Vaccine hesitancy and public health US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vaccine hesitancy and public health. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vaccine hesitancy and public health US Medical PG Question 1: A scientist in Chicago is studying a new blood test to detect Ab to EBV with increased sensitivity and specificity. So far, her best attempt at creating such an exam reached 82% sensitivity and 88% specificity. She is hoping to increase these numbers by at least 2 percent for each value. After several years of work, she believes that she has actually managed to reach a sensitivity and specificity much greater than what she had originally hoped for. She travels to China to begin testing her newest blood test. She finds 2,000 patients who are willing to participate in her study. Of the 2,000 patients, 1,200 of them are known to be infected with EBV. The scientist tests these 1,200 patients' blood and finds that only 120 of them tested negative with her new exam. Of the patients who are known to be EBV-free, only 20 of them tested positive. Given these results, which of the following correlates with the exam's specificity?
- A. 82%
- B. 90%
- C. 84%
- D. 86%
- E. 98% (Correct Answer)
Vaccine hesitancy and public health Explanation: ***98%***
- **Specificity** measures the proportion of **true negatives** among all actual negatives.
- In this case, 800 patients are known to be EBV-free (actual negatives), and 20 of them tested positive (false positives). This means 800 - 20 = 780 tested negative (true negatives). Specificity = (780 / 800) * 100% = **98%**.
*82%*
- This value represents the *original sensitivity* before the scientist’s new attempts to improve the test.
- It does not reflect the *newly calculated specificity* based on the provided data.
*90%*
- This value represents the *newly calculated sensitivity* of the test, not the specificity.
- Out of 1200 EBV-infected patients, 120 tested negative (false negatives), meaning 1080 tested positive (true positives). Sensitivity = (1080 / 1200) * 100% = 90%.
*84%*
- This percentage is not directly derived from the information given for either sensitivity or specificity after the new test results.
- It does not correspond to any of the calculated values for the new test's performance.
*86%*
- This percentage is not directly derived from the information given for either sensitivity or specificity after the new test results.
- It does not correspond to any of the calculated values for the new test's performance.
Vaccine hesitancy and public health US Medical PG Question 2: You have been asked to quantify the relative risk of developing bacterial meningitis following exposure to a patient with active disease. You analyze 200 patients in total, half of which are controls. In the trial arm, 30% of exposed patients ultimately contracted bacterial meningitis. In the unexposed group, only 1% contracted the disease. Which of the following is the relative risk due to disease exposure?
- A. (30 * 99) / (70 * 1)
- B. [30 / (30 + 70)] / [1 / (1 + 99)] (Correct Answer)
- C. [70 / (30 + 70)] / [99 / (1 + 99)]
- D. [[1 / (1 + 99)] / [30 / (30 + 70)]]
- E. (70 * 1) / (30 * 99)
Vaccine hesitancy and public health Explanation: ***[30 / (30 + 70)] / [1 / (1 + 99)]***
- This formula correctly calculates the **relative risk (RR)**. The numerator represents the **incidence rate in the exposed group** (30% of 100 exposed patients = 30 cases out of 100), and the denominator represents the **incidence rate in the unexposed group** (1% of 100 unexposed patients = 1 case out of 100).
- Relative risk is the ratio of the **risk of an event** in an **exposed group** to the **risk of an event** in an **unexposed group**.
*[(30 * 99) / (70 * 1)]*
- This formula is for calculating the **odds ratio (OR)**, specifically using a 2x2 table setup where 30 represents exposed cases, 70 represents exposed non-cases, 1 represents unexposed cases, and 99 represents unexposed non-cases.
- The odds ratio is a measure of association between an exposure and an outcome, representing the **odds of an outcome** given exposure compared to the odds of the outcome without exposure.
*[70 / (30 + 70)] / [99 / (1 + 99)]*
- This formula calculates the **relative risk of *not* developing the disease**, which is the inverse of what the question asks for.
- It compares the proportion of exposed individuals who *do not* contract the disease to the proportion of unexposed individuals who *do not* contract the disease.
*[[1 / (1 + 99)] / [30 / (30 + 70)]]*
- This formula calculates the **inverse of the relative risk**, which is not what the question asks for.
- It would represent the ratio of the incidence in the unexposed group to the incidence in the exposed group.
*[(70 * 1) / (30 * 99)]*
- This is an **incorrect variation** of the odds ratio calculation, with the terms in the numerator and denominator swapped compared to the standard formula.
- Therefore, it does not represent the relative risk or a correctly calculated odds ratio.
Vaccine hesitancy and public health US Medical PG Question 3: An 11-year-old boy is brought to his pediatrician by his parents for the routine Tdap immunization booster dose that is given during adolescence. Upon reviewing the patient’s medical records, the pediatrician notes that he was immunized according to CDC recommendations, with the exception that he received a catch-up Tdap immunization at the age of 8 years. When the pediatrician asks the boy’s parents about this delay, they inform the doctor that they immigrated to this country 3 years ago from Southeast Asia, where the child had not been immunized against diphtheria, tetanus, and pertussis. Therefore, he received a catch-up series at 8 years of age, which included the first dose of the Tdap vaccine. Which of the following options should the pediatrician choose to continue the boy’s immunization schedule?
- A. A single dose of Td vaccine at 18 years of age
- B. A single dose of Td vaccine now
- C. No further vaccination needed
- D. A single dose of Tdap vaccine now
- E. A single dose of Tdap vaccine at 13 years of age (Correct Answer)
Vaccine hesitancy and public health Explanation: ***A single dose of Tdap vaccine at 13 years of age***
- The CDC recommends a **minimum interval of 5 years** between Tdap doses when Tdap is given as part of a catch-up series.
- Since this patient received his first Tdap at age 8, the earliest he should receive the adolescent booster is at **age 13** (5 years later).
- This timing ensures adequate spacing while still providing the recommended adolescent booster for **pertussis, tetanus, and diphtheria** protection.
- The 5-year interval prevents excessive antigen exposure and optimizes immune response.
*A single dose of Tdap vaccine now*
- Giving Tdap now would result in only a **3-year interval** from the previous Tdap dose at age 8.
- This violates the CDC recommendation of a **minimum 5-year interval** between Tdap doses.
- Shorter intervals may increase local reactogenicity without improving protection.
*A single dose of Td vaccine now*
- While this would provide tetanus and diphtheria protection, it would **not protect against pertussis**, which is a critical component of adolescent vaccination.
- The Tdap vaccine is specifically recommended for adolescents to boost waning pertussis immunity.
- Additionally, giving it now would still be earlier than the recommended 5-year interval from the previous pertussis-containing vaccine.
*A single dose of Td vaccine at 18 years of age*
- This option would result in a **10-year gap** from the last pertussis-containing vaccine, leaving the adolescent vulnerable during high-risk years.
- The adolescent Tdap booster is specifically timed for ages 11-13 to protect during peak transmission periods in middle and high school.
- Waiting until 18 would miss the critical window for pertussis protection.
*No further vaccination needed*
- While the patient completed a catch-up series, the CDC still recommends an **adolescent Tdap booster** even for those who received Tdap in a catch-up series.
- The adolescent booster is important to maintain immunity against pertussis, which wanes significantly over time.
- The booster should be given at age 13 to maintain the 5-year minimum interval.
Vaccine hesitancy and public health US Medical PG Question 4: A 15-year-old female presents to her family physician for an annual school physical exam and check-up. She is accompanied by her mother to the visit and is present in the exam room. The patient has no complaints, and she does not have any past medical problems. She takes no medications. The patient reports that she remains active, exercising 5 times a week, and eats a healthy and varied diet. Which of the following would be the best way for the physician to obtain a more in-depth social history, including sexual history and use of alcohol, tobacco, or recreational drugs?
- A. Disallow the mother to be present in the examination room throughout the entirety of the visit
- B. Give the patient a social history questionnaire to fill out in the exam room
- C. Ask the mother to step outside into the hall for a portion of the visit (Correct Answer)
- D. Ask the patient the questions directly, with her mother still in the exam room
- E. Speak softly to the patient so that the mother does not hear and the patient is not embarrassed
Vaccine hesitancy and public health Explanation: ***Ask the mother to step outside into the hall for a portion of the visit***
- This approach allows the physician to speak with the adolescent **privately and confidentially**, which is crucial for obtaining sensitive information such as sexual history, drug use, and mental health concerns.
- Adolescents are more likely to disclose personal information when their parents are not present, fostering trust and ensuring **comprehensive history-taking** vital for their well-being.
*Disallow the mother to be present in the examination room throughout the entirety of the visit*
- This is an **overly restrictive** approach that might create tension or distrust between the physician, patient, and parent, especially at the start of the visit.
- While privacy is essential for sensitive topics, parental presence can be valuable for discussing general health, family history, and **treatment plans**, especially for younger adolescents.
*Give the patient a social history questionnaire to fill out in the exam room*
- While questionnaires can be useful for gathering basic information, they often **lack the nuance** of a direct conversation and may not prompt the patient to elaborate on sensitive issues.
- Furthermore, having the mother present while the patient fills out a questionnaire on sensitive topics still **compromises confidentiality** and may lead to incomplete or dishonest answers.
*Ask the patient the questions directly, with her mother still in the exam room*
- Asking sensitive questions with a parent present is **unlikely to yield truthful and complete answers**, as adolescents may feel embarrassed, judged, or fear parental disapproval.
- This approach compromises the **confidentiality** that is fundamental to building trust with adolescent patients.
*Speak softly to the patient so that the mother does not hear and the patient is not embarrassed*
- Speaking softly is **unprofessional** and still does not guarantee privacy, as the mother might still overhear parts of the conversation.
- This method also **fails to establish true confidentiality**, which is central to building rapport and encouraging open communication with adolescent patients about sensitive topics.
Vaccine hesitancy and public health US Medical PG Question 5: A 15-year-old girl is brought to the physician by her mother for an annual well-child examination. Her mother complains that the patient has a poor diet and spends most of the evening at home texting her friends instead of doing homework. She has been caught smoking cigarettes in the school bathroom several times and appears indifferent to the dean's threats of suspension. Two weeks ago, the patient allowed a friend to pierce her ears with unsterilized safety pins. The mother appeals to the physician to lecture the patient about her behavior and “set her straight.” The patient appears aloof and does not make eye contact. Her grooming is poor. Upon questioning the daughter about her mood, the mother responds “She acts like a rebel. I can't wait until puberty is over.” Which of the following is the most appropriate response?
- A. You should listen to your mother's concerns. You don't want to make poor choices early on or else you might end up on the streets.
- B. Would it be possible for you to step out for a few moments so that I can interview your daughter alone? (Correct Answer)
- C. Let's run a routine urine toxicology screen to make sure your daughter is not doing drugs.
- D. I am very concerned that your daughter is displaying signs of depression, and I'd suggest that she is seen by a psychiatrist.
- E. Your daughter displays normal signs of puberty. Being overly critical of your daughter is not helpful.
Vaccine hesitancy and public health Explanation: ***"Would it be possible for you to step out for a few moments so that I can interview your daughter alone?"***
- This approach respects the adolescent's **autonomy** and provides a safe space for her to disclose sensitive information without parental presence.
- Adolescents are more likely to be **candid** about risky behaviors like smoking, substance use, or sexual activity if they feel their privacy is protected.
*"You should listen to your mother's concerns. You don't want to make poor choices early on or else you might end up on the streets."*
- This response is **confrontational** and judgmental, which is likely to alienate the patient and shut down communication.
- It also uses **fear tactics** rather than fostering trust and a therapeutic relationship.
*"Let's run a routine urine toxicology screen to make sure your daughter is not doing drugs."*
- While drug use is a concern given her risky behaviors, immediately suggesting a **toxicology screen** without building rapport can feel accusatory and escalate distrust.
- It's often more effective to establish communication first before moving to definitive testing, especially in a well-child visit where drug use has not been directly admitted.
*"I am very concerned that your daughter is displaying signs of depression, and I'd suggest that she is seen by a psychiatrist."*
- While some of the patient's behaviors (poor grooming, aloofness, indifference) could be consistent with **depression**, immediately jumping to a diagnosis and referral without a direct interview is premature.
- It can also be perceived as labeling and might be rejected by the patient and mother without further exploration.
*"Your daughter displays normal signs of puberty. Being overly critical of your daughter is not helpful."*
- This response dismisses the mother's valid concerns about genuinely **risky behaviors** (smoking, unsterilized piercing, indifference to consequences) as "normal puberty."
- It also implicitly criticizes the mother, which can damage the therapeutic alliance with both the parent and the patient.
Vaccine hesitancy and public health US Medical PG Question 6: A 27-year-old man presents to the family medicine clinic for a routine check-up. The patient recently accepted a new job at a childcare center and the employer is requesting his vaccination history. After checking the records from the patient’s childhood, the physician realizes that the patient never had the varicella vaccine. The patient is unsure if he had chickenpox as a child, and there is no record of him having had the disease in the medical record. There is no significant medical history, and the patient takes no current medications. The patient’s heart rate is 82/min, respiratory rate is 14/min, temperature is 37.5°C (99.5°F), and blood pressure is 120/72 mm Hg. The patient appears alert and oriented. Auscultation of the heart reveals no murmurs, rubs, or gallops. The lungs are clear to auscultation bilaterally. With regard to the varicella vaccine, which of the following is recommended for the patient at this time?
- A. Two doses of vaccine (Correct Answer)
- B. One dose of the vaccine
- C. Wait until patient turns 50
- D. Serology then administer the vaccine (2 doses)
- E. Serology then administer the vaccine (1 dose)
Vaccine hesitancy and public health Explanation: ***Two doses of vaccine***
- According to **CDC/ACIP guidelines**, adults without evidence of immunity to varicella should receive **two doses of varicella vaccine** (4-8 weeks apart) without prior serologic testing.
- The patient has no documentation of vaccination or prior disease, and works in a **high-risk setting (childcare center)** with frequent exposure to children.
- **Routine serologic testing is NOT recommended** before vaccination as it delays protection, is cost-ineffective, and the vaccine is safe even if the person is already immune.
- Two doses provide **97% protection** against varicella and significant protection against breakthrough disease.
*Serology then administer the vaccine (2 doses)*
- While the two-dose schedule is correct, obtaining serology first is **not recommended by CDC** for routine adult varicella vaccination.
- Serologic testing delays protection and is cost-ineffective; the vaccine is safe to give even if immunity already exists.
- Serology may be considered in special circumstances (e.g., for healthcare workers when cost-benefit analysis favors testing), but not routinely.
*One dose of the vaccine*
- A single dose provides only **80-85% protection** and is insufficient for adults.
- **Two doses are required** for optimal immunity in adults without evidence of immunity.
*Wait until patient turns 50*
- This confuses the **varicella (chickenpox) vaccine** with the **herpes zoster (shingles) vaccine** (Shingrix), which is recommended at age 50.
- The patient needs immediate protection due to high-risk occupational exposure and current susceptibility.
*Serology then administer the vaccine (1 dose)*
- This option is incorrect for two reasons: serology is not routinely recommended, and one dose is insufficient for adult vaccination.
- Adults require a **two-dose series** for adequate protection against varicella.
Vaccine hesitancy and public health US Medical PG Question 7: A parent presents to her pediatrician requesting information about immunizations for her newborn. The pediatrician explains about basic principles of immunization, types of vaccines, possible adverse effects, and the immunization schedule. Regarding how immunizations work, the pediatrician explains that there are mainly 2 types of vaccines. The first type of vaccine provides stronger and more lasting immunity as it induces both cellular and humoral immune responses. The second type of vaccine produces mainly a humoral response only, and its overall efficacy is less as compared to the first type. Which of the following vaccines belongs to the first type of vaccine that the pediatrician is talking about?
- A. Hepatitis A vaccine
- B. Polio vaccine (Salk)
- C. Yellow fever vaccine (Correct Answer)
- D. Rabies vaccine
- E. Hepatitis B vaccine
Vaccine hesitancy and public health Explanation: ***Yellow fever vaccine***
- The Yellow fever vaccine is a **live-attenuated vaccine**, which mimics natural infection and effectively stimulates both **cellular and humoral immune responses**, leading to strong and long-lasting immunity.
- Live-attenuated vaccines contain a weakened form of the pathogen, allowing for replication within the host and robust immune system activation.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is an **inactivated vaccine**, which primarily induces a **humoral (antibody-mediated) immune response**.
- Inactivated vaccines generally do not stimulate a strong cellular immune response and often require booster doses to maintain protective immunity.
*Polio vaccine (Salk)*
- The Salk polio vaccine is an **inactivated polio vaccine (IPV)**, meaning it contains killed viral particles.
- As an inactivated vaccine, it mainly elicits a **humoral immune response** producing circulating antibodies but less mucosal or cellular immunity.
*Rabies vaccine*
- The Rabies vaccine is an **inactivated vaccine** given after exposure or for pre-exposure prophylaxis.
- It primarily induces a **humoral antibody response** rather than a strong cellular immune response.
*Hepatitis B vaccine*
- The Hepatitis B vaccine is a **recombinant vaccine**, containing only a portion of the viral antigen (HBsAg).
- This type of vaccine primarily stimulates a **humoral immune response** leading to antibody production, which is effective but does not typically induce a strong cellular response like live vaccines.
Vaccine hesitancy and public health US Medical PG Question 8: A regional academic medical center has 10 cases of adenovirus in the span of a week among its ICU patients. A committee is formed to investigate this outbreak. They are tasked with identifying the patients and interviewing the care providers to understand how adenovirus could have been spread from patient to patient. This committee will review charts, talk to the care provider teams, and investigate current patient safety and sanitation measures in the ICU. The goal of the committee is to identify weaknesses in the current system and to put in place a plan to help prevent this sort of outbreak from reoccurring in the future. The committee is most likely using what type of analysis?
- A. Simulation
- B. Root cause analysis (Correct Answer)
- C. Algorithmic analysis
- D. Heuristic analysis
- E. Failure mode and effects analysis
Vaccine hesitancy and public health Explanation: ***Root cause analysis***
- The committee's goal is to **identify weaknesses** in the current system and **prevent recurrence**, which aligns perfectly with the principles of **root cause analysis (RCA)**.
- RCA is a structured method for **identifying the underlying causes** of problems or incidents, rather than just addressing symptoms.
*Simulation*
- **Simulation** involves creating a model of a process or system to test different scenarios and predict outcomes.
- While useful for planning, it's not the primary method for investigating an actual past event or identifying causative factors after an outbreak has occurred.
*Algorithmic analysis*
- **Algorithmic analysis** is primarily used in computer science to evaluate the efficiency and complexity of algorithms.
- It does not apply to investigating the spread of infectious diseases or healthcare system failures.
*Heuristic analysis*
- **Heuristic analysis** involves using a rule of thumb or an educated guess to solve a problem quickly and efficiently, especially when perfect solutions are not feasible.
- This approach is less systematic and comprehensive than what is required to thoroughly investigate an outbreak and identify root causes.
*Failure mode and effects analysis*
- **Failure mode and effects analysis (FMEA)** is a proactive method used to identify **potential failure modes** in a system and their effects *before* an event occurs.
- The committee is investigating an **already existing problem**, making RCA more appropriate than FMEA, which is used for risk assessment of future processes.
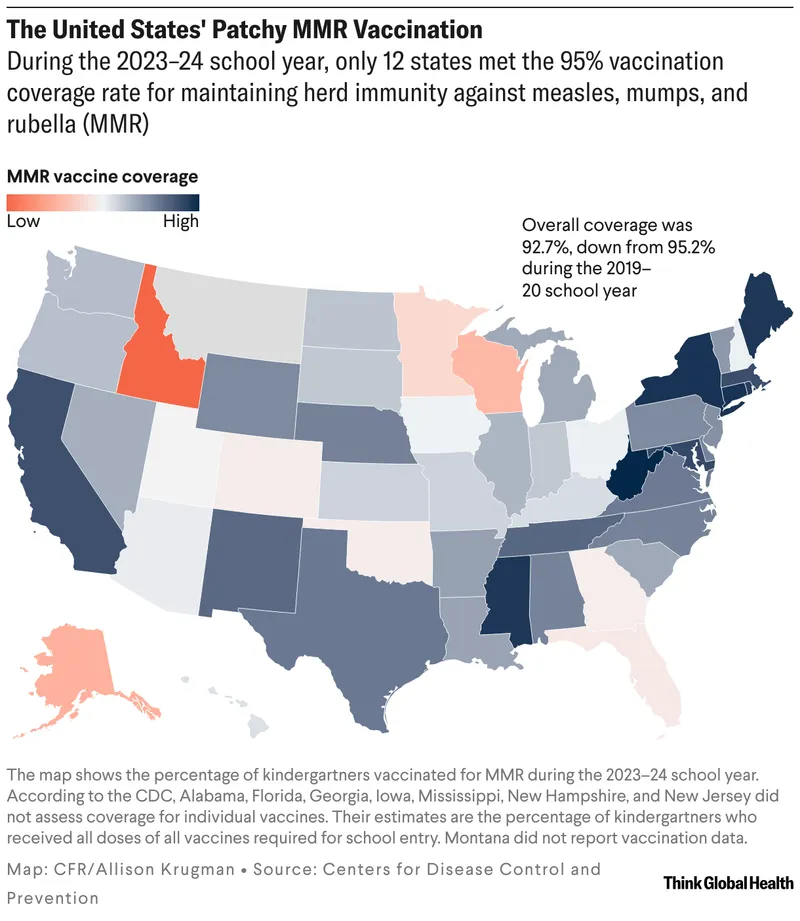
Vaccine hesitancy and public health US Medical PG Question 9: A 1-year-old immigrant girl has not received any recommended vaccines since birth. She attends daycare and remains healthy despite her daily association with several other children for the past 3 months at a home day-care facility. Which of the following phenomena explains why she has not contracted any vaccine-preventable diseases such as measles, diphtheria, or pertussis?
- A. Herd immunity (Correct Answer)
- B. Immune evasion
- C. Tolerance
- D. Genetic drift
- E. Genetic shift
Vaccine hesitancy and public health Explanation: ***Herd immunity***
- **Herd immunity** occurs when a significant portion of a population is immune to a disease, providing **indirect protection** to unvaccinated individuals.
- In a daycare setting with vaccinated children, the low prevalence of disease agents protects the unvaccinated girl.
*Immune evasion*
- **Immune evasion** refers to mechanisms used by pathogens to **avoid detection** and destruction by the host immune system.
- This concept describes how a pathogen survives in an infected individual, not why an uninfected individual avoids disease.
*Tolerance*
- **Tolerance** in immunology is a state of **unresponsiveness to antigens**, preventing the immune system from attacking self-components or harmless foreign substances.
- It does not explain protection from infectious diseases; rather, it's about not mounting an immune response when one is usually expected.
*Genetic drift*
- **Genetic drift** is a change in the frequency of an existing gene variant (allele) in a population due to **random sampling** of organisms.
- This is a concept in population genetics that does not explain an individual's protection from infectious disease.
*Genetic shift*
- **Genetic shift** (antigenic shift) refers to an **abrupt, major change** in the influenza virus, leading to new hemagglutinin and/or neuraminidase proteins.
- This phenomenon explains the emergence of new influenza strains, not the protection of an individual from vaccine-preventable diseases.
Vaccine hesitancy and public health US Medical PG Question 10: A 2-year-old boy presents to the pediatrician for evaluation of an elevated temperature, sore throat, runny nose, and lacrimation for the past week, and a rash which he developed yesterday. The rash began on the patient’s face and spread down to the trunk, hands, and feet. The patient’s mother gave him ibuprofen to control the fever. The child has not received mumps, measles, and rubella vaccinations because he was ill when the vaccine was scheduled and was later lost to follow-up. The vital signs include blood pressure 90/50 mm Hg, heart rate 110/min, respiratory rate 22/min, and temperature 37.8°C (100.0℉). On physical examination, the child was drowsy. His face, trunk, and extremities were covered with a maculopapular erythematous rash. Two irregularly-shaped red dots were also noted on the mucosa of the lower lip. The remainder of the physical examination was within normal limits. What is the probable causative agent for this child’s condition?
- A. Group A Streptococcus
- B. Rubulavirus
- C. Influenzavirus
- D. Morbillivirus (Correct Answer)
- E. Herpesvirus
Vaccine hesitancy and public health Explanation: ***Morbillivirus***
- The constellation of symptoms—**elevated temperature**, **sore throat**, **runny nose**, **lacrimation**, a **maculopapular erythematous rash** that began on the face and spread downward, and especially the **irregularly-shaped red dots on the mucosa of the lower lip** (likely **Koplik spots**)—are classic for **measles**, caused by Morbillivirus.
- The patient's **unvaccinated status** against MMR further supports measles as the most probable diagnosis, as it is a highly contagious disease prevented by vaccination.
*Group A Streptococcus*
- This bacterium causes **scarlet fever**, characterized by a **sandpaper-like rash** and **strawberry tongue**, not a maculopapular rash spreading from face to extremities with Koplik spots.
- While it can cause pharyngitis and fever, the specific rash progression and oral lesions rule out Group A Streptococcus.
*Rubulavirus*
- Rubulavirus causes **mumps**, which primarily presents with **parotitis** (swelling of parotid glands), fever, and headache.
- It does not typically cause a generalized maculopapular rash or Koplik spots, making it an unlikely cause for the described symptoms.
*Influenzavirus*
- Influenzavirus causes **influenza**, characterized by sudden onset of high fever, cough, myalgia, and headache.
- While it can cause fever and respiratory symptoms, it does not typically present with a widespread maculopapular rash or Koplik spots.
*Herpesvirus*
- Herpesviruses cause a variety of conditions, including **chickenpox** (Varicella-zoster virus), which presents with **vesicular lesions** that crust over, and **roseola infantum** (HHV-6/7), which primarily causes a high fever followed by a non-pruritic rash appearing *after* the fever subsides.
- Neither of these typically presents with Koplik spots or the specific maculopapular rash progression described.
More Vaccine hesitancy and public health US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.