Principles of vaccination US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Principles of vaccination. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Principles of vaccination US Medical PG Question 1: A 24-year-old woman with HIV infection comes to the physician for a follow-up examination. She has been inconsistently taking combined antiretroviral therapy for the past 5 years. She did not receive any childhood vaccinations because her parents were against them. During the consultation, the patient says that she wants to catch up on the missed vaccinations. Laboratory studies show a CD4+ T lymphocyte cell count of 180/mm3. Administration of the vaccine against which of the following agents should be avoided in this patient?
- A. Clostridium tetani
- B. Human papillomavirus
- C. Varicella zoster virus (Correct Answer)
- D. Bordetella pertussis
- E. Haemophilus influenzae
Principles of vaccination Explanation: ***Varicella zoster virus***
- The **varicella zoster vaccine is a live attenuated vaccine**, which is generally contraindicated in individuals with severe **immunodeficiency**, such as HIV patients with a **CD4+ count below 200 cells/mm³**.
- Administering a live vaccine to an immunocompromised patient can lead to **uncontrolled viral replication** and potentially cause the disease it is meant to prevent.
*Clostridium tetani*
- The **tetanus vaccine** is a **toxoid vaccine**, meaning it contains inactivated bacterial toxins, not live organisms.
- It is **safe and recommended** for individuals with HIV, regardless of their CD4+ count, to provide protection against tetanus.
*Human papillomavirus*
- The **HPV vaccine** is a **recombinant vaccine**, consisting of viral-like particles (VLPs) and containing no live virus.
- It is **safe and recommended** for HIV-positive individuals and helps prevent HPV-related cancers.
*Bordetella pertussis*
- The **pertussis vaccine** (part of DTaP or Tdap) is an **acellular vaccine**, containing purified bacterial components, not live bacteria.
- It is **safe and recommended** for HIV patients to protect against whooping cough.
*Haemophilus influenzae*
- The **Haemophilus influenzae type b (Hib) vaccine** is a **conjugate vaccine**, made from bacterial capsular polysaccharide linked to a carrier protein.
- It is **safe and recommended** for HIV-positive individuals, as they are at increased risk for invasive Hib disease.
Principles of vaccination US Medical PG Question 2: A 12-month-old girl is brought to her pediatrician for a checkup and vaccines. The patient’s mother wants to send her to daycare but is worried about exposure to unvaccinated children and other potential sources of infection. The toddler was born at 39 weeks gestation via spontaneous vaginal delivery. She is up to date on all vaccines. She does not walk yet but stands in place and can say a few words. The toddler drinks formula and eats a mixture of soft vegetables and pureed meals. She has no current medications. On physical exam, the vital signs include: temperature 37.0°C (98.6°F), blood pressure 95/50 mm Hg, pulse 130/min, and respiratory rate 28/min. The patient is alert and responsive. The remainder of the exam is unremarkable. Which of the following is most appropriate for this patient at this visit?
- A. Meningococcal vaccine
- B. Gross motor workup and evaluation
- C. Rotavirus vaccine
- D. Referral for speech pathology
- E. MMR vaccine (Correct Answer)
Principles of vaccination Explanation: ***MMR vaccine***
- The **measles, mumps, and rubella (MMR) vaccine** is recommended for administration at **12-15 months of age**.
- This timing offers protection against these common childhood diseases, which is especially important for children attending **daycare**.
*Meningococcal vaccine*
- The routine **meningococcal vaccine (MenACWY)** is typically recommended for adolescents at **11-12 years of age**, with a booster at 16 years.
- While there are specific circumstances for earlier vaccination (e.g., high-risk conditions), it is **not routine** for a 12-month-old.
*Gross motor workup and evaluation*
- The patient's motor development, standing in place but not yet walking, is **within the normal range** for a 12-month-old.
- A definitive **gross motor workup** would generally be considered if there were more significant delays or regressions.
*Rotavirus vaccine*
- The **rotavirus vaccine** series is typically given at **2, 4, and 6 months of age**, with the final dose administered no later than **8 months of age**.
- A 12-month-old is **outside the recommended age range** for initiating or completing this vaccine series.
*Referral for speech pathology*
- Saying "a few words" at 12 months is **within the normal developmental milestone** for expressive language at this age.
- A referral for **speech pathology** would generally be indicated for more significant language delays.
Principles of vaccination US Medical PG Question 3: A 2-year-old boy is brought in by his parents to his pediatrician. The boy was born by spontaneous vaginal delivery at 39 weeks and 5 days after a normal pregnancy. The boy has received all age-appropriate vaccinations as of his last visit at 18 months of age. Of note, the boy has confirmed sickle cell disease and the only medication he takes is penicillin prophylaxis. The parents state that they plan on enrolling their son in a daycare, which requires documentation of up-to-date vaccinations. The pediatrician states that their son needs an additional vaccination at this visit, which is a polysaccharide vaccine that is not conjugated to protein. Which of the following matches this description?
- A. Pneumovax (Correct Answer)
- B. Menactra
- C. Prevnar
- D. Hib vaccine
- E. Live attenuated influenza vaccine
Principles of vaccination Explanation: ***Pneumovax***
- **Pneumovax** (PCV23, PPSV23) is a **polysaccharide vaccine** that is not conjugated to a protein carrier. Children with **sickle cell disease** should receive this vaccine due to their immunocompromised state and increased risk of encapsulated bacterial infections.
- The Centers for Disease Control and Prevention (CDC) recommends PPSV23 for children aged 2 years and older with chronic medical conditions such as **sickle cell disease**, usually administered 8 weeks after their last PCV13 dose.
*Menactra*
- **Menactra** is a **quadrivalent meningococcal conjugate vaccine** (MCV4), meaning it contains a polysaccharide antigen conjugated to a protein carrier.
- This vaccine primarily targets *Neisseria meningitidis* and is different from the pneumococcal vaccine required here.
*Prevnar*
- **Prevnar** (PCV13) is a **pneumococcal conjugate vaccine**, meaning its polysaccharide antigens are conjugated to a protein carrier.
- While important for children with sickle cell disease, the question specifically asks for a vaccination that is a **polysaccharide vaccine that is not conjugated to protein**.
*Hib vaccine*
- The **Hib vaccine** (against *Haemophilus influenzae* type b) is a **conjugate vaccine**, meaning its polysaccharide capsule is linked to a protein carrier to enhance immunogenicity, particularly in infants.
- This vaccine is typically given earlier in childhood and is not the "additional" unconjugated polysaccharide vaccine described.
*Live attenuated influenza vaccine*
- The **live attenuated influenza vaccine (LAIV)** is a live virus vaccine, not a polysaccharide vaccine.
- It is also contraindicated in individuals with certain immunocompromising conditions, such as some patients with sickle cell disease.
Principles of vaccination US Medical PG Question 4: A young man about to leave for his freshman year of college visits his physician in order to ensure that his immunizations are up-to-date. Because he is living in a college dormitory, his physician gives him a vaccine that prevents meningococcal disease. What type of vaccine did this patient likely receive?
- A. Live, attenuated
- B. Killed, attenuated
- C. Toxoid
- D. Conjugated polysaccharide (Correct Answer)
- E. Killed, inactivated
Principles of vaccination Explanation: ***Conjugated polysaccharide***
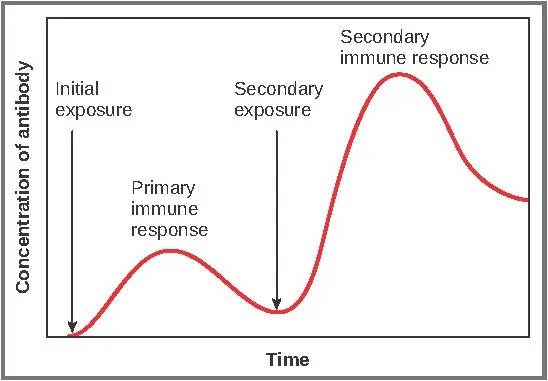
- The **meningococcal vaccine** commonly administered to college students is a **polysaccharide vaccine** wherein the polysaccharide antigens are conjugated to a protein carrier.
- This **conjugation** improves the immune response by converting a T-independent antigen into a T-dependent one, inducing better memory responses and allowing for vaccination of infants.
*Live, attenuated*
- Live, attenuated vaccines contain a **weakened form of the pathogen** that can replicate but does not cause disease, such as the MMR or varicella vaccine.
- While they elicit strong, long-lasting immunity, the meningococcal vaccine is not typically of this type due to the risk of opportunistic infection, especially in immunocompromised individuals.
*Killed, attenuated*
- This term is a **contradiction**; vaccines are either **killed (inactivated)** or **live (attenuated)**, but not both.
- Attenuation implies weakening, for which the organism would still be alive.
*Toxoid*
- **Toxoid vaccines** are made from inactivated bacterial toxins, used to protect against diseases where the toxin, not the bacterium itself, causes the disease, such as diphtheria and tetanus.
- Meningococcal disease is primarily caused by **direct bacterial invasion and inflammation**, not solely by a toxin.
*Killed, inactivated*
- **Killed, inactivated vaccines** contain whole pathogens that have been killed and cannot replicate, such as the inactivated poliovirus vaccine.
- While there are inactivated meningococcal vaccines, the most common type for broad use, especially in college settings, is the conjugated polysaccharide vaccine, which elicits a stronger and more long-lasting immune response against multiple serotypes compared to plain inactivated whole-cell vaccines.
Principles of vaccination US Medical PG Question 5: A 3255-g (7-lb) female newborn is delivered at term. Pregnancy and delivery were uncomplicated. On the day of her birth, she is given a routine childhood vaccine that contains a noninfectious glycoprotein. This vaccine will most likely help prevent infection by which of the following pathogens?
- A. Bordetella pertussis
- B. Rotavirus
- C. Poliovirus
- D. Haemophilus influenzae type b
- E. Hepatitis B virus (Correct Answer)
Principles of vaccination Explanation: ***Hepatitis B virus***
- The **Hepatitis B vaccine** is routinely given at birth and contains a **noninfectious glycoprotein** (HBsAg) that elicits an immune response.
- This vaccine is crucial for preventing mother-to-child transmission and provides long-term protection against **Hepatitis B infection**.
*Bordetella pertussis*
- The vaccine for **Bordetella pertussis** (whooping cough) is part of the DTaP vaccine and is typically given at 2 months of age, not at birth.
- The DTaP vaccine usually contains **inactivated toxins** or acellular components, not solely a glycoprotein.
*Rotavirus*
- The **Rotavirus vaccine** is an **oral live-attenuated vaccine** administered in two or three doses, with the first dose typically given at 2 months of age.
- It does not contain a noninfectious glycoprotein.
*Poliovirus*
- The **Poliovirus vaccine** (IPV) is an **inactivated vaccine** given at 2 months of age, and the **oral poliovirus vaccine (OPV)** is a live-attenuated vaccine.
- Neither is routinely given at birth, nor described as a noninfectious glycoprotein.
*Haemophilus influenzae type b*
- The **Haemophilus influenzae type b (Hib) vaccine** is a polysaccharide-protein conjugate vaccine, first administered at 2 months of age.
- While it contains a protein component, it is not typically given at birth.
Principles of vaccination US Medical PG Question 6: A 9-month-old boy is brought to a pediatrician by his parents for routine immunization. The parents say they have recently immigrated to the United States from a developing country, where the infant was receiving immunizations as per the national immunization schedule for that country. The pediatrician prepares a plan for the infant’s immunizations as per standard US guidelines. Looking at the plan, the parents ask why the infant needs to be vaccinated with injectable polio vaccine, as he had already received an oral polio vaccine back in their home country. The pediatrician explains to them that, as per the recommended immunization schedule for children and adolescents in the United States, it is important to complete the schedule of immunizations using the injectable polio vaccine (IPV). He also mentions that IPV is considered safer than OPV, and IPV has some distinct advantages over OPV. Which of the following statements best explains the advantage of IPV over OPV to which the pediatrician is referring?
- A. IPV is known to produce higher titers of mucosal IgG antibodies than OPV
- B. IPV is known to produce virus-specific CD4+ T cells that produce interleukins and interferons to control polio viruses
- C. IPV is known to produce higher titers of mucosal IgA antibodies than OPV
- D. IPV is known to produce higher titers of serum IgG antibodies than OPV (Correct Answer)
- E. IPV is known to produce virus-specific CD8+ T cells that directly kill polio-infected cells
Principles of vaccination Explanation: ***IPV is known to produce higher titers of serum IgG antibodies than OPV***
- The **injectable polio vaccine (IPV)** is an **inactivated vaccine** that primarily induces a systemic immune response, leading to high levels of **serum IgG antibodies**. These antibodies are crucial for preventing **viremia** and subsequently protecting against paralytic poliomyelitis.
- While OPV (oral polio vaccine) induces both mucosal and humoral immunity, IPV's strength lies in its ability to generate robust systemic immunity without the risk of vaccine-associated paralytic polio (VAPP), a rare but serious complication of OPV.
*IPV is known to produce higher titers of mucosal IgG antibodies than OPV*
- IPV primarily stimulates **systemic immunity** rather than strong mucosal immunity, meaning it does not typically produce higher titers of mucosal IgG antibodies than OPV.
- Mucosal immunity, especially IgA, is better stimulated by vaccines administered orally, like **OPV**, as it directly interacts with the gut-associated lymphoid tissue.
*IPV is known to produce virus-specific CD4+ T cells that produce interleukins and interferons to control polio viruses*
- Both IPV and OPV can induce **CD4+ T cell responses**, but this statement does not highlight a distinct advantage of IPV over OPV.
- While CD4+ T cells are important for immune coordination and antibody production, the primary advantage of IPV is its **safety profile** and systemic antibody levels, not necessarily a superior CD4+ T cell response.
*IPV is known to produce higher titers of mucosal IgA antibodies than OPV*
- **OPV**, being an oral vaccine, is highly effective at inducing a strong **mucosal IgA response** in the gut, which is important for preventing viral shedding and transmission.
- **IPV**, administered parenterally, produces minimal to no mucosal IgA response, making this statement incorrect.
*IPV is known to produce virus-specific CD8+ T cells that directly kill polio-infected cells*
- **Cytotoxic CD8+ T cells** are primarily involved in clearing cells infected with intracellular pathogens.
- While both vaccines may induce some cellular immunity, their primary mechanism for protecting against polio is through **neutralizing antibodies**, and the induction of CD8+ T cells is not the principal advantage of IPV over OPV.
Principles of vaccination US Medical PG Question 7: A 2-month-old girl is brought to the physician by her father for a routine well-child examination. She is given a vaccine that contains polyribosylribitol phosphate conjugated to a toxoid carrier. The vaccine is most likely to provide immunity against which of the following pathogens?
- A. Haemophilus influenzae (Correct Answer)
- B. Neisseria meningitidis
- C. Bordetella pertussis
- D. Streptococcus pneumoniae
- E. Corynebacterium diphtheriae
Principles of vaccination Explanation: **Haemophilus influenzae**
- The vaccine described, containing **polyribosylribitol phosphate (PRP)** conjugated to a toxoid carrier, is characteristic of the **Haemophilus influenzae type b (Hib) vaccine**.
- PRP is the **polysaccharide capsule** of *H. influenzae* type b, and conjugating it to a protein (toxoid carrier) allows for T-cell dependent immunity, effective in infants.
*Neisseria meningitidis*
- While *N. meningitidis* also has a **polysaccharide capsule** and vaccines are available, their capsular components differ (e.g., serogroups A, C, Y, W-135, or B outer membrane protein).
- The description of **polyribosylribitol phosphate** is specific to *H. influenzae* type b.
*Bordetella pertussis*
- Vaccines against *Bordetella pertussis* are typically **acellular pertussis vaccines (aP)**, which contain purified components like pertussis toxoid, filamentous hemagglutinin, and pertactin, not a PRP conjugate.
- These vaccines target bacterial toxins and adhesins, not a polysaccharide capsule unique to PRP.
*Streptococcus pneumoniae*
- Vaccines for *S. pneumoniae* (pneumococcal vaccines) use **capsular polysaccharides** from various serotypes, often conjugated to a protein carrier (e.g., diphtheria toxoid), but the specific polysaccharide is not PRP.
- The structure and serotypes of pneumococcal capsular polysaccharides are distinct from PRP.
*Corynebacterium diphtheriae*
- The vaccine for *C. diphtheriae* is the **diphtheria toxoid**, which is an inactivated form of the diphtheria toxin, not a polysaccharide conjugate.
- It provides immunity by inducing antibodies against the toxin, preventing its harmful effects.
Principles of vaccination US Medical PG Question 8: A 1-year-old girl is brought to the physician for a well-child examination. She has no history of serious illness. She receives a vaccine in which a polysaccharide is conjugated to a carrier protein. Which of the following pathogens is the most likely target of this vaccine?
- A. Hepatitis A virus
- B. Varicella zoster virus
- C. Streptococcus pneumoniae (Correct Answer)
- D. Bordetella pertussis
- E. Clostridium tetani
Principles of vaccination Explanation: ***Streptococcus pneumoniae***
- This pathogen is a common cause of **pneumonia**, **otitis media**, and **meningitis** in young children. The **pneumococcal conjugate vaccine (PCV)** targets *Streptococcus pneumoniae*'s polysaccharide capsule by conjugating it to a carrier protein.
- Conjugating the polysaccharide to a protein carrier allows for a **T-cell-dependent immune response**, which is crucial for eliciting a robust and long-lasting antibody response in infants and young children, whose immune systems are not yet mature enough to respond effectively to unconjugated polysaccharide antigens.
*Hepatitis A virus*
- The vaccine for **Hepatitis A virus** is an **inactivated vaccine** containing whole killed virus particles, not a polysaccharide conjugated to a carrier protein.
- It is typically given to children to prevent **Hepatitis A infection**, which causes liver inflammation.
*Varicella zoster virus*
- The **varicella vaccine** for **Varicella zoster virus** is a **live, attenuated vaccine**, meaning it contains a weakened form of the live virus.
- This vaccine aims to prevent **chickenpox** and is not a polysaccharide-protein conjugate vaccine.
*Bordetella pertussis*
- The vaccine for **Bordetella pertussis** (whooping cough) is part of the **DTaP vaccine** and is an **acellular vaccine**, containing purified components of the bacterium.
- These components are primarily **toxoids** (inactivated toxins) or other bacterial proteins, not polysaccharides.
*Clostridium tetani*
- The vaccine for **Clostridium tetani** is a **toxoid vaccine**, meaning it contains an inactivated form of the **tetanus toxin**.
- This is part of the **DTaP vaccine** and works by stimulating an immune response against the toxin, not bacterial polysaccharides.
Principles of vaccination US Medical PG Question 9: A parent presents to her pediatrician requesting information about immunizations for her newborn. The pediatrician explains about basic principles of immunization, types of vaccines, possible adverse effects, and the immunization schedule. Regarding how immunizations work, the pediatrician explains that there are mainly 2 types of vaccines. The first type of vaccine provides stronger and more lasting immunity as it induces both cellular and humoral immune responses. The second type of vaccine produces mainly a humoral response only, and its overall efficacy is less as compared to the first type. Which of the following vaccines belongs to the first type of vaccine that the pediatrician is talking about?
- A. Hepatitis A vaccine
- B. Polio vaccine (Salk)
- C. Yellow fever vaccine (Correct Answer)
- D. Rabies vaccine
- E. Hepatitis B vaccine
Principles of vaccination Explanation: ***Yellow fever vaccine***
- The Yellow fever vaccine is a **live-attenuated vaccine**, which mimics natural infection and effectively stimulates both **cellular and humoral immune responses**, leading to strong and long-lasting immunity.
- Live-attenuated vaccines contain a weakened form of the pathogen, allowing for replication within the host and robust immune system activation.
*Hepatitis A vaccine*
- The Hepatitis A vaccine is an **inactivated vaccine**, which primarily induces a **humoral (antibody-mediated) immune response**.
- Inactivated vaccines generally do not stimulate a strong cellular immune response and often require booster doses to maintain protective immunity.
*Polio vaccine (Salk)*
- The Salk polio vaccine is an **inactivated polio vaccine (IPV)**, meaning it contains killed viral particles.
- As an inactivated vaccine, it mainly elicits a **humoral immune response** producing circulating antibodies but less mucosal or cellular immunity.
*Rabies vaccine*
- The Rabies vaccine is an **inactivated vaccine** given after exposure or for pre-exposure prophylaxis.
- It primarily induces a **humoral antibody response** rather than a strong cellular immune response.
*Hepatitis B vaccine*
- The Hepatitis B vaccine is a **recombinant vaccine**, containing only a portion of the viral antigen (HBsAg).
- This type of vaccine primarily stimulates a **humoral immune response** leading to antibody production, which is effective but does not typically induce a strong cellular response like live vaccines.
Principles of vaccination US Medical PG Question 10: A 45-year-old male presents to the emergency room complaining of severe nausea and vomiting. He returned from a business trip to Nigeria five days ago. Since then, he has developed progressively worsening fevers, headache, nausea, and vomiting. He has lost his appetite and cannot hold down food or water. He did not receive any vaccinations before traveling. His medical history is notable for alcohol abuse and peptic ulcer disease for which he takes omeprazole regularly. His temperature is 103.0°F (39.4°C), blood pressure is 100/70 mmHg, pulse is 128/min, and respirations are 22/min. Physical examination reveals scleral icterus, hepatomegaly, and tenderness to palpation in the right and left upper quadrants. While in the examination room, he vomits up dark vomitus. The patient is admitted and started on multiple anti-protozoal and anti-bacterial medications. Serology studies are pending; however, the patient dies soon after admission. The virus that likely gave rise to this patient’s condition is part of which of the following families?
- A. Togavirus
- B. Flavivirus (Correct Answer)
- C. Calicivirus
- D. Hepevirus
- E. Bunyavirus
Principles of vaccination Explanation: ***Flavivirus***
- The clinical presentation, including acute onset of **high fever**, headache, nausea, vomiting (**dark vomitus**), **scleral icterus**, and **hepatomegaly** following travel to Nigeria, is highly suggestive of **yellow fever**.
- Yellow fever is caused by the **yellow fever virus**, which is a **flavivirus** transmitted by mosquitoes, primarily *Aedes aegypti*.
*Togavirus*
- The Togavirus family includes viruses like **rubella virus** and **alphaviruses** (e.g., Eastern equine encephalitis virus).
- While some alphaviruses can cause fever and encephalitis, they typically do not present with the characteristic **hemorrhagic fever** and severe liver involvement seen in this case.
*Calicivirus*
- The Calicivirus family includes **Norovirus**, which is a common cause of **gastroenteritis** with vomiting and diarrhea.
- Norovirus infections are typically self-limiting and do not usually lead to the severe systemic symptoms, **jaundice**, or fatal outcome described here.
*Hepevirus*
- The Hepevirus family includes the **hepatitis E virus (HEV)**.
- HEV causes **acute viral hepatitis**, characterized by jaundice, nausea, and vomiting, but it rarely progresses to the rapid, severe, and fatal hemorrhagic form seen in this patient.
*Bunyavirus*
- The Bunyavirus family (now split into several families) includes viruses like Hantavirus and Rift Valley fever virus, which can cause **hemorrhagic fevers**.
- While some bunyaviruses are found in Africa, the specific constellation of symptoms, particularly the prominent **scleral icterus** and rapid progression to severe liver failure and death, is most consistent with **yellow fever**, a flavivirus.
More Principles of vaccination US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.