Types of vaccines US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Types of vaccines. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Types of vaccines US Medical PG Question 1: A young man about to leave for his freshman year of college visits his physician in order to ensure that his immunizations are up-to-date. Because he is living in a college dormitory, his physician gives him a vaccine that prevents meningococcal disease. What type of vaccine did this patient likely receive?
- A. Live, attenuated
- B. Killed, attenuated
- C. Toxoid
- D. Conjugated polysaccharide (Correct Answer)
- E. Killed, inactivated
Types of vaccines Explanation: ***Conjugated polysaccharide***
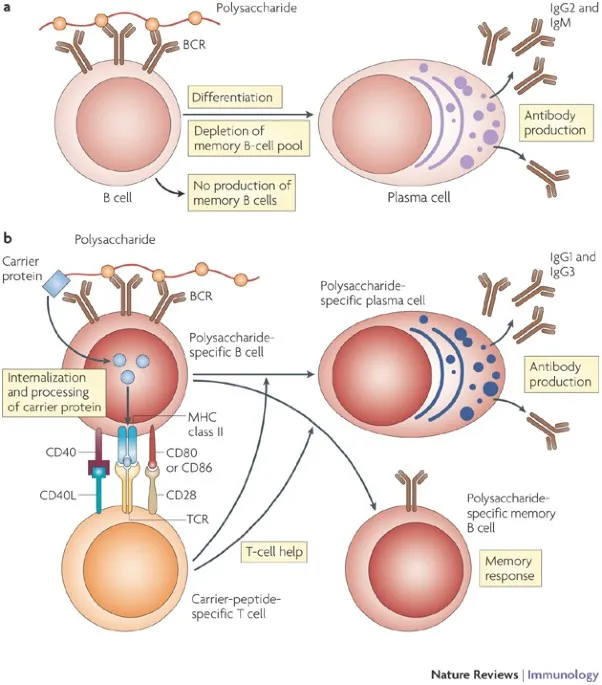
- The **meningococcal vaccine** commonly administered to college students is a **polysaccharide vaccine** wherein the polysaccharide antigens are conjugated to a protein carrier.
- This **conjugation** improves the immune response by converting a T-independent antigen into a T-dependent one, inducing better memory responses and allowing for vaccination of infants.
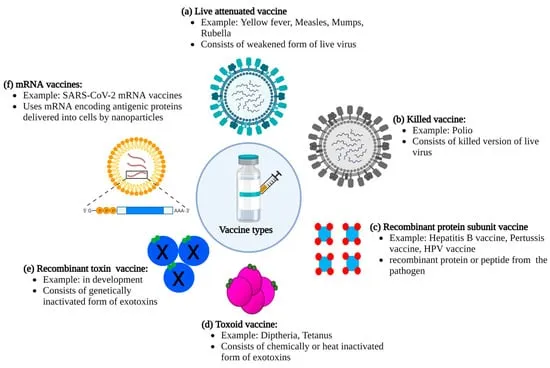
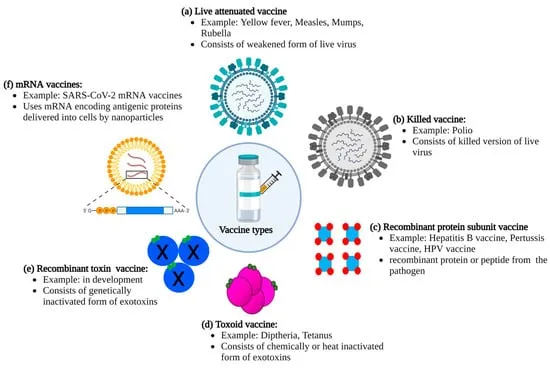
*Live, attenuated*
- Live, attenuated vaccines contain a **weakened form of the pathogen** that can replicate but does not cause disease, such as the MMR or varicella vaccine.
- While they elicit strong, long-lasting immunity, the meningococcal vaccine is not typically of this type due to the risk of opportunistic infection, especially in immunocompromised individuals.
*Killed, attenuated*
- This term is a **contradiction**; vaccines are either **killed (inactivated)** or **live (attenuated)**, but not both.
- Attenuation implies weakening, for which the organism would still be alive.
*Toxoid*
- **Toxoid vaccines** are made from inactivated bacterial toxins, used to protect against diseases where the toxin, not the bacterium itself, causes the disease, such as diphtheria and tetanus.
- Meningococcal disease is primarily caused by **direct bacterial invasion and inflammation**, not solely by a toxin.
*Killed, inactivated*
- **Killed, inactivated vaccines** contain whole pathogens that have been killed and cannot replicate, such as the inactivated poliovirus vaccine.
- While there are inactivated meningococcal vaccines, the most common type for broad use, especially in college settings, is the conjugated polysaccharide vaccine, which elicits a stronger and more long-lasting immune response against multiple serotypes compared to plain inactivated whole-cell vaccines.
Types of vaccines US Medical PG Question 2: To protect against a potentially deadly infection, a 19-year-old female receives a vaccine containing capsular polysaccharide. This vaccine will stimulate her immune system to produce antibodies against which organism?
- A. Corynebacterium diphtheriae
- B. Neisseria meningitidis (Correct Answer)
- C. Streptococcus pneumoniae
- D. Clostridium tetani
- E. Haemophilus influenzae type b
Types of vaccines Explanation: ***Neisseria meningitidis***
- The vaccine described, containing **capsular polysaccharide**, targets the **polysaccharide capsule** of *Neisseria meningitidis*, which is a key virulence factor.
- This bacterium causes **meningococcal meningitis**, a potentially deadly infection, especially in adolescents and young adults.
- The **meningococcal vaccine** is specifically recommended for adolescents and college students due to increased risk in this population.
*Corynebacterium diphtheriae*
- The vaccine against *C. diphtheriae* is a **toxoid vaccine**, meaning it contains an inactivated form of the **diphtheria toxin**, not capsular polysaccharide.
- This vaccine primarily protects against the effects of the **exotoxin**, which causes major symptoms like myocarditis and neuropathy.
*Streptococcus pneumoniae*
- While *S. pneumoniae* also has a **capsular polysaccharide vaccine** (PPSV23 and PCV13), it is primarily recommended for **young children, elderly adults, and immunocompromised patients**.
- A **19-year-old healthy female** would not routinely receive pneumococcal vaccine unless she had specific risk factors.
- The question context of a "potentially deadly infection" in this age group more specifically points to meningococcus.
*Clostridium tetani*
- The vaccine for *C. tetani* is a **tetanus toxoid vaccine**, similar to diphtheria, targeting the inactivated **tetanospasmin toxin** produced by the bacterium.
- This vaccine prevents the neurological symptoms of tetanus by neutralizing the toxin, not by targeting capsular polysaccharides.
*Haemophilus influenzae type b*
- While *H. influenzae* type b also has a **capsular polysaccharide-based vaccine** (conjugate vaccine), it is primarily given to **infants and young children** as part of routine childhood immunization.
- A 19-year-old would have already received this vaccine in childhood, and it is not routinely given to adolescents or adults.
- The age group and clinical context make meningococcus the more likely answer.
Types of vaccines US Medical PG Question 3: A 20-year-old man who is a biology major presents to his physician for a simple check-up. He is informed that he hasn't received a hepatitis B vaccine. When the first injection is applied, the medical professional informs him that he will need to come back 2 more times on assigned days, since the vaccine is given in 3 doses. Which of the following antibodies is produced first in the college student as a result of the first vaccination?
- A. IgE
- B. IgG
- C. IgM (Correct Answer)
- D. IgD
- E. IgA
Types of vaccines Explanation: ***IgM***
- Upon initial exposure to an antigen (like in the first vaccine dose), **IgM antibodies** are the first class to be produced and secreted by plasma cells.
- This **primary immune response** is characterized by a rapid, but short-lived, **IgM** peak.
*IgE*
- **IgE antibodies** are primarily involved in **allergic reactions** and defense against parasites, not the initial response to vaccination.
- Their production is typically triggered by exposure to specific allergens or parasites and mediated by Th2 helper T cells.
*IgG*
- **IgG antibodies** are the most abundant class in serum and are produced later in the primary response and predominantly during the **secondary immune response**.
- They provide **long-term immunity** and can cross the placenta, but are not the first antibody produced after initial antigen exposure.
*IgD*
- **IgD antibodies** are mainly found on the surface of **naive B cells** and act as B-cell receptors, playing a role in B-cell activation.
- They are not secreted in significant amounts into the serum and thus are not the first circulating antibody produced after vaccination.
*IgA*
- **IgA antibodies** are primarily found in **mucosal secretions** (e.g., saliva, tears, breast milk, gastrointestinal fluid) and play a key role in mucosal immunity.
- They are not the first antibody produced systemically in response to an initial vaccine exposure.
Types of vaccines US Medical PG Question 4: A 27-year-old man presents to the family medicine clinic for a routine check-up. The patient recently accepted a new job at a childcare center and the employer is requesting his vaccination history. After checking the records from the patient’s childhood, the physician realizes that the patient never had the varicella vaccine. The patient is unsure if he had chickenpox as a child, and there is no record of him having had the disease in the medical record. There is no significant medical history, and the patient takes no current medications. The patient’s heart rate is 82/min, respiratory rate is 14/min, temperature is 37.5°C (99.5°F), and blood pressure is 120/72 mm Hg. The patient appears alert and oriented. Auscultation of the heart reveals no murmurs, rubs, or gallops. The lungs are clear to auscultation bilaterally. With regard to the varicella vaccine, which of the following is recommended for the patient at this time?
- A. Two doses of vaccine (Correct Answer)
- B. One dose of the vaccine
- C. Wait until patient turns 50
- D. Serology then administer the vaccine (2 doses)
- E. Serology then administer the vaccine (1 dose)
Types of vaccines Explanation: ***Two doses of vaccine***
- According to **CDC/ACIP guidelines**, adults without evidence of immunity to varicella should receive **two doses of varicella vaccine** (4-8 weeks apart) without prior serologic testing.
- The patient has no documentation of vaccination or prior disease, and works in a **high-risk setting (childcare center)** with frequent exposure to children.
- **Routine serologic testing is NOT recommended** before vaccination as it delays protection, is cost-ineffective, and the vaccine is safe even if the person is already immune.
- Two doses provide **97% protection** against varicella and significant protection against breakthrough disease.
*Serology then administer the vaccine (2 doses)*
- While the two-dose schedule is correct, obtaining serology first is **not recommended by CDC** for routine adult varicella vaccination.
- Serologic testing delays protection and is cost-ineffective; the vaccine is safe to give even if immunity already exists.
- Serology may be considered in special circumstances (e.g., for healthcare workers when cost-benefit analysis favors testing), but not routinely.
*One dose of the vaccine*
- A single dose provides only **80-85% protection** and is insufficient for adults.
- **Two doses are required** for optimal immunity in adults without evidence of immunity.
*Wait until patient turns 50*
- This confuses the **varicella (chickenpox) vaccine** with the **herpes zoster (shingles) vaccine** (Shingrix), which is recommended at age 50.
- The patient needs immediate protection due to high-risk occupational exposure and current susceptibility.
*Serology then administer the vaccine (1 dose)*
- This option is incorrect for two reasons: serology is not routinely recommended, and one dose is insufficient for adult vaccination.
- Adults require a **two-dose series** for adequate protection against varicella.
Types of vaccines US Medical PG Question 5: A 2-month-old girl is brought to the physician by her father for a routine well-child examination. She is given a vaccine that contains polyribosylribitol phosphate conjugated to a toxoid carrier. The vaccine is most likely to provide immunity against which of the following pathogens?
- A. Haemophilus influenzae (Correct Answer)
- B. Neisseria meningitidis
- C. Bordetella pertussis
- D. Streptococcus pneumoniae
- E. Corynebacterium diphtheriae
Types of vaccines Explanation: **Haemophilus influenzae**
- The vaccine described, containing **polyribosylribitol phosphate (PRP)** conjugated to a toxoid carrier, is characteristic of the **Haemophilus influenzae type b (Hib) vaccine**.
- PRP is the **polysaccharide capsule** of *H. influenzae* type b, and conjugating it to a protein (toxoid carrier) allows for T-cell dependent immunity, effective in infants.
*Neisseria meningitidis*
- While *N. meningitidis* also has a **polysaccharide capsule** and vaccines are available, their capsular components differ (e.g., serogroups A, C, Y, W-135, or B outer membrane protein).
- The description of **polyribosylribitol phosphate** is specific to *H. influenzae* type b.
*Bordetella pertussis*
- Vaccines against *Bordetella pertussis* are typically **acellular pertussis vaccines (aP)**, which contain purified components like pertussis toxoid, filamentous hemagglutinin, and pertactin, not a PRP conjugate.
- These vaccines target bacterial toxins and adhesins, not a polysaccharide capsule unique to PRP.
*Streptococcus pneumoniae*
- Vaccines for *S. pneumoniae* (pneumococcal vaccines) use **capsular polysaccharides** from various serotypes, often conjugated to a protein carrier (e.g., diphtheria toxoid), but the specific polysaccharide is not PRP.
- The structure and serotypes of pneumococcal capsular polysaccharides are distinct from PRP.
*Corynebacterium diphtheriae*
- The vaccine for *C. diphtheriae* is the **diphtheria toxoid**, which is an inactivated form of the diphtheria toxin, not a polysaccharide conjugate.
- It provides immunity by inducing antibodies against the toxin, preventing its harmful effects.
Types of vaccines US Medical PG Question 6: A parent presents to her pediatrician requesting information about immunizations for her newborn. The pediatrician explains about basic principles of immunization, types of vaccines, possible adverse effects, and the immunization schedule. Regarding how immunizations work, the pediatrician explains that there are mainly 2 types of vaccines. The first type of vaccine provides stronger and more lasting immunity as it induces both cellular and humoral immune responses. The second type of vaccine produces mainly a humoral response only, and its overall efficacy is less as compared to the first type. Which of the following vaccines belongs to the first type of vaccine that the pediatrician is talking about?
- A. Hepatitis A vaccine
- B. Polio vaccine (Salk)
- C. Yellow fever vaccine (Correct Answer)
- D. Rabies vaccine
- E. Hepatitis B vaccine
Types of vaccines Explanation: ***Yellow fever vaccine***
- The Yellow fever vaccine is a **live-attenuated vaccine**, which mimics natural infection and effectively stimulates both **cellular and humoral immune responses**, leading to strong and long-lasting immunity.
- Live-attenuated vaccines contain a weakened form of the pathogen, allowing for replication within the host and robust immune system activation.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is an **inactivated vaccine**, which primarily induces a **humoral (antibody-mediated) immune response**.
- Inactivated vaccines generally do not stimulate a strong cellular immune response and often require booster doses to maintain protective immunity.
*Polio vaccine (Salk)*
- The Salk polio vaccine is an **inactivated polio vaccine (IPV)**, meaning it contains killed viral particles.
- As an inactivated vaccine, it mainly elicits a **humoral immune response** producing circulating antibodies but less mucosal or cellular immunity.
*Rabies vaccine*
- The Rabies vaccine is an **inactivated vaccine** given after exposure or for pre-exposure prophylaxis.
- It primarily induces a **humoral antibody response** rather than a strong cellular immune response.
*Hepatitis B vaccine*
- The Hepatitis B vaccine is a **recombinant vaccine**, containing only a portion of the viral antigen (HBsAg).
- This type of vaccine primarily stimulates a **humoral immune response** leading to antibody production, which is effective but does not typically induce a strong cellular response like live vaccines.
Types of vaccines US Medical PG Question 7: A 1-year-old immigrant girl has not received any recommended vaccines since birth. She attends daycare and remains healthy despite her daily association with several other children for the past 3 months at a home day-care facility. Which of the following phenomena explains why she has not contracted any vaccine-preventable diseases such as measles, diphtheria, or pertussis?
- A. Herd immunity (Correct Answer)
- B. Immune evasion
- C. Tolerance
- D. Genetic drift
- E. Genetic shift
Types of vaccines Explanation: ***Herd immunity***
- **Herd immunity** occurs when a significant portion of a population is immune to a disease, providing **indirect protection** to unvaccinated individuals.
- In a daycare setting with vaccinated children, the low prevalence of disease agents protects the unvaccinated girl.
*Immune evasion*
- **Immune evasion** refers to mechanisms used by pathogens to **avoid detection** and destruction by the host immune system.
- This concept describes how a pathogen survives in an infected individual, not why an uninfected individual avoids disease.
*Tolerance*
- **Tolerance** in immunology is a state of **unresponsiveness to antigens**, preventing the immune system from attacking self-components or harmless foreign substances.
- It does not explain protection from infectious diseases; rather, it's about not mounting an immune response when one is usually expected.
*Genetic drift*
- **Genetic drift** is a change in the frequency of an existing gene variant (allele) in a population due to **random sampling** of organisms.
- This is a concept in population genetics that does not explain an individual's protection from infectious disease.
*Genetic shift*
- **Genetic shift** (antigenic shift) refers to an **abrupt, major change** in the influenza virus, leading to new hemagglutinin and/or neuraminidase proteins.
- This phenomenon explains the emergence of new influenza strains, not the protection of an individual from vaccine-preventable diseases.
Types of vaccines US Medical PG Question 8: A 62-year-old woman presents to the clinic with a lacerated wound on her left forearm. She got the wound accidentally when she slipped in her garden and scraped her hand against some nails sticking out of the fence. The patient has rheumatoid arthritis and takes methylprednisolone 16 mg/day. She cannot recall her vaccination history. On physical examination her blood pressure is 140/95 mm Hg, heart rate is 81/min, respiratory rate is 16/min, and temperature is 36.9°C (98.4°F). The wound is irregularly shaped and lacerated and measures 4 × 5 cm with a depth of 0.5 cm. It is contaminated with dirt. The physician decides to administer both the tetanus toxoid and immunoglobulin after wound treatment. What is true regarding the tetanus prophylaxis in this patient?
- A. It does not make sense to administer tetanus toxoid as it will fail to induce sufficient immunity in a patient who takes oral glucocorticoids.
- B. The immunoglobulin administration will provide sufficient levels of anti-tetanus toxin antibodies until the production of the patient’s own antibodies starts. (Correct Answer)
- C. It does not make sense to administer tetanus toxoid as it will fail to induce sufficient immunity in patients aged more than 60 years.
- D. The immunoglobulin is given to this patient to promote the action of the toxoid and antibody production.
- E. Immunoglobulin administration can provide constant levels of antibodies in the patient’s blood for more than 4 months.
Types of vaccines Explanation: ***The immunoglobulin administration will provide sufficient levels of anti-tetanus toxin antibodies until the production of the patient’s own antibodies starts.***
* **Tetanus immunoglobulin (TIG)** provides immediate, but temporary, passive immunity through pre-formed antibodies, crucial for high-risk wounds in unvaccinated or immunocompromised individuals.
* This **passive immunity** offers immediate protection while the patient's immune system begins to mount an active response to the **tetanus toxoid vaccine**.
*It does not make sense to administer tetanus toxoid as it will fail to induce sufficient immunity in a patient who takes oral glucocorticoids.*
* While **glucocorticoids (like methylprednisolone)** can reduce the immune response, **tetanus toxoid** vaccination is still recommended, although the immune response might be attenuated.
* A **reduced, but still present, immune response** from vaccination in combination with passive immunity from TIG offers better long-term protection than TIG alone.
*It does not make sense to administer tetanus toxoid as it will fail to induce sufficient immunity in patients aged more than 60 years.*
* **Age alone** is not a contraindication for tetanus toxoid vaccination; while the immune response may be somewhat reduced in older adults, it can still provide significant protection.
* The **immunogenicity of tetanus toxoid** remains high in older adults, and it is part of routine vaccination schedules for all ages.
*The immunoglobulin is given to this patient to promote the action of the toxoid and antibody production.*
* **Immunoglobulin (TIG)** provides immediate passive immunity; it does not promote or enhance the active immune response induced by the **tetanus toxoid vaccine**.
* The toxoid stimulates the patient's own immune system to produce antibodies, a process that is separate from the immediate, temporary protection offered by immunoglobulin.
*Immunoglobulin administration can provide constant levels of antibodies in the patient’s blood for more than 4 months.*
* **Tetanus immunoglobulin** provides only **short-term passive immunity**, with antibodies typically lasting for a few weeks to a few months, not more than 4 months.
* For long-term protection, **active immunization with tetanus toxoid** is necessary, as it induces memory B and T cells.
Types of vaccines US Medical PG Question 9: A 26-year-old woman comes to the physician because of several days of fever, abdominal cramps, and diarrhea. She drank water from a stream 1 week ago while she was hiking in the woods. Abdominal examination shows increased bowel sounds. Stool analysis for ova and parasites shows flagellated multinucleated trophozoites. Further evaluation shows the presence of antibodies directed against the pathogen. Secretion of these antibodies most likely requires binding of which of the following?
- A. CD28 to B7 protein
- B. CD80/86 to CTLA-4
- C. gp120 to CD4
- D. CD8 to MHC I
- E. CD40 to CD40 ligand (Correct Answer)
Types of vaccines Explanation: ***CD40 to CD40 ligand***
- The interaction between **CD40 on B cells** and **CD40 ligand (CD40L) on activated T helper cells** is crucial for **T cell-dependent B cell activation** and antibody class switching.
- This binding leads to the maturation of the immune response, including the secretion of **high-affinity antibodies** like IgA, which is especially important for mucosal immunity against pathogens like *Giardia lamblia* (the likely cause of the patient's symptoms).
*CD28 to B7 protein*
- The binding of **CD28 on T cells** to **B7 protein (CD80/86) on antigen-presenting cells (APCs)** provides the **second co-stimulatory signal** required for T cell activation.
- While essential for T cell activation, this interaction primarily supports T cell proliferation and differentiation, rather than directly mediating antibody secretion by B cells.
*CD80/86 to CTLA-4*
- **CTLA-4 (cytotoxic T-lymphocyte-associated protein 4)** is a receptor on T cells that binds to **CD80/86 (B7)** on APCs with higher affinity than CD28.
- This interaction provides an **inhibitory signal** that downregulates T cell activation, serving as a negative feedback mechanism, and does not promote antibody secretion.
*gp120 to CD4*
- The **gp120 glycoprotein** on the surface of **HIV** binds to the **CD4 receptor** on T helper cells, initiating the entry of the virus into the cell.
- This interaction is specific to HIV infection and is not involved in the normal process of antibody secretion in response to other pathogens.
*CD8 to MHC I*
- **CD8** is a co-receptor expressed on **cytotoxic T lymphocytes (CTLs)** that binds to **MHC class I molecules** on target cells.
- This interaction is essential for the recognition of virally infected or cancerous cells by CTLs, leading to their destruction, but it is not directly involved in antibody production.
Types of vaccines US Medical PG Question 10: A 12-year-old child is exposed to pollen while playing outside. The allergen stimulates TH2 cells of his immune system to secrete a factor that leads to B-cell class switching to IgE. What factor is secreted by the TH2 cell?
- A. IL-4 (Correct Answer)
- B. IL-22
- C. TGF-beta
- D. IL-17
- E. IFN-gamma
Types of vaccines Explanation: ***IL-4***
- **Interleukin-4 (IL-4)** is a key cytokine produced by **TH2 cells** that promotes **B-cell class switching to IgE**, central to allergic reactions.
- It also stimulates the differentiation of naive T cells into **TH2 cells**, further amplifying the **allergic response**.
*IL-22*
- **IL-22** is primarily involved in maintaining **epithelial barrier integrity** and promoting **tissue repair**, especially in the gut and skin.
- It does not play a direct role in **IgE class switching** or the pathogenesis of type I hypersensitivity.
*TGF-beta*
- **TGF-beta (Transforming Growth Factor-beta)** is a pleiotropic cytokine involved in **cell growth**, differentiation, apoptosis, and immune regulation, particularly promoting **Treg cell development** and IgA class switching.
- It primarily suppresses rather than promotes **allergic reactions** and IgE production.
*IL-17*
- **IL-17** is a cytokine predominantly produced by **TH17 cells** and is crucial in protection against **extracellular bacteria and fungi**.
- It is associated with **autoimmune diseases** and inflammation but not directly with IgE-mediated allergic responses.
*IFN-gamma*
- **Interferon-gamma (IFN-gamma)** is a critical **TH1 cytokine** that activates macrophages, enhances natural killer cell activity, and promotes the cell-mediated immune response.
- It typically **inhibits TH2 responses** and IgE production, thus working against the development of allergic reactions.
More Types of vaccines US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.