Viral hemorrhagic fevers US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Viral hemorrhagic fevers. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Viral hemorrhagic fevers US Medical PG Question 1: A 43-year-old male visits the emergency room around 4 weeks after getting bitten by a bat during a cave diving trip. After cleansing the wound with water, the patient reports that he felt well enough not to seek medical attention immediately following his trip. He does endorse feeling feverish in the past week but a new onset of photophobia and irritability led him to seek help today. What would the post-mortem pathology report show if the patient succumbs to this infection?
- A. Howell-Jolly bodies
- B. Heinz bodies
- C. Psammoma bodies
- D. Pick bodies
- E. Negri bodies (Correct Answer)
Viral hemorrhagic fevers Explanation: ***Negri bodies***
- This patient's symptoms (fever, photophobia, irritability) and history of a bat bite point to rabies. **Negri bodies** are eosinophilic inclusions found in the cytoplasm of hippocampal and Purkinje cells in cases of rabies.
- They are **pathognomonic** for rabies infection and represent viral nucleocapsid proteins.
*Howell-Jolly bodies*
- These are **nuclear remnants** found in red blood cells that indicate impaired splenic function or asplenia.
- They are not associated with viral infections like rabies and are observed in conditions like sickle cell disease or after splenectomy.
*Heinz bodies*
- **Heinz bodies** are inclusions within red blood cells composed of denatured hemoglobin.
- They are typically seen in conditions involving **oxidative stress** to red blood cells, such as G6PD deficiency or alpha-thalassemia, not rabies.
*Psammoma bodies*
- These are **calcified, laminated, concentric spherules** found in some tumors (e.g., papillary thyroid carcinoma, meningioma, serous ovarian cystadenocarcinoma).
- They are a marker of specific neoplastic conditions and have no relevance to viral infections.
*Pick bodies*
- **Pick bodies** are aggregates of tau protein found in neurons, characteristic of **Pick's disease**, a type of frontotemporal dementia.
- They are neurodegenerative markers and are unrelated to infectious diseases.
Viral hemorrhagic fevers US Medical PG Question 2: A 25-year-old woman comes to the physician because of a 2-week history of episodic bleeding from the nose and gums and one episode of blood in her urine. She was treated with chloramphenicol 1 month ago for Rickettsia rickettsii infection. Her pulse is 130/min, respirations are 22/min, and blood pressure is 105/70 mm Hg. Examination shows mucosal pallor, scattered petechiae, and ecchymoses on the extremities. Laboratory studies show:
Hemoglobin 6.3 g/dL
Hematocrit 26%
Leukocyte count 900/mm3 (30% neutrophils)
Platelet count 50,000/mm3
The physician recommends a blood transfusion and informs her of the risks and benefits. Which of the following red blood cell preparations will most significantly reduce the risk of transfusion-related cytomegalovirus infection?
- A. Warming
- B. Irradiation
- C. Centrifugation
- D. Washing
- E. Leukoreduction (Correct Answer)
Viral hemorrhagic fevers Explanation: ***Leukoreduction***
- **Cytomegalovirus (CMV)** is primarily transmitted via **leukocytes** in blood products, as it is a latent infection within these cells.
- **Leukoreduction** removes most white blood cells, thereby significantly reducing the risk of CMV transmission, especially in immunocompromised patients or those at high risk.
*Warming*
- **Warming blood** to body temperature before transfusion helps prevent hypothermia in the recipient and reduces the risk of cardiac arrhythmias.
- It does not, however, have any significant effect on reducing the transmission of infectious agents like CMV.
*Irradiation*
- **Irradiation** of blood products inactivates donor T lymphocytes, preventing **transfusion-associated graft-versus-host disease (TA-GVHD)**, predominantly in immunocompromised recipients.
- It does not effectively remove or inactivate viruses like CMV that reside within cells.
*Centrifugation*
- **Centrifugation** is used to separate blood components based on their different densities (e.g., plasma, platelets, red blood cells).
- While it separates components, it does not specifically remove or inactivate CMV-infected white blood cells from the remaining red blood cell product in a manner that significantly reduces infection risk.
*Washing*
- **Washing red blood cells** with saline removes plasma proteins, antibodies, and some white blood cells, which can prevent allergic reactions to plasma proteins or hyperkalemia.
- While it may remove some leukocytes, it is generally less effective than leukoreduction for preventing CMV transmission and is primarily indicated for other specific transfusion reactions.
Viral hemorrhagic fevers US Medical PG Question 3: A previously healthy 25-year-old man comes to the physician because of a 4-day history of fever, joint and body pain, diffuse headache, and pain behind the eyes. This morning he noticed that his gums bled when he brushed his teeth. He returned from a backpacking trip to the Philippines 4 days ago. His temperature is 39.4°C (103.0°F). Physical examination shows a diffuse maculopapular rash. His leukocyte count is 3,200/mm3 and platelet count is 89,000/mm3. Further evaluation shows increased serum levels of a flavivirus. Which of the following is the most likely causal pathogen?
- A. Dengue virus (Correct Answer)
- B. Ebola virus
- C. Chikungunya virus
- D. Lassa virus
- E. Hantavirus
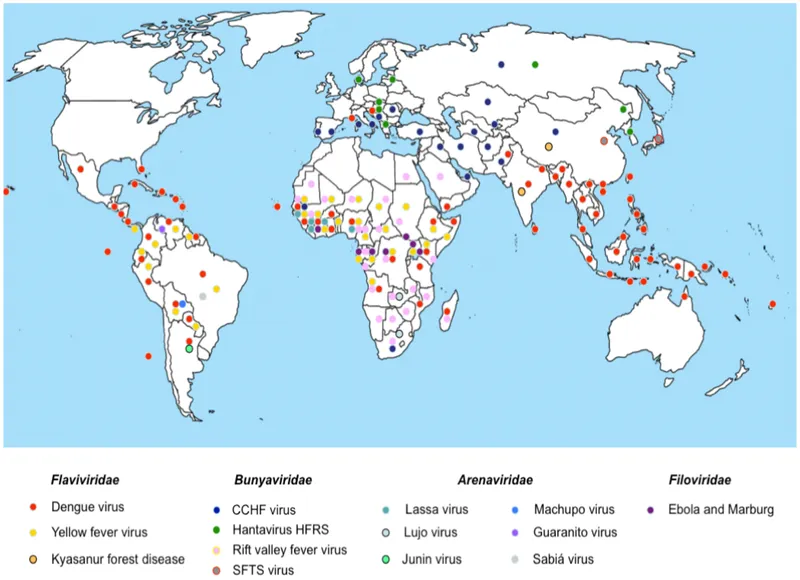
Viral hemorrhagic fevers Explanation: ***Dengue virus***
- The patient's symptoms (fever, joint/body pain, headache, **retro-orbital pain**, maculopapular rash, **thrombocytopenia**, **leukopenia**, and **gum bleeding**) are classic for **dengue fever**, especially with recent travel to an endemic area like the **Philippines**.
- **Dengue** is a **flavivirus** transmitted by *Aedes aegypti* mosquitoes, and the clinical picture, including hemorrhagic manifestations and positive flavivirus test, strongly points to this diagnosis.
- Importantly, the laboratory finding of **increased serum flavivirus levels definitively identifies this as dengue**, as none of the other options are flaviviruses.
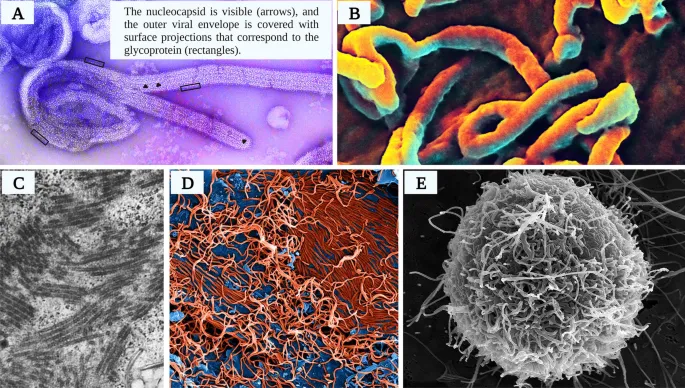
*Ebola virus*
- **Ebola is a filovirus, not a flavivirus**, which excludes it based on the laboratory findings.
- While Ebola causes hemorrhagic fever, it typically presents with more severe symptoms, including **profuse vomiting, diarrhea, and widespread internal and external bleeding**, which are not described in this case.
*Chikungunya virus*
- **Chikungunya is an alphavirus, not a flavivirus**, which excludes it based on the laboratory findings.
- **Chikungunya** also causes fever, rash, and joint pain, but is distinguished by more prominent and often **debilitating arthralgia** that can be chronic.
- **Hemorrhagic manifestations** like gum bleeding and severe thrombocytopenia are uncommon with Chikungunya and are more characteristic of dengue.
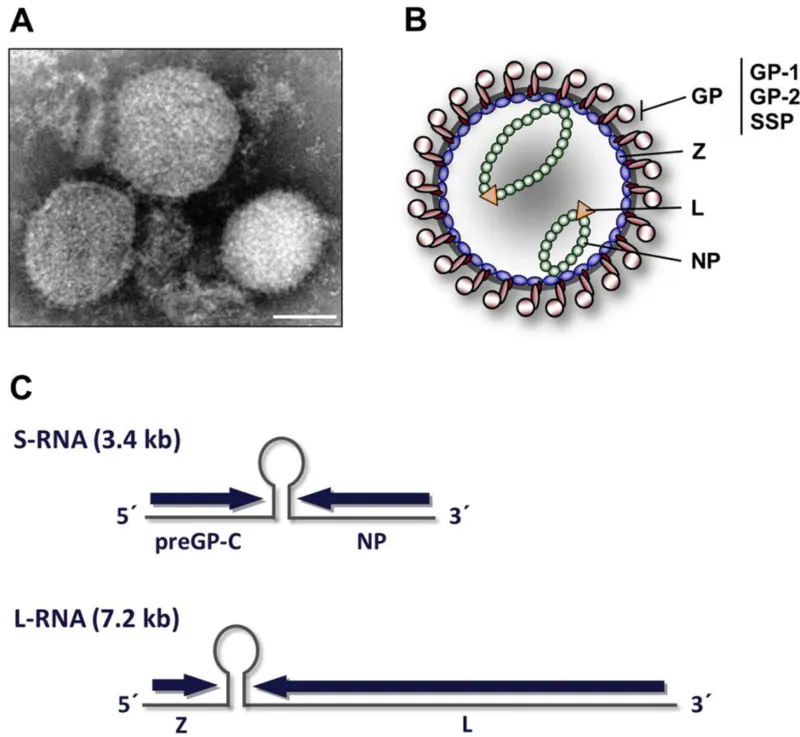
*Lassa virus*
- **Lassa is an arenavirus, not a flavivirus**, which excludes it based on the laboratory findings.
- **Lassa fever** is endemic to West Africa and presents with a gradual onset of fever, malaise, headache, and atypical rash, progressing to more severe manifestations like **facial edema** and **hemorrhage**.
- The geographic exposure (Philippines) does not align with Lassa virus endemicity.
*Hantavirus*
- **Hantavirus is a bunyavirus, not a flavivirus**, which excludes it based on the laboratory findings.
- **Hantavirus infections** can cause two main syndromes: **Hantavirus Pulmonary Syndrome (HPS)** with severe respiratory distress, or **Hemorrhagic Fever with Renal Syndrome (HFRS)**, which involves kidney failure and hemorrhagic manifestations.
- The patient's symptoms of retro-orbital pain, prominent rash, and specific lab findings (leukopenia, thrombocytopenia) are not typical for hantavirus, and there is no mention of severe respiratory or renal involvement.
Viral hemorrhagic fevers US Medical PG Question 4: A 30-year-old forest landscape specialist is brought to the emergency department with hematemesis and confusion. One week ago she was diagnosed with influenza when she had fevers, severe headaches, myalgias, hip and shoulder pain, and a maculopapular rash. After a day of relative remission, she developed abdominal pain, vomiting, and diarrhea. A single episode of hematemesis occurred prior to admission. Two weeks ago she visited rainforests and caves in western Africa where she had direct contact with animals, including apes. She has no history of serious illnesses or use of medications. She is restless. Her temperature is 38.0℃ (100.4℉); the pulse is 95/min, the respiratory rate is 20/min; and supine and upright blood pressure is 130/70 mm Hg and 100/65 mm Hg, respectively. Conjunctival suffusion is noted. Ecchymoses are observed on the lower extremities. She is bleeding from one of her intravenous lines. The peripheral blood smear is negative for organisms. Filovirus genomes were detected during a reverse transcription-polymerase chain reaction. The laboratory studies show the following:
Laboratory test
Hemoglobin 10 g/dL
Leukocyte count 1,000/mm3
Segmented neutrophils 65%
Lymphocytes 20%
Platelet count 50,000/mm3
Partial thromboplastin time (activated) 60 seconds
Prothrombin time 25 seconds
Fibrin split products positive
Serum
Alanine aminotransferase (ALT) 85 U/L
Aspartate aminotransferase (AST) 120 U/L
γ-Glutamyltransferase (GGT) 83 U/L
Creatinine 2 mg/dL
Which of the following is the most appropriate immediate step in management?
- A. Esophagogastroduodenoscopy
- B. Postexposure vaccination of close contacts
- C. Parenteral artesunate plus sulfadoxine/pyrimethamine
- D. Use of N95 masks
- E. Intravenous fluids and electrolytes (Correct Answer)
Viral hemorrhagic fevers Explanation: ***Intravenous fluids and electrolytes***
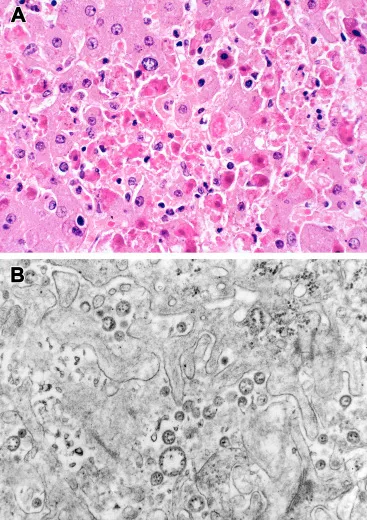
- The patient presents with **orthostatic hypotension**, internal bleeding (hematemesis, ecchymoses), and deranged renal function (elevated creatinine). These indicate significant **fluid loss** and potential **hypovolemic shock**, making immediate fluid resuscitation critical.
- **Ebola virus disease** (indicated by the travel history, symptoms, and positive filovirus genomes) often leads to severe dehydration due to fluid loss from vomiting, diarrhea, and internal bleeding, necessitating aggressive fluid and electrolyte replacement as a cornerstone of supportive care.
*Esophagogastroduodenoscopy*
- While the patient has hematemesis, her overall clinical picture with **severe coagulopathy** (elevated PT/aPTT, low platelets, positive fibrin split products) and **multisystem involvement** suggests a systemic bleeding disorder rather than a focal upper GI bleed that would be the primary target of an EGD.
- Performing an invasive procedure like EGD in a patient with severe coagulopathy and a highly contagious disease like Ebola (implied by filovirus detection) carries significant risks and is not the most immediate priority compared to stabilizing vital signs and correcting fluid deficits.
*Postexposure vaccination of close contacts*
- This is a crucial public health measure for **Ebola virus disease** but is a secondary step in management focused on prevention for others, not the immediate stabilization or treatment of the acutely ill patient.
- While important, it does not address the patient's immediate, life-threatening symptoms of hypovolemia, bleeding, and organ dysfunction.
*Parenteral artesunate plus sulfadoxine/pyrimethamine*
- This regimen is an antimalarial treatment. While the patient traveled to Western Africa, her symptoms and the detection of **filovirus genomes** rule out malaria as the primary diagnosis requiring this specific treatment.
- Administering antimalarials would delay appropriate supportive care for Ebola virus disease and is not indicated given the specific viral diagnosis.
*Use of N95 masks*
- **N95 masks** are important for healthcare worker protection given the patient's symptoms and confirmed filovirus. However, the question asks for the most appropriate *immediate step in management* of the patient's condition.
- While infection control is paramount, providing immediate direct patient care like fluid resuscitation takes precedence for the patient's survival over PPE considerations, assuming adequate PPE is already being donned by healthcare providers.
Viral hemorrhagic fevers US Medical PG Question 5: A 29-year-old man presents to the clinic complaining of fatigue and loss of sensation in his lower legs. The patient notes no history of trauma or chronic disease but states that he spends a lot of time outside and often encounters wild animals. On examination, the patient has multiple dark lesions over the skin of his face and back, as well as a decreased sensation of fine touch and vibration bilaterally in the lower extremities. What is the morphology of the etiologic agent causing this patient’s symptoms?
- A. An acid-fast, intracellular bacillus (Correct Answer)
- B. Reactivation of latent viral infection
- C. Maltose-fermenting gram-negative diplococci
- D. A spirochete transmitted via tick
- E. Gram-positive, branching anaerobe
Viral hemorrhagic fevers Explanation: ***An acid-fast, intracellular bacillus***
- The patient's symptoms (fatigue, loss of sensation in lower legs, dark skin lesions, exposure to wild animals, and decreased fine touch/vibration) are highly suggestive of **leprosy** (Hansen's disease).
- Leprosy is caused by **_Mycobacterium leprae_**, which is an **acid-fast, obligate intracellular bacillus** that preferentially infects macrophages and Schwann cells, leading to nerve damage and skin lesions.
*Reactivation of latent viral infection*
- While viral infections can cause neurological symptoms, the presentation with specific **dark skin lesions** and the history of exposure to **wild animals** (potentially armadillos, a reservoir for _M. leprae_) point away from a common latent viral reactivation.
- **Herpes zoster** (shingles) is a common reactivation of a latent viral infection (varicella-zoster virus), but it typically presents with a dermatomal rash and neuropathic pain rather than widespread dark lesions and bilateral sensory loss in the lower extremities.
*Maltose-fermenting gram-negative diplococci*
- **Maltose-fermenting gram-negative diplococci** describe **_Neisseria meningitidis_**, which causes meningitis.
- This organism primarily causes symptoms related to meningitis (fever, headache, neck stiffness), and does not typically present with the chronic sensory loss or characteristic skin lesions seen in this patient.
*A spirochete transmitted via tick*
- A **spirochete transmitted via a tick** refers to **_Borrelia burgdorferi_**, the causative agent of **Lyme disease**.
- Lyme disease presents with an **erythema migrans rash** (bull's-eye rash), joint pain, and neurological symptoms, but the skin lesions described here (multiple dark lesions) and the progressive sensory loss are not typical for Lyme disease.
*Gram-positive, branching anaerobe*
- A **gram-positive, branching anaerobe** describes **_Actinomyces_ species**, which cause **actinomycosis**.
- Actinomycosis typically presents with chronic abscesses and sinus tracts, often affecting the head and neck, thorax, or abdomen, and does not cause the diffuse sensory loss or skin lesions described in this case.
Viral hemorrhagic fevers US Medical PG Question 6: A 45-year-old male presents to the emergency room complaining of severe nausea and vomiting. He returned from a business trip to Nigeria five days ago. Since then, he has developed progressively worsening fevers, headache, nausea, and vomiting. He has lost his appetite and cannot hold down food or water. He did not receive any vaccinations before traveling. His medical history is notable for alcohol abuse and peptic ulcer disease for which he takes omeprazole regularly. His temperature is 103.0°F (39.4°C), blood pressure is 100/70 mmHg, pulse is 128/min, and respirations are 22/min. Physical examination reveals scleral icterus, hepatomegaly, and tenderness to palpation in the right and left upper quadrants. While in the examination room, he vomits up dark vomitus. The patient is admitted and started on multiple anti-protozoal and anti-bacterial medications. Serology studies are pending; however, the patient dies soon after admission. The virus that likely gave rise to this patient’s condition is part of which of the following families?
- A. Togavirus
- B. Flavivirus (Correct Answer)
- C. Calicivirus
- D. Hepevirus
- E. Bunyavirus
Viral hemorrhagic fevers Explanation: ***Flavivirus***
- The clinical presentation, including acute onset of **high fever**, headache, nausea, vomiting (**dark vomitus**), **scleral icterus**, and **hepatomegaly** following travel to Nigeria, is highly suggestive of **yellow fever**.
- Yellow fever is caused by the **yellow fever virus**, which is a **flavivirus** transmitted by mosquitoes, primarily *Aedes aegypti*.
*Togavirus*
- The Togavirus family includes viruses like **rubella virus** and **alphaviruses** (e.g., Eastern equine encephalitis virus).
- While some alphaviruses can cause fever and encephalitis, they typically do not present with the characteristic **hemorrhagic fever** and severe liver involvement seen in this case.
*Calicivirus*
- The Calicivirus family includes **Norovirus**, which is a common cause of **gastroenteritis** with vomiting and diarrhea.
- Norovirus infections are typically self-limiting and do not usually lead to the severe systemic symptoms, **jaundice**, or fatal outcome described here.
*Hepevirus*
- The Hepevirus family includes the **hepatitis E virus (HEV)**.
- HEV causes **acute viral hepatitis**, characterized by jaundice, nausea, and vomiting, but it rarely progresses to the rapid, severe, and fatal hemorrhagic form seen in this patient.
*Bunyavirus*
- The Bunyavirus family (now split into several families) includes viruses like Hantavirus and Rift Valley fever virus, which can cause **hemorrhagic fevers**.
- While some bunyaviruses are found in Africa, the specific constellation of symptoms, particularly the prominent **scleral icterus** and rapid progression to severe liver failure and death, is most consistent with **yellow fever**, a flavivirus.
Viral hemorrhagic fevers US Medical PG Question 7: A 57-year-old man presents to the emergency department for feeling weak for the past week. He states that he has felt much more tired than usual and has had a subjective fever during this time. The patient has a past medical history of IV drug use, hepatitis C, atrial fibrillation, cirrhosis, alcohol dependence, obesity, and depression. His temperature is 102°F (38.9°C), blood pressure is 157/98 mmHg, pulse is 110/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note a fatigued man with diffuse yellowing of his skin. Cardiopulmonary exam is notable for bibasilar crackles on auscultation. Abdominal exam is notable for abdominal distension, dullness to percussion, and a fluid wave. The patient complains of generalized tenderness on palpation of his abdomen. The patient is started on piperacillin-tazobactam and is admitted to the medical floor. On day 4 of his stay in the hospital the patient is afebrile and his pulse is 92/min. His abdominal tenderness is reduced but is still present. Diffuse yellowing of the patient's skin and sclera is still notable. The nurses notice bleeding from the patient's 2 peripheral IV sites that she has to control with pressure. A few new bruises are seen on the patient's arms and legs. Which of the following is the best explanation for this patient's condition?
- A. Decreased metabolism of an anticoagulant
- B. Worsening infection
- C. Decreased renal excretion of an anticoagulant
- D. Diffuse activation of the coagulation cascade (Correct Answer)
- E. Bacterial destruction
Viral hemorrhagic fevers Explanation: ***Diffuse activation of the coagulation cascade***
- The development of new bleeding and bruising in a patient with **sepsis** and **cirrhosis**, despite being afebrile, suggests disseminated intravascular coagulation (DIC), which involves diffuse activation of the coagulation cascade leading to consumption of clotting factors and platelets.
- While initial infection caused the patient's presentation, the subsequent bleeding indicates a progression to a **consumptive coagulopathy** rather than an ongoing or worsening infection alone.
*Decreased metabolism of an anticoagulant*
- The patient's history includes atrial fibrillation, which might suggest anticoagulant use; however, there is **no mention of active anticoagulant therapy**, and the widespread nature of bleeding points to a systemic coagulopathy.
- While liver disease can impair metabolism, the patient's symptoms are more consistent with a **primary clotting disorder** rather than an exaggerated effect of medication.
*Worsening infection*
- The patient's vital signs, specifically being **afebrile and having a reduced pulse**, indicate improvement in the immediate infectious response.
- While infection can lead to coagulopathy, the direct cause of bleeding is the **consumption of clotting factors** due to systemic activation, not simply a worsening of the infection itself.
*Decreased renal excretion of an anticoagulant*
- Similar to decreased metabolism, this option assumes the patient is on an anticoagulant and that renal impairment is contributing, neither of which is explicitly stated or the most proximal cause of the widespread bleeding.
- The patient's presentation is more indicative of a **consumptive process affecting multiple clotting factors** rather than delayed clearance of a single drug.
*Bacterial destruction*
- While bacteria can damage endothelial cells and trigger coagulation, "bacterial destruction" itself is not a direct explanation for the bleeding.
- The bleeding is a consequence of the **body's response to infection (sepsis)** leading to coagulation cascade activation and subsequent consumption of clotting factors.
Viral hemorrhagic fevers US Medical PG Question 8: A 16-year-old female presents to her pediatrician complaining of 2 weeks of fever and 1 week of swollen lumps in her left armpit. Upon examination of the left upper extremity, her physician notes the presence of a single papule which the patient claimed appeared one week ago. The patient started her first job at a pet store 2.5 weeks ago. Which of the following is the vector of transmission of the causative agent?
- A. Cats (Correct Answer)
- B. Rabbits
- C. Animal urine
- D. Parrots
- E. Armadillos
Viral hemorrhagic fevers Explanation: ***Cats***
- The combination of **fever**, **swollen lymph nodes** (lumps in the armpit), a **single papule**, and a recent history of working at a **pet store** strongly suggests **cat scratch disease**.
- **Cat scratch disease** is caused by *Bartonella henselae*, which is primarily transmitted to humans through the **scratch or bite of a cat**, especially kittens.
*Rabbits*
- Rabbits are known vectors for diseases like **tularemia**, which can cause fever and swollen lymph nodes.
- However, the typical presentation of tularemia often includes a more prominent **ulcerative lesion** at the site of inoculation, and the papule described is less characteristic.
*Animal urine*
- While animal urine can transmit diseases like **leptospirosis**, which can cause fever and various systemic symptoms, it typically does not present with a localized papule followed by regional lymphadenopathy in this manner.
- Exposure to animal urine usually occurs through contact with contaminated water or soil, and the pet store context points more towards direct animal contact.
*Parrots*
- Parrots are associated with **psittacosis** (parrot fever), caused by *Chlamydia psittaci*.
- Psittacosis primarily manifests as a **respiratory illness** (pneumonia) and does not typically present with a localized papule and regional lymphadenopathy.
*Armadillos*
- Armadillos are significant reservoirs for **Mycobacterium leprae**, the causative agent of **leprosy**.
- Leprosy has a very long incubation period and presents with skin lesions, nerve damage, and sometimes lymphadenopathy, but a 2-week onset and the described acute symptoms are inconsistent with leprosy.
Viral hemorrhagic fevers US Medical PG Question 9: A 32-year-old woman comes to the emergency department with a 2-day history of abdominal pain and diarrhea. She has had about 8 voluminous stools per day, some of which were bloody. She visited an international food festival three days ago. She takes no medications. Her temperature is 39.5°C (103.1°F), pulse is 90/min, and blood pressure is 110/65 mm Hg. Examination shows a tender abdomen, increased bowel sounds, and dry mucous membranes. Microscopic examination of the stool shows polymorphonuclear leukocytes. Stool culture results are pending. Which of the following most likely caused the patient's symptoms?
- A. Home-canned vegetables
- B. Yogurt dip
- C. Reheated rice
- D. Toxic mushrooms
- E. Omelette (Correct Answer)
Viral hemorrhagic fevers Explanation: **Omelette**
- The symptoms, including **bloody diarrhea**, fever, and exposure to an international food festival suggest a **bacterial infection**, likely from contaminated eggs (e.g., **Salmonella**).
- The presence of **polymorphonuclear leukocytes** in the stool indicates an **invasive bacterial infection**, consistent with salmonellosis.
*Home-canned vegetables*
- Poorly preserved home-canned vegetables are a classic cause of **botulism**, which presents with **neurological symptoms** (e.g., flaccid paralysis) and is not characterized by bloody diarrhea or fever.
- While it can cause gastrointestinal upset, bloody stools are not typical, and the primary concern is neurotoxicity due to **Clostridium botulinum toxin**.
*Yogurt dip*
- Yogurt is a dairy product, and contamination typically leads to **non-bloody diarrhea** and vomiting, often caused by bacteria like *Staphylococcus aureus* or *Bacillus cereus* producing enterotoxins.
- The symptoms would likely be less severe and lack the invasive features (bloody stools, fever, PMNs) seen in this patient.
*Reheated rice*
- Reheated rice is commonly associated with **Bacillus cereus** food poisoning, which typically causes either an emetic (vomiting) or diarrheal syndrome.
- The diarrhea caused by *Bacillus cereus* is usually **watery and non-bloody**, and it rarely presents with significant fever or invasive features like polymorphonuclear leukocytes in stool.
*Toxic mushrooms*
- Mushroom poisoning can present with a wide range of symptoms, including gastrointestinal distress (vomiting, diarrhea), but the presentation varies greatly depending on the mushroom species.
- **Bloody diarrhea** with fever and polymorphonuclear leukocytes in stool is not a typical hallmark of common toxic mushroom ingestions, which often involve hepatotoxicity or neurotoxicity.
Viral hemorrhagic fevers US Medical PG Question 10: A previously healthy 24-year-old woman comes to the physician because of a 1-day history of nausea and weakness. She is sexually active with 2 male partners and uses an oral contraceptive; she uses condoms inconsistently. Her last menstrual period was 4 days ago. Her temperature is 38.4°C (101°F). Physical examination shows right costovertebral angle tenderness. Pelvic examination is normal. Which of the following is the most likely cause of this patient's condition?
- A. Noninfectious inflammation of the bladder
- B. Ascending bacteria from the endocervix
- C. Decreased renal calcium reabsorption
- D. Decreased urinary pH
- E. Ascending bacteria from the bladder (Correct Answer)
Viral hemorrhagic fevers Explanation: ***Ascending bacteria from the bladder***
- The patient presents with **fever**, **nausea**, **weakness**, and **right costovertebral angle (CVA) tenderness**, which are classic symptoms of **acute pyelonephritis**.
- **Pyelonephritis** most commonly results from an **ascending urinary tract infection**, where bacteria (typically *E. coli*) from the bladder travel up the ureters to infect the kidneys.
- This accounts for approximately **95% of pyelonephritis cases** in young women.
*Noninfectious inflammation of the bladder*
- **Noninfectious cystitis** (interstitial cystitis) would not typically present with systemic symptoms like **fever** and **nausea**, or with **CVA tenderness**, which indicates kidney involvement.
- Bladder inflammation typically causes dysuria and frequency without systemic signs of infection.
*Ascending bacteria from the endocervix*
- **Ascending bacteria from the endocervix** can cause **pelvic inflammatory disease (PID)**, which presents with lower abdominal pain, cervical motion tenderness, and vaginal discharge.
- While PID can cause fever, the **normal pelvic examination** in this patient rules out this diagnosis, and PID **does not typically cause CVA tenderness**.
*Decreased renal calcium reabsorption*
- **Decreased renal calcium reabsorption** is associated with **hypercalciuria** and **nephrolithiasis** (kidney stones), which can present with acute flank pain if obstruction occurs.
- However, this condition does not explain the **fever** and systemic symptoms characteristic of an acute infectious process.
*Decreased urinary pH*
- **Decreased urinary pH** (acidic urine) can predispose to certain types of kidney stone formation but is not a direct cause of **pyelonephritis**.
- It does not explain the presence of **fever**, **CVA tenderness**, and systemic symptoms indicative of a bacterial kidney infection.
More Viral hemorrhagic fevers US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.