Cardiac disease in pregnancy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiac disease in pregnancy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cardiac disease in pregnancy US Medical PG Question 1: A 27-year-old primigravid woman at 32 weeks' gestation comes to the physician for a prenatal visit. She has had swollen legs, mild shortness of breath, and generalized fatigue for the past 2 weeks. Medications include iron supplements and a multivitamin. Her temperature is 37.2°C (99°F), pulse is 93/min, respirations are 20/min, and blood pressure is 108/60 mm Hg. There is 2+ pitting edema of the lower extremities, but no erythema or tenderness. The lungs are clear to auscultation. Cardiac examination shows an S3 gallop. Pelvic examination shows a uterus consistent in size with a 32-week gestation. Which of the following is the most appropriate next step in management for this patient's symptoms?
- A. Ventilation-perfusion scan
- B. Urinalysis
- C. Echocardiography (Correct Answer)
- D. Lower extremity doppler
- E. Reassurance and monitoring
Cardiac disease in pregnancy Explanation: ***Echocardiography***
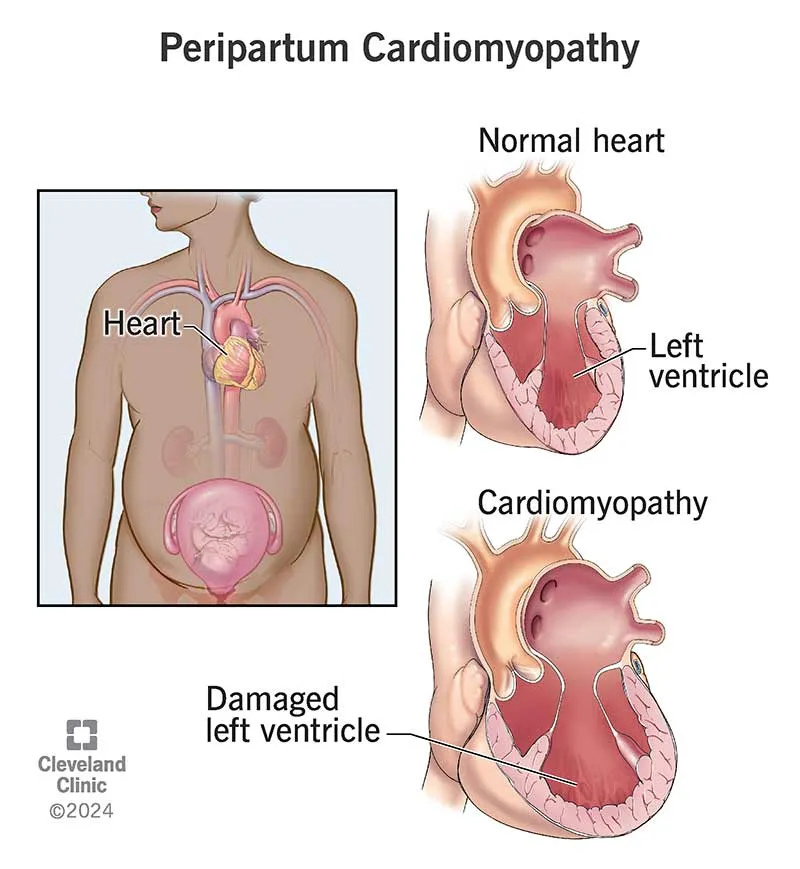
- The patient presents with classic signs of **peripartum cardiomyopathy**, including **new-onset heart failure** symptoms (dyspnea, fatigue, edema) in the late stages of pregnancy (32 weeks) with an **S3 gallop**.
- **Echocardiography** is the definitive diagnostic tool to visualize cardiac function, assess ventricular size, and measure the **ejection fraction** to confirm cardiomyopathy.
*Ventilation-perfusion scan*
- This test is primarily used to diagnose **pulmonary embolism**, which typically presents with sudden onset dyspnea, pleuritic chest pain, and sometimes hypoxemia, none of which are prominent here.
- While shortness of breath is present, the **S3 gallop** and widespread edema are more indicative of cardiac dysfunction than pulmonary embolism.
*Urinalysis*
- A urinalysis is used to screen for kidney issues or **preeclampsia** (proteinuria), which can present with edema and hypertension.
- However, this patient's blood pressure is normal, and her symptoms point more directly to cardiac rather than renal pathology.
*Lower extremity doppler*
- This is used to diagnose **deep vein thrombosis (DVT)**, which would typically cause unilateral leg swelling, warmth, and tenderness.
- The patient has **bilateral pitting edema** with no erythema or tenderness, making DVT less likely as the primary cause of her symptoms.
*Reassurance and monitoring*
- Given the patient's significant and worsening symptoms (**dyspnea, S3 gallop, widespread edema**), simply reassuring her and monitoring would be inappropriate and could lead to delayed diagnosis and treatment of a serious cardiac condition.
- These symptoms are beyond the normal physiological changes of pregnancy and warrant urgent investigation.
Cardiac disease in pregnancy US Medical PG Question 2: A 27-year-old P1G1 who has had minimal prenatal care delivers a newborn female infant. Exam reveals a dusky child who appears to be in distress. Her neck veins are distended and you note an enlarged v wave. She has a holosystolic murmur. Following echocardiogram, immediate surgery is recommended.
For which of the following conditions was the mother likely receiving treatment during pregnancy?
- A. Bipolar disorder (Correct Answer)
- B. Hypothyroidism
- C. Depression
- D. Hypertension
- E. Diabetes
Cardiac disease in pregnancy Explanation: ***Bipolar disorder***
- The newborn's symptoms, including a **holosystolic murmur**, **distended neck veins** with an **enlarged v wave**, and cyanosis, are highly suggestive of **Ebstein's anomaly**.
- **Ebstein's anomaly** is a congenital heart defect strongly associated with maternal **lithium use** during pregnancy, a common treatment for bipolar disorder.
*Hypothyroidism*
- Maternal hypothyroidism is associated with an increased risk of miscarriage, stillbirth, and neurodevelopmental problems in the child, but not specifically with Ebstein's anomaly.
- Treatment for hypothyroidism primarily involves thyroid hormone replacement, which is not linked to this specific cardiac defect.
*Depression*
- While various antidepressant medications can be taken during pregnancy, none are specifically linked to Ebstein's anomaly.
- Maternal depression itself can impact fetal development due to stress, but not typically through this specific congenital heart defect.
*Hypertension*
- Maternal hypertension is associated with conditions like **pre-eclampsia**, fetal growth restriction, and preterm birth, but not specifically with Ebstein's anomaly.
- Antihypertensive medications generally do not cause this specific congenital heart defect.
*Diabetes*
- Maternal diabetes can lead to **macrosomia**, **hypoglycemia**, and an increased risk of various congenital anomalies, including **ventricular septal defects** and **transposition of the great arteries**.
- However, it is not specifically linked to Ebstein's anomaly, which is more characteristic of lithium exposure.
Cardiac disease in pregnancy US Medical PG Question 3: A 39-year-old woman, gravida 5, para 4, at 41 weeks' gestation is brought to the hospital because of regular uterine contractions that started 2 hours ago. Pregnancy has been complicated by iron deficiency anemia treated with iron supplements. Pelvic examination shows the cervix is 90% effaced and 7-cm dilated; the vertex is at -1 station. Fetal heart tracing is shown. The patient is repositioned, O2 therapy is initiated, and amnioinfusion is done. A repeat assessment after 20 minutes shows a similar cervical status, and no changes in the fetal heart tracing, and less than 5 contractions in a period of 10 minutes.What is the most appropriate next step in management?
- A. Emergent cesarean delivery (Correct Answer)
- B. Monitor without intervention
- C. Begin active pushing
- D. Retry maternal repositioning
- E. Administer tocolytics
Cardiac disease in pregnancy Explanation: ***Emergent cesarean delivery***
- The fetal heart tracing shows **recurrent late decelerations** unresponsive to **intrauterine resuscitation** (repositioning, O2, amnioinfusion), indicating fetal distress and uteroplacental insufficiency.
- Given the fetal distress and persistent late decelerations despite interventions, **expedited delivery** via cesarean section is indicated to prevent further fetal compromise.
*Monitor without intervention*
- This approach is inappropriate as the fetal heart tracing indicates **fetal distress** with recurrent **late decelerations** that have not resolved with initial interventions.
- Continued monitoring without action would place the fetus at risk for **hypoxia** and acidosis.
*Begin active pushing*
- The cervix is 7-cm dilated, meaning the patient is still in the **active phase of labor** and has not reached **complete cervical dilation** (10 cm) necessary for effective pushing.
- Pushing at this stage is unlikely to resolve the fetal distress and can potentially worsen **fetal acidosis** and maternal exhaustion.
*Retry maternal repositioning*
- The patient has already been repositioned and received other intrauterine resuscitation measures (O2 therapy, amnioinfusion) without improvement in the fetal heart tracing.
- Repeated repositioning alone is unlikely to resolve the underlying cause of the **late decelerations** in this context.
*Administer tocolytics*
- Tocolytics are used to **reduce uterine contractions** and manage conditions like **uterine tachysystole** or arrested labor, which are not explicitly present as the primary problem here (less than 5 contractions in 10 minutes).
- While they can temporarily improve uterine blood flow, they do not address the persistent **fetal distress** indicated by the recurrent late decelerations unresponsive to other interventions.
Cardiac disease in pregnancy US Medical PG Question 4: A 34-year-old primigravida presents with progressive shortness of breath on exertion and while sleeping. The patient says that she uses 2 pillows to breathe comfortably while sleeping at night. These symptoms started in the 3rd week of the 2nd trimester of pregnancy. She does not have any chronic health problems. She denies smoking and alcohol intake. Vital signs include: blood pressure 110/50 mm Hg, temperature 36.9°C (98.4°F), and regular pulse 90/min. Previous physical examination in the 1st trimester had disclosed no cardiac abnormalities, but on current physical examination, she has a loud S1 and a 2/6 diastolic rumble over the cardiac apex. A transthoracic echocardiogram shows evidence of mitral valve stenosis. Which of the following is the best initial treatment for this patient?
- A. Loop diuretics
- B. Percutaneous mitral balloon valvotomy (PMBV) (Correct Answer)
- C. Valve replacement
- D. Open valve commissurotomy
- E. No therapy is required
Cardiac disease in pregnancy Explanation: **Percutaneous mitral balloon valvotomy (PMBV)**
- This patient presents with **symptomatic mitral stenosis** during the second trimester of pregnancy, evidenced by progressive **shortness of breath, orthopnea**, and characteristic findings of a **loud S1 and diastolic rumble**. Due to the high risk of **maternal and fetal complications** with continued severe symptoms, an intervention is necessary.
- **PMBV** is the **preferred initial treatment for symptomatic severe mitral stenosis** in pregnant patients with suitable valve morphology who are not responding to medical therapy because it is less invasive than surgery and generally well-tolerated.
*Loop diuretics*
- While **loop diuretics** can help manage **pulmonary congestion** and **dyspnea** by reducing preload, they are a **symptomatic treatment** and do not address the underlying mechanical obstruction of mitral stenosis.
- In a patient with severe, progressive symptoms of mitral stenosis during pregnancy, medical therapy alone is often insufficient, and definitive intervention is required.
*Valve replacement*
- **Surgical valve replacement** is a **major invasive procedure** with significant risks to both the mother and fetus, including higher rates of miscarriage, prematurity, and maternal mortality.
- It is typically reserved for cases where PMBV is not feasible or has failed, or if there are other concomitant cardiac lesions requiring surgical correction.
*Open valve commissurotomy*
- **Open valve commissurotomy** is a surgical procedure that is more invasive than PMBV and carries similar risks as valve replacement for a pregnant patient.
- It is generally considered when **PMBV is contraindicated** due to unsuitable valve anatomy or has been unsuccessful, and surgical intervention is deemed necessary.
*No therapy is required*
- This patient's symptoms are **progressive and significantly impacting her quality of life**, indicating that medical intervention is necessary to prevent further decompensation and improve maternal and fetal outcomes.
- Untreated symptomatic mitral stenosis in pregnancy can lead to severe complications such as **pulmonary edema, heart failure, and maternal/fetal mortality**.
Cardiac disease in pregnancy US Medical PG Question 5: A 27-year-old woman G2P1 at 34 weeks estimated gestational age presents with bouts of sweating, weakness, and dizziness lasting a few minutes after lying down on the bed. She says symptoms resolve if she rolls on her side. She reports that these episodes have occurred several times over the last 3 weeks. On lying down, her blood pressure is 90/50 mm Hg and her pulse is 50/min. When she rolls on her side, her blood pressure slowly increases to 120/65 mm Hg, and her pulse increases to 72/min. Which of the following best describes the mechanism which underlies this patient’s most likely condition?
- A. Peripheral vasodilation
- B. Increase in plasma volume
- C. Progesterone surge
- D. Renin-angiotensin system activation
- E. Aortocaval compression (Correct Answer)
Cardiac disease in pregnancy Explanation: ***Aortocaval compression***
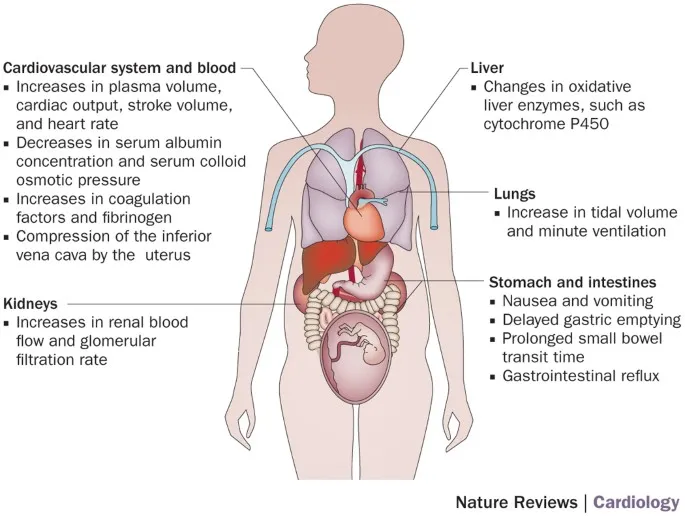
- This condition, also known as **supine hypotensive syndrome**, occurs when the gravid uterus **compresses the inferior vena cava (IVC)** and potentially the aorta, reducing **venous return** to the heart.
- The symptoms (sweating, weakness, dizziness, hypotension, bradycardia) and their resolution upon changing position are classic signs of reduced cardiac output due to IVC compression.
*Peripheral vasodilation*
- While **peripheral vasodilation** does occur in pregnancy due to hormonal changes, it generally contributes to a **mild decrease in systemic vascular resistance** and is not the primary mechanism behind acute, position-dependent hypotensive episodes.
- It would not explain the sudden, severe symptoms that resolve promptly with a change in position, nor the associated bradycardia which is more indicative of a **vasovagal response** to decreased cardiac filling.
*Increase in plasma volume*
- Pregnancy is associated with a significant **increase in plasma volume** (up to 50%), which is a physiological adaptation to support the uteroplacental unit.
- An increase in plasma volume would generally help **maintain blood pressure** and prevent hypotension, rather than causing the specific symptoms described in this patient.
*Progesterone surge*
- **Progesterone levels do increase significantly** during pregnancy and contribute to **smooth muscle relaxation**, which can lead to vasodilation.
- However, a progesterone surge itself does not directly cause acute, position-dependent hypotensive episodes; its vasodilatory effects are more chronic and physiological.
*Renin-angiotensin system activation*
- The **renin-angiotensin system (RAS) is typically activated** and upregulated during pregnancy, contributing to fluid balance and blood pressure regulation.
- Activation of the RAS would generally lead to **vasoconstriction and increased blood pressure**, not the hypotensive episodes observed in this patient.
Cardiac disease in pregnancy US Medical PG Question 6: A 44-year-old woman with high blood pressure and diabetes presents to the outpatient clinic and informs you that she is trying to get pregnant. Her current medications include lisinopril, metformin, and sitagliptin. Her blood pressure is 136/92 mm Hg and heart rate is 79/min. Her physical examination is unremarkable. What should you do regarding her medication for high blood pressure?
- A. Discontinue lisinopril and initiate aliskiren
- B. Discontinue lisinopril and initiate labetalol (Correct Answer)
- C. Continue her current regimen
- D. Continue her current regimen and add a beta-blocker for increased control
- E. Discontinue lisinopril and initiate candesartan
Cardiac disease in pregnancy Explanation: ***Discontinue lisinopril and initiate labetalol***
- **Lisinopril**, an ACE inhibitor, is **teratogenic** and is contraindicated in pregnancy due to the risk of fetal renal dysfunction, oligohydramnios, and neonatal death.
- **Labetalol** is a **beta-blocker** commonly used in pregnancy for hypertension as it is considered safe and effective in this population.
*Discontinue lisinopril and initiate aliskiren*
- **Aliskiren**, a direct renin inhibitor, is also **teratogenic** and contraindicated in pregnancy due to similar risks as ACE inhibitors and ARBs.
- Replacing one teratogenic drug with another does not solve the primary concern of fetal safety.
*Continue her current regimen*
- **Continuing lisinopril** would expose the fetus to significant risks, as it is a known teratogen.
- The patient is actively trying to conceive, making it imperative to switch medications immediately.
*Continue her current regimen and add a beta-blocker for increased control*
- Adding a beta-blocker while continuing lisinopril is still inappropriate because **lisinopril itself is harmful during pregnancy**.
- The primary goal is to **discontinue teratogenic medications**, not simply to improve blood pressure control with an additional drug.
*Discontinue lisinopril and initiate candesartan*
- **Candesartan**, an **angiotensin receptor blocker (ARB)**, shares the same **teratogenic risks** as ACE inhibitors and is contraindicated in pregnancy.
- Replacing an ACE inhibitor with an ARB provides no benefit in terms of fetal safety.
Cardiac disease in pregnancy US Medical PG Question 7: A 25-year-old woman, gravida 2, para 1, at 25 weeks' gestation comes to the emergency department because of a 1-day history of fever and right-sided flank pain. During this period, she also had chills, nausea, vomiting, and burning on urination. Her last prenatal visit was 10 weeks ago. Pregnancy and delivery of her first child were uncomplicated. Her temperature is 39°C (102.2°F), pulse is 110/min, respirations are 20/min, and blood pressure is 110/70 mm Hg. Physical examination shows costovertebral angle tenderness on the right. The abdomen is soft and nontender, and no contractions are felt. Pelvic examination shows a uterus consistent in size with a 25-week gestation. Fetal heart rate is 170/min. Laboratory studies show:
Leukocyte count 15,000/mm3
Urine
Nitrite 2+
Protein 1+
Blood 1+
RBC 5/hpf
WBC 500/hpf
Blood and urine samples are obtained for culture and drug sensitivity. Which of the following is the most appropriate next step in management?
- A. Inpatient treatment with intravenous ceftriaxone (Correct Answer)
- B. Perform a renal ultrasound
- C. Outpatient treatment with oral ciprofloxacin
- D. Inpatient treatment with intravenous ampicillin and gentamicin
- E. Admit the patient and request an emergent obstetrical consult
Cardiac disease in pregnancy Explanation: ***Inpatient treatment with intravenous ceftriaxone***
- The patient presents with classic signs of **pyelonephritis** (fever, flank pain, nausea, vomiting, CVA tenderness) in pregnancy, which warrants **inpatient admission** and **IV antibiotics** to prevent complications such as sepsis, preterm labor, and fetal compromise.
- **Ceftriaxone** is a broad-spectrum cephalosporin that is safe and effective in pregnancy for treating urinary tract infections, including pyelonephritis.
*Perform a renal ultrasound*
- While a **renal ultrasound** may be considered in cases of persistent fever after 48-72 hours of antibiotic therapy or if there's suspicion of obstruction or abscess, it is **not the immediate next step**.
- The priority is to initiate antibiotics promptly to treat the acute infection and prevent further complications.
*Outpatient treatment with oral ciprofloxacin*
- **Outpatient treatment** is inappropriate for **pyelonephritis in pregnancy** due to the high risk of complications for both the mother and the fetus.
- **Ciprofloxacin** (a fluoroquinolone) is generally **contraindicated in pregnancy** because of potential adverse effects on fetal cartilage development.
*Inpatient treatment with intravenous ampicillin and gentamicin*
- Although **ampicillin and gentamicin** are effective for many UTIs and safe in pregnancy, they are often reserved for cases where local resistance patterns favor this combination or as a second-line option.
- **Ceftriaxone** is a preferred first-line empiric choice for pyelonephritis in pregnancy due to its broad coverage and once-daily dosing.
*Admit the patient and request an emergent obstetrical consult*
- While admitting the patient is correct, **immediately requesting an emergent obstetrical consult** is premature as the primary issue is an acute infection requiring medical management.
- Obstetrics consultation is important in managing high-risk pregnancies or complications like preterm labor, but antibiotics for pyelonephritis should be initiated first, and then an obstetrician can be consulted for comanagement.
Cardiac disease in pregnancy US Medical PG Question 8: A 25-year-old woman presents to her physician with a missed mense and occasional morning nausea. Her menstrual cycles have previously been normal and on time. She has hypothyroidism resulting from Hashimoto thyroiditis diagnosed 2 years ago. She receives levothyroxine (50 mcg daily) and is euthyroid. She does not take any other medications, including birth control pills. At the time of presentation, her vital signs are as follows: blood pressure 120/80 mm Hg, heart rate 68/min, respiratory rate 12/min, and temperature 36.5℃ (97.7℉). The physical examination shows slight breast engorgement and nipple hyperpigmentation. The gynecologic examination reveals cervical softening and increased mobility. The uterus is enlarged. There are no adnexal masses. The thyroid panel is as follows:
Thyroid stimulating hormone (TSH) 3.41 mU/L
Total T4 111 nmol/L
Free T4 20 pmol/L
Which of the following adjustments should be made to the patient’s therapy?
- A. Increase levothyroxine dosage by 20%–30% (Correct Answer)
- B. Decrease levothyroxine dosage by 30%
- C. Discontinue levothyroxine
- D. The patient is euthyroid, so no adjustments should be made
- E. Increase levothyroxine dosage by 5% each week up to 50%
Cardiac disease in pregnancy Explanation: ***Increase levothyroxine dosage by 20%–30%***
- The patient's symptoms (missed menses, nausea, breast changes, enlarged uterus, cervical changes) are highly suggestive of **pregnancy**. During pregnancy, **thyroid hormone requirements increase significantly** due to increased levels of **thyroid-binding globulin (TBG)** stimulated by estrogen, and the production of **human chorionic gonadotropin (hCG)** which has TSH-like activity.
- The recommended management for pregnant women with hypothyroidism is to **increase the levothyroxine dose by approximately 25-50%** and monitor TSH and free T4 levels every 4-6 weeks to maintain a TSH level within the goal range for pregnancy (typically <2.5 mU/L in the first trimester).
*Decrease levothyroxine dosage by 30%*
- Decreasing levothyroxine would lead to **hypothyroidism**, which is detrimental in pregnancy and associated with adverse outcomes such as **preeclampsia**, **gestational hypertension**, **low birth weight**, and **neurocognitive impairment** in the offspring.
- Thyroid hormone requirements increase, not decrease, during pregnancy.
*Discontinue levothyroxine*
- **Discontinuing levothyroxine** would result in severe hypothyroidism, posing significant risks to both the mother and the developing fetus.
- Hypothyroidism must be treated throughout pregnancy to ensure proper fetal development.
*The patient is euthyroid, so no adjustments should be made*
- While the patient's thyroid panel currently shows euthyroid values (TSH 3.41 mU/L is within normal range but slightly elevated for first-trimester pregnancy goals), the **onset of pregnancy** rapidly increases thyroid hormone demand.
- Failure to adjust the dose can lead to **maternal and fetal hypothyroidism** as pregnancy progresses, even if the patient is currently euthyroid.
*Increase levothyroxine dosage by 5% each week up to 50%*
- A gradual increase of 5% each week may be too slow and insufficient to meet the rapidly increasing thyroid hormone demands of early pregnancy.
- The standard recommendation is to make a more substantial initial adjustment (20-30%) as soon as pregnancy is confirmed, followed by close monitoring and further adjustments.
Cardiac disease in pregnancy US Medical PG Question 9: A 28-year-old primigravida presents to the office with complaints of heartburn while lying flat on the bed at night and mild constipation that started a couple of weeks ago. She is 10 weeks pregnant, as determined by her last menstrual period. Her first menstruation was at 13 years of age and she has always had regular 28-day cycles. Her past medical history is insignificant. She does not smoke cigarettes or drink alcohol and does not take any medications. Her father died of colon cancer at 70 years of age, while her mother has diabetes and hypertension. Her vital signs include: temperature 36.9℃ (98.4℉), blood pressure 98/52 mm Hg, pulse 113/minute, oxygen saturation 99%, and respiratory rate 12 /minute. The physical examination was unremarkable, except for a diastolic murmur heard over the apex. Which of the following is considered abnormal in this woman?
- A. Decreased vascular resistance
- B. Diastolic murmur (Correct Answer)
- C. Tachycardia
- D. Increased cardiac output
- E. Low blood pressure
Cardiac disease in pregnancy Explanation: ***Diastolic murmur***
- Diastolic murmurs in pregnancy are **never normal** and always require further investigation to rule out significant **cardiac pathology**, such as valvular stenosis or regurgitation.
- While physiological changes in pregnancy can lead to systolic murmurs, **diastolic murmurs** are considered pathological.
*Decreased vascular resistance*
- **Peripheral vasodilation** due to hormonal changes (**progesterone**) is a normal physiological adaptation in early pregnancy, leading to decreased systemic vascular resistance.
- This decrease helps accommodate the **increased blood volume** and cardiac output, contributing to a slight drop in blood pressure.
*Tachycardia*
- An **increased heart rate** is a normal physiological response in pregnancy, typically seen as early as the first trimester.
- This compensatory mechanism helps maintain **cardiac output** in the face of decreased systemic vascular resistance and increased blood volume.
*Increased cardiac output*
- **Cardiac output increases** significantly during pregnancy, primarily due to increases in both heart rate and stroke volume, to meet the metabolic demands of the mother and fetus.
- This increase begins in the **first trimester** and peaks in the second trimester, remaining elevated until delivery.
*Low blood pressure*
- A **mild decrease in blood pressure**, particularly the diastolic pressure, is common in early pregnancy due to generalized vasodilation.
- The given blood pressure (98/52 mm Hg) is within the expected physiological range for a healthy pregnant woman in her first trimester.
Cardiac disease in pregnancy US Medical PG Question 10: A 33-year-old G1P0 at 32 weeks gestation presents to her OB/GYN for a prenatal check-up. Her medical history is significant for type II pregestational diabetes mellitus, which has been well-controlled with diet and insulin so far throughout her pregnancy. Which of the following is the recommended future follow-up for this patient?
- A. Twice weekly nonstress test now until delivery (Correct Answer)
- B. Ultrasound for fetal growth every week starting now until delivery
- C. Monthly biophysical profile now until delivery
- D. Monitor fetal kick counts starting now until 40 weeks gestation
- E. Monthly nonstress test starting at 34 weeks gestation until delivery
Cardiac disease in pregnancy Explanation: ***Twice weekly nonstress test now until delivery***
- For pregnant patients with **pregestational diabetes**, fetal surveillance with **twice-weekly nonstress tests (NSTs)** is recommended starting at 32 weeks gestation.
- This intensive monitoring helps detect potential **fetal compromise** due to risks associated with maternal diabetes, such as **placental insufficiency** or **macrosomia**.
*Ultrasound for fetal growth every week starting now until delivery*
- While **serial ultrasounds** for fetal growth are often performed in diabetic pregnancies, weekly ultrasounds are typically **not recommended** due to practical limitations and lack of clear evidence for improved outcomes.
- Fetal growth monitoring in diabetic pregnancies is more commonly performed every **2-4 weeks**, or as clinically indicated by other surveillance methods.
*Monthly biophysical profile now until delivery*
- A **biophysical profile (BPP)** is a comprehensive assessment of fetal well-being, but a **monthly frequency** is generally insufficient for high-risk conditions like pregestational diabetes, especially starting at 32 weeks.
- Furthermore, for patients with well-controlled diabetes, **NSTs** are often the initial and primary method of surveillance, with BPPs reserved for reassuring NSTs or specific clinical indications.
*Monitor fetal kick counts starting now until 40 weeks gestation*
- While **fetal kick counts** are a valuable tool for daily assessment of fetal well-being, they are often used as a **screening method** to prompt further evaluation, rather than the sole or primary method of formal antenatal surveillance in a high-risk pregnancy.
- They do not replace more objective and comprehensive tests like **NSTs** for a patient with pregestational diabetes.
*Monthly nonstress test starting at 34 weeks gestation until delivery*
- A **monthly nonstress test** is **insufficient** for a patient with pregestational diabetes, as the risk of fetal compromise is higher and requires more frequent monitoring.
- Additionally, waiting until **34 weeks gestation** to start surveillance is generally too late; current guidelines recommend initiation at **32 weeks gestation** in such cases.
More Cardiac disease in pregnancy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.