)
- B. Advise the patient to follow an American Diabetic Association diet plan
- C. Repeat the 50 g oral glucose challenge
- D. Begin insulin treatment
- E. Order a fetal ultrasound examination
Pregestational diabetes Explanation: ***Administer an oral, 3-hour 100 g glucose dose***
- This patient failed the initial **50 g, 1-hour glucose challenge test** (screen) because her plasma glucose was 156 mg/dL, which is above the typical threshold of 130-140 mg/dL.
- The next appropriate step for a failed screening test is to perform a **diagnostic 3-hour, 100 g oral glucose tolerance test (OGTT)** to confirm or rule out gestational diabetes.
*Advise the patient to follow an American Diabetic Association diet plan*
- While lifestyle modifications are important for managing gestational diabetes, this step is premature as the diagnosis has not yet been confirmed by the **diagnostic 3-hour OGTT**.
- Diet modification is part of the treatment for confirmed gestational diabetes, not the next diagnostic step.
*Repeat the 50 g oral glucose challenge*
- Repeating the screening test is not appropriate after a positive result; a diagnostic test is required to confirm the condition.
- The **50 g challenge** is a screening test with a high sensitivity but lower specificity, thus requiring a follow-up diagnostic test.
*Begin insulin treatment*
- **Insulin treatment** is reserved for patients officially diagnosed with gestational diabetes whose blood glucose levels cannot be controlled with diet and exercise alone.
- Prescribing insulin without a confirmed diagnosis is inappropriate and potentially harmful.
*Order a fetal ultrasound examination*
- A fetal ultrasound is used to monitor for complications of gestational diabetes like **macrosomia**, but it is not the next step in diagnosing the condition.
- While important for fetal surveillance in confirmed cases, it does not aid in the initial diagnosis of gestational diabetes itself.
Pregestational diabetes US Medical PG Question 4: A 23-year-old G1P0 primigravid woman at 28 weeks estimated gestational age presents for a prenatal checkup. She says she has been having occasional headaches but is otherwise fine. The patient says she feels regular fetal movements and mild abdominal pain at times. Her past medical history is unremarkable. Current medications are a prenatal multivitamin and the occasional acetaminophen. Her blood pressure is 148/110 mm Hg today. On her last visit at 24 weeks of gestation, her blood pressure was 146/96 mm Hg. On physical exam, the fundus measures 28 cm above the pubic symphysis. Laboratory findings are significant for the following:
Serum Glucose (fasting) 88 mg/dL
Sodium 142 mEq/L
Potassium 3.9 mEq/L
Chloride 101 mEq/L
Serum Creatinine 0.9 mg/dL
Blood Urea Nitrogen 10 mg/dL
Alanine aminotransferase (ALT) 18 U/L
Aspartate aminotransferase (AST) 16 U/L
Mean Corpuscular Volume (MCV) 85 fL
Leukocyte count 4,200/mm3
Reticulocyte count 1%
Erythrocyte count 5.1 million/mm3
Platelet count 95,000mm3
Urinalysis show:
Proteins 2+
Glucose negative
Ketones negative
Leucocytes negative
Nitrites negative
Red Blood Cells (RBCs) negative
Casts negative
Which of the following medications would be the next best step in the treatment of this patient?
- A. Magnesium sulfate (Correct Answer)
- B. Phenobarbital
- C. Valproic acid
- D. Ethosuximide
- E. Diazepam
Pregestational diabetes Explanation: ***Magnesium sulfate***
- The patient presents with **gestational hypertension**, **proteinuria (2+)**, **thrombocytopenia (platelets 95,000/mm³)**, and **headaches at 28 weeks gestation**, indicating severe preeclampsia.
- **Magnesium sulfate** is the drug of choice for the prevention and treatment of **eclampsia-related seizures** in women with severe preeclampsia.
*Phenobarbital*
- **Phenobarbital** is an anticonvulsant but is generally reserved for refractory seizures or in situations where magnesium sulfate is contraindicated.
- It has a risk of **fetal respiratory depression** and neonatal withdrawal symptoms if used close to delivery.
*Valproic acid*
- **Valproic acid** is an anticonvulsant that carries a significant risk of **teratogenicity**, including **neural tube defects**, especially if used in early pregnancy.
- It is not the preferred agent for acute seizure prophylaxis in preeclampsia.
*Ethosuximide*
- **Ethosuximide** is primarily used for **absence seizures** and has no role in the management or prevention of seizures in preeclampsia.
- It would not address the underlying pathology or provide seizure prophylaxis in this patient.
*Diazepam*
- While **diazepam** can be used to abort an active seizure, it is not recommended for routine seizure prophylaxis in preeclampsia due to its **sedative effects** and potential for **fetal depression**.
- Magnesium sulfate is more effective and has a better safety profile for seizure prevention in preeclampsia.
Pregestational diabetes US Medical PG Question 5: A 25-year-old woman presents to the emergency department with intermittent uterine contractions. She is 39 weeks pregnant and experienced a deluge of fluid between her legs while she was grocery shopping. She now complains of painful contractions. She is transferred to the labor and delivery floor and a healthy male baby is delivered. He has a ruddy complexion and is crying audibly. Laboratory values demonstrate a hemoglobin of 22 g/dL and electrolytes that are within normal limits. Which of the following is the best description for the cause of this neonate's presentation?
- A. Renal abnormality
- B. Maternal hyperglycemia during the pregnancy
- C. Healthy infant (Correct Answer)
- D. Post-term infant
- E. Dehydration
Pregestational diabetes Explanation: ***Healthy infant***
- A **ruddy complexion** and a **hemoglobin (Hb) of 22 g/dL** are normal findings in a **healthy neonate**.
- Polycythemia with a ruddy complexion is common and often benign in newborns, a normal Hb for a term neonate is between **14-24 g/dL**.
*Renal abnormality*
- Renal abnormalities, such as **renal artery stenosis**, can cause polycythemia in adults due to increased erythropoietin secretion.
- However, there are no other symptoms to suggest renal pathology, making a healthy infant a more likely diagnosis.
*Maternal hyperglycemia during the pregnancy*
- **Maternal diabetes** can cause **neonatal polycythemia** due to increased oxygen demands.
- However, the question specifies normal electrolytes and no other indicators of maternal diabetes, such as macrosomia or hypoglycemia in the neonate.
*Post-term infant*
- **Post-term infants** (born after 42 weeks) can be at increased risk for **polycythemia** due to placental insufficiency.
- This infant is described as 39 weeks **gestation**, which is a term delivery, ruling out this option.
*Dehydration*
- **Dehydration** can lead to **hemoconcentration** and an increased hemoglobin level, which presents in the same way as polycythemia.
- However, the description of a **ruddy complexion** is more indicative of true polycythemia, and neonatal dehydration would be accompanied by other signs like poor feeding, lethargy, or decreased urine output, none of which are mentioned.
Pregestational diabetes US Medical PG Question 6: A 27-year-old Hispanic G2P1 presents for a routine antepartum visit at 26 weeks gestation. She has no complaints. The vital signs are normal, the physical examination is within normal limits, and the gynecologic examination corresponds to 25 weeks gestation. The oral glucose tolerance test (OGTT) with a 75-g glucose load is significant for a glucose level of 177 mg/dL at 1 hour and 167 mg/dL at 2 hour. The fasting blood glucose level is 138 mg/dL (7.7 mmol/L), and the HbA1c is 7%. Which of the following represents the proper initial management?
- A. Sitagliptin
- B. Dietary and lifestyle modification
- C. Metformin
- D. Glyburide
- E. Insulin (Correct Answer)
Pregestational diabetes Explanation: **Insulin**
- The patient's **fasting glucose of 138 mg/dL** and **HbA1c of 7%** indicate pre-existing **Type 2 Diabetes Mellitus**, not just gestational diabetes. Both values exceed the diagnostic thresholds for overt diabetes in pregnancy.
- **Insulin** is the preferred initial pharmacologic treatment for **overt diabetes in pregnancy** because it does not cross the placenta, ensuring fetal safety, and is highly effective in controlling maternal glucose levels.
*Sitagliptin*
- **Sitagliptin** is a **DPP-4 inhibitor** and is not recommended during pregnancy due to limited safety data and the availability of safer alternatives.
- Oral hypoglycemic agents are generally avoided as first-line therapy for established diabetes in pregnancy due to potential for placental transfer and adverse fetal effects.
*Dietary and lifestyle modification*
- While crucial, **dietary and lifestyle modification** alone are insufficient for managing overt diabetes with such high fasting glucose and HbA1c levels.
- These measures are usually the first step for **gestational diabetes**, but a patient with overt diabetes requires immediate pharmacologic intervention to prevent complications.
*Metformin*
- **Metformin** can be used in pregnancy but is primarily considered for **gestational diabetes** or as an alternative to insulin if the patient has milder hyperglycemia, or if insulin is poorly tolerated.
- Given the patient's significantly elevated fasting glucose and HbA1c, **insulin** is a more effective and immediate treatment to achieve glycemic control and reduce risks.
*Glyburide*
- **Glyburide** is an **oral sulfonylurea** that can cross the placenta, leading to potential fetal hyperinsulinemia and neonatal hypoglycemia.
- Its use in pregnancy is generally discouraged due to these risks, making **insulin** a safer and more appropriate choice.
Pregestational diabetes US Medical PG Question 7: A newborn whose mother had uncontrolled diabetes mellitus during pregnancy is likely to have which of the following findings?
- A. Amyloid deposits in pancreatic islets
- B. Atrophy of pancreatic islets cells
- C. Hyperglycemia
- D. Ketoacidosis
- E. Hypoglycemia (Correct Answer)
Pregestational diabetes Explanation: ***Hypoglycemia***
- Uncontrolled maternal diabetes leads to **fetal hyperglycemia**, causing the fetal pancreas to produce **excessive insulin** (fetal hyperinsulinism) to compensate.
- After birth, the maternal glucose supply is cut off, but the newborn's pancreas continues to overproduce insulin, leading to **rapid drops in blood glucose** and severe hypoglycemia.
*Amyloid deposits in pancreatic islets*
- **Amyloid deposits** in pancreatic islets are characteristic of **Type 2 Diabetes Mellitus** in adults, typically not seen in newborns or as a direct consequence of maternal diabetes.
- This condition involves the accumulation of **islet amyloid polypeptide (IAPP)**, which is different from the physiological responses seen in infants of diabetic mothers.
*Atrophy of pancreatic islets cells*
- **Atrophy of pancreatic islet cells** is seen in late-stage **Type 1 Diabetes Mellitus** due to autoimmune destruction, not in infants of diabetic mothers, who typically have hypertrophied islets.
- In newborns of diabetic mothers, the pancreatic beta cells are usually **hypertrophic and hyperplastic** due to chronic glucose stimulation.
*Hyperglycemia*
- While the fetus experiences **hyperglycemia** in utero due to maternal diabetes, the newborn after birth typically develops **hypoglycemia** once the continuous maternal glucose supply is removed.
- The newborn's elevated insulin levels, in response to chronic fetal hyperglycemia, quickly deplete available glucose post-delivery, leading to low blood sugar.
*Ketoacidosis*
- **Ketoacidosis** occurs when the body produces high levels of **ketones** due to severe insulin deficiency and high glucose, which is primarily seen in **Type 1 Diabetes Mellitus** or severe stress states.
- Newborns of diabetic mothers are more prone to hypoglycemia due to **hyperinsulinism**, which inhibits ketogenesis, rather than ketoacidosis.
Pregestational diabetes US Medical PG Question 8: A 26-year-old woman comes to the physician for evaluation of nausea and fatigue. Her last menstrual period was 8 weeks ago. She has a history of bipolar disorder controlled by a drug known to sometimes cause hypothyroidism and nephrogenic diabetes insipidus. She does not smoke cigarettes or drink alcohol. A urine pregnancy test is positive. An ultrasound of the pelvis shows a viable intrauterine pregnancy. The fetus is most likely at increased risk for which of the following anomalies?
- A. Neural tube defects
- B. Aplasia cutis
- C. Hypoplastic or absent limbs
- D. Abnormal placentation
- E. Atrialization of the right ventricle (Correct Answer)
Pregestational diabetes Explanation: ***Atrialization of the right ventricle***
- The patient's history of **bipolar disorder** controlled by a drug causing **hypothyroidism** and **nephrogenic diabetes insipidus** strongly points to **lithium**.
- **Lithium** exposure during the first trimester of pregnancy is associated with an increased risk of **Ebstein's anomaly**, which involves the **apical displacement of the tricuspid valve** leaflets leading to **atrialization of the right ventricle**.
*Neural tube defects*
- These anomalies are often associated with deficiencies in **folic acid** or exposure to certain **antiepileptic drugs** like valproate, not lithium.
- While concerning, there is no information in the vignette to suggest these specific risk factors exist for this patient besides lithium use.
*Aplasia cutis*
- This is a localized absence of skin at birth, most commonly on the scalp. It is associated with gestational exposure to **methimazole** or **carbimazole**, used to treat hyperthyroidism, which is not indicated here.
- There is no direct link between lithium exposure and aplasia cutis.
*Hypoplastic or absent limbs*
- This type of anomaly is historically associated with exposure to **thalidomide** during early pregnancy.
- Lithium is not known to cause limb reduction defects.
*Abnormal placentation*
- Conditions like **placenta previa** or **placenta accreta** can result from previous uterine surgery (e.g., C-section) or advanced maternal age.
- Lithium use is not a recognized risk factor for abnormal placentation.
Pregestational diabetes US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Pregestational diabetes Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Pregestational diabetes US Medical PG Question 10: A 36-year-old primigravida presents to her obstetrician for antenatal care. She is at 24 weeks of gestation and does not have any current complaint except for occasional leg cramps. She does not smoke or drink alcohol. Family history is irrelevant. Her temperature is 36.9°C (98.42°F), blood pressure is 100/60 mm Hg, and pulse of 95/minute. Her body mass index is 21 kg/m² (46 pounds/m²). Physical examination reveals a palpable uterus above the umbilicus with no other abnormalities. Which of the following screening tests is suitable for this patient?
- A. Fasting and random glucose testing for gestational diabetes mellitus
- B. HbA1C for gestational diabetes mellitus
- C. Oral glucose tolerance test for gestational diabetes mellitus (Correct Answer)
- D. Complete blood count for iron deficiency anemia
- E. Wet mount microscopy of vaginal secretions for bacterial vaginosis
Pregestational diabetes Explanation: ***Oral glucose tolerance test for gestational diabetes mellitus***
- The **oral glucose tolerance test (OGTT)**, typically performed between **24 and 28 weeks of gestation**, is the gold standard for screening and diagnosing **gestational diabetes mellitus (GDM)**. This patient is at 24 weeks, making it the appropriate time for this screening.
- GDM, if undiagnosed and untreated, can lead to significant maternal and fetal complications, including **macrosomia**, **preeclampsia**, **neonatal hypoglycemia**, and **shoulder dystocia**.
*Fasting and random glucose testing for gestational diabetes mellitus*
- While **fasting** or **random glucose** values can indicate hyperglycemia, they are **not sensitive or specific enough** on their own to reliably screen for or diagnose GDM.
- A single elevated reading might prompt further testing, but it's not the primary or most suitable screening method.
*HbA1C for gestational diabetes mellitus*
- **HbA1c** reflects **average blood glucose levels over the past 2-3 months** and is primarily used for diagnosing and monitoring **pre-existing diabetes** or assessing glycemic control in non-pregnant individuals.
- Due to the **physiological changes in red blood cell turnover during pregnancy** and the acute onset nature of GDM, HbA1c is **not recommended** as a first-line screening tool for GDM.
*Complete blood count for iron deficiency anemia*
- While **complete blood count (CBC)** is a routine prenatal screening test to check for **anemia**, it is typically done earlier in pregnancy and again in the third trimester. There are no specific symptoms in this patient that strongly suggest immediate concern for anemia beyond routine.
- The question specifically asks for the "most suitable" screening test at this gestational age, and the **GDM screening** takes precedence given the timing.
*Wet mount microscopy of vaginal secretions for bacterial vaginosis*
- There are **no symptoms of vaginal infection** (e.g., unusual discharge, itching, odor) mentioned in the patient's presentation that would warrant immediate screening for **bacterial vaginosis (BV)** at this visit.
- While BV can be associated with adverse pregnancy outcomes, routine asymptomatic screening by wet mount is **not universally recommended** at 24 weeks gestation without other indications.
More Pregestational diabetes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.