Viral vaccines US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Viral vaccines. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Viral vaccines US Medical PG Question 1: A 24-year-old woman with HIV infection comes to the physician for a follow-up examination. She has been inconsistently taking combined antiretroviral therapy for the past 5 years. She did not receive any childhood vaccinations because her parents were against them. During the consultation, the patient says that she wants to catch up on the missed vaccinations. Laboratory studies show a CD4+ T lymphocyte cell count of 180/mm3. Administration of the vaccine against which of the following agents should be avoided in this patient?
- A. Clostridium tetani
- B. Human papillomavirus
- C. Varicella zoster virus (Correct Answer)
- D. Bordetella pertussis
- E. Haemophilus influenzae
Viral vaccines Explanation: ***Varicella zoster virus***
- The **varicella zoster vaccine is a live attenuated vaccine**, which is generally contraindicated in individuals with severe **immunodeficiency**, such as HIV patients with a **CD4+ count below 200 cells/mm³**.
- Administering a live vaccine to an immunocompromised patient can lead to **uncontrolled viral replication** and potentially cause the disease it is meant to prevent.
*Clostridium tetani*
- The **tetanus vaccine** is a **toxoid vaccine**, meaning it contains inactivated bacterial toxins, not live organisms.
- It is **safe and recommended** for individuals with HIV, regardless of their CD4+ count, to provide protection against tetanus.
*Human papillomavirus*
- The **HPV vaccine** is a **recombinant vaccine**, consisting of viral-like particles (VLPs) and containing no live virus.
- It is **safe and recommended** for HIV-positive individuals and helps prevent HPV-related cancers.
*Bordetella pertussis*
- The **pertussis vaccine** (part of DTaP or Tdap) is an **acellular vaccine**, containing purified bacterial components, not live bacteria.
- It is **safe and recommended** for HIV patients to protect against whooping cough.
*Haemophilus influenzae*
- The **Haemophilus influenzae type b (Hib) vaccine** is a **conjugate vaccine**, made from bacterial capsular polysaccharide linked to a carrier protein.
- It is **safe and recommended** for HIV-positive individuals, as they are at increased risk for invasive Hib disease.
Viral vaccines US Medical PG Question 2: A 2-year-old boy is brought in by his parents to his pediatrician. The boy was born by spontaneous vaginal delivery at 39 weeks and 5 days after a normal pregnancy. The boy has received all age-appropriate vaccinations as of his last visit at 18 months of age. Of note, the boy has confirmed sickle cell disease and the only medication he takes is penicillin prophylaxis. The parents state that they plan on enrolling their son in a daycare, which requires documentation of up-to-date vaccinations. The pediatrician states that their son needs an additional vaccination at this visit, which is a polysaccharide vaccine that is not conjugated to protein. Which of the following matches this description?
- A. Pneumovax (Correct Answer)
- B. Menactra
- C. Prevnar
- D. Hib vaccine
- E. Live attenuated influenza vaccine
Viral vaccines Explanation: ***Pneumovax***
- **Pneumovax** (PCV23, PPSV23) is a **polysaccharide vaccine** that is not conjugated to a protein carrier. Children with **sickle cell disease** should receive this vaccine due to their immunocompromised state and increased risk of encapsulated bacterial infections.
- The Centers for Disease Control and Prevention (CDC) recommends PPSV23 for children aged 2 years and older with chronic medical conditions such as **sickle cell disease**, usually administered 8 weeks after their last PCV13 dose.
*Menactra*
- **Menactra** is a **quadrivalent meningococcal conjugate vaccine** (MCV4), meaning it contains a polysaccharide antigen conjugated to a protein carrier.
- This vaccine primarily targets *Neisseria meningitidis* and is different from the pneumococcal vaccine required here.
*Prevnar*
- **Prevnar** (PCV13) is a **pneumococcal conjugate vaccine**, meaning its polysaccharide antigens are conjugated to a protein carrier.
- While important for children with sickle cell disease, the question specifically asks for a vaccination that is a **polysaccharide vaccine that is not conjugated to protein**.
*Hib vaccine*
- The **Hib vaccine** (against *Haemophilus influenzae* type b) is a **conjugate vaccine**, meaning its polysaccharide capsule is linked to a protein carrier to enhance immunogenicity, particularly in infants.
- This vaccine is typically given earlier in childhood and is not the "additional" unconjugated polysaccharide vaccine described.
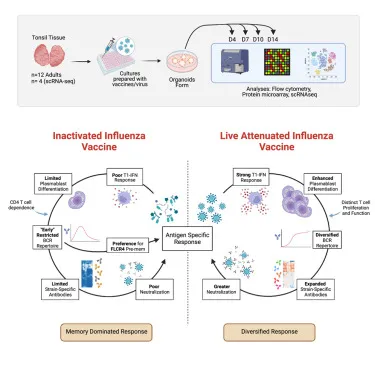
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is a live virus vaccine, not a polysaccharide vaccine.
- It is also contraindicated in individuals with certain immunocompromising conditions, such as some patients with sickle cell disease.
Viral vaccines US Medical PG Question 3: A young man about to leave for his freshman year of college visits his physician in order to ensure that his immunizations are up-to-date. Because he is living in a college dormitory, his physician gives him a vaccine that prevents meningococcal disease. What type of vaccine did this patient likely receive?
- A. Live, attenuated
- B. Killed, attenuated
- C. Toxoid
- D. Conjugated polysaccharide (Correct Answer)
- E. Killed, inactivated
Viral vaccines Explanation: ***Conjugated polysaccharide***
- The **meningococcal vaccine** commonly administered to college students is a **polysaccharide vaccine** wherein the polysaccharide antigens are conjugated to a protein carrier.
- This **conjugation** improves the immune response by converting a T-independent antigen into a T-dependent one, inducing better memory responses and allowing for vaccination of infants.
*Live, attenuated*
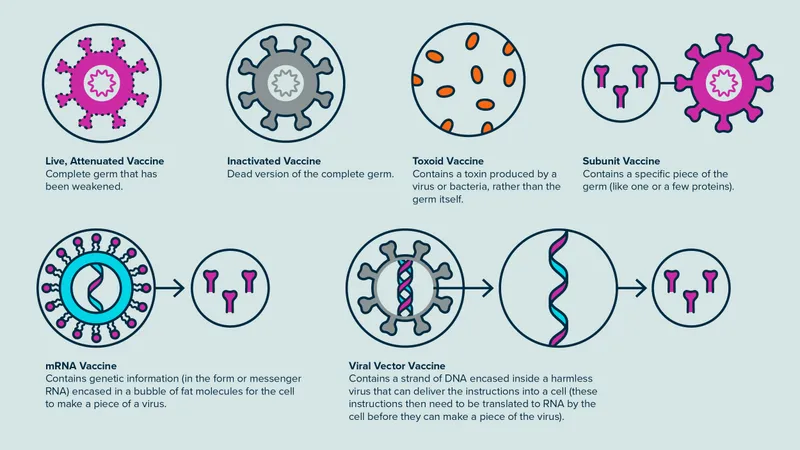
- Live, attenuated vaccines contain a **weakened form of the pathogen** that can replicate but does not cause disease, such as the MMR or varicella vaccine.
- While they elicit strong, long-lasting immunity, the meningococcal vaccine is not typically of this type due to the risk of opportunistic infection, especially in immunocompromised individuals.
*Killed, attenuated*
- This term is a **contradiction**; vaccines are either **killed (inactivated)** or **live (attenuated)**, but not both.
- Attenuation implies weakening, for which the organism would still be alive.
*Toxoid*
- **Toxoid vaccines** are made from inactivated bacterial toxins, used to protect against diseases where the toxin, not the bacterium itself, causes the disease, such as diphtheria and tetanus.
- Meningococcal disease is primarily caused by **direct bacterial invasion and inflammation**, not solely by a toxin.
*Killed, inactivated*
- **Killed, inactivated vaccines** contain whole pathogens that have been killed and cannot replicate, such as the inactivated poliovirus vaccine.
- While there are inactivated meningococcal vaccines, the most common type for broad use, especially in college settings, is the conjugated polysaccharide vaccine, which elicits a stronger and more long-lasting immune response against multiple serotypes compared to plain inactivated whole-cell vaccines.
Viral vaccines US Medical PG Question 4: A 9-month-old boy is brought to a pediatrician by his parents for routine immunization. The parents say they have recently immigrated to the United States from a developing country, where the infant was receiving immunizations as per the national immunization schedule for that country. The pediatrician prepares a plan for the infant’s immunizations as per standard US guidelines. Looking at the plan, the parents ask why the infant needs to be vaccinated with injectable polio vaccine, as he had already received an oral polio vaccine back in their home country. The pediatrician explains to them that, as per the recommended immunization schedule for children and adolescents in the United States, it is important to complete the schedule of immunizations using the injectable polio vaccine (IPV). He also mentions that IPV is considered safer than OPV, and IPV has some distinct advantages over OPV. Which of the following statements best explains the advantage of IPV over OPV to which the pediatrician is referring?
- A. IPV is known to produce higher titers of mucosal IgG antibodies than OPV
- B. IPV is known to produce virus-specific CD4+ T cells that produce interleukins and interferons to control polio viruses
- C. IPV is known to produce higher titers of mucosal IgA antibodies than OPV
- D. IPV is known to produce higher titers of serum IgG antibodies than OPV (Correct Answer)
- E. IPV is known to produce virus-specific CD8+ T cells that directly kill polio-infected cells
Viral vaccines Explanation: ***IPV is known to produce higher titers of serum IgG antibodies than OPV***
- The **injectable polio vaccine (IPV)** is an **inactivated vaccine** that primarily induces a systemic immune response, leading to high levels of **serum IgG antibodies**. These antibodies are crucial for preventing **viremia** and subsequently protecting against paralytic poliomyelitis.
- While OPV (oral polio vaccine) induces both mucosal and humoral immunity, IPV's strength lies in its ability to generate robust systemic immunity without the risk of vaccine-associated paralytic polio (VAPP), a rare but serious complication of OPV.
*IPV is known to produce higher titers of mucosal IgG antibodies than OPV*
- IPV primarily stimulates **systemic immunity** rather than strong mucosal immunity, meaning it does not typically produce higher titers of mucosal IgG antibodies than OPV.
- Mucosal immunity, especially IgA, is better stimulated by vaccines administered orally, like **OPV**, as it directly interacts with the gut-associated lymphoid tissue.
*IPV is known to produce virus-specific CD4+ T cells that produce interleukins and interferons to control polio viruses*
- Both IPV and OPV can induce **CD4+ T cell responses**, but this statement does not highlight a distinct advantage of IPV over OPV.
- While CD4+ T cells are important for immune coordination and antibody production, the primary advantage of IPV is its **safety profile** and systemic antibody levels, not necessarily a superior CD4+ T cell response.
*IPV is known to produce higher titers of mucosal IgA antibodies than OPV*
- **OPV**, being an oral vaccine, is highly effective at inducing a strong **mucosal IgA response** in the gut, which is important for preventing viral shedding and transmission.
- **IPV**, administered parenterally, produces minimal to no mucosal IgA response, making this statement incorrect.
*IPV is known to produce virus-specific CD8+ T cells that directly kill polio-infected cells*
- **Cytotoxic CD8+ T cells** are primarily involved in clearing cells infected with intracellular pathogens.
- While both vaccines may induce some cellular immunity, their primary mechanism for protecting against polio is through **neutralizing antibodies**, and the induction of CD8+ T cells is not the principal advantage of IPV over OPV.
Viral vaccines US Medical PG Question 5: A 2-month-old girl is brought to the physician by her father for a routine well-child examination. She is given a vaccine that contains polyribosylribitol phosphate conjugated to a toxoid carrier. The vaccine is most likely to provide immunity against which of the following pathogens?
- A. Haemophilus influenzae (Correct Answer)
- B. Neisseria meningitidis
- C. Bordetella pertussis
- D. Streptococcus pneumoniae
- E. Corynebacterium diphtheriae
Viral vaccines Explanation: **Haemophilus influenzae**
- The vaccine described, containing **polyribosylribitol phosphate (PRP)** conjugated to a toxoid carrier, is characteristic of the **Haemophilus influenzae type b (Hib) vaccine**.
- PRP is the **polysaccharide capsule** of *H. influenzae* type b, and conjugating it to a protein (toxoid carrier) allows for T-cell dependent immunity, effective in infants.
*Neisseria meningitidis*
- While *N. meningitidis* also has a **polysaccharide capsule** and vaccines are available, their capsular components differ (e.g., serogroups A, C, Y, W-135, or B outer membrane protein).
- The description of **polyribosylribitol phosphate** is specific to *H. influenzae* type b.
*Bordetella pertussis*
- Vaccines against *Bordetella pertussis* are typically **acellular pertussis vaccines (aP)**, which contain purified components like pertussis toxoid, filamentous hemagglutinin, and pertactin, not a PRP conjugate.
- These vaccines target bacterial toxins and adhesins, not a polysaccharide capsule unique to PRP.
*Streptococcus pneumoniae*
- Vaccines for *S. pneumoniae* (pneumococcal vaccines) use **capsular polysaccharides** from various serotypes, often conjugated to a protein carrier (e.g., diphtheria toxoid), but the specific polysaccharide is not PRP.
- The structure and serotypes of pneumococcal capsular polysaccharides are distinct from PRP.
*Corynebacterium diphtheriae*
- The vaccine for *C. diphtheriae* is the **diphtheria toxoid**, which is an inactivated form of the diphtheria toxin, not a polysaccharide conjugate.
- It provides immunity by inducing antibodies against the toxin, preventing its harmful effects.
Viral vaccines US Medical PG Question 6: A 1-year-old girl is brought to the physician for a well-child examination. She has no history of serious illness. She receives a vaccine in which a polysaccharide is conjugated to a carrier protein. Which of the following pathogens is the most likely target of this vaccine?
- A. Hepatitis A virus
- B. Varicella zoster virus
- C. Streptococcus pneumoniae (Correct Answer)
- D. Bordetella pertussis
- E. Clostridium tetani
Viral vaccines Explanation: ***Streptococcus pneumoniae***
- This pathogen is a common cause of **pneumonia**, **otitis media**, and **meningitis** in young children. The **pneumococcal conjugate vaccine (PCV)** targets *Streptococcus pneumoniae*'s polysaccharide capsule by conjugating it to a carrier protein.
- Conjugating the polysaccharide to a protein carrier allows for a **T-cell-dependent immune response**, which is crucial for eliciting a robust and long-lasting antibody response in infants and young children, whose immune systems are not yet mature enough to respond effectively to unconjugated polysaccharide antigens.
*Hepatitis A virus*
- The vaccine for **Hepatitis A virus** is an **inactivated vaccine** containing whole killed virus particles, not a polysaccharide conjugated to a carrier protein.
- It is typically given to children to prevent **Hepatitis A infection**, which causes liver inflammation.
*Varicella zoster virus*
- The **varicella vaccine** for **Varicella zoster virus** is a **live, attenuated vaccine**, meaning it contains a weakened form of the live virus.
- This vaccine aims to prevent **chickenpox** and is not a polysaccharide-protein conjugate vaccine.
*Bordetella pertussis*
- The vaccine for **Bordetella pertussis** (whooping cough) is part of the **DTaP vaccine** and is an **acellular vaccine**, containing purified components of the bacterium.
- These components are primarily **toxoids** (inactivated toxins) or other bacterial proteins, not polysaccharides.
*Clostridium tetani*
- The vaccine for **Clostridium tetani** is a **toxoid vaccine**, meaning it contains an inactivated form of the **tetanus toxin**.
- This is part of the **DTaP vaccine** and works by stimulating an immune response against the toxin, not bacterial polysaccharides.
Viral vaccines US Medical PG Question 7: A 35-year-old man is brought to the emergency department by his wife because of a 1-week history of progressive confusion, myalgia, and nausea. His wife says that he first reported headaches and fatigue 10 days ago, and since then “he has not been himself”. He has refused to drink any liquids for the last day. Two months ago, he helped his neighbor remove a raccoon's den from her backyard. He appears agitated. His temperature is 100.8°F (38.2°C). Examination shows excessive drooling. Muscle tone and deep tendon reflexes are increased bilaterally. Administration of which of the following is most likely to have prevented this patient's condition?
- A. Inosine monophosphate dehydrogenase inhibitor
- B. RNA-dependent DNA polymerase inhibitor
- C. Live attenuated vaccine
- D. Chemically-inactivated virus (Correct Answer)
- E. Immunoglobulin against a bacterial protein
Viral vaccines Explanation: ***Chemically-inactivated virus***
- This patient presents with symptoms highly suggestive of **rabies**, including progressive confusion, myalgias, agitation, excessive drooling, and increased muscle tone, following exposure to a raccoon.
- The rabies vaccine is a **chemically-inactivated virus** type that induces active immunity, and post-exposure prophylaxis with this vaccine (along with rabies immunoglobulin) would have prevented the disease.
*Inosine monophosphate dehydrogenase inhibitor*
- **Inosine monophosphate dehydrogenase inhibitors** (e.g., mycophenolate mofetil) are immunosuppressants used to prevent organ transplant rejection or treat autoimmune diseases.
- They do not have a role in preventing or treating viral infections like rabies.
*RNA-dependent DNA polymerase inhibitor*
- **RNA-dependent DNA polymerase inhibitors** (e.g., reverse transcriptase inhibitors) are mainly used in the treatment of **HIV infection**, a retrovirus that uses reverse transcriptase.
- Rabies virus is an RNA virus (rhabdovirus), but it does not use reverse transcriptase, and these inhibitors are not effective against it.
*Live attenuated vaccine*
- While many effective viral vaccines are **live attenuated** (e.g., MMR, varicella), the rabies vaccine used for post-exposure prophylaxis and prevention is not live attenuated, due to safety concerns.
- A live attenuated vaccine, if available and safe, would induce a strong immune response, but it is not the type of vaccine used for rabies in humans.
*Immunoglobulin against a bacterial protein*
- This describes antitoxins or immunoglobulins used against **bacterial infections** or their toxins (e.g., tetanus antitoxin).
- Rabies is a viral infection, and while passive immunization with **rabies immunoglobulin** is part of post-exposure prophylaxis, it is specific to the rabies virus and not a bacterial protein.
Viral vaccines US Medical PG Question 8: A parent presents to her pediatrician requesting information about immunizations for her newborn. The pediatrician explains about basic principles of immunization, types of vaccines, possible adverse effects, and the immunization schedule. Regarding how immunizations work, the pediatrician explains that there are mainly 2 types of vaccines. The first type of vaccine provides stronger and more lasting immunity as it induces both cellular and humoral immune responses. The second type of vaccine produces mainly a humoral response only, and its overall efficacy is less as compared to the first type. Which of the following vaccines belongs to the first type of vaccine that the pediatrician is talking about?
- A. Hepatitis A vaccine
- B. Polio vaccine (Salk)
- C. Yellow fever vaccine (Correct Answer)
- D. Rabies vaccine
- E. Hepatitis B vaccine
Viral vaccines Explanation: ***Yellow fever vaccine***
- The Yellow fever vaccine is a **live-attenuated vaccine**, which mimics natural infection and effectively stimulates both **cellular and humoral immune responses**, leading to strong and long-lasting immunity.
- Live-attenuated vaccines contain a weakened form of the pathogen, allowing for replication within the host and robust immune system activation.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is an **inactivated vaccine**, which primarily induces a **humoral (antibody-mediated) immune response**.
- Inactivated vaccines generally do not stimulate a strong cellular immune response and often require booster doses to maintain protective immunity.
*Polio vaccine (Salk)*
- The Salk polio vaccine is an **inactivated polio vaccine (IPV)**, meaning it contains killed viral particles.
- As an inactivated vaccine, it mainly elicits a **humoral immune response** producing circulating antibodies but less mucosal or cellular immunity.
*Rabies vaccine*
- The Rabies vaccine is an **inactivated vaccine** given after exposure or for pre-exposure prophylaxis.
- It primarily induces a **humoral antibody response** rather than a strong cellular immune response.
*Hepatitis B vaccine*
- The Hepatitis B vaccine is a **recombinant vaccine**, containing only a portion of the viral antigen (HBsAg).
- This type of vaccine primarily stimulates a **humoral immune response** leading to antibody production, which is effective but does not typically induce a strong cellular response like live vaccines.
Viral vaccines US Medical PG Question 9: A scientist performed an experiment to produce hybrid viruses by mixing two different serotypes of influenza virus, H1N1 and H2N2, in a respiratory epithelium cell line. Several days later, the scientist collected the media and analyzed the viral progeny. She found the following serotypes of virus: H1N1, H2N2, H1N2, and H2N1. Which of the following terms best explains the appearance of new serotypes?
- A. Phenotypic mixing
- B. Complementation
- C. Reassortment (Correct Answer)
- D. Transformation
- E. Recombination
Viral vaccines Explanation: ***Reassortment***
- **Reassortment** occurs in viruses with **segmented genomes**, like influenza, when a host cell is co-infected with two different viral strains.
- During replication, the progeny viruses can package segments from either parent, leading to novel combinations of surface proteins (**H** and **N** antigens), as seen with the emergence of H1N2 and H2N1.
*Phenotypic mixing*
- **Phenotypic mixing** involves the packaging of the genome of one virus into the capsid or envelope proteins derived from another virus, without genetic exchange.
- While progeny viruses might temporarily display characteristics of both parents, their genetic material remains unchanged, so subsequent generations would revert to the original serotype unless continuous co-infection occurs.
*Complementation*
- **Complementation** happens when one virus provides a functional protein that is deficient in another co-infecting virus, allowing the deficient virus to replicate.
- This process does not lead to the formation of new hybrid serotypes but rather allows a 'defective' virus to replicate alongside a 'helper' virus.
*Transformation*
- **Transformation** in microbiology typically refers to the uptake of foreign genetic material (DNA) by a bacterial cell, altering its genetic makeup.
- In virology, it can also refer to the process by which some viruses induce uncontrolled cell growth in eukaryotic cells, leading to oncogenesis, which is unrelated to the formation of hybrid serotypes.
*Recombination*
- **Recombination** involves the exchange of genetic material between two homologous chromosomes or DNA molecules, leading to a new genetic sequence.
- While it results in new genetic combinations, the term **reassortment** is specifically used for the exchange of entire genome segments characteristic of viruses like influenza.
Viral vaccines US Medical PG Question 10: A previously healthy 15-year-old girl is brought to the emergency department 24 hours after the onset of a severe headache. She returned from a 1-week camping trip 3 days ago; she went spelunking and swimming in a freshwater lake during the trip. She is agitated, uncooperative, and oriented only to person. Her temperature is 38.9°C (102°F), pulse is 112/min, respirations are 20/min, and blood pressure is 100/68 mm Hg. There are several crusted insect bites on her extremities. Neurologic examination shows diffuse hyperreflexia and an extensor plantar response bilaterally. Her neck is supple without lymphadenopathy. An MRI of the brain shows asymmetrical, bitemporal hyperintensities. A lumbar puncture is performed. Cerebrospinal fluid analysis shows:
Opening pressure 150 mm H2O
Glucose 58 mg/dL
Protein 108 mg/dL
Leukocyte count 150/mm3
Segmented neutrophils 15%
Lymphocytes 85%
Erythrocyte count 25/mm3
Which of the following is the most likely causal pathogen?
- A. Naegleria fowleri
- B. Herpes simplex virus (HSV) (Correct Answer)
- C. West Nile virus (WNV)
- D. Tick-borne encephalitis virus (TBEV)
- E. La Crosse virus (LACV)
Viral vaccines Explanation: ***Herpes simplex virus (HSV)***
- The combination of **bitemporal hyperintensities** on MRI, **agitation**, **uncooperativeness**, **fever**, and **lymphocytic pleocytosis** with elevated protein in the CSF is highly suggestive of **HSV encephalitis**. The history of a camping trip and insect bites is a distractor, but the MRI and CSF findings are classic for HSV.
- HSV encephalitis often presents with **focal neurologic deficits**, such as diffuse hyperreflexia and an extensor plantar response, and behavioral changes, reflecting the **temporal lobe involvement**.
*Naegleria fowleri*
- Causes **primary amebic meningoencephalitis**, which is rapidly fatal and typically associated with recent exposure to **warm freshwater**. While she went swimming in a freshwater lake, the MRI findings and CSF profile (lymphocytic predominance, moderate protein elevation) are not typical for Naegleria, which usually causes a **hemorrhagic necrosis** and often a **neutrophilic pleocytosis**.
- The disease progression with Naegleria fowleri is much more aggressive and rapid, usually leading to death within 3-7 days, and the MRI findings would often be more widespread.
*West Nile virus (WNV)*
- Transmitted by **mosquitoes** and can cause West Nile encephalitis, characterized by fever, headache, body aches, and sometimes a rash. However, WNV encephalitis typically does not show the characteristic **bitemporal hyperintensities** on MRI and often presents with more generalized encephalopathy or flaccid paralysis rather than focal temporal lobe findings.
- While CSF can show lymphocytic pleocytosis, the specific MRI findings are less consistent with WNV compared to HSV.
*Tick-borne encephalitis virus (TBEV)*
- Transmitted by **ticks** and is common in parts of Europe and Asia. It can cause encephalitis with fever, headache, and neurologic symptoms. However, it typically does not present with the specific **bitemporal hyperintensities** seen in this patient's MRI.
- The clinical picture, particularly the MRI findings and behavioral changes, is not a classic presentation for TBEV, which often has a more diffuse cerebral involvement.
*La Crosse virus (LACV)*
- Transmitted by **mosquitoes** and primarily affects children, causing encephalitis with fever, headache, nausea, and seizures. While it can cause an acute encephalitis, it typically does not feature the distinct **bitemporal hyperintensities** on MRI that are characteristic of HSV encephalitis.
- The geographic distribution of LACV is typically in the Midwestern and eastern United States, and while possible, the specific MRI pattern strongly points away from LACV.
More Viral vaccines US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.