Trypanosomes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Trypanosomes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Trypanosomes US Medical PG Question 1: A 23-year-old woman presents with progressively worsening headache, photophobia, and intermittent fever that have lasted for 6 days. She says her headache is mostly frontal and radiates down her neck. She denies any recent history of blood transfusions, recent travel, or contact with animals. Her past medical history is unremarkable. She is sexually active with a single partner for the past 3 years. Her temperature is 38.5°C (101.3°F). On physical examination, she appears pale and diaphoretic. A fine erythematous rash is noted on the neck and forearms. A lumbar puncture is performed and CSF analysis reveals:
Opening pressure: 300 mm H2O
Erythrocytes: None
Leukocytes: 72/mm3
Neutrophils: 10%
Lymphocytes: 75%
Mononuclear: 15%
Protein: 100 mg/dL
Glucose: 70 mg/dL
Which of the following is the most likely diagnosis in this patient?
- A. Lymphocytic choriomeningitis virus
- B. Ehrlichiosis
- C. Enterovirus meningitis (Correct Answer)
- D. Brucellosis
- E. Mumps meningitis
Trypanosomes Explanation: ***Enterovirus meningitis***
- The patient's symptoms of **headache**, **photophobia**, **fever**, and a **fine erythematous rash**, combined with CSF findings of **lymphocytic pleocytosis (75%)**, **elevated protein**, and **normal glucose**, are classic for **viral (aseptic) meningitis**.
- Enteroviruses (including coxsackievirus and echovirus) are the **most common cause** of viral meningitis in immunocompetent adults, particularly in summer and fall.
- The **normal glucose level** (70 mg/dL) effectively rules out bacterial meningitis, while the **lymphocytic predominance** with mildly elevated protein is pathognomonic for viral etiology.
- The fine erythematous rash is consistent with enteroviral exanthem.
*Lymphocytic choriomeningitis virus*
- While LCMV can cause aseptic meningitis with similar CSF findings (lymphocytic pleocytosis, normal glucose), it is typically acquired through contact with **rodent urine or feces**, particularly from pet hamsters or mice.
- The patient **denies animal contact**, making this diagnosis less likely than the more prevalent enterovirus infection.
*Ehrlichiosis*
- Ehrlichiosis is a **tick-borne illness** (from *Ehrlichia* species) that can cause fever, headache, and rash, but typically presents with **leukopenia**, **thrombocytopenia**, and elevated liver enzymes.
- The rash in ehrlichiosis is often petechial or absent entirely. CNS involvement is uncommon and would more likely present as meningoencephalitis rather than isolated meningitis.
- The CSF profile with prominent lymphocytic pleocytosis and normal glucose fits viral meningitis better than ehrlichiosis.
*Brucellosis*
- Brucellosis is a **zoonotic infection** acquired through contact with **unpasteurized dairy products** or infected livestock (cattle, goats, pigs), which the patient denies.
- While *Brucella* can cause chronic meningitis with lymphocytic pleocytosis, it classically presents with **undulating fever**, hepatosplenomegaly, and a more protracted course (weeks to months).
- The acute 6-day presentation without exposure history makes this unlikely.
*Mumps meningitis*
- Mumps virus can cause aseptic meningitis with a similar CSF profile (lymphocytic pleocytosis, normal glucose).
- However, mumps meningitis typically occurs in association with or following **parotitis (parotid gland swelling)**, which is not mentioned in this case.
- With widespread MMR vaccination, mumps is now rare in immunized populations, making enterovirus a more likely diagnosis.
Trypanosomes US Medical PG Question 2: A 21-year-old woman is diagnosed with a rare subtype of anti-NMDA encephalitis. During the diagnostic workup, she was found to have an ovarian teratoma. Her physician is curious about the association between anti-NMDA encephalitis and ovarian teratomas. A causal relationship between this subtype of anti-NMDA encephalitis and ovarian teratomas is suspected. The physician aims to identify patients with anti-NMDA encephalitis and subsequently evaluate them for the presence of ovarian teratomas. Which type of study design would be the most appropriate?
- A. Case-control study
- B. Retrospective cohort study (Correct Answer)
- C. Cross-sectional study
- D. Case series
- E. Randomized controlled trial
Trypanosomes Explanation: ***Retrospective cohort study***
- This is the **most appropriate design** because the physician starts with a defined group of patients **with anti-NMDA encephalitis** (the exposure/condition) and then evaluates them for the **presence of ovarian teratomas** (the outcome).
- A **cohort study** follows this directional approach: identify individuals with a specific exposure or condition, then assess the frequency or presence of an outcome within that group.
- **Retrospective** cohort studies use **existing medical records** to identify the exposed cohort and determine outcome status, making this practical for studying a rare condition like anti-NMDA encephalitis.
- This design allows calculation of the **prevalence** of ovarian teratomas among anti-NMDA encephalitis patients and can suggest an association between the two conditions.
*Cross-sectional study*
- Cross-sectional studies assess **both exposure and outcome simultaneously** at a single point in time in a population, rather than starting with one condition and looking for another.
- This design would be appropriate if the physician surveyed a population and assessed both anti-NMDA encephalitis and ovarian teratomas at the same time, but the question describes a **directional evaluation** (first identify encephalitis patients, then evaluate for teratomas).
- While cross-sectional studies can identify associations, they do not follow the sequential approach described in the clinical scenario.
*Case series*
- A **case series** is a descriptive study that reports characteristics or outcomes in a group of patients with a particular condition but lacks a comparison group and does not systematically evaluate associations.
- While it could describe ovarian teratoma findings in anti-NMDA encephalitis patients, it does not provide the structured framework for assessing prevalence or association that a cohort study offers.
*Case-control study*
- **Case-control studies** work in the **opposite direction**: they start with the outcome (e.g., ovarian teratoma cases) and look backward for the exposure (e.g., anti-NMDA encephalitis).
- The physician's approach starts with the **exposure first** (anti-NMDA encephalitis), making a case-control design inappropriate.
- Case-control studies are efficient for studying rare outcomes but are not aligned with the described study plan.
*Randomized controlled trial*
- **RCTs** are experimental studies that randomly assign participants to different interventions to evaluate treatment efficacy or causation.
- This is an **observational research question** about naturally occurring associations, not an intervention study, making RCTs inappropriate and unethical for this scenario.
Trypanosomes US Medical PG Question 3: A 13-year-old boy is brought to a physician with severe fevers and headaches for 3 days. The pain is constant and mainly behind the eyes. He has myalgias, nausea, vomiting, and a rash for one day. Last week, during an academic winter break, he traveled on a tour with his family to several countries, including Brazil, Panama, and Peru. They spent many evenings outdoors without any protection against insect bites. There is no history of contact with pets, serious illness, or use of medications. The temperature is 40.0℃ (104.0℉); the pulse is 110/min; the respiratory rate is 18/min, and the blood pressure is 110/60 mm Hg. A maculopapular rash is seen over the trunk and extremities. Several tender lymph nodes are palpated in the neck on both sides. A peripheral blood smear shows no organisms. Which of the following is most likely responsible for this patient’s presentation?
- A. Chagas disease
- B. Zika virus
- C. Babesiosis
- D. Malaria
- E. Dengue fever (Correct Answer)
Trypanosomes Explanation: ***Dengue fever***
- This patient's symptoms (fever, **retro-orbital headache**, myalgias, nausea, vomiting, rash, and travel history to endemic areas like **Brazil, Panama, and Peru**) are classic for dengue fever. The **high fever (40°C)** and rash are also highly suggestive.
- Exposure to mosquito bites in tropical regions, typical of travel during an academic break, is a common mode of transmission for this **flavivirus**.
*Chagas disease*
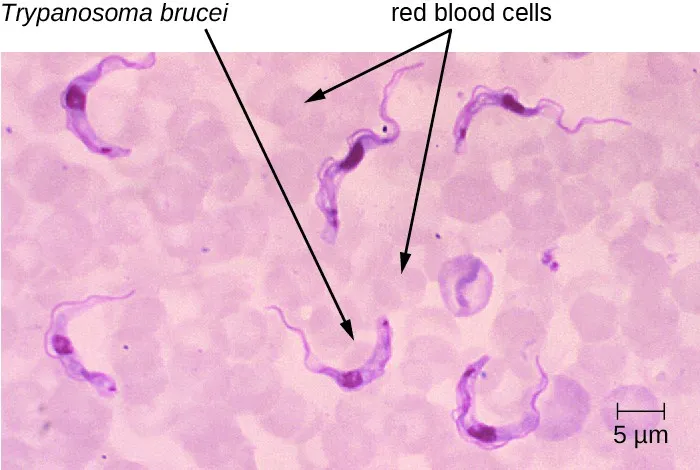
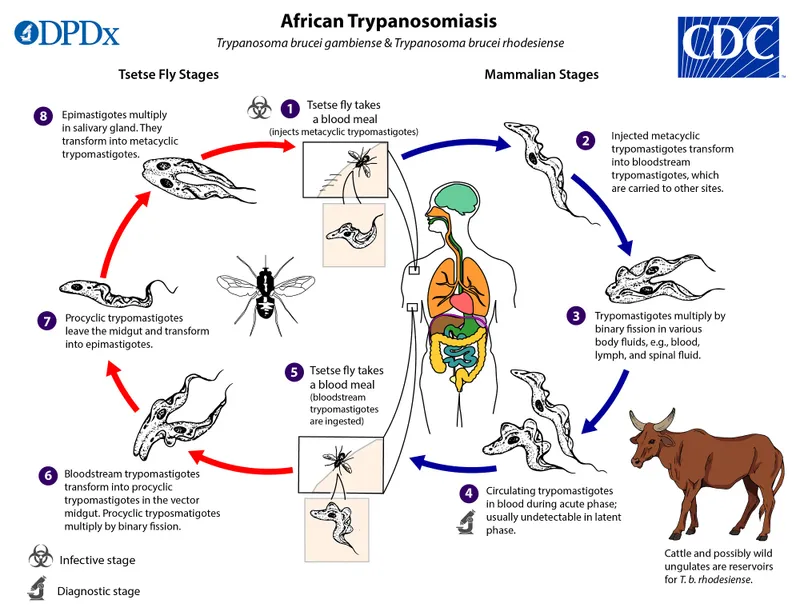
- Chagas disease, caused by **Trypanosoma cruzi**, is typically transmitted by the **reduviid bug** (kissing bug).
- Acute symptoms can include **fever**, **Romana's sign** (unilateral periorbital swelling), and sometimes a chagoma, but the widespread **maculopapular rash** and severe retro-orbital headache are less characteristic.
*Zika virus*
- Zika virus infection can present with **fever**, **rash**, **arthralgia**, and **conjunctivitis**.
- While the travel history fits, the **severe retro-orbital headache**, high fever, and myalgias are more prominent in dengue fever; Zika symptoms are generally milder in adults.
*Babesiosis*
- Babesiosis is a **tick-borne** illness caused by **Babesia parasites**, often presenting with **fever**, **fatigue**, chills, and **hemolytic anemia**.
- There is no mention of tick exposure, and the characteristic rash and retro-orbital headache are not typical features of babesiosis.
*Malaria*
- Malaria, caused by **Plasmodium parasites** transmitted by **Anopheles mosquitoes**, presents with cyclical fevers, chills, sweats, and fatigue.
- While the travel history to endemic areas is relevant, the **retro-orbital headache** and **maculopapular rash** as described are not typical for uncomplicated malaria; malaria is also detected on a peripheral blood smear, which was negative here.
Trypanosomes US Medical PG Question 4: A 30-year-old forest landscape specialist is brought to the emergency department with hematemesis and confusion. One week ago she was diagnosed with influenza when she had fevers, severe headaches, myalgias, hip and shoulder pain, and a maculopapular rash. After a day of relative remission, she developed abdominal pain, vomiting, and diarrhea. A single episode of hematemesis occurred prior to admission. Two weeks ago she visited rainforests and caves in western Africa where she had direct contact with animals, including apes. She has no history of serious illnesses or use of medications. She is restless. Her temperature is 38.0℃ (100.4℉); the pulse is 95/min, the respiratory rate is 20/min; and supine and upright blood pressure is 130/70 mm Hg and 100/65 mm Hg, respectively. Conjunctival suffusion is noted. Ecchymoses are observed on the lower extremities. She is bleeding from one of her intravenous lines. The peripheral blood smear is negative for organisms. Filovirus genomes were detected during a reverse transcription-polymerase chain reaction. The laboratory studies show the following:
Laboratory test
Hemoglobin 10 g/dL
Leukocyte count 1,000/mm3
Segmented neutrophils 65%
Lymphocytes 20%
Platelet count 50,000/mm3
Partial thromboplastin time (activated) 60 seconds
Prothrombin time 25 seconds
Fibrin split products positive
Serum
Alanine aminotransferase (ALT) 85 U/L
Aspartate aminotransferase (AST) 120 U/L
γ-Glutamyltransferase (GGT) 83 U/L
Creatinine 2 mg/dL
Which of the following is the most appropriate immediate step in management?
- A. Esophagogastroduodenoscopy
- B. Postexposure vaccination of close contacts
- C. Parenteral artesunate plus sulfadoxine/pyrimethamine
- D. Use of N95 masks
- E. Intravenous fluids and electrolytes (Correct Answer)
Trypanosomes Explanation: ***Intravenous fluids and electrolytes***
- The patient presents with **orthostatic hypotension**, internal bleeding (hematemesis, ecchymoses), and deranged renal function (elevated creatinine). These indicate significant **fluid loss** and potential **hypovolemic shock**, making immediate fluid resuscitation critical.
- **Ebola virus disease** (indicated by the travel history, symptoms, and positive filovirus genomes) often leads to severe dehydration due to fluid loss from vomiting, diarrhea, and internal bleeding, necessitating aggressive fluid and electrolyte replacement as a cornerstone of supportive care.
*Esophagogastroduodenoscopy*
- While the patient has hematemesis, her overall clinical picture with **severe coagulopathy** (elevated PT/aPTT, low platelets, positive fibrin split products) and **multisystem involvement** suggests a systemic bleeding disorder rather than a focal upper GI bleed that would be the primary target of an EGD.
- Performing an invasive procedure like EGD in a patient with severe coagulopathy and a highly contagious disease like Ebola (implied by filovirus detection) carries significant risks and is not the most immediate priority compared to stabilizing vital signs and correcting fluid deficits.
*Postexposure vaccination of close contacts*
- This is a crucial public health measure for **Ebola virus disease** but is a secondary step in management focused on prevention for others, not the immediate stabilization or treatment of the acutely ill patient.
- While important, it does not address the patient's immediate, life-threatening symptoms of hypovolemia, bleeding, and organ dysfunction.
*Parenteral artesunate plus sulfadoxine/pyrimethamine*
- This regimen is an antimalarial treatment. While the patient traveled to Western Africa, her symptoms and the detection of **filovirus genomes** rule out malaria as the primary diagnosis requiring this specific treatment.
- Administering antimalarials would delay appropriate supportive care for Ebola virus disease and is not indicated given the specific viral diagnosis.
*Use of N95 masks*
- **N95 masks** are important for healthcare worker protection given the patient's symptoms and confirmed filovirus. However, the question asks for the most appropriate *immediate step in management* of the patient's condition.
- While infection control is paramount, providing immediate direct patient care like fluid resuscitation takes precedence for the patient's survival over PPE considerations, assuming adequate PPE is already being donned by healthcare providers.
Trypanosomes US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Trypanosomes Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Trypanosomes US Medical PG Question 6: A 19-year-old woman presents to the family medical center with a 2-week history of a sore throat. She says that she has felt increasingly tired during the day and has a difficult time staying awake during her classes at the university. She appears well-nourished with a low energy level. Her vital signs include the following: the heart rate is 82/min, the respiratory rate is 14/min, the temperature is 37.8°C (100.0°F), and the blood pressure is 112/82 mm Hg. Inspection of the pharynx is depicted in the picture. Palpation of the neck reveals posterior cervical lymphadenopathy. The membrane does not bleed upon scraping. What is the most specific finding for detecting the syndrome described in the vignette?
- A. > 10% atypical lymphocytes
- B. Positive rapid strep test
- C. Growth in Loffler’s medium
- D. Increased transaminase levels
- E. Positive monospot test (Correct Answer)
Trypanosomes Explanation: ***Positive monospot test***
- The patient's symptoms (sore throat, fatigue, posterior cervical lymphadenopathy, pharyngitis with exudates, age) are highly suggestive of **infectious mononucleosis**, which is caused by the **Epstein-Barr virus (EBV)**.
- A **positive monospot test**, which detects **heterophile antibodies**, is the most specific and widely used rapid diagnostic test for infectious mononucleosis.
* > 10% atypical lymphocytes*
- While **atypical lymphocytes** are characteristic of infectious mononucleosis, they are not exclusive to EBV infection and can be seen in other viral infections (e.g., CMV, HIV). Therefore, this finding is less specific than a positive monospot test.
- A definitive diagnosis usually requires a combination of clinical symptoms and specific serological tests like the **monospot test** or **EBV-specific antibodies**.
*Positive rapid strep test*
- A rapid strep test detects **Group A Streptococcus (GAS)**. While bacterial pharyngitis can present with a sore throat, the accompanying fatigue and posterior cervical lymphadenopathy make streptococcal pharyngitis less likely as the primary diagnosis.
- The rapid strep test would be negative in infectious mononucleosis, and therefore, a positive result would rule out mononucleosis as the sole cause.
*Growth in Loffler’s medium*
- **Loffler's medium** is used to culture **Corynebacterium diphtheriae**, the causative agent of diphtheria. Diphtheria presents with a severe sore throat and a tenacious gray membrane that **bleeds upon scraping**, unlike the description in the vignette.
- While it's a specific diagnostic test for diphtheria, the patient's presentation does not align with diphtheria, and this test would not be positive in infectious mononucleosis.
*Increased transaminase levels*
- **Increased transaminase levels** (AST, ALT) indicate liver involvement, which can occur in infectious mononucleosis due to **hepatitis**.
- While this is a common finding in many cases of mononucleosis (and supports the diagnosis), it is an indicator of organ involvement rather than a specific diagnostic test for the presence of the virus or its unique immunological response (like the monospot test).
Trypanosomes US Medical PG Question 7: A 32-year-old woman presents to your office with abdominal pain and bloating over the last month. She also complains of intermittent, copious, non-bloody diarrhea over the same time. Last month, she had a cough that has since improved but has not completely resolved. She has no sick contacts and has not left the country recently. She denies any myalgias, itching, or rashes. Physical and laboratory evaluations are unremarkable. Examination of her stool reveals the causative organism. This organism is most likely transmitted to the human host through which of the following routes?
- A. Insect bite
- B. Penetration of skin (Correct Answer)
- C. Sexual contact
- D. Inhalation
- E. Animal bite
Trypanosomes Explanation: ***Penetration of skin***
- The symptoms of **abdominal pain**, **bloating**, **intermittent copious non-bloody diarrhea**, and a recent **cough** are highly suggestive of a **hookworm infection**.
- Hookworm larvae (filariform larvae) primarily penetrate the skin, usually through bare feet, as their mode of entry into the human host.
*Insect bite*
- Although some parasitic infections are transmitted by insect bites (e.g., malaria, Chagas disease), hookworms are not transmitted this way.
- **Insect-borne diseases** typically present with different clinical manifestations or geographical associations.
*Sexual contact*
- **Sexually transmitted infections** involve direct contact of mucous membranes or body fluids during sexual activity.
- Hookworm infection transmission through sexual contact is not a recognized route.
*Inhalation*
- **Inhalation** is a route of transmission for respiratory pathogens (e.g., influenza, tuberculosis) or certain fungal infections, but not for hookworms.
- While hookworm larvae migrate through the lungs, the initial infection pathway is not via inhalation.
*Animal bite*
- **Animal bites** transmit diseases like rabies or certain bacterial infections, but not parasitic hookworms.
- Hookworm infection does not result from direct contact with an animal's saliva or puncture wound.
Trypanosomes US Medical PG Question 8: A 24-year-old man presents with a painless genital ulcer for the past 2 weeks. He reports that he recently has been having unprotected sex with multiple partners. Past medical history is unremarkable. On physical examination, a single ulcer is present on the dorsal shaft of the penis which is circumscribed, indurated, and partially healed. There is moderate inguinal lymphadenopathy but no buboes. Which of the following tests would confirm the most likely diagnosis in this patient?
- A. Perform a darkfield microscopic examination of a swab from the chancre (Correct Answer)
- B. Swab the chancre and perform a saline wet mount
- C. Fluorescent treponemal antibody absorption (FTA-ABS) test
- D. Frei test
- E. Venereal Disease Research Laboratory (VDRL) test
Trypanosomes Explanation: ***Perform a darkfield microscopic examination of a swab from the chancre***
- This patient's presentation with a **painless, indurated genital ulcer** (chancre) and regional lymphadenopathy is highly suggestive of **primary syphilis**.
- **Darkfield microscopy** directly visualizes the spirochetes (**_Treponema pallidum_**) from the chancre, providing a definitive and rapid diagnosis.
*Swab the chancre and perform a saline wet mount*
- A **saline wet mount** is used to identify mobile organisms like **_Trichomonas vaginalis_** or clue cells suggestive of **bacterial vaginosis**, neither of which are associated with this type of ulcer.
- This test would not reveal the spirochetes responsible for syphilis and is not appropriate for diagnosing a genital ulcer.
*Fluorescent treponemal antibody absorption (FTA-ABS) test*
- The **FTA-ABS test** is a **treponemal-specific serological test** used to confirm a syphilis diagnosis, particularly in later stages or when non-treponemal tests are reactive.
- While sensitive for syphilis, it's typically reactive later in the disease course and cannot directly visualize the bacteria from the ulcer, making darkfield microscopy a more immediate and direct diagnostic tool for primary syphilis.
*Frei test*
- The **Frei test** is an obsolete intradermal skin test used to diagnose **lymphogranuloma venereum (LGV)**, which typically presents with a transient, unnoticed lesion followed by severe lymphadenopathy and buboes.
- It is not used for the diagnosis of syphilis and would not be helpful for this patient's presentation.
*Viral and rickettsial disease research laboratory (VDRL) test*
- The **VDRL test** is a **non-treponemal serological test** for syphilis that detects antibodies against cardiolipin, a lipid released from damaged host cells.
- While used for screening and monitoring treatment response, it can be **negative in early primary syphilis** (before seroconversion) and may not be positive at the time of presentation with a fresh chancre.
Trypanosomes US Medical PG Question 9: A previously healthy 24-year-old male is brought to the emergency department because of fevers, congestion, and chest pain for 3 days. The chest pain is exacerbated by deep inspiration. He takes no medications. His temperature is 37.5°C (99.5°F), blood pressure is 118/75 mm Hg, pulse is 130/min, and respirations are 12/min. He appears weak and lethargic. Cardiac examination shows a scratchy sound best heard along the left sternal border when the patient leans forward. There are crackles in both lung bases. Examination of the lower extremities shows pitting edema. Results of a rapid influenza test are negative. EKG shows diffuse ST-elevations with depressed PR interval. An echocardiogram shows left ventricular chamber enlargement with contractile dysfunction. Infection with which of the following pathogens is the most likely cause of this patient's symptoms?
- A. Orthomyxovirus
- B. Flavivirus
- C. Togavirus
- D. Paramyxovirus
- E. Picornavirus (Correct Answer)
Trypanosomes Explanation: ***Picornavirus***
- This patient presents with **myopericarditis** (concurrent myocarditis and pericarditis), which is particularly characteristic of **picornavirus** infection, specifically **coxsackievirus B**.
- **Pericarditis features:** Pleuritic chest pain, pericardial friction rub (scratchy sound), diffuse ST elevations with PR depression on EKG.
- **Myocarditis features:** Left ventricular enlargement with contractile dysfunction, signs of heart failure (pitting edema, tachycardia, weakness).
- **Coxsackievirus B** is the **most common viral cause** of acute myocarditis and pericarditis in previously healthy young adults, often following a prodrome of respiratory or gastrointestinal symptoms.
*Orthomyxovirus*
- **Orthomyxoviruses** (influenza virus) can cause myocarditis, but the **negative rapid influenza test** makes this diagnosis unlikely in this case.
- While influenza commonly causes respiratory symptoms and fever, the combination of classic pericarditis findings with severe myocarditis points more strongly toward coxsackievirus infection.
*Flavivirus*
- **Flaviviruses** (e.g., Dengue, Zika, West Nile) typically present with **fever, arthralgias, rash**, or **neurological symptoms**, which are not described here.
- Cardiac complications from flaviviruses are rare and would typically occur in the context of their characteristic systemic manifestations. They are not a common cause of acute myopericarditis.
*Togavirus*
- **Togaviruses** include **rubella virus** and **alphaviruses** (e.g., Chikungunya). Rubella presents with diffuse rash and lymphadenopathy, while alphaviruses cause prominent arthralgias.
- While rubella can rarely cause myocarditis, it is not a common cause of acute myopericarditis, and the characteristic rash and joint symptoms are absent in this patient.
*Paramyxovirus*
- **Paramyxoviruses** include measles, mumps, RSV, and parainfluenza. **Mumps virus** is the paramyxovirus most associated with myocarditis.
- However, mumps typically presents with characteristic **parotitis** (parotid gland swelling), which is absent in this patient, making it less likely than coxsackievirus as the cause of this myopericarditis presentation.
Trypanosomes US Medical PG Question 10: A 27-year-old male who works on an organic farm is diagnosed with infection by N. americanus, a helminthic parasite. Eosinophils require which antibody isotype to destroy these parasites via antibody-dependent cellular cytotoxicity?
- A. IgE (Correct Answer)
- B. IgA
- C. IgG
- D. IgM
- E. IgD
Trypanosomes Explanation: ***IgE***
- **IgE** antibodies are crucial in the immune response against helminthic parasites, including *N. americanus*, by sensitizing **mast cells** and **eosinophils**.
- When **IgE** binds to the surface of parasites, the **Fc receptor** on eosinophils recognizes the Fc portion of IgE, leading to the release of cytotoxic granules that destroy the parasite (antibody-dependent cellular cytotoxicity).
*IgA*
- **IgA** is primarily found in **mucosal secretions** and plays a role in defending against pathogens at mucosal surfaces, but it is not the primary isotype involved in eosinophil-mediated **ADCC** against helminths.
- While IgA can bind to some immune cells, its main function is to **neutralize toxins** and prevent microbial adhesion at mucosal sites.
*IgG*
- **IgG** is the most abundant antibody in serum and is involved in various immune functions, including **opsonization**, **neutralization**, and **complement activation**.
- Although IgG can mediate ADCC by **NK cells** and **macrophages**, it is not the primary isotype for eosinophil-mediated killing of helminths, which is dominated by IgE.
*IgM*
- **IgM** is typically the first antibody produced during a primary immune response and is very effective at **activating the complement system**.
- Its large pentameric structure also limits its diffusion into tissues, and it does not play a direct role in eosinophil-mediated ADCC against helminthic parasites.
*IgD*
- **IgD** primarily functions as a **B cell receptor** on naive B lymphocytes, signaling for their activation and differentiation.
- It is present in very low concentrations in serum and its role in host defense against parasites or in ADCC is negligible.
More Trypanosomes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.