Antiviral agents and mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antiviral agents and mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antiviral agents and mechanisms US Medical PG Question 1: A 57-year-old man comes to the emergency department because he has been having problems seeing over the last week. He says that he has been seeing specks in his vision and his vision also becomes blurry when he tries to focus on objects. He says that he cannot recall anything that may have precipitated this; however, he has been homeless for several months. His CD4+ cell count is 27 cells/mL so he is started on a new medication. Notably, this drug has the following properties when mixed with various proteins:
Drug alone - drug remains unphosphorylated
Drug and HSV proteins - drug remains unphosphorylated
Drug and CMV proteins - drug remains unphosphorylated
Drug and human proteins - drug is phosphorylated
Which of the following drugs is most consistent with this set of findings?
- A. Cidofovir (Correct Answer)
- B. Oseltamivir
- C. Ganciclovir
- D. Acyclovir
- E. Foscarnet
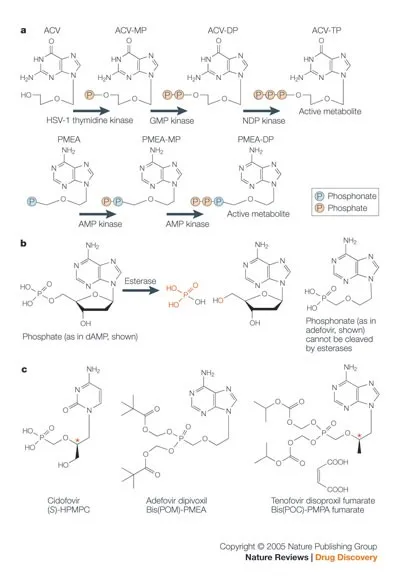
Antiviral agents and mechanisms Explanation: ***Cidofovir***
- The patient's presentation with **seeing specks and blurry vision** (floaters) along with a **CD4+ count of 27 cells/mL** strongly suggests **CMV retinitis**, a common opportunistic infection in advanced HIV/AIDS.
- **Cidofovir** is a nucleotide analog that **does NOT require viral kinases for activation** - it remains unphosphorylated when mixed with HSV or CMV proteins, as stated in the question.
- However, cidofovir **DOES require phosphorylation by host cellular kinases** (specifically cellular kinases, not viral kinases) to become the active triphosphate form. This matches the drug property showing it **becomes phosphorylated with human proteins**.
- This unique activation mechanism (host-dependent, viral-independent) distinguishes it from other antivirals and matches the experimental findings described.
*Foscarnet*
- **Foscarnet** is also used for CMV retinitis and **does NOT require ANY phosphorylation** - neither viral nor host enzymes.
- It acts as a **pyrophosphate analog** that directly inhibits viral DNA polymerase without requiring activation.
- The drug properties show phosphorylation occurs with human proteins, which is **inconsistent with foscarnet** that remains unphosphorylated under all conditions.
*Ganciclovir*
- **Ganciclovir** requires phosphorylation by **viral kinase UL97 in CMV** (or thymidine kinase in HSV) for initial activation, followed by host kinases.
- The drug properties state it remains unphosphorylated with CMV proteins, which is **inconsistent with ganciclovir's mechanism**.
*Acyclovir*
- **Acyclovir** is primarily used for **HSV and VZV infections**, not CMV retinitis in AIDS patients.
- It requires initial phosphorylation by **viral thymidine kinase** (HSV-TK), which contradicts the finding that it remains unphosphorylated with HSV proteins.
*Oseltamivir*
- **Oseltamivir** is a **neuraminidase inhibitor** used for **influenza treatment**.
- It has no role in CMV retinitis and does not act via phosphorylation-dependent DNA polymerase inhibition.
Antiviral agents and mechanisms US Medical PG Question 2: A 3-year-old recent immigrant is diagnosed with primary tuberculosis. Her body produces T cells that do not have IL-12 receptors on their surface, and she is noted to have impaired development of Th1 T-helper cells. Which of the following cytokines would benefit this patient?
- A. IL-4
- B. IL-22
- C. TGF-beta
- D. IL-17
- E. Interferon-gamma (Correct Answer)
Antiviral agents and mechanisms Explanation: ***Interferon-gamma***
- This patient has an impaired **Th1 response**, which is crucial for controlling intracellular infections like **tuberculosis** by activating macrophages.
- **Interferon-gamma** is the primary cytokine produced by **Th1 cells** that activates macrophages, leading to enhanced phagocytosis and killing of intracellular pathogens.
*IL-4*
- **IL-4** is a key cytokine produced by **Th2 cells**, which primarily drive **humoral immunity** and allergic responses, not cellular immunity against intracellular bacteria.
- Its administration would promote a **Th2 response**, which is not beneficial for combating **tuberculosis** and might even suppress the desirable Th1 response.
*IL-22*
- **IL-22** is mainly involved in **epithelial cell proliferation**, host defense at mucosal surfaces, and tissue repair.
- While it has a role in host defense against certain pathogens, it is not the primary cytokine required to compensate for a deficient **Th1 response** in **tuberculosis**.
*TGF-beta*
- **TGF-beta** is a pleiotropic cytokine with roles in cell growth, differentiation, and immune regulation, often acting as an **immunosuppressant** or driving **Treg differentiation**.
- It would not directly compensate for a lack of **Th1 cell function** needed to activate macrophages against **tuberculosis**.
*IL-17*
- **IL-17** is the signature cytokine of **Th17 cells**, which are important for host defense against **extracellular bacteria** and fungi, primarily by recruiting neutrophils.
- While it plays a role in some immune responses, it is not the crucial cytokine to boost in a patient with impaired **Th1 development** against **intracellular M. tuberculosis**.
Antiviral agents and mechanisms US Medical PG Question 3: An investigator is studying the effect of different cytokines on the growth and differentiation of B cells. The investigator isolates a population of B cells from the germinal center of a lymph node. After exposure to a particular cytokine, these B cells begin to produce an antibody that prevents attachment of pathogens to mucous membranes but does not fix complement. Which of the following cytokines is most likely responsible for the observed changes in B-cell function?
- A. Interleukin-5 (Correct Answer)
- B. Interleukin-6
- C. Interleukin-8
- D. Interleukin-2
- E. Interleukin-4
Antiviral agents and mechanisms Explanation: ***Interleukin-5***
- The antibody described (prevents pathogen attachment to mucous membranes, does not fix complement) is characteristic of **IgA**.
- **IL-5** plays a crucial role in promoting **IgA secretion** by differentiated B cells and supports B cell growth and differentiation in mucosal immunity.
- IL-5 works synergistically with **TGF-β** (the primary cytokine for IgA class switching) to enhance IgA production, particularly in mucosal-associated lymphoid tissue.
- Among the options provided, **IL-5 has the strongest association with IgA production**.
*Interleukin-4*
- **IL-4** is the primary cytokine driving class switching to **IgE** (and IgG4), not IgA.
- IL-4 is central to **allergic responses** and type 2 immunity, promoting B cells to produce IgE antibodies against allergens and parasites.
- It does not play a significant role in IgA production or mucosal immunity.
*Interleukin-6*
- **IL-6** is a pleiotropic cytokine involved in acute phase reactions, inflammation, and promoting B cell **differentiation into plasma cells**.
- While it supports general B cell maturation and antibody secretion, it is not specifically associated with **IgA production** or class switching.
*Interleukin-8*
- **IL-8** (CXCL8) is a **chemokine** that primarily recruits and activates neutrophils during inflammation.
- It has no direct role in B cell class switching or antibody production.
*Interleukin-2*
- **IL-2** is essential for T cell proliferation and differentiation, enhancing **cell-mediated immunity**.
- While it can indirectly affect B cell responses through T cell help, it is not directly responsible for promoting **IgA production** or class switching.
Antiviral agents and mechanisms US Medical PG Question 4: A 49-year-old man presents to a new primary care provider complaining of fatigue and occasional fever over the last month. These symptoms are starting to affect his job and he would like treatment. The physician runs a standard metabolic panel that shows elevated AST and ALT. The patient is then tested for hepatitis viruses. He is hepatitis C positive. The patient and his doctor discuss treatment options and agree upon pegylated interferon and oral ribavirin. Which side-effect is most likely while taking the ribavirin?
- A. Hemolytic anemia (Correct Answer)
- B. Leukopenia
- C. Rash
- D. Drug-associated lupus
- E. Hyperthyroidism
Antiviral agents and mechanisms Explanation: ***Hemolytic anemia***
- **Ribavirin** is a guanosine analog that causes **hemolytic anemia** by accumulating in red blood cells and disrupting their metabolism.
- This side effect is common and often dose-limiting, requiring close monitoring of hemoglobin levels.
*Leukopenia*
- **Leukopenia** (low white blood cell count) is a known side effect of **interferon therapy**, not primarily ribavirin.
- While patients on combination therapy may experience this, it's more directly attributable to the interferon component.
*Rash*
- **Rash** can occur with various medications, including combination hepatitis C therapy, but it is not a hallmark or most likely side effect specifically associated with **ribavirin**.
- It's generally less clinically significant than hemolytic anemia.
*Drug-associated lupus*
- **Drug-associated lupus** is a rare and severe reaction, sometimes linked to certain drugs like **hydralazine** or **procainamide**, but not typically associated with **ribavirin** or hepatitis C treatment.
- Its occurrence probability is much lower than hemolytic anemia.
*Hyperthyroidism*
- **Thyroid dysfunction**, including **hyperthyroidism** and hypothyroidism, is a known side effect of **interferon therapy**, due to its immunomodulatory effects.
- It is not a primary side effect of **ribavirin**.
Antiviral agents and mechanisms US Medical PG Question 5: A 49-year-old woman presents to her primary care doctor in late December with malaise. She reports worsening fatigue, myalgias, headache, and malaise that started 1 day ago. She works as a lunch lady at an elementary school. Her past medical history is notable for a distal radius fracture after a fall 2 years ago, but she is otherwise healthy and takes no medications. She does not smoke or drink alcohol. She is married and has 3 adult children who are healthy. Her temperature is 102.9°F (39.4°C), blood pressure is 101/61 mmHg, pulse is 112/min, and respirations are 21/min. On exam, she appears lethargic and uncomfortable but is able to answer questions appropriately. Breath sounds are normal bilaterally. She is started on intravenous fluids and a pharmacologic agent for treatment. Which of the following is the most likely mechanism of action of the drug being used to treat this patient?
- A. Neuraminidase inhibitor (Correct Answer)
- B. Reverse transcriptase inhibitor
- C. RNA-dependent polymerase inhibitor
- D. DNA polymerase inhibitor
- E. Protease inhibitor
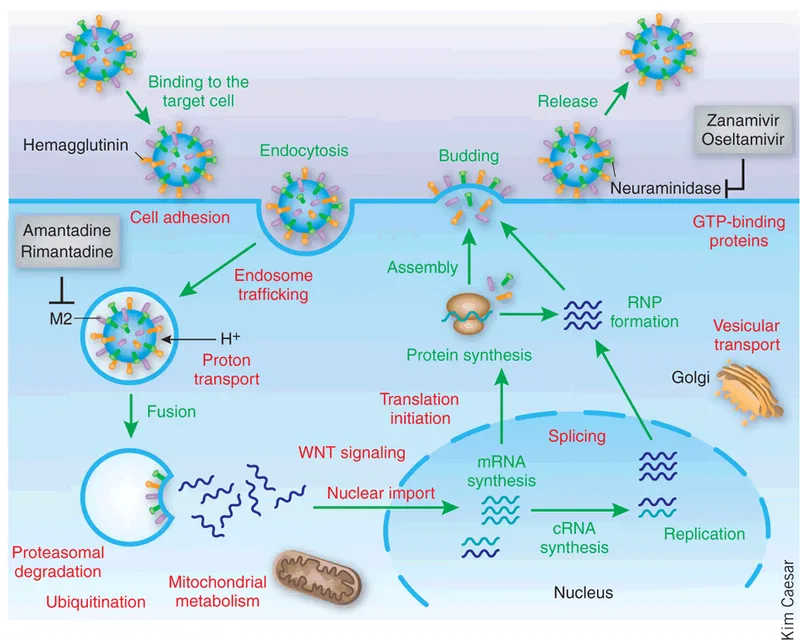
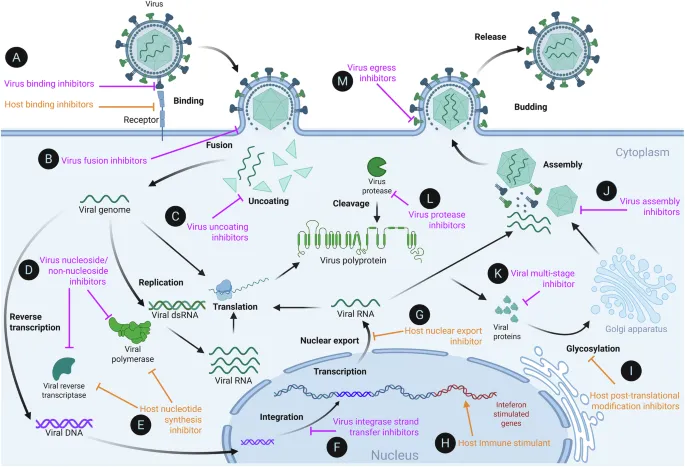
Antiviral agents and mechanisms Explanation: ***Neuraminidase inhibitor***
- The patient's symptoms (malaise, fatigue, myalgias, headache, fever) with rapid onset in **late December**, especially given her exposure to children in an elementary school, are highly suggestive of **influenza**.
- **Neuraminidase inhibitors** (e.g., oseltamivir, zanamivir) are the primary antiviral treatment for influenza, preventing the release of new viral particles from infected cells.
*Reverse transcriptase inhibitor*
- **Reverse transcriptase inhibitors** are primarily used in the treatment of **HIV infection**, which typically presents with a different constellation of symptoms and has a chronic rather than acute course.
- This class of drugs targets the enzyme **reverse transcriptase**, which is not central to the influenza virus replication cycle.
*RNA-dependent polymerase inhibitor*
- While **baloxavir marboxil** (an RNA polymerase inhibitor) is FDA-approved for influenza treatment, **neuraminidase inhibitors** remain the most commonly used first-line agents.
- In this clinical scenario without specific contraindications to neuraminidase inhibitors, oseltamivir or zanamivir would be the most likely agents prescribed.
*DNA polymerase inhibitor*
- **DNA polymerase inhibitors** are primarily used to treat **DNA viral infections** such as herpes viruses (e.g., acyclovir for HSV/VZV) or cytomegalovirus (e.g., ganciclovir).
- Influenza is an **RNA virus** and therefore does not have a DNA polymerase for replication.
*Protease inhibitor*
- **Protease inhibitors** are a class of antiviral drugs predominantly used in the treatment of **HIV** and **Hepatitis C virus** infections.
- Influenza viruses do not have a protease target that is typically inhibited by these drugs for therapeutic purposes.
Antiviral agents and mechanisms US Medical PG Question 6: A 35-year-old man comes to the physician because of a 6-month history of fatigue and increased sweating at night. He says that he feels “constantly tired” and needs more rest than usual although he sleeps well. In the morning, his sheets are often wet and his skin is clammy. He has not had any sore throat, runny nose, or cough recently. He has not traveled anywhere. Over the past 4 months, he has had a 6.8-kg (15-lb) weight loss, despite having a normal appetite. He does not drink or urinate more than usual. He is 181 cm (5 ft 11 in) tall and weighs 72 kg (159 lb); BMI is 22 kg/m2. His temperature is 37.9°C (100.2°F), pulse is 65/min, and blood pressure is 120/70 mm Hg. Physical examination shows no abnormalities. An HIV screening test and confirmatory test are both positive. The CD4 count is 600 cells/μl and the viral load is 104 copies/mL. Treatment with lamivudine, zidovudine, and indinavir is begun. The patient is at greatest risk for which of the following adverse effects?
- A. Urolithiasis (Correct Answer)
- B. Stevens-Johnson syndrome
- C. Hypersensitivity reaction
- D. Chronic kidney disease
- E. Pancreatitis
Antiviral agents and mechanisms Explanation: ***Urolithiasis***
- The patient is receiving **indinavir**, a protease inhibitor known to cause **nephrolithiasis** (kidney stones) due to the drug's poor solubility.
- Patients on indinavir should be well-hydrated to reduce the risk of stone formation.
*Stevens-Johnson syndrome*
- This severe skin reaction is more commonly associated with non-nucleoside reverse transcriptase inhibitors (NNRTIs) like **nevirapine** and **efavirenz**, or with sulfonamide antibiotics, rather than indinavir.
- While possible with many drugs, it is not the *greatest risk* among the options for this specific regimen.
*Hypersensitivity reaction*
- While hypersensitivity can occur with many drugs, particularly abacavir (an NRTI not included in this regimen), it is not the most prominent or specific adverse effect for the given combination, especially indinavir.
- Symptoms usually include fever, rash, and multi-organ involvement, which can be acute.
*Chronic kidney disease*
- While some antiretrovirals, particularly **tenofovir disoproxil fumarate (TDF)**, can cause renal tubular dysfunction and lead to chronic kidney disease, TDF is not part of this patient's regimen.
- Indinavir's primary renal complication is acute stone formation, not typically chronic kidney disease in the absence of pre-existing conditions or other nephrotoxic drugs.
*Pancreatitis*
- Pancreatitis is a known adverse effect of some NRTIs, particularly **didanosine** and **stavudine**, neither of which are in this patient's treatment plan.
- Lamivudine and zidovudine have a lower risk of pancreatitis compared to other NRTIs.
Antiviral agents and mechanisms US Medical PG Question 7: A 29-year-old female presents to her gynecologist complaining of a painful rash around her genitals. She has multiple sexual partners and uses condoms intermittently. Her last STD screen one year ago was negative. On examination, she has bilateral erosive vesicles on her labia majora and painful inguinal lymphadenopathy. She is started on an oral medication that requires a specific thymidine kinase for activation. Which of the following adverse effects is associated with this drug?
- A. Photosensitivity
- B. Deafness
- C. Renal failure (Correct Answer)
- D. Gingival hyperplasia
- E. Pulmonary fibrosis
Antiviral agents and mechanisms Explanation: ***Renal failure***
- The patient's symptoms (painful genital rash, erosive vesicles, inguinal lymphadenopathy) are highly suggestive of **herpes simplex virus (HSV) infection**, likely genital herpes.
- The drug described is an antiviral agent like **acyclovir, valacyclovir, or famciclovir**, which require **viral thymidine kinase** for activation and are known to cause **renal impairment** (nephrotoxicity) as an adverse effect, especially with high doses or in dehydrated patients due to crystal nephropathy.
*Photosensitivity*
- **Photosensitivity** is a common side effect of some antibiotics (e.g., tetracyclines, sulfonamides), diuretics (e.g., thiazides), and antifungals, but it is **not a prominent adverse effect of acyclovir or its derivatives**.
- While theoretical, it is not a clinically significant or frequently observed adverse effect associated with the class of antiviral drugs used for HSV.
*Deafness*
- **Ototoxicity**, leading to deafness or hearing loss, is a well-known adverse effect of certain classes of drugs, such as **aminoglycoside antibiotics** (e.g., gentamicin) and **loop diuretics** (e.g., furosemide).
- It is **not an adverse effect** associated with antiviral medications like acyclovir.
*Gingival hyperplasia*
- **Gingival hyperplasia** (overgrowth of gum tissue) is a recognized side effect of specific medications including **phenytoin** (an anticonvulsant), **cyclosporine** (an immunosuppressant), and **calcium channel blockers** (e.g., nifedipine, amlodipine).
- This adverse effect is **not associated with antiviral drugs** used to treat herpes simplex.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a serious adverse effect linked to various drugs like **amiodarone** (an antiarrhythmic), **bleomycin** (a chemotherapeutic agent), **methotrexate** (an immunosuppressant/chemotherapeutic), and **nitrofurantoin** (an antibiotic).
- **Antiviral medications for HSV** do not typically cause pulmonary fibrosis.
Antiviral agents and mechanisms US Medical PG Question 8: An HIV-positive patient with a CD4+ count of 45 is receiving recommended first-line treatment for a case of cytomegalovirus retinitis. Coadministration with which of the following agents would be most likely to precipitate a deficiency of neutrophils in this patient?
- A. Ritonavir
- B. Raltegravir
- C. Foscarnet
- D. Efavirenz
- E. Zidovudine (Correct Answer)
Antiviral agents and mechanisms Explanation: ***Zidovudine***
- **Zidovudine (AZT)** is a nucleoside reverse transcriptase inhibitor (NRTI) that is well-known for causing **myelosuppression**, particularly **neutropenia** and **anemia**.
- In an HIV-positive patient with a low **CD4+ count** and concurrent treatment for **CMV retinitis** (which often involves drugs like ganciclovir that can also cause myelosuppression), adding zidovudine significantly increases the risk of severe neutropenia.
*Ritonavir*
- **Ritonavir** is a protease inhibitor primarily known for its role as a **pharmacokinetic booster** in HIV therapy, enhancing the levels of other antiretrovirals.
- While it can cause gastrointestinal side effects and hepatotoxicity, **myelosuppression** and specifically neutropenia are not its primary or common adverse effects.
*Raltegravir*
- **Raltegravir** is an integrase strand transfer inhibitor (INSTI) generally well-tolerated with a favorable side effect profile.
- Common side effects include headache, nausea, and fatigue, but it is **not typically associated with significant myelosuppression** or neutropenia.
*Foscarnet*
- **Foscarnet** is an antiviral agent used for treating CMV retinitis, particularly in cases of ganciclovir resistance.
- Its major dose-limiting toxicities include **nephrotoxicity** and **electrolyte disturbances** (e.g., hypocalcemia, hypomagnesemia), not primarily neutropenia.
*Efavirenz*
- **Efavirenz** is a non-nucleoside reverse transcriptase inhibitor (NNRTI) associated with central nervous system side effects such as dizziness, insomnia, and vivid dreams.
- While skin rash and hepatotoxicity can occur, **bone marrow suppression** leading to neutropenia is not a characteristic or frequent adverse effect of efavirenz.
Antiviral agents and mechanisms US Medical PG Question 9: A 27-year-old dental radiographer presented to a clinic with red lesions on his palate, right lower and mid-upper lip, as well as one of his fingers. These lesions were accompanied by slight pain, and the patient had a low-grade fever 1 week before the appearance of the lesions. The patient touched the affected area repeatedly, which resulted in bleeding. Two days prior to his visit, he observed a small vesicular eruption on his right index finger, which merged with other eruptions and became cloudy on the day of the visit. He has not had similar symptoms previously. He did not report drug usage. A Tzanck smear was prepared from scrapings of the aforementioned lesions by the attending physician, and multinucleated epithelial giant cells were observed microscopically. According to the clinical presentation and histologic finding, which viral infection should be suspected in this case?
- A. Herpes simplex infection (Correct Answer)
- B. Varicella-zoster infection
- C. Measles
- D. Herpangina
- E. Hand-foot-and-mouth disease
Antiviral agents and mechanisms Explanation: ***Herpes simplex infection***
- The presence of **red lesions on the palate, lips, and finger**, along with **vesicular eruptions** that become cloudy and are accompanied by **pain** and a preceding **low-grade fever**, are classic signs of **herpes simplex virus (HSV) infection**.
- The histological finding of **multinucleated epithelial giant cells** on a **Tzanck smear** is highly characteristic of herpes virus infections, including HSV.
*Varicella-zoster infection*
- While **varicella-zoster virus (VZV)** also causes vesicular lesions and produces multinucleated giant cells, it typically presents with a **widespread rash** (chickenpox) or a **dermatomal distribution** (shingles), which is not described here.
- The patient's initial symptoms are more consistent with **primary herpes simplex infection**, particularly with the localized presentation.
*Measles*
- **Measles** presents with a characteristic **maculopapular rash** that starts on the face and spreads downwards, often preceded by **Koplik spots** in the mouth, and significant **catarrhal symptoms** (cough, coryza, conjunctivitis).
- It does not typically involve vesicular lesions or the presence of multinucleated giant cells on a Tzanck smear.
*Herpangina*
- **Herpangina** is characterized by painful **vesicles and ulcers localized to the posterior oropharynx** (soft palate, tonsillar pillars, uvula), typically caused by Coxsackieviruses.
- It does not usually affect the lips or fingers, and a Tzanck smear would not show multinucleated giant cells.
*Hand-foot-and-mouth disease*
- **Hand-foot-and-mouth disease (HFMD)** is caused by coxsackieviruses and presents with **vesicular lesions** on the **hands, feet, and oral cavity**, particularly the tongue and buccal mucosa.
- While oral lesions are present, the specific involvement of the palate and the characteristic Tzanck smear findings point away from HFMD.
Antiviral agents and mechanisms US Medical PG Question 10: A 16-year-old male presents to his pediatrician with a sore throat. He reports a severely painful throat preceded by several days of malaise and fatigue. He has a history of seasonal allergies and asthma. The patient is a high school student and is on the school wrestling team. He takes cetirizine and albuterol. His temperature is 100.9°F (38.3°C), blood pressure is 100/70 mmHg, pulse is 100/min, and respirations are 20/min. Physical examination reveals splenomegaly and posterior cervical lymphadenopathy. Laboratory analysis reveals the following:
Serum:
Na+: 145 mEq/L
K+: 4.0 mEq/L
Cl-: 100 mEq/L
HCO3-: 24 mEq/L
BUN: 12 mg/dL
Ca2+: 10.2 mg/dL
Mg2+: 2.0 mEq/L
Creatinine: 1.0 mg/dL
Glucose: 77 mg/dL
Hemoglobin: 17 g/dL
Hematocrit: 47%
Mean corpuscular volume: 90 µm3
Reticulocyte count: 1.0%
Platelet count: 250,000/mm3
Leukocyte count: 13,000/mm3
Neutrophil: 45%
Lymphocyte: 42%
Monocyte: 12%
Eosinophil: 1%
Basophil: 0%
Which of the following cell surface markers is bound by the pathogen responsible for this patient’s condition?
- A. CD3
- B. CD4
- C. CD21 (Correct Answer)
- D. CD20
- E. CD19
Antiviral agents and mechanisms Explanation: ***CD21***
- The patient's symptoms (sore throat, fatigue, splenomegaly, posterior cervical lymphadenopathy, and increased lymphocytes) are consistent with **infectious mononucleosis**, which is caused by the **Epstein-Barr virus (EBV)**.
- EBV primarily infects **B lymphocytes** by binding to the **CD21 receptor** (also known as the C3d complement receptor or CR2) on their surface.
*CD3*
- **CD3** is a protein complex found on the surface of **T lymphocytes**, associated with the T-cell receptor.
- EBV primarily targets B cells, not T cells, for initial infection and replication.
*CD4*
- **CD4** is a glycoprotein found on the surface of **helper T cells, monocytes, macrophages, and dendritic cells**.
- It is primarily known as the co-receptor for HIV entry into T cells.
*CD20*
- **CD20** is a transmembrane protein expressed on the surface of **B lymphocytes** from the pre-B cell stage through differentiated B cells, but not on plasma cells.
- While involved in B cell activation and a target for certain immunotherapies, it is not the primary receptor used by EBV for entry.
*CD19*
- **CD19** is another transmembrane glycoprotein expressed on the surface of **B lymphocytes** and is involved in B cell development, activation, and signaling.
- Although it's a B cell marker, **CD21** is the specific receptor that EBV uses for attachment and entry into B cells.
More Antiviral agents and mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.