Maternal cancer in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Maternal cancer in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Maternal cancer in pregnancy US Medical PG Question 1: A 20-year-old woman presents with nausea, fatigue, and breast tenderness. She is sexually active with two partners and occasionally uses condoms during intercourse. A β-hCG urinary test is positive. A transvaginal ultrasound reveals an 8-week fetus in the uterine cavity. The patient is distressed by this news and requests an immediate abortion. Which of the following is the most appropriate step in management?
- A. Explain the risk and potential harmful effects of the procedure. (Correct Answer)
- B. Ask the patient to reconsider and refer her to a social worker.
- C. Ask the patient to obtain consent from legal guardians.
- D. Ask the patient to obtain consent from the baby’s father.
- E. Conduct a psychiatric evaluation for mental competence.
Maternal cancer in pregnancy Explanation: ***Explain the risk and potential harmful effects of the procedure.***
- It is crucial to **inform the patient fully** about the medical procedure, including its risks and benefits, as part of the **informed consent** process.
- This ensures the patient makes an autonomous, well-considered decision, which is a fundamental ethical principle in medicine.
*Ask the patient to reconsider and refer her to a social worker.*
- While it's important to ensure the patient has considered all aspects, **directly asking the patient to reconsider** can be perceived as coercive and may undermine her autonomy.
- Referring to a social worker might be appropriate if the patient expresses uncertainty or needs support, but it should not be a replacement for proper medical counseling about the procedure itself.
*Ask the patient to obtain consent from legal guardians.*
- At 20 years old, the patient is an **adult** and legally capable of making her own medical decisions, including consent for abortion.
- Forcing her to obtain consent from legal guardians would infringe upon her **autonomy and legal rights**.
*Ask the patient to obtain consent from the baby’s father.*
- In most jurisdictions, a woman's decision to have an abortion is **her legal right**, and the consent of the father is **not required**.
- Requiring paternal consent would violate her **personal autonomy** and could create unnecessary barriers to care.
*Conduct a psychiatric evaluation for mental competence.*
- There is **no indication** in the patient's presentation (nausea, fatigue, breast tenderness, distress about pregnancy) that suggests she lacks the mental competence to make her own medical decisions.
- Requesting a psychiatric evaluation without clinical grounds would be **unethical and inappropriate**.
Maternal cancer in pregnancy US Medical PG Question 2: A 30-year-old woman, gravida 2, para 1, at 12 weeks' gestation comes to the physician for a prenatal visit. She feels well. Pregnancy and vaginal delivery of her first child were uncomplicated. Five years ago, she was diagnosed with hypertension but reports that she has been noncompliant with her hypertension regimen. The patient does not smoke or drink alcohol. She does not use illicit drugs. Medications include methyldopa, folic acid, and a multivitamin. Her temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 145/90 mm Hg. Physical examination shows no abnormalities. Laboratory studies, including serum glucose level, and thyroid-stimulating hormone concentration, are within normal limits. The patient is at increased risk of developing which of the following complications?
- A. Placenta previa
- B. Abruptio placentae (Correct Answer)
- C. Spontaneous abortion
- D. Polyhydramnios
- E. Uterine rupture
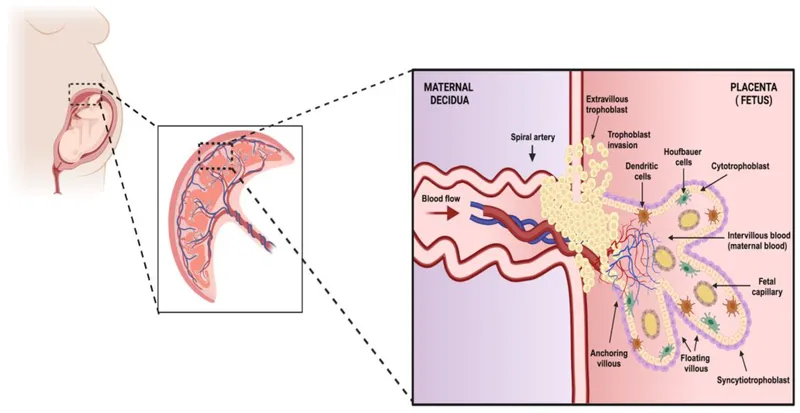
Maternal cancer in pregnancy Explanation: ***Abruptio placentae***
- The patient's history of **chronic hypertension** (145/90 mmHg) and her noncompliance with antihypertensive medication significantly increase her risk for **abruptio placentae**. Hypertension is a major risk factor for this condition.
- Abruptio placentae involves the **premature separation of the placenta** from the uterine wall, which can lead to severe maternal hemorrhage, fetal distress, and preterm birth.
*Placenta previa*
- **Placenta previa** is characterized by the placenta covering the cervical os and is primarily associated with risk factors like **previous C-section**, multiple gestations, or advanced maternal age.
- While a serious complication, it is **not directly linked to chronic hypertension** in the same manner as abruptio placentae.
*Spontaneous abortion*
- **Spontaneous abortion** typically occurs in the **first trimester** and is often due to chromosomal abnormalities, endocrine disorders, or uterine anomalies.
- While hypertension could theoretically contribute to some pregnancy complications, it is **not a primary risk factor** for spontaneous abortion at 12 weeks gestation.
*Polyhydramnios*
- **Polyhydramnios** is an excessive accumulation of amniotic fluid, often associated with **maternal diabetes**, fetal anomalies (e.g., GI obstruction, anencephaly), or multiple gestations.
- Maternal hypertension is **not a direct risk factor** for polyhydramnios.
*Uterine rupture*
- **Uterine rupture** is a rare but catastrophic event, most commonly associated with a **previous uterine scar** (e.g., from a prior C-section or myomectomy).
- The patient's history of a prior vaginal delivery and absence of uterine surgery means she is **not at increased risk** for uterine rupture at this stage.
Maternal cancer in pregnancy US Medical PG Question 3: A 40-year-old, gravida 2, nulliparous woman, at 14 weeks' gestation comes to the physician because of a 6-hour history of light vaginal bleeding and lower abdominal discomfort. Eight months ago she had a spontaneous abortion at 10 weeks' gestation. Her pulse is 92/min, respirations are 18/min, and blood pressure is 134/76 mm Hg. Abdominal examination shows no tenderness or masses; bowel sounds are normal. On pelvic examination, there is old blood in the vaginal vault and at the closed cervical os. The uterus is larger than expected for the length of gestation and there are bilateral adnexal masses. Serum β-hCG concentration is 120,000 mIU/ml. Which of the following is the most appropriate next step in management?
- A. Fetal blood sampling
- B. Fetal Doppler ultrasound
- C. Chorionic villus sampling
- D. Thyroid function tests
- E. Transvaginal ultrasound (Correct Answer)
Maternal cancer in pregnancy Explanation: ***Transvaginal ultrasound***
- The patient's presentation with **vaginal bleeding**, **uterus larger than expected**, **bilateral adnexal masses**, and **extremely elevated β-hCG (120,000 mIU/ml at 14 weeks)** strongly suggests a **hydatidiform mole** (a type of gestational trophoblastic disease).
- A **transvaginal ultrasound** is the definitive diagnostic tool to confirm a molar pregnancy, visualize the characteristic "snowstorm" appearance, and assess for any retained products of conception or ovarian theca-lutein cysts associated with high β-hCG.
*Fetal blood sampling*
- This procedure is typically performed later in pregnancy (after 18-20 weeks) to diagnose **fetal anemia**, **infections**, or **chromosomal abnormalities**, none of which are indicated by the current findings.
- The likelihood of a viable fetus with the clinical picture of a molar pregnancy is very low, making this intervention inappropriate.
*Fetal Doppler ultrasound*
- A fetal Doppler ultrasound primarily assesses **fetal blood flow** and well-being, which is not the priority given the high suspicion of a molar pregnancy.
- While it can detect a fetal heart rate in normal pregnancies, it would not provide the structural detail needed to diagnose a molar pregnancy.
*Chorionic villus sampling*
- This procedure is used for **prenatal genetic diagnosis** in early pregnancy (10-13 weeks) but would not be the first line of investigation for suspected molar pregnancy.
- The primary concern here is the diagnosis of a growth abnormality of the placenta, not fetal genetics, especially given the other strongly suggestive signs of a molar pregnancy.
*Thyroid function tests*
- While **hyperthyroidism** can be a rare complication of exceptionally high β-hCG levels due to its structural similarity to TSH, it is a secondary concern.
- Diagnosing the underlying cause of the high β-hCG and abnormal pregnancy, which is most likely a molar pregnancy, takes precedence over evaluating for potential secondary complications at this stage.
Maternal cancer in pregnancy US Medical PG Question 4: A 24-year-old primigravida presents at 36 weeks gestation with vaginal bleeding, mild abdominal pain, and uterine contractions that appeared after bumping into a handrail. The vital signs are as follows: blood pressure 130/80 mm Hg, heart rate 79/min, respiratory rate 12/min, and temperature 36.5℃ (97.7℉). The fetal heart rate was 145/min. Uterine fundus is at the level of the xiphoid process. Slight uterine tenderness and contractions are noted on palpation. The perineum is bloody. The gynecologic examination shows no vaginal or cervical lesions. The cervix is long and closed. Streaks of bright red blood are passing through the cervix. A transabdominal ultrasound shows the placenta to be attached to the lateral uterine wall with a marginal retroplacental hematoma (an approximate volume of 150 ml). The maternal hematocrit is 36%. What is the next best step in the management of this patient?
- A. Manage as an outpatient with modified rest
- B. Induction of vaginal labor
- C. Corticosteroid administration and schedule a cesarean section after
- D. Admit for maternal and fetal monitoring and observation (Correct Answer)
- E. Urgent cesarean delivery
Maternal cancer in pregnancy Explanation: ***Admit for maternal and fetal monitoring and observation***
- This patient presents with signs of a **mild placental abruption** (vaginal bleeding, contractions, mild abdominal pain, retroplacental hematoma) after trauma, but her **vital signs are stable**, fetal heart rate is reassuring, and the abruption volume is relatively small.
- Expectant management with **close monitoring** for signs of worsening abruption (increasing pain, vital sign changes, fetal distress) is appropriate for a patient at 36 weeks with a non-catastrophic abruption.
*Manage as an outpatient with modified rest*
- Given the presence of **vaginal bleeding, contractions**, and a **retroplacental hematoma** suggesting placental abruption, outpatient management is not safe.
- There is a risk of the abruption progressing, requiring immediate medical intervention, making **hospital admission for close monitoring** essential.
*Induction of vaginal labor*
- While vaginal delivery might be considered for a stable abruption in some cases, **active induction is not the immediate next step** given the patient's stable status and the need for continuous monitoring.
- The **cervix is long and closed**, indicating that she is not in active labor and immediate induction might not be successful or necessary.
*Corticosteroid administration and schedule a cesarean section after*
- **Corticosteroids** are typically administered for fetal lung maturity when delivery is anticipated before **34 weeks of gestation**; at 36 weeks, this is generally not indicated.
- A scheduled cesarean section is premature as the patient is **stable**, and the immediate goal is to monitor for progression or resolution of the abruption, not immediate delivery.
*Urgent cesarean delivery*
- There are no signs of **maternal or fetal distress** (stable vitals, reassuring fetal heart rate) that would necessitate an urgent cesarean delivery.
- An urgent cesarean is reserved for cases of **severe abruption** with significant bleeding, hemodynamic instability, or fetal compromise.
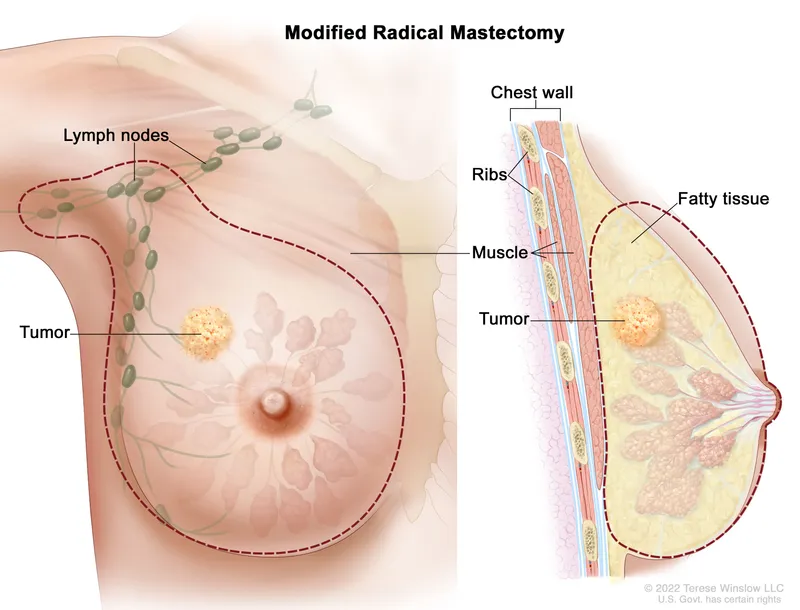
Maternal cancer in pregnancy US Medical PG Question 5: An obese 34-year-old primigravid woman at 20 weeks' gestation comes to the physician for a follow-up examination for a mass she found in her left breast 2 weeks ago. Until pregnancy, menses had occurred at 30- to 40-day intervals since the age of 11 years. Vital signs are within normal limits. Examination shows a 3.0-cm, non-mobile, firm, and nontender mass in the upper outer quadrant of the left breast. There is no palpable axillary lymphadenopathy. Pelvic examination shows a uterus consistent in size with a 20-week gestation. Mammography and core needle biopsy confirm an infiltrating lobular carcinoma. The pathological specimen is positive for estrogen and human epidermal growth factor receptor 2 (HER2) receptors and negative for progesterone receptors. Staging shows no distant metastatic disease. Which of the following is the most appropriate management?
- A. Surgical resection and chemotherapy (Correct Answer)
- B. Surgical resection
- C. Radiotherapy and chemotherapy
- D. Radiotherapy only
- E. Surgical resection and radiotherapy
Maternal cancer in pregnancy Explanation: ***Surgical resection and chemotherapy***
- This patient has **infiltrating lobular carcinoma** with **positive estrogen and HER2 receptors** but **negative progesterone receptors**.
- Given the patient's **pregnancy status** and the tumor's receptor profile, chemotherapy is indicated in addition to surgical resection.
*Surgical resection*
- While surgical resection is a critical component of breast cancer treatment, it is insufficient alone for this patient given the tumor's aggressive features and receptor status, particularly the **HER2 positivity**.
- **HER2-positive cancers** benefit significantly from targeted chemotherapy, which would be missed with surgery alone.
*Radiotherapy and chemotherapy*
- **Radiotherapy** for breast cancer typically involves daily treatments over several weeks and is often **deferred until after delivery** in pregnant patients due to potential fetal risks.
- While chemotherapy is appropriate, initiation of radiotherapy is generally postponed or individualized based on gestational age and specific circumstances.
*Radiotherapy only*
- **Radiotherapy alone** is not an appropriate primary treatment for an invasive breast carcinoma in this context.
- It often follows surgery to reduce local recurrence but does not address the systemic nature of **HER2-positive cancer**.
*Surgical resection and radiotherapy*
- As mentioned, **radiotherapy** is generally avoided or delayed in pregnant patients due to concerns about **fetal exposure**.
- Moreover, this approach omits **chemotherapy**, which is crucial for **HER2-positive breast cancer** to prevent recurrence and improve survival.
Maternal cancer in pregnancy US Medical PG Question 6: A 23-year-old primigravid woman comes to the physician at 28 weeks' gestation for a prenatal visit. Over the past 2 months, she has developed a hoarse voice and facial hair. Her medications include iron and a multivitamin. The last fetal ultrasonography, performed at 21 weeks' gestation, was unremarkable. Vital signs are within normal limits. Examination shows facial acne and hirsutism. Pelvic examination shows clitoromegaly. The uterus is consistent in size with a 28-week gestation. There are bilateral adnexal masses present on palpation. Ultrasonography shows a single live intrauterine pregnancy consistent with a 28-week gestation and bilateral 6-cm solid, multinodular ovarian masses. Serum androgen levels are increased. Which of the following is the most appropriate next step in management?
- A. Measurement of serum inhibin levels (Correct Answer)
- B. Diagnostic laparoscopy
- C. Oophorectomy
- D. Fine needle aspiration cytology
- E. Monitoring
Maternal cancer in pregnancy Explanation: **Measurement of serum inhibin levels**
* **Sertoli-Leydig cell tumors** are a common cause of **virilization** in pregnancy and are often associated with elevated **androgen levels**.
* **Inhibin A** and **inhibin B** are tumor markers that can be elevated in Sertoli-Leydig cell tumors.
*Diagnostic laparoscopy*
* While a definitive diagnosis might require surgery, performing a **diagnostic laparoscopy** is not the immediate next step.
* More **non-invasive investigations**, such as tumor marker measurements, should be conducted first to narrow down the differential diagnosis.
*Oophorectomy*
* **Oophorectomy** is a surgical procedure to remove the ovaries and is a definitive treatment for ovarian tumors.
* It is not the initial step in management and is usually reserved after more diagnostic information is obtained, especially given the ongoing pregnancy.
*Fine needle aspiration cytology*
* **Fine needle aspiration (FNA) cytology** is generally **contraindicated** for ovarian masses, especially in pregnancy, due to the risk of **tumor seeding** and potential rupture.
* Such a procedure could also lead to complications for the pregnancy itself.
*Monitoring*
* The patient is exhibiting clear signs of **virilization** and has **bilateral solid ovarian masses**, which strongly suggest a **tumor** producing androgens.
* **Monitoring** without further investigation would delay diagnosis and potential treatment, putting both the mother and fetus at risk.
Maternal cancer in pregnancy US Medical PG Question 7: A 29-year-old woman presents to a medical office complaining of fatigue, nausea, and vomiting for 1 week. Recently, the smell of certain foods makes her nauseous. Her symptoms are more pronounced in the mornings. The emesis is clear-to-yellow without blood. She has had no recent travel out of the country. The medical history is significant for peptic ulcer, for which she takes pantoprazole. The blood pressure is 100/60 mm Hg, the pulse is 70/min, and the respiratory rate is 12/min. The physical examination reveals pale mucosa and conjunctiva, and bilateral breast tenderness. The LMP was 9 weeks ago. What is the most appropriate next step in the management of this patient?
- A. Beta-HCG levels and a transvaginal ultrasound (Correct Answer)
- B. Beta-HCG levels and a transabdominal ultrasound
- C. Beta-HCG levels and a pelvic CT
- D. Abdominal x-ray
- E. Abdominal CT with contrast
Maternal cancer in pregnancy Explanation: ***Beta-HCG levels and a transvaginal ultrasound***
- The patient's symptoms (fatigue, nausea, vomiting, morning sickness, breast tenderness, and **amenorrhea** for 9 weeks) strongly suggest **early pregnancy**.
- **Urine or serum beta-HCG** confirms pregnancy, and a **transvaginal ultrasound** is crucial for confirming an **intrauterine pregnancy**, estimating gestational age, and ruling out complications like ectopic pregnancy, especially at this early stage when transabdominal ultrasound might not provide clear images.
*Beta-HCG levels and a transabdominal ultrasound*
- While beta-HCG levels are appropriate, a **transabdominal ultrasound** may not be sufficient to visualize an early intrauterine pregnancy at 9 weeks due to limited resolution compared to transvaginal ultrasound.
- A definitive confirmation of **intrauterine pregnancy** is critical to rule out an **ectopic pregnancy**, which is better achieved with transvaginal imaging in early gestation.
*Beta-HCG levels and a pelvic CT*
- **CT scans** expose the patient to significant **ionizing radiation**, which is **contraindicated in pregnancy** unless absolutely necessary for life-threatening conditions.
- While it could identify some pelvic pathologies, it is **not the primary imaging modality** for confirming or evaluating early pregnancy due to radiation risks and inferior soft tissue resolution for early gestational sacs compared to ultrasound.
*Abdominal x-ray*
- An **abdominal X-ray** involves **ionizing radiation** and offers very limited diagnostic value for early pregnancy, as it cannot visualize the gestational sac, fetus, or fetal heart activity.
- It is **contraindicated** in suspected pregnancy due to the risk of fetal harm.
*Abdominal CT with contrast*
- **Abdominal CT with contrast** involves both **ionizing radiation** and **contrast agents**, both of which pose significant risks to a developing fetus.
- It is an **inappropriate initial step** for suspected pregnancy and offers no specific diagnostic benefits for confirming or characterizing early gestation.
Maternal cancer in pregnancy US Medical PG Question 8: A G1P0 34-year-old woman presents to the clinic complaining of difficulty breathing and coughing up blood for 2 days. Past medical history is significant for molar pregnancy 6 months ago. The patient was lost to follow up as she was abruptly laid off and had to stay at a homeless shelter for the past few months. She endorses nausea and vomiting, abdominal discomfort, and “feeling hot all the time.” The patient is a past smoker of 1 pack per day for 10 years. Vital signs are within normal limits except for tachycardia. What is the disease process that most likely explains this patient’s symptoms?
- A. Malignant proliferation of trophoblastic tissue (Correct Answer)
- B. Malignant proliferation of squamous cells in the lung
- C. Acute infection with campylobacter jejuni
- D. Infectious process by mycobacterium tuberculosis
- E. Excessive production of thyroid hormone
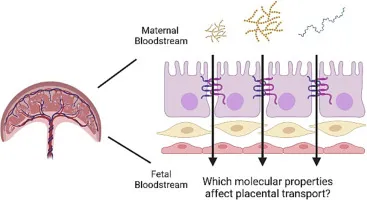
Maternal cancer in pregnancy Explanation: **Malignant proliferation of trophoblastic tissue**
- This patient's history of a **molar pregnancy** 6 months ago, followed by symptoms of **hemoptysis**, **difficulty breathing**, **nausea/vomiting**, and **abdominal discomfort**, is highly suggestive of **metastatic gestational trophoblastic neoplasia (GTN)**.
- GTN, particularly **choriocarcinoma**, can spread aggressively, most commonly to the lungs, presenting with respiratory symptoms and hemoptysis, and can also cause widespread systemic symptoms due to elevated **hCG** and distant metastases.
*Malignant proliferation of squamous cells in the lung*
- While **smoking** is a risk factor for **squamous cell carcinoma of the lung**, the patient's specific history of a **molar pregnancy** and the constellation of symptoms (nausea, vomiting, abdominal discomfort, "feeling hot") points more strongly towards GTN.
- Lung cancer typically doesn't present with symptoms like persistent nausea, vomiting, or abdominal discomfort unless there is advanced metastatic disease in those areas, which doesn't fit the primary cause here.
*Acute infection with campylobacter jejuni*
- **Campylobacter jejuni** causes acute **gastroenteritis**, characterized by diarrhea, abdominal pain, fever, and sometimes bloody stools, but it does not cause hemoptysis or relate to a past molar pregnancy.
- The presented symptoms are more systemic and involve respiratory compromise not typical of isolated gastrointestinal infection.
*Infectious process by mycobacterium tuberculosis*
- **Mycobacterium tuberculosis** can cause **hemoptysis** and respiratory symptoms, especially in individuals with compromised living situations, but it does not explain the history of molar pregnancy or the systemic symptoms of nausea, vomiting, and abdominal discomfort in this context.
- The rapid onset of symptoms and the specific obstetric history make tuberculosis less likely as the primary diagnosis.
*Excessive production of thyroid hormone*
- **Hyperthyroidism** can cause tachycardia and a sensation of "feeling hot," but it would not explain the **hemoptysis**, **difficulty breathing**, **nausea**, **vomiting**, or **abdominal discomfort** described in this patient.
- While gestational trophoblastic disease can sometimes lead to transient hyperthyroidism due to high hCG levels mimicking TSH, it is a secondary effect and not the primary disease process causing all symptoms.
Maternal cancer in pregnancy US Medical PG Question 9: A 25-year-old woman presents to her physician with a missed mense and occasional morning nausea. Her menstrual cycles have previously been normal and on time. She has hypothyroidism resulting from Hashimoto thyroiditis diagnosed 2 years ago. She receives levothyroxine (50 mcg daily) and is euthyroid. She does not take any other medications, including birth control pills. At the time of presentation, her vital signs are as follows: blood pressure 120/80 mm Hg, heart rate 68/min, respiratory rate 12/min, and temperature 36.5℃ (97.7℉). The physical examination shows slight breast engorgement and nipple hyperpigmentation. The gynecologic examination reveals cervical softening and increased mobility. The uterus is enlarged. There are no adnexal masses. The thyroid panel is as follows:
Thyroid stimulating hormone (TSH) 3.41 mU/L
Total T4 111 nmol/L
Free T4 20 pmol/L
Which of the following adjustments should be made to the patient’s therapy?
- A. Increase levothyroxine dosage by 20%–30% (Correct Answer)
- B. Decrease levothyroxine dosage by 30%
- C. Discontinue levothyroxine
- D. The patient is euthyroid, so no adjustments should be made
- E. Increase levothyroxine dosage by 5% each week up to 50%
Maternal cancer in pregnancy Explanation: ***Increase levothyroxine dosage by 20%–30%***
- The patient's symptoms (missed menses, nausea, breast changes, enlarged uterus, cervical changes) are highly suggestive of **pregnancy**. During pregnancy, **thyroid hormone requirements increase significantly** due to increased levels of **thyroid-binding globulin (TBG)** stimulated by estrogen, and the production of **human chorionic gonadotropin (hCG)** which has TSH-like activity.
- The recommended management for pregnant women with hypothyroidism is to **increase the levothyroxine dose by approximately 25-50%** and monitor TSH and free T4 levels every 4-6 weeks to maintain a TSH level within the goal range for pregnancy (typically <2.5 mU/L in the first trimester).
*Decrease levothyroxine dosage by 30%*
- Decreasing levothyroxine would lead to **hypothyroidism**, which is detrimental in pregnancy and associated with adverse outcomes such as **preeclampsia**, **gestational hypertension**, **low birth weight**, and **neurocognitive impairment** in the offspring.
- Thyroid hormone requirements increase, not decrease, during pregnancy.
*Discontinue levothyroxine*
- **Discontinuing levothyroxine** would result in severe hypothyroidism, posing significant risks to both the mother and the developing fetus.
- Hypothyroidism must be treated throughout pregnancy to ensure proper fetal development.
*The patient is euthyroid, so no adjustments should be made*
- While the patient's thyroid panel currently shows euthyroid values (TSH 3.41 mU/L is within normal range but slightly elevated for first-trimester pregnancy goals), the **onset of pregnancy** rapidly increases thyroid hormone demand.
- Failure to adjust the dose can lead to **maternal and fetal hypothyroidism** as pregnancy progresses, even if the patient is currently euthyroid.
*Increase levothyroxine dosage by 5% each week up to 50%*
- A gradual increase of 5% each week may be too slow and insufficient to meet the rapidly increasing thyroid hormone demands of early pregnancy.
- The standard recommendation is to make a more substantial initial adjustment (20-30%) as soon as pregnancy is confirmed, followed by close monitoring and further adjustments.
Maternal cancer in pregnancy US Medical PG Question 10: A 25-year-old woman, gravida 2, para 1, at 25 weeks' gestation comes to the emergency department because of a 1-day history of fever and right-sided flank pain. During this period, she also had chills, nausea, vomiting, and burning on urination. Her last prenatal visit was 10 weeks ago. Pregnancy and delivery of her first child were uncomplicated. Her temperature is 39°C (102.2°F), pulse is 110/min, respirations are 20/min, and blood pressure is 110/70 mm Hg. Physical examination shows costovertebral angle tenderness on the right. The abdomen is soft and nontender, and no contractions are felt. Pelvic examination shows a uterus consistent in size with a 25-week gestation. Fetal heart rate is 170/min. Laboratory studies show:
Leukocyte count 15,000/mm3
Urine
Nitrite 2+
Protein 1+
Blood 1+
RBC 5/hpf
WBC 500/hpf
Blood and urine samples are obtained for culture and drug sensitivity. Which of the following is the most appropriate next step in management?
- A. Inpatient treatment with intravenous ceftriaxone (Correct Answer)
- B. Perform a renal ultrasound
- C. Outpatient treatment with oral ciprofloxacin
- D. Inpatient treatment with intravenous ampicillin and gentamicin
- E. Admit the patient and request an emergent obstetrical consult
Maternal cancer in pregnancy Explanation: ***Inpatient treatment with intravenous ceftriaxone***
- The patient presents with classic signs of **pyelonephritis** (fever, flank pain, nausea, vomiting, CVA tenderness) in pregnancy, which warrants **inpatient admission** and **IV antibiotics** to prevent complications such as sepsis, preterm labor, and fetal compromise.
- **Ceftriaxone** is a broad-spectrum cephalosporin that is safe and effective in pregnancy for treating urinary tract infections, including pyelonephritis.
*Perform a renal ultrasound*
- While a **renal ultrasound** may be considered in cases of persistent fever after 48-72 hours of antibiotic therapy or if there's suspicion of obstruction or abscess, it is **not the immediate next step**.
- The priority is to initiate antibiotics promptly to treat the acute infection and prevent further complications.
*Outpatient treatment with oral ciprofloxacin*
- **Outpatient treatment** is inappropriate for **pyelonephritis in pregnancy** due to the high risk of complications for both the mother and the fetus.
- **Ciprofloxacin** (a fluoroquinolone) is generally **contraindicated in pregnancy** because of potential adverse effects on fetal cartilage development.
*Inpatient treatment with intravenous ampicillin and gentamicin*
- Although **ampicillin and gentamicin** are effective for many UTIs and safe in pregnancy, they are often reserved for cases where local resistance patterns favor this combination or as a second-line option.
- **Ceftriaxone** is a preferred first-line empiric choice for pyelonephritis in pregnancy due to its broad coverage and once-daily dosing.
*Admit the patient and request an emergent obstetrical consult*
- While admitting the patient is correct, **immediately requesting an emergent obstetrical consult** is premature as the primary issue is an acute infection requiring medical management.
- Obstetrics consultation is important in managing high-risk pregnancies or complications like preterm labor, but antibiotics for pyelonephritis should be initiated first, and then an obstetrician can be consulted for comanagement.
More Maternal cancer in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.