Toxoplasma gondii US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Toxoplasma gondii. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Toxoplasma gondii US Medical PG Question 1: A 26-year-old man comes to the physician for a follow-up examination. He was diagnosed with HIV infection 2 weeks ago. His CD4+ T-lymphocyte count is 162/mm3 (N ≥ 500). An interferon-gamma release assay is negative. Prophylactic treatment against which of the following pathogens is most appropriate at this time?
- A. Cytomegalovirus
- B. Toxoplasma gondii
- C. Mycobacterium tuberculosis
- D. Aspergillus fumigatus
- E. Pneumocystis jirovecii (Correct Answer)
Toxoplasma gondii Explanation: ***Pneumocystis jirovecii***
- This patient's **CD4+ T-lymphocyte count of 162/mm3** is below the threshold of 200/mm3, indicating a significant risk for **Pneumocystis pneumonia (PCP)**, an opportunistic infection in HIV.
- Prophylaxis with **trimethoprim-sulfamethoxazole (TMP-SMX)** is highly effective and recommended for HIV patients with CD4 counts less than 200/mm3.
*Cytomegalovirus*
- **CMV prophylaxis** is generally not recommended for all HIV patients, even with low CD4 counts, unless there is evidence of active disease or extremely low CD4 counts (e.g., <50/mm3) with high viral loads.
- While CMV can cause end-organ disease in advanced HIV, routine primary prophylaxis is not standard for this CD4 level.
*Toxoplasma gondii*
- **Toxoplasma prophylaxis** is indicated for HIV patients with **CD4 counts less than 100/mm3** who are also seropositive for *Toxoplasma gondii*.
- The patient's CD4 count is 162/mm3, and there's no mention of *Toxoplasma* serostatus, making it less appropriate than PCP prophylaxis.
*Mycobacterium tuberculosis*
- The patient's **interferon-gamma release assay (IGRA) is negative**, which suggests no **latent tuberculosis infection (LTBI)**, thus making primary prophylaxis unnecessary at this time.
- While HIV patients are at high risk for TB, prophylaxis is typically given for LTBI or as secondary prophylaxis for those who have completed treatment for active TB.
*Aspergillus fumigatus*
- **Aspergillus infections** are typically seen in patients with severe **neutropenia** or those receiving high-dose corticosteroids, not primarily in HIV patients based solely on CD4 count.
- Routine prophylaxis for Aspergillus is not recommended for HIV patients, even with low CD4 counts, unless there is a specific risk factor.
Toxoplasma gondii US Medical PG Question 2: A 63-year-old man with non-Hodgkin lymphoma is brought to the emergency department because of fever and confusion that have progressively worsened over the past 3 days. He also has a 3-day history of loose stools. He returned from France 2 weeks ago where he stayed in the countryside and ate typical French cuisine, including frog, snail, and various homemade cheeses. His last chemotherapy cycle was 3 weeks ago. He is oriented to person but not to place or time. His temperature is 39.5°C (103.1°F), pulse is 110/min, and blood pressure is 100/60 mm Hg. Examination shows cervical and axillary lymphadenopathy. The lungs are clear to auscultation. There is involuntary flexion of the bilateral hips and knees with passive flexion of the neck. Neurologic examination shows no focal findings. Laboratory studies show:
Hemoglobin 9.3 g/dL
Leukocyte count 3600/mm3
Platelet count 151,000/mm3
Serum
Na+ 134 mEq/L
Cl- 103 mEq/L
K+ 3.7 mEq/L
Glucose 102 mg/dL
Creatinine 1.3 mg/dL
A lumbar puncture is performed. Cerebrospinal fluid analysis shows a leukocyte count of 1200/mm3 (76% segmented neutrophils, 24% lymphocytes), a protein concentration of 113 mg/dL, and a glucose concentration of 21 mg/dL. The results of blood cultures are pending. Which of the following is the most appropriate initial pharmacotherapy?
- A. Acyclovir and dexamethasone
- B. Vancomycin, ampicillin, and cefepime (Correct Answer)
- C. Ampicillin, gentamicin, and dexamethasone
- D. Ampicillin and cefotaxime
- E. Acyclovir
Toxoplasma gondii Explanation: **Vancomycin, ampicillin, and cefepime**
- The patient has bacterial meningitis with features suggesting **immunosuppression** (non-Hodgkin lymphoma, recent chemotherapy, leukopenia), placing him at risk for a broad spectrum of pathogens including *Listeria*, gram-negative rods, *S. pneumoniae*, and *N. meningitidis*.
- This combination provides broad-spectrum coverage: **vancomycin** for resistant *S. pneumoniae* and methicillin-resistant *Staphylococcus aureus* (MRSA), **ampicillin** for *Listeria monocytogenes*, and **cefepime** for gram-negative bacteria, including those common in immunocompromised hosts.
*Acyclovir and dexamethasone*
- **Acyclovir** is used for **viral meningitis/encephalitis**, which is less likely given the CSF profile (high neutrophils, low glucose, high protein) strongly indicative of bacterial infection.
- **Dexamethasone** may be considered as an adjunct in some cases of bacterial meningitis (e.g., *S. pneumoniae*), but should be given with antibiotics, and its use alone or with acyclovir is inappropriate for suspected bacterial meningitis.
*Ampicillin, gentamicin, and dexamethasone*
- While **ampicillin** covers *Listeria* and **dexamethasone** can be an adjunct, **gentamicin** is generally not a first-line agent for meningitis due to poor CSF penetration and potential for nephrotoxicity/ototoxicity, and it does not adequately cover *S. pneumoniae* or gram-negative bacilli as well as a third or fourth-generation cephalosporin.
- This combination lacks robust coverage against **resistant *S. pneumoniae*** and broad gram-negative bacteria, which are crucial in an immunocompromised patient.
*Ampicillin and cefotaxime*
- This combination covers common pathogens like *S. pneumoniae*, *N. meningitidis*, and *Listeria*. However, given the patient's **immunosuppression** and risk factors (recent travel, potential foodborne exposure), it might lack sufficient coverage for **resistant *S. pneumoniae*** (addressed by vancomycin) and **extended-spectrum gram-negative rods** (better covered by cefepime).
- The patient's risk profile warrants broader initial empiric coverage until sensitivities are known.
*Acyclovir*
- **Acyclovir** specifically targets **herpes simplex virus (HSV)**, which causes viral encephalitis/meningitis.
- The patient's CSF findings (marked pleocytosis with high neutrophils, very low glucose, and high protein) are highly suggestive of **bacterial meningitis**, not viral.
Toxoplasma gondii US Medical PG Question 3: A 26-year-old woman with poor prenatal care and minimal antenatal screening presents to the emergency department in labor. Shortly thereafter, she delivers a baby girl who subsequently demonstrates symptoms of chorioretinitis on examination. A series of postpartum screening questions is significant only for the presence of multiple cats in the mother’s household. The clinical team orders an enhanced MRI examination of the infant’s brain which reveals hydrocephalus, multiple punctate intracranial calcifications, and 2 sub-cortical ring-enhancing lesions. Which is the most likely diagnosis?
- A. Rubella
- B. Syphilis
- C. CMV
- D. HSV
- E. Toxoplasmosis (Correct Answer)
Toxoplasma gondii Explanation: ***Toxoplasmosis***
- The triad of **chorioretinitis**, **hydrocephalus**, and **intracranial calcifications** is classic for congenital toxoplasmosis.
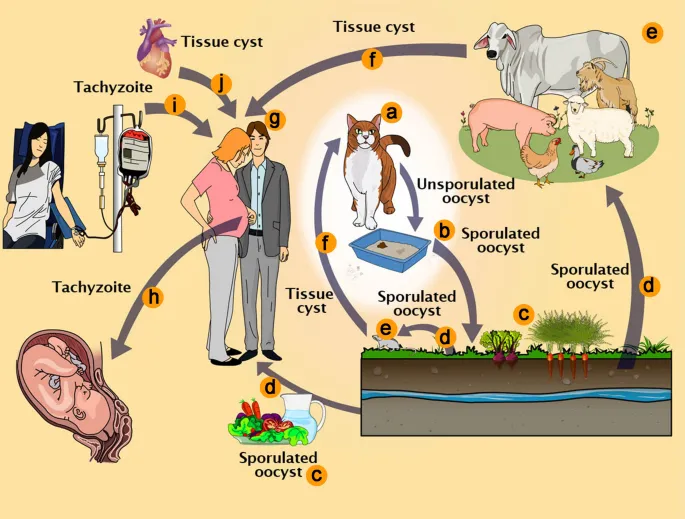
- The mother's exposure to **cats** (definitive hosts) and poor prenatal care supports the diagnosis of an acute maternal infection with vertical transmission.
*Rubella*
- Congenital rubella presents with **sensorineural hearing loss**, **cardiac defects** (e.g., patent ductus arteriosus, pulmonary artery stenosis), and **cataracts**, not chorioretinitis and intracranial calcifications.
- While it can cause microcephaly, the specific **hydrocephalus** and diffuse calcifications seen here are not typical.
*Syphilis*
- Congenital syphilis manifests with early symptoms like **hepatosplenomegaly**, **rash**, and **rhinitis**, and later signs such as **Hutchinson's teeth** and **saddle nose**.
- **Chorioretinitis** and the specific pattern of **intracranial calcifications** observed are not characteristic features of congenital syphilis.
*CMV*
- Congenital cytomegalovirus (CMV) often causes **periventricular calcifications**, **microcephaly**, and **sensorineural hearing loss**, but typically not the diffuse punctate calcifications and subcortical ring-enhancing lesions seen in this case.
- While chorioretinitis can occur, the overall clinical picture with **hydrocephalus** points away from CMV as the most likely diagnosis.
*HSV*
- Congenital herpes simplex virus (HSV) infection typically presents with **skin vesicles**, **keratoconjunctivitis**, and encephalitis, often with focal brain lesions.
- The lack of skin lesions and the specific pattern of diffuse **intracranial calcifications** and **chorioretinitis** make HSV less likely.
Toxoplasma gondii US Medical PG Question 4: A 32-year-old woman presents to your office with abdominal pain and bloating over the last month. She also complains of intermittent, copious, non-bloody diarrhea over the same time. Last month, she had a cough that has since improved but has not completely resolved. She has no sick contacts and has not left the country recently. She denies any myalgias, itching, or rashes. Physical and laboratory evaluations are unremarkable. Examination of her stool reveals the causative organism. This organism is most likely transmitted to the human host through which of the following routes?
- A. Insect bite
- B. Penetration of skin (Correct Answer)
- C. Sexual contact
- D. Inhalation
- E. Animal bite
Toxoplasma gondii Explanation: ***Penetration of skin***
- The symptoms of **abdominal pain**, **bloating**, **intermittent copious non-bloody diarrhea**, and a recent **cough** are highly suggestive of a **hookworm infection**.
- Hookworm larvae (filariform larvae) primarily penetrate the skin, usually through bare feet, as their mode of entry into the human host.
*Insect bite*
- Although some parasitic infections are transmitted by insect bites (e.g., malaria, Chagas disease), hookworms are not transmitted this way.
- **Insect-borne diseases** typically present with different clinical manifestations or geographical associations.
*Sexual contact*
- **Sexually transmitted infections** involve direct contact of mucous membranes or body fluids during sexual activity.
- Hookworm infection transmission through sexual contact is not a recognized route.
*Inhalation*
- **Inhalation** is a route of transmission for respiratory pathogens (e.g., influenza, tuberculosis) or certain fungal infections, but not for hookworms.
- While hookworm larvae migrate through the lungs, the initial infection pathway is not via inhalation.
*Animal bite*
- **Animal bites** transmit diseases like rabies or certain bacterial infections, but not parasitic hookworms.
- Hookworm infection does not result from direct contact with an animal's saliva or puncture wound.
Toxoplasma gondii US Medical PG Question 5: A 33-year-old man is brought into the emergency department with fever, lethargy, and confusion. He is a cachectic man in acute distress, unable to respond to questions or follow commands. His friend confides that the patient has been sexually active with multiple male partners and was diagnosed with HIV several months ago, but was lost to follow up. Based on prior records, his most recent CD4 count was 65 cells/uL. Which of the following is the most appropriate next step in management?
- A. CT head without contrast (Correct Answer)
- B. Lumbar puncture
- C. Recheck CD4 and HIV viral load serologies
- D. MRI brain with contrast
- E. Neurological exam with fundoscopy
Toxoplasma gondii Explanation: ***CT head without contrast***
- With signs of **increased intracranial pressure** (lethargy, confusion, inability to follow commands), performing a non-contrast CT head is crucial to rule out a **mass lesion** or **herniation risk** before any invasive procedures like a lumbar puncture.
- This patient's severely low **CD4 count** (65 cells/uL) puts him at very high risk for opportunistic central nervous system infections such as **toxoplasmosis** or **PML**, or even CNS lymphoma, which can cause mass lesions.
*Lumbar puncture*
- A **lumbar puncture** is contraindicated in the presence of signs suggestive of increased intracranial pressure until a **mass lesion** has been excluded by imaging.
- Performing a lumbar puncture in such a situation could precipitate **brain herniation**, which can be fatal.
*Recheck CD4 and HIV viral load serologies*
- While important for long-term management, rechecking these labs is not the most **immediate next step** for an acutely ill patient with severe neurological symptoms.
- The patient requires urgent diagnosis and treatment for his acute condition, which could be life-threatening, before focusing on **baseline serologies**.
*MRI brain with contrast*
- An **MRI brain with contrast** provides more detailed imaging than a CT, but a non-contrast CT is faster and sufficient for initial screening for mass lesions or herniation risk.
- In an emergency setting with an unstable patient, the **rapid accessibility** of CT makes it the preferred initial imaging modality.
*Neurological exam with fundoscopy*
- A neurological exam and fundoscopy are important components of the work-up but are **diagnostic steps**, not a management step.
- These exams will help localize the lesion and assess for **papilledema**, but imaging is required to confirm the presence of a mass or rule out herniation risk.
Toxoplasma gondii US Medical PG Question 6: A 3-day-old female newborn delivered vaginally at 36 weeks to a 27-year-old woman has generalized convulsions lasting 3 minutes. Prior to the event, she was lethargic and had difficulty feeding. The infant has two healthy older siblings and the mother's immunizations are up-to-date. The infant appears icteric. The infant's weight and length are at the 5th percentile, and her head circumference is at the 99th percentile for gestational age. There are several purpura of the skin. Ocular examination shows posterior uveitis. Cranial ultrasonography shows ventricular dilatation, as well as hyperechoic foci within the cortex, basal ganglia, and periventricular region. Which of the following is the most likely diagnosis?
- A. Congenital parvovirus infection
- B. Congenital Toxoplasma gondii infection (Correct Answer)
- C. Congenital Treponema pallidum infection
- D. Congenital cytomegalovirus infection
- E. Congenital rubella infection
Toxoplasma gondii Explanation: ***Congenital Toxoplasma gondii infection***
- **Ventricular dilatation** with widespread **hyperechoic foci** (calcifications) in the brain, along with **posterior uveitis**, highly suggests congenital toxoplasmosis.
- Other features like **generalized convulsions**, **icterus**, **purpura**, and **microcephaly** (indicated by 5th percentile weight/length vs 99th percentile head circumference discrepancy suggesting hydrocephalus with macrocephaly) are also consistent with this diagnosis.
*Congenital parvovirus infection*
- Primarily causes severe **anemia**, **hydrops fetalis**, and **myocarditis**; it does not typically present with extensive cerebral calcifications or uveitis.
- While it can lead to neurological issues, the specific brain imaging findings and ocular involvement described are not characteristic.
*Congenital Treponema pallidum infection*
- Characterized by rhinitis (**snuffles**), **hepatosplenomegaly**, **bone abnormalities** (e.g., osteochondritis), and **rash**.
- While it can cause CNS involvement and developmental delays, the distinct pattern of brain calcifications and uveitis is not typical.
*Congenital cytomegalovirus infection*
- Can cause **periventricular calcifications**, but the widespread, diffuse calcifications (cortex, basal ganglia, periventricular) are less typical than with toxoplasmosis, which often shows more diffuse parenchymal calcifications.
- While it shares features like small for gestational age, icterus, and purpura, **posterior uveitis** is more strongly associated with toxoplasmosis.
*Congenital rubella infection*
- Classic triad includes **cataracts** (or glaucoma), **sensorineural hearing loss**, and **congenital heart defects** (e.g., PDA, pulmonary artery stenosis).
- While CNS involvement (e.g., intellectual disability, microcephaly) can occur, the widespread cerebral calcifications and posterior uveitis are not characteristic.
Toxoplasma gondii US Medical PG Question 7: A 2-day old male newborn delivered vaginally at 36 weeks to a 29-year-old woman, gravida 3, para 2, has generalized convulsions lasting 2 minutes. Previous to the event, he had difficulty feeding and was lethargic. Pregnancy and delivery were uncomplicated. Apgar scores were 7 and 8 at 1 and 5 minutes, respectively. Pregnancy and delivery of the mother's first 2 children were also uncomplicated. Medications of the mother include folic acid and a multivitamin. The mother's immunizations are up-to-date. The infant appears icteric. His vital signs are within normal limits. The infant's weight and length are at the 5th percentile, and his head circumference at the 99th percentile for gestational age. There are several purpura of the skin. Ocular examination shows posterior uveitis. The patient does not pass his auditory screening tests. Cranial ultrasonography shows ventricular dilatation, as well as hyperechoic foci within the cortex, basal ganglia, and periventricular region. Which of the following is the most likely diagnosis?
- A. Congenital toxoplasmosis (Correct Answer)
- B. Congenital rubella infection
- C. Congenital parvovirus infection
- D. Congenital varicella infection
- E. Congenital syphilis infection
Toxoplasma gondii Explanation: ***Congenital toxoplasmosis***
- The constellation of **hydrocephalus** (ventricular dilatation, large head circumference), **intracranial calcifications** (hyperechoic foci), and **chorioretinitis/uveitis** is pathognomonic for congenital toxoplasmosis.
- Other supporting features include **seizures**, **icterus**, **purpura** (thrombocytopenia), and **growth restriction** (weight and length at 5th percentile).
*Congenital rubella infection*
- Characterized by a triad of **cataracts**, **sensorineural hearing loss** (failed auditory screening), and **patent ductus arteriosus** or other cardiac defects.
- While rubella can cause microcephaly and purpura, the classic ocular finding is cataracts, not uveitis, and intracranial calcifications are not typical.
*Congenital parvovirus infection*
- Primarily causes **fetal hydrops**, **severe anemia**, and **myocarditis** due to its tropism for erythroid progenitor cells.
- It is not associated with intracranial calcifications, uveitis, or hydrocephalus as seen in this case.
*Congenital varicella infection*
- Typically results in **skin scarring** (zigzag pattern), **limb hypoplasia**, **chorioretinitis**, and **neurological defects** such as cortical atrophy, but not significant hydrocephalus or extensive calcifications.
- The absence of characteristic skin scarring and the presence of hydrocephalus and extensive calcifications make this diagnosis less likely.
*Congenital syphilis infection*
- Can present with varied symptoms, including **hepatosplenomegaly**, **bone abnormalities** (e.g., periostitis), **blueberry muffin rash** (due to dermal erythropoiesis), and **snuffles**.
- While it can cause neurological symptoms, the classic triad of hydrocephalus, intracranial calcifications, and chorioretinitis is not typical for congenital syphilis.
Toxoplasma gondii US Medical PG Question 8: A pathologist receives a patient sample for analysis. Cells in the sample are first labeled with fluorescent antibodies and then passed across a laser beam in a single file of particles. The light scatter and fluorescent intensity of the particles are plotted on a graph; this information is used to characterize the sample. This laboratory method would be most useful to establish the diagnosis of a patient with which of the following?
- A. Ventricular septal defect and facial dysmorphism with low T-lymphocyte count
- B. Painless generalized lymphadenopathy with monomorphic cells and interspersed benign histiocytes on histology
- C. Pancytopenia and deep vein thrombosis with intermittent hemoglobinuria (Correct Answer)
- D. Multiple opportunistic infections with decreased CD4 counts
- E. Vesicular lesions with dermatomal distribution and dendritic corneal ulcers
Toxoplasma gondii Explanation: ***Pancytopenia and deep vein thrombosis with intermittent hemoglobinuria***
- The described laboratory method is **flow cytometry**, which is the **gold standard for diagnosing paroxysmal nocturnal hemoglobinuria (PNH)** by detecting the absence of **CD55** and **CD59** on red blood cells due to impaired GPI anchor synthesis.
- PNH classically presents with **pancytopenia**, **hemolytic anemia** (leading to hemoglobinuria), and a high risk of **thrombosis** (e.g., deep vein thrombosis).
*Ventricular septal defect and facial dysmorphism with low T-lymphocyte count*
- This clinical picture suggests **DiGeorge syndrome**, which involves a developmental defect of the **third and fourth pharyngeal pouches**, leading to thymic hypoplasia and **T-cell deficiency**.
- While flow cytometry is used to quantify T-lymphocyte subsets (e.g., CD3, CD4, CD8), the primary method for diagnosing DiGeorge syndrome is **fluorescent in situ hybridization (FISH)** for a **22q11 deletion**, making it less ideal for flow cytometry diagnosis.
*Painless generalized lymphadenopathy with monomorphic cells and interspersed benign histiocytes on histology*
- This description with "**monomorphic cells**" is more consistent with certain **non-Hodgkin lymphomas** (e.g., Burkitt lymphoma) rather than Hodgkin lymphoma, which typically shows a **polymorphic** cellular infiltrate.
- While flow cytometry can be useful in characterizing lymphomas by identifying cell surface markers, the diagnosis is primarily established by **lymph node biopsy and histopathology** with **immunohistochemistry**, making flow cytometry a supplementary rather than primary diagnostic tool.
*Multiple opportunistic infections with decreased CD4 counts*
- This presentation is highly suggestive of **HIV infection leading to AIDS**. The "decreased CD4 counts" are a key diagnostic and prognostic marker.
- While flow cytometry is used to **monitor CD4 cell counts** in HIV patients, the initial diagnosis of HIV is established via **antibody/antigen combination tests** and confirmed by **Western blot** or **PCR for viral load**, not by flow cytometry.
*Vesicular lesions with dermatomal distribution and dendritic corneal ulcers*
- This clinical presentation points to **herpes zoster ophthalmicus** (shingles affecting the eye due to **varicella-zoster virus** reactivation).
- Diagnosis is primarily **clinical** based on the characteristic rash and eye findings, although **PCR** of vesicular fluid can confirm VZV infection. Flow cytometry has no role in this diagnosis.
Toxoplasma gondii US Medical PG Question 9: A 28-year-old female in the 2nd trimester of pregnancy is diagnosed with primary Toxoplasma gondii infection. Her physician fears that the fetus may be infected in utero. Which of the following are associated with T. gondii infection in neonates?
- A. Hutchinson’s teeth, saddle nose, short maxilla
- B. Deafness, seizures, petechial rash
- C. Hydrocephalus, chorioretinitis, intracranial calcifications (Correct Answer)
- D. Patent ductus arteriosus, cataracts, deafness
- E. Temporal encephalitis, vesicular lesions
Toxoplasma gondii Explanation: ***Hydrocephalus, chorioretinitis, intracranial calcifications***
- These are the classic triad of symptoms (known as the **Sabin triad**) often associated with **congenital toxoplasmosis**.
- **Hydrocephalus** results from obstruction of cerebrospinal fluid flow, **chorioretinitis** can lead to vision loss, and **intracranial calcifications** are a hallmark of the infection's impact on the brain.
*Hutchinson’s teeth, saddle nose, short maxilla*
- These are characteristic features of **congenital syphilis**, not *Toxoplasma gondii* infection.
- **Hutchinson's triad** includes Hutchinson's teeth, interstitial keratitis, and sensorineural hearing loss in congenital syphilis.
*Deafness, seizures, petechial rash*
- While seizures can occur with severe congenital infections, this combination is more suggestive of **cytomegalovirus (CMV)** infection or **rubella**, which can cause petechial rash (blueberry muffin baby) and profound sensorineural deafness.
- *Toxoplasma gondii* does not typically cause a petechial rash as a primary symptom.
*Patent ductus arteriosus, cataracts, deafness*
- This constellation of symptoms is highly characteristic of **congenital rubella syndrome**.
- **Cardiac defects** (like patent ductus arteriosus), **ocular abnormalities** (cataracts), and **sensorineural deafness** are classical signs of rubella.
*Temporal encephalitis, vesicular lesions*
- **Temporal encephalitis** with vesicular lesions, particularly in a neonatal context, is a classic presentation of **congenital herpes simplex virus (HSV) infection**.
- *Toxoplasma gondii* can cause encephalitis, but not typically with vesicular lesions or a primary predilection for the temporal lobe in this specific clinical presentation.
Toxoplasma gondii US Medical PG Question 10: A 2900-g (6.4-lb) male newborn is delivered at term to a 29-year-old primigravid woman. His mother had no routine prenatal care. She reports that the pregnancy was uncomplicated apart from a 2-week episode of a low-grade fever and swollen lymph nodes during her early pregnancy. She has avoided all routine vaccinations because she believes that “natural immunity is better.” The newborn is at the 35th percentile for height, 15th percentile for weight, and 3rd percentile for head circumference. Fundoscopic examination shows inflammation of the choroid and the retina in both eyes. A CT scan of the head shows diffuse intracranial calcifications and mild ventriculomegaly. Prenatal avoidance of which of the following would have most likely prevented this newborn's condition?
- A. Undercooked pork (Correct Answer)
- B. Raw cow milk products
- C. Mosquito bites
- D. Exposure to unvaccinated children
- E. Unprotected sexual intercourse
Toxoplasma gondii Explanation: ***Undercooked pork***
- The constellation of **hydrocephalus**, **chorioretinitis**, and **intracranial calcifications** (classic triad) in a newborn, coupled with maternal symptoms of fever and lymphadenopathy, is highly suggestive of **congenital toxoplasmosis**.
- **Toxoplasmosis** is caused by the parasite *Toxoplasma gondii*, which can be acquired by consuming **undercooked meat** (especially pork and lamb) or exposure to **contaminated cat feces/litter**.
- Avoiding undercooked meat during pregnancy is a key preventive measure.
*Raw cow milk products*
- While raw milk can transmit various infections (e.g., *Listeria*, *Brucella*, *E. coli*), it is not a typical source of **congenital toxoplasmosis**.
- **Listeriosis** can cause congenital infection, but the symptoms (e.g., sepsis, granulomatosis infantiseptica) differ from those described.
*Mosquito bites*
- Mosquitoes are vectors for diseases like **Zika virus**, **Malaria**, and **Dengue fever**, which can affect newborns.
- **Congenital Zika syndrome** can cause microcephaly, but typically not the classic triad of toxoplasmosis, and malaria presents with fever and hemolytic anemia.
*Exposure to unvaccinated children*
- This primarily refers to common childhood infections like **measles**, **rubella**, and **chickenpox**.
- **Congenital rubella syndrome** can cause cataracts, heart defects, and sensorineural hearing loss, but not the specific triad of chorioretinitis, hydrocephalus, and intracranial calcifications.
*Unprotected sexual intercourse*
- This is a route for sexually transmitted infections (STIs), such as **HIV**, **syphilis**, and **gonorrhea**, which can be transmitted vertically.
- **Congenital syphilis** can cause bone abnormalities, rash, and hepatosplenomegaly, but not the distinct neurological and ocular findings seen here.
More Toxoplasma gondii US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.