Chronic hypertension in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Chronic hypertension in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Chronic hypertension in pregnancy US Medical PG Question 1: A 24-year-old primigravida presents to her physician for regular prenatal care at 31 weeks gestation. She has no complaints and the antepartum course has been uncomplicated. Her pre-gestational history is significant for obesity (BMI = 30.5 kg/m2). She has gained a total of 10 kg (22.4 lb) during pregnancy, and 2 kg (4.48 lb) since her last visit 4 weeks ago. Her vital signs are as follows: blood pressure, 145/90 mm Hg; heart rate, 87/min; respiratory rate, 14/min; and temperature, 36.7℃ (98℉). The fetal heart rate is 153/min. The physical examination shows no edema and is only significant for a 2/6 systolic murmur best heard at the apex of the heart. A 24-hour urine is negative for protein. Which of the following options describe the best management strategy in this case?
- A. Treatment in outpatient settings with labetalol
- B. Treatment in the outpatient settings with nifedipine
- C. Observation in the outpatient settings (Correct Answer)
- D. Treatment in the inpatient settings with methyldopa
- E. Admission to hospital for observation
Chronic hypertension in pregnancy Explanation: ***Observation in the outpatient settings***
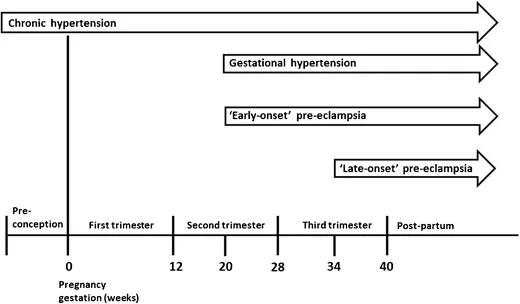
- The patient's blood pressure is 145/90 mmHg, which meets the criteria for **gestational hypertension** according to ACOG (systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg on two occasions at least 4 hours apart after 20 weeks gestation in a previously normotensive woman, without proteinuria).
- Since this is a single elevated blood pressure reading (not yet confirmed by a second reading after 4 hours) and there is no evidence of **proteinuria** or **severe features** (e.g., severe headache, visual disturbances, epigastric pain, elevated liver enzymes, thrombocytopenia, pulmonary edema), **close outpatient monitoring** is the appropriate initial step.
*Treatment in outpatient settings with labetalol*
- **Antihypertensive medication** is typically initiated for gestational hypertension if BP is consistently ≥160/110 mmHg, or if there are signs of severe features.
- While labetalol is a safe and common first-line agent, starting treatment based on a **single, non-severe elevated BP reading** without confirmed gestational hypertension or severe features is premature.
*Treatment in the outpatient settings with nifedipine*
- Similar to labetalol, **nifedipine** is an appropriate antihypertensive if medication is warranted for gestational hypertension.
- However, initiating medication is not the **first step** for an isolated, non-severe elevated blood pressure reading without confirmed diagnosis or severe features.
*Treatment in the inpatient settings with methyldopa*
- **Inpatient treatment** is reserved for patients with severe gestational hypertension, preeclampsia with severe features, or uncontrollable hypertension.
- While methyldopa is a safe antihypertensive in pregnancy, inpatient treatment is **not indicated** for this patient's presentation.
*Admission to hospital for observation*
- **Hospital admission** for observation is generally reserved for patients with more severe hypertension, suspected preeclampsia with severe features, or concerns about fetal well-being.
- Given the patient's **asymptomatic state**, normal fetal heart rate, and lack of proteinuria or severe features, inpatient admission is **unnecessary** at this stage.
Chronic hypertension in pregnancy US Medical PG Question 2: A 35-year-old G3P2 woman currently 39 weeks pregnant presents to the emergency department with painful vaginal bleeding shortly after a motor vehicle accident in which she was a passenger. She had her seat belt on and reports that the airbag deployed immediately upon her car's impact against a tree. She admits that she actively smokes cigarettes. Her prenatal workup is unremarkable. Her previous pregnancies were remarkable for one episode of chorioamnionitis that resolved with antibiotics. Her temperature is 98.6°F (37°C), blood pressure is 90/60 mmHg, pulse is 130/min, and respirations are 20/min. The fetal pulse is 110/min. Her uterus is tender and firm. The remainder of her physical exam is unremarkable. What is the most likely diagnosis?
- A. Placental abruption (Correct Answer)
- B. Eclampsia
- C. Vasa previa
- D. Preterm labor
- E. Preeclampsia
Chronic hypertension in pregnancy Explanation: ***Placental abruption***
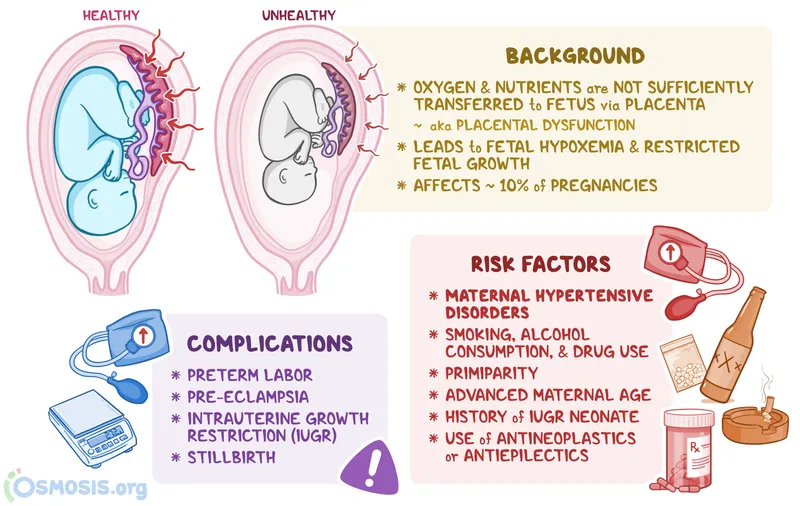
- The patient's presentation with **painful vaginal bleeding** after blunt abdominal trauma (motor vehicle accident), a **tender and firm uterus**, maternal **hypotension** and **tachycardia**, and fetal **bradycardia** is highly characteristic of placental abruption.
- Risk factors like **smoking** and trauma further increase the likelihood of placental abruption.
*Eclampsia*
- Eclampsia is characterized by **new-onset grand mal seizures** in a pregnant woman with preeclampsia, which is not present in this scenario.
- While the patient's low blood pressure and tachycardia are concerning, they do not point to eclampsia.
*Vasa previa*
- Vasa previa involves **fetal blood vessels** running within the fetal membranes over the internal cervical os, risking rupture during labor or membrane rupture, leading to **painless vaginal bleeding** and **fetal distress**.
- The bleeding in this case is described as painful, and the uterine tenderness and firmness are not typical of vasa previa.
*Preterm labor*
- Preterm labor is defined by **regular uterine contractions** causing cervical changes before 37 weeks of gestation, which is not aligned with the patient being 39 weeks pregnant or her symptoms.
- While trauma can initiate labor, the severity of the bleeding and maternal/fetal distress point away from isolated preterm labor.
*Preeclampsia*
- Preeclampsia is characterized by **new-onset hypertension** (blood pressure ≥140/90 mmHg) and **proteinuria** after 20 weeks of gestation.
- This patient presents with hypotension and no mention of hypertension or proteinuria, making preeclampsia unlikely.
Chronic hypertension in pregnancy US Medical PG Question 3: A 26-year-old woman, gravida 2, para 1, at 28 weeks' gestation comes to the physician for a prenatal visit. She feels well. Pregnancy and delivery of her first child were uncomplicated. Her temperature is 37.2°C (99°F) and blood pressure is 163/105 mm Hg. Her blood pressure 10 weeks ago was 128/84 mm Hg. At her last visit two weeks ago, her blood pressure was 142/92 mm Hg. Pelvic examination shows a uterus consistent in size with a 28-week gestation. A complete blood count and serum concentrations of electrolytes, creatinine, and hepatic transaminases are within the reference range. A urinalysis is within normal limits. Which of the following is the most appropriate next step in management?
- A. Oral labetalol therapy (Correct Answer)
- B. Lisinopril therapy
- C. Magnesium sulfate therapy
- D. Complete bed rest
- E. Dietary salt restriction
Chronic hypertension in pregnancy Explanation: **Oral labetalol therapy**
- The patient has developed **gestational hypertension** (blood pressure ≥140/90 mmHg on two occasions at least 4 hours apart after 20 weeks gestation, without proteinuria or other signs of preeclampsia), with her current BP of 163/105 mmHg confirming **severe range hypertension** (systolic ≥160 mmHg or diastolic ≥110 mmHg).
- **Labetalol** is a first-line agent for managing hypertension in pregnancy due to its established safety profile and efficacy in lowering blood pressure.
*Lisinopril therapy*
- **Angiotensin-converting enzyme (ACE) inhibitors** like lisinopril are **contraindicated in pregnancy** as they can cause fetal renal dysfunction, oligohydramnios, and neonatal hypotension.
- This medication choice would be harmful to the fetus.
*Magnesium sulfate therapy*
- **Magnesium sulfate** is indicated for the **prevention and treatment of seizures in preeclampsia/eclampsia**, not for blood pressure control itself.
- While the patient has hypertension, there are no signs of preeclampsia (e.g., proteinuria, signs of end-organ damage), making magnesium sulfate inappropriate at this stage.
*Complete bed rest*
- **Complete bed rest** is no longer recommended for the management of gestational hypertension or preeclampsia, as studies have shown it does not improve maternal or fetal outcomes and can increase the risk of **thromboembolism**.
- It can also negatively impact a patient's quality of life without providing therapeutic benefit.
*Dietary salt restriction*
- While generally recommended for hypertension outside of pregnancy, **severe salt restriction** in pregnancy is **not typically recommended** for gestational hypertension or preeclampsia, as it has not been shown to improve outcomes and could potentially worsen maternal fluid balance.
- The primary management for severe range gestational hypertension involves antihypertensive medications.
Chronic hypertension in pregnancy US Medical PG Question 4: A 22-year-old primigravida is admitted to the obstetrics ward with leg swelling at 35 weeks gestation. She denies any other symptoms. Her pregnancy has been uneventful and she was compliant with the recommended prenatal care. Her vital signs were as follows: blood pressure, 168/95 mm Hg; heart rate, 86/min; respiratory rate, 16/min; and temperature, 36.7℃ (98℉). The fetal heart rate was 141/min. The physical examination was significant for 2+ pitting edema of the lower extremity. A dipstick test shows 1+ proteinuria. On reassessment 15 minutes later without administration of an antihypertensive, her blood pressure was 141/88 mm Hg, and the fetal heart rate was 147/min. A decision was made to observe the patient and continue the work-up without initiating antihypertensive therapy. Which of the following clinical features would make the suspected diagnosis into a more severe form?
- A. Serum creatinine 0.98 mg/dL
- B. 24-hour urinary protein of 5 g/L (Correct Answer)
- C. Hematocrit of 0.55
- D. Platelet count 133,000/μL
- E. Blood pressure of 165/90 mm Hg reassessed 4 hours later
Chronic hypertension in pregnancy Explanation: ***24-hour urinary protein of 5 g/L***
- A 24-hour urine protein collection exceeding **5 g/L (or 5000 mg)** is a criterion for **severe preeclampsia**, indicating significant renal involvement.
- This level of proteinuria suggests extensive **glomerular damage** and impaired renal function beyond what is seen in mild preeclampsia.
*Serum creatinine 0.98 mg/dL*
- A serum **creatinine of 0.98 mg/dL** is within the normal range for this patient and does not indicate renal insufficiency or severe preeclampsia.
- Renal dysfunction in severe preeclampsia is typically defined by a **creatinine >1.1 mg/dL** or a doubling of baseline creatinine.
*Hematocrit of 0.55*
- A **hematocrit of 0.55 (55%)** might indicate hemoconcentration, but not necessarily severe preeclampsia. **Hemoconcentration** is common in preeclampsia due to plasma volume contraction but is not a primary diagnostic criterion for severity.
- Severe preeclampsia is often associated with **microangiopathic hemolytic anemia**, which would typically manifest as a *decreasing* hematocrit due to red blood cell destruction.
*Platelet count 133,000/μL*
- A **platelet count of 133,000/μL** is within the normal range or slightly below, but it is not indicative of severe **thrombocytopenia**.
- **Severe thrombocytopenia** in preeclampsia is defined as a platelet count **<100,000/μL**.
*Blood pressure of 165/90 mm Hg reassessed 4 hours later*
- This blood pressure reading, while elevated, does not meet the criteria for severe preeclampsia on its own, as **severe hypertension** is defined as **systolic BP ≥160 mm Hg or diastolic BP ≥110 mm Hg on two occasions at least 4 hours apart** while the patient is on bed rest.
- The initial reading improved, and this single elevated reading after 4 hours requires another confirming reading to classify as severe hypertension.
Chronic hypertension in pregnancy US Medical PG Question 5: A 27-year-old woman presents to her primary care physician for a concern about her pregnancy. This is her first pregnancy, and she is currently at 33 weeks gestation. She states that she has experienced diffuse swelling of her ankles and legs and is concerned that it is abnormal. Otherwise, she has no concerns. The patient has a past medical history of obesity and diabetes. Her temperature is 98.5°F (36.9°C), blood pressure is 147/92 mmHg, pulse is 80/min, respirations are 15/min, and oxygen saturation is 97% on room air. Physical exam reveals bilateral edema of the lower extremities. Which of the following is the best next step in management?
- A. Urinalysis and urine protein
- B. Echocardiography
- C. Reassurance and followup in 1 week
- D. A 24 hour urine protein
- E. Spot protein to creatinine ratio (Correct Answer)
Chronic hypertension in pregnancy Explanation: ***Spot protein to creatinine ratio***
- The patient presents with **hypertension** (147/92 mmHg) and **edema** in the third trimester of pregnancy, raising suspicion for **preeclampsia**.
- A spot urine protein-to-creatinine ratio is a **rapid** and **convenient screening test** to assess for significant proteinuria, which is a diagnostic criterion for preeclampsia.
*Urinalysis and urine protein*
- While a urinalysis can detect protein, it is **qualitative** and less precise than quantitative methods for diagnosing preeclampsia.
- A plain urine dipstick for protein can yield **false positives** or **false negatives**, making it an unreliable sole diagnostic test for proteinuria in this context.
*Echocardiography*
- Echocardiography is primarily used to evaluate **cardiac function** and structure, and there are no signs or symptoms in this patient suggesting primary cardiac pathology.
- While preeclampsia can affect the heart, an echocardiogram is **not the initial diagnostic step** for suspected preeclampsia itself.
*Reassurance and followup in 1 week*
- Given the elevated blood pressure and edema, **preeclampsia is a serious concern** that requires immediate evaluation, not delayed follow-up.
- Delaying assessment could lead to progression of the condition, increasing risks for both the mother and the fetus.
*A 24 hour urine protein*
- A 24-hour urine collection for protein is considered the **gold standard** for quantifying proteinuria.
- However, it is **time-consuming** and less practical as an initial rapid assessment tool compared to a spot protein-to-creatinine ratio when immediate evaluation for preeclampsia is warranted.
Chronic hypertension in pregnancy US Medical PG Question 6: A 32-year-old G2P1 female at 30 weeks gestation presents to the emergency department with complaints of vaginal bleeding and severe abdominal pain. She states that she began feeling poorly yesterday with a stomach-ache, nausea, and vomiting. She first noted a small amount of spotting this morning that progressed to much larger amounts of vaginal bleeding with worsened abdominal pain a few hours later, prompting her to come to the emergency department. Her previous pregnancy was without complications, and the fetus was delivered at 40 weeks by Cesarean section. Fetal heart monitoring shows fetal distress with late decelerations. Which of the following is a risk factor for this patient's presenting condition?
- A. Singleton pregnancy
- B. Hyperlipidemia
- C. Patient age
- D. Hypertension (Correct Answer)
- E. Prior Cesarean section
Chronic hypertension in pregnancy Explanation: ***Hypertension***
- The presenting symptoms of **vaginal bleeding**, **severe abdominal pain**, and **fetal distress** in a pregnant woman are highly suggestive of **placental abruption**.
- **Chronic hypertension** is a well-established and significant risk factor for placental abruption, increasing the risk by two to three times.
*Singleton pregnancy*
- This is typical for most pregnancies and does not increase the risk of placental abruption.
- **Multiple gestations** (twins, triplets) are actually associated with an increased risk of placental abruption, not singleton pregnancies.
*Hyperlipidemia*
- **Hyperlipidemia** is generally not considered a direct risk factor for placental abruption.
- While it can be associated with other cardiovascular issues, its link to placental abruption is not significant in the way hypertension is.
*Patient age*
- At 32 years old, the patient is not at an extremely advanced maternal age, which typically refers to 35 years or older.
- While **advanced maternal age** can be a slight risk factor for some pregnancy complications, it is not as strong a risk factor for placental abruption as hypertension in this context.
*Prior Cesarean section*
- A **prior Cesarean section** is a risk factor for conditions like **placenta previa** and **placenta accreta**, where the placenta implants abnormally.
- It is not a primary risk factor for **placental abruption**, which involves premature separation of a normally implanted placenta.
Chronic hypertension in pregnancy US Medical PG Question 7: A 28-year-old woman at 28 weeks gestation seeks evaluation at her obstetrician’s office with complaints of a severe headache, blurred vision, and vomiting for the past 2 days. Her pregnancy has been otherwise uneventful. The past medical history is unremarkable. The blood pressure is 195/150 mm Hg and the pulse is 88/min. On examination, moderate pitting edema is present in her ankles. The urinalysis is normal except for 3+ proteinuria. The obstetrician orders a complete blood count (CBC), liver function tests (LFTs), creatinine, and a coagulation profile. The obstetrician transfers her to the hospital by ambulance for expectant management. Which of the following medications would be most helpful for this patient?
- A. Olmesartan
- B. Lisinopril
- C. Nifedipine (Correct Answer)
- D. Hydrochlorothiazide
- E. Metoprolol
Chronic hypertension in pregnancy Explanation: ***Nifedipine***
- The patient presents with **severe preeclampsia** (hypertension, proteinuria, and symptoms like headache and blurred vision), necessitating immediate **blood pressure reduction**. [1]
- **Nifedipine** is a **calcium channel blocker** that is effective and safe for acute blood pressure control in pregnancy, and is a first-line agent in this context. [1]
*Olmesartan*
- **Olmesartan** is an **angiotensin receptor blocker (ARB)**, which is **contraindicated in pregnancy** due to the risk of fetal renal toxicity and other adverse outcomes.
- ARBs can cause **fetal growth restriction**, oligohydramnios, and neonatal renal failure during the second and third trimesters.
*Lisinopril*
- **Lisinopril** is an **ACE inhibitor**, which, like ARBs, is **contraindicated in pregnancy** due to its teratogenic effects, particularly in the second and third trimesters.
- It can lead to **fetal renal dysfunction**, oligohydramnios, and other severe birth defects.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a **thiazide diuretic**; while sometimes used in chronic hypertension in pregnancy, it is **not appropriate for acute, severe hypertension** in preeclampsia.
- Diuretics can reduce maternal intravascular volume, which is already compromised in preeclampsia, potentially worsening placental perfusion and fetal well-being.
*Metoprolol*
- **Metoprolol** is a **beta-blocker** sometimes used for chronic hypertension in pregnancy, but it may not be the optimal choice for **acute, severe hypertension** in preeclampsia.
- While generally considered safe, it can be associated with **fetal growth restriction** and **neonatal bradycardia** or hypoglycemia, and other agents like nifedipine or labetalol are often preferred for acute management.
Chronic hypertension in pregnancy US Medical PG Question 8: A 37-year-old woman presents to her physician with a newly detected pregnancy for the initial prenatal care visit. She is gravida 3 para 2 with a history of preeclampsia in her 1st pregnancy. Her history is also significant for arterial hypertension diagnosed 1 year ago for which she did not take any medications. The patient reports an 8-pack-year smoking history and states she quit smoking a year ago. On examination, the vital signs are as follows: blood pressure 140/90 mm Hg, heart rate 69/min, respiratory rate 14/min, and temperature 36.6°C (97.9°F). The physical examination is unremarkable. Which of the following options is the most appropriate next step in the management for this woman?
- A. Methyldopa (Correct Answer)
- B. Magnesium sulfate
- C. Fosinopril
- D. Labetalol
- E. No medications needed
Chronic hypertension in pregnancy Explanation: ***Methyldopa***
- **Methyldopa** is a **centrally acting alpha-2 adrenergic agonist** that is considered a first-line agent for the treatment of **chronic hypertension in pregnancy**.
- Its **safety profile** and effectiveness in controlling blood pressure without significant fetal harm make it an appropriate choice.
*Magnesium sulfate*
- **Magnesium sulfate** is primarily used for the **prevention and treatment of seizures in preeclampsia** and **eclampsia**.
- It is not indicated for the chronic management of hypertension and is prescribed for specific acute indications during pregnancy.
*Fosinopril*
- **Fosinopril** is an **ACE inhibitor**, which is **contraindicated in pregnancy** due to its association with **fetal renal dysfunction**, **oligohydramnios**, and **malformations**, especially in the second and third trimesters.
- ACE inhibitors and ARBs should be avoided during pregnancy.
*Labetalol*
- **Labetalol** is an **alpha and beta-blocker that can be used for chronic hypertension in pregnancy**, but given the patient's history of asthma (implied through a history of smoking), **methyldopa** might be a slightly safer initial choice, although labetalol could also be considered.
- While generally safe, its use can be associated with **fetal growth restriction** and **neonatal bradycardia** if used indiscriminately, making methyldopa a preferred first-line agent in many cases.
*No medications needed*
- The patient has **chronic hypertension** (diagnosed 1 year ago) and previous **preeclampsia**, indicating a need for **antihypertensive management** to prevent adverse maternal and fetal outcomes.
- Not initiating treatment would put the patient at increased risk for **severe preeclampsia**, **placental abruption**, and other complications.
Chronic hypertension in pregnancy US Medical PG Question 9: A 44-year-old woman with high blood pressure and diabetes presents to the outpatient clinic and informs you that she is trying to get pregnant. Her current medications include lisinopril, metformin, and sitagliptin. Her blood pressure is 136/92 mm Hg and heart rate is 79/min. Her physical examination is unremarkable. What should you do regarding her medication for high blood pressure?
- A. Discontinue lisinopril and initiate aliskiren
- B. Discontinue lisinopril and initiate labetalol (Correct Answer)
- C. Continue her current regimen
- D. Continue her current regimen and add a beta-blocker for increased control
- E. Discontinue lisinopril and initiate candesartan
Chronic hypertension in pregnancy Explanation: ***Discontinue lisinopril and initiate labetalol***
- **Lisinopril**, an ACE inhibitor, is **teratogenic** and is contraindicated in pregnancy due to the risk of fetal renal dysfunction, oligohydramnios, and neonatal death.
- **Labetalol** is a **beta-blocker** commonly used in pregnancy for hypertension as it is considered safe and effective in this population.
*Discontinue lisinopril and initiate aliskiren*
- **Aliskiren**, a direct renin inhibitor, is also **teratogenic** and contraindicated in pregnancy due to similar risks as ACE inhibitors and ARBs.
- Replacing one teratogenic drug with another does not solve the primary concern of fetal safety.
*Continue her current regimen*
- **Continuing lisinopril** would expose the fetus to significant risks, as it is a known teratogen.
- The patient is actively trying to conceive, making it imperative to switch medications immediately.
*Continue her current regimen and add a beta-blocker for increased control*
- Adding a beta-blocker while continuing lisinopril is still inappropriate because **lisinopril itself is harmful during pregnancy**.
- The primary goal is to **discontinue teratogenic medications**, not simply to improve blood pressure control with an additional drug.
*Discontinue lisinopril and initiate candesartan*
- **Candesartan**, an **angiotensin receptor blocker (ARB)**, shares the same **teratogenic risks** as ACE inhibitors and is contraindicated in pregnancy.
- Replacing an ACE inhibitor with an ARB provides no benefit in terms of fetal safety.
Chronic hypertension in pregnancy US Medical PG Question 10: A 37-year-old woman presents to the clinic to discuss various options for contraception. The patient has a past medical history of hypertension, Wilson's disease, and constipation-dominant irritable bowel syndrome. The patient takes rivaroxaban and polyethylene glycol. The blood pressure is 152/98 mm Hg. On physical examination, the patient appears alert and oriented. The heart auscultation demonstrates regular rate and rhythm, and it is absent of murmurs. The lungs are clear to auscultation bilaterally without wheezing. The first day of the last menstrual period was 12 days ago. The urine hCG is negative. Given the patient's history and physical examination, which of the following forms of contraception is the most appropriate?
- A. Levonorgestrel (Correct Answer)
- B. levonorgestrel/ethinyl estradiol
- C. Depot-medroxyprogesterone acetate
- D. Ethinyl estradiol
- E. Copper IUD
Chronic hypertension in pregnancy Explanation: ***Levonorgestrel***
- This patient has **hypertension** that is not well-controlled given her blood pressure of 152/98 mm Hg, as well as a history of **rivaroxaban** use, indicating a risk for **thromboembolic events.**
- **Progestin-only** contraception, such as a levonorgestrel-releasing intrauterine device (IUD) or implant, is generally considered safe and effective in patients with these risk factors because it avoids the estrogenic effects associated with increased risk of **thrombosis** and worsening hypertension.
*Levonorgestrel/ethinyl estradiol*
- This is a **combined hormonal contraceptive** containing both estrogen and progestin.
- The **estrogen component** significantly increases the risk of **thromboembolic events**, which is contraindicated in patients with a history of hypertension and those on anticoagulants like rivaroxaban.
*Depot-medroroxyprogesterone acetate*
- While it is a **progestin-only method** and does not carry the same thromboembolic risks as estrogen, it has been associated with **bone density loss** with long-term use.
- Given the patient's existing medical conditions and the availability of other equally effective progestin-only options without this side effect profile, it may not be the most appropriate first-line choice.
*Ethinyl estradiol*
- This is a form of **estrogen** and would be used in a combined hormonal contraceptive.
- As discussed, the **estrogen component** significantly increases the risk of **thromboembolic events**, which is contraindicated in this patient due to her hypertension and rivaroxaban use.
*Copper IUD*
- The copper IUD is a **non-hormonal** option, making it safe for patients with cardiovascular risk factors or those on anticoagulants.
- However, for patients with **constipation-dominant IBS**, there is a theoretical concern that the insertion and presence of an IUD could exacerbate gastrointestinal symptoms, though this is not a strong contraindication compared to the risks associated with estrogen.
More Chronic hypertension in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.