Malaria parasites and life cycle US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Malaria parasites and life cycle. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
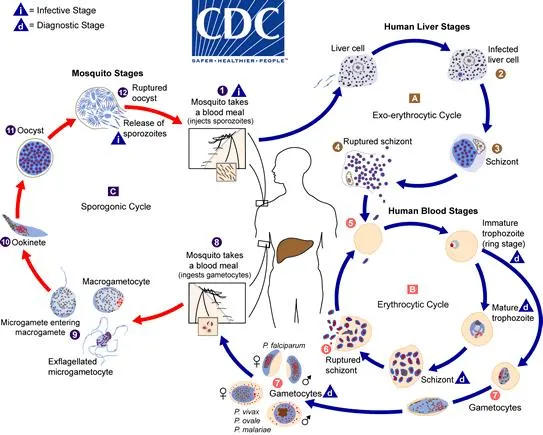
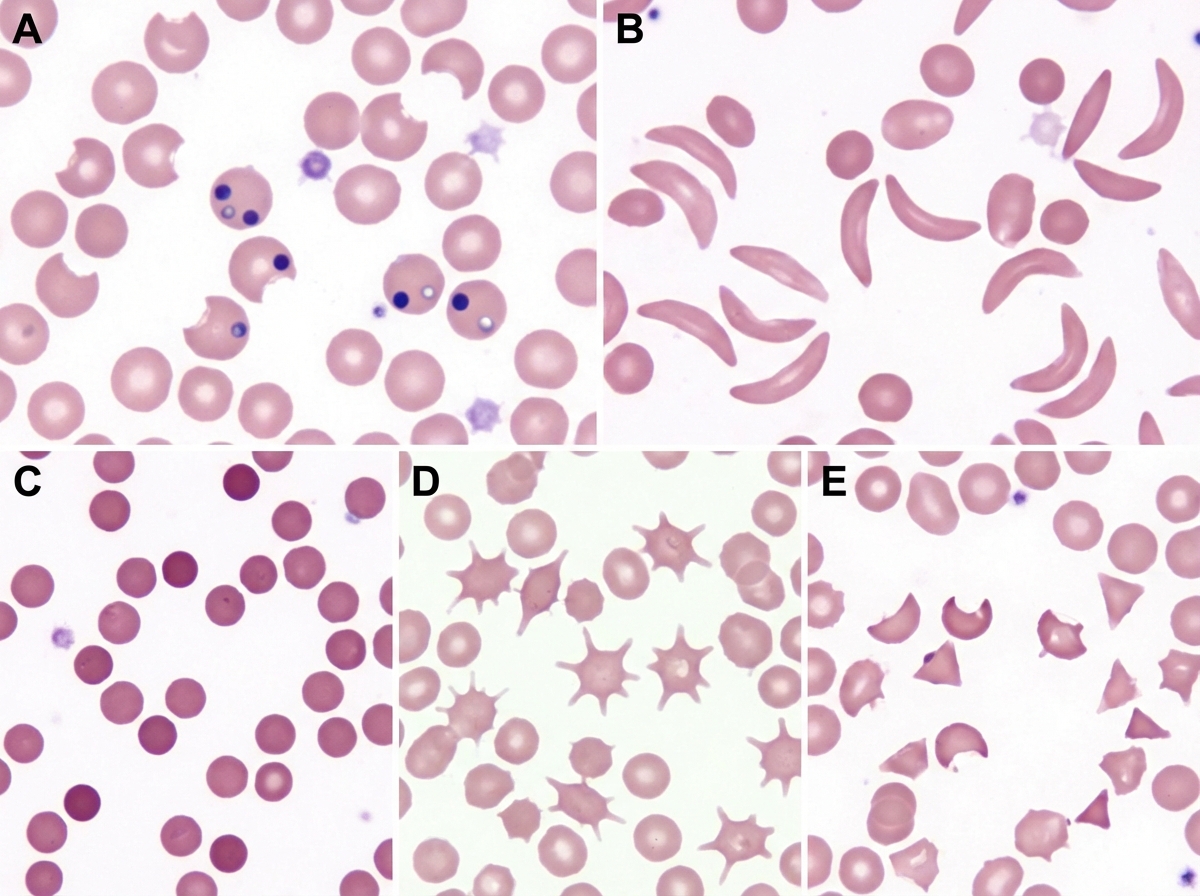
Malaria parasites and life cycle US Medical PG Question 1: A 68-year-old man of Mediterranean descent comes to the clinic with complaints of fatigue for the past month. He reports that it is increasingly difficult for him to complete his after-dinner walks as he would get breathless and tired around 10 minutes. He endorses dizziness and an upper respiratory infection last week for which he “took a lot of aspirin.” Past medical history is significant for malaria 10 years ago (for which he was adequately treated with anti-malarial medications) and aortic stenosis status post prosthetic valve replacement 5 months ago. When asked if he has had similar episodes before, he claims, “Never! I’ve been as healthy as a horse until my heart surgery.” Physical examination is significant for mild scleral icterus bilaterally and a faint systolic murmur. Which of the following images represents a potential peripheral smear in this patient?
- A. B
- B. E
- C. C
- D. D
- E. A (Correct Answer)
Malaria parasites and life cycle Explanation: ***A***
- Image A depicts **bite cells** and **Heinz bodies**, which are characteristic findings in **hemolysis** caused by **G6PD deficiency**. This patient's Mediterranean descent, recent aspirin use (an oxidant drug), and symptoms of fatigue, dyspnea, dizziness, and scleral icterus are highly suggestive of an acute hemolytic crisis in G6PD deficiency patients.
- **G6PD deficiency** is an X-linked recessive disorder prevalent in Mediterranean populations, where certain medications (like aspirin, sulfonamides, antimalarials) or infections can trigger episodes of acute hemolytic anemia due to oxidative stress.
*B*
- Image B shows **sickle cells**, which are characteristic of **sickle cell anemia**. While individuals with sickle cell disease can experience fatigue and anemia, there are no specific clinical elements in the vignette that point to sickle cell disease (e.g., pain crises, vaso-occlusion, or chronic hemolytic anemia from birth).
- The patient's presentation with an acute episode triggered by aspirin is less typical for a first presentation of sickle cell anemia at this age, and his prior malaria exposure is not directly linked to sickle cell disease as the cause of this acute presentation.
*E*
- Image E illustrates **schistocytes** (fragmented red blood cells) and potentially an occasional spherocyte, which are hallmarks of **microangiopathic hemolytic anemia (MAHA)**, often seen in conditions like **thrombotic thrombocytopenic purpura (TTP)**, **hemolytic uremic syndrome (HUS)**, or **disseminated intravascular coagulation (DIC)**.
- While the patient has a prosthetic valve (which can cause hemolytic anemia through mechanical stress, leading to schistocytes), the primary trigger for this acute episode appears to be G6PD deficiency, given the history of aspirin use and Mediterranean descent.
*C*
- Image C displays **spherocytes**, which are small, dense red blood cells lacking central pallor, commonly seen in **hereditary spherocytosis** or **autoimmune hemolytic anemia (AIHA)**.
- Although the patient's symptoms suggest hemolysis, the trigger (aspirin) and his ethnic background make G6PD deficiency a more likely diagnosis than hereditary spherocytosis or AIHA, which would typically present differently or have other specific findings.
*D*
- Image D demonstrates **acanthocytes (spur cells)**, which are red blood cells with irregular, spiny projections, typically associated with severe **liver disease** (e.g., cirrhosis, alcoholic liver disease), **abetalipoproteinemia**, or **hypothyroidism**.
- There are no clinical features in the vignette to suggest any of these underlying conditions, and acanthocytes are not characteristic of the acute hemolytic anemia described.
Malaria parasites and life cycle US Medical PG Question 2: An investigator is studying the outcomes of a malaria outbreak in an endemic region of Africa. 500 men and 500 women with known malaria exposure are selected to participate in the study. Participants with G6PD deficiency are excluded from the study. The clinical records of the study subjects are reviewed and their peripheral blood smears are evaluated for the presence of Plasmodium trophozoites. Results show that 9% of the exposed population does not have clinical or laboratory evidence of malaria infection. Which of the following best explains the absence of infection seen in this subset of participants?
- A. Translocation of c-myc gene
- B. Glutamic acid substitution in the β-globin chain (Correct Answer)
- C. Inherited mutation affecting ribosome synthesis
- D. Inherited defect in erythrocyte membrane ankyrin protein
- E. Defective X-linked ALA synthase gene
Malaria parasites and life cycle Explanation: ***Glutamic acid substitution in the β-globin chain***
- This describes **sickle cell trait (heterozygous HbS)**, which confers significant protection against severe malaria, explaining the absence of infection despite exposure.
- Individuals with sickle cell trait have **abnormally shaped red blood cells** under low oxygen conditions, which are less hospitable for **Plasmodium falciparum** growth and are more rapidly cleared by the spleen.
*Translocation of c-myc gene*
- A **t(8;14) translocation of the c-myc gene** is characteristic of **Burkitt lymphoma**, a B-cell malignancy, and has no protective effect against malaria.
- This genetic alteration leads to overexpression of **c-myc**, a proto-oncogene, contributing to uncontrolled cell growth.
*Inherited mutation affecting ribosome synthesis*
- Defects in **ribosome synthesis** can lead to various **ribosomopathies**, affecting cell proliferation and function, but they are not known to provide protection against malaria.
- Such mutations often result in syndromes with **developmental abnormalities** or **bone marrow failure**.
*Inherited defect in erythrocyte membrane ankyrin protein*
- Defects in **ankyrin protein** are associated with **hereditary spherocytosis**, causing fragile, spherical red blood cells that are prematurely destroyed.
- While hereditary spherocytosis can reduce malaria severity, its role in preventing initial infection is less pronounced, and the question refers to absence of infection.
*Defective X-linked ALA synthase gene*
- A defective **X-linked ALA synthase gene** (ALAS2) is associated with **X-linked sideroblastic anemia**, causing impaired heme synthesis.
- This condition is characterized by **microcytic, hypochromic anemia** and iron overload in erythroid precursors, with no known protective effect against malaria.
Malaria parasites and life cycle US Medical PG Question 3: A 31-year-old male traveler in Thailand experiences fever, headache, and excessive sweating every 48 hours. Peripheral blood smear shows trophozoites and schizonts indicative of Plasmodia infection. The patient is given chloroquine and primaquine. Primaquine targets which of the following Plasmodia forms:
- A. Schizont
- B. Hypnozoite (Correct Answer)
- C. Trophozoite
- D. Merozoite
- E. Sporozoite
Malaria parasites and life cycle Explanation: ***Hypnozoite***
- **Primaquine** is a **radical cure** for malaria caused by *Plasmodium vivax* and *Plasmodium ovale* because it targets the dormant **hypnozoite** forms in the liver.
- The presence of **hypnozoites** leads to relapses, as they can reactivate and re-initiate the erythrocytic cycle.
*Schizont*
- **Schizonts** are merozoite-producing forms in red blood cells (**erythrocytic schizonts**) or liver cells (**hepatic schizonts**).
- While chloroquine targets **erythrocytic schizonts**, primaquine's primary unique action is against the dormant liver stages.
*Trophozoite*
- **Trophozoites** are the feeding and growing stages of the parasite within red blood cells, which mature into schizonts.
- **Chloroquine** is highly effective against **erythrocytic trophozoites** and schizonts, resolving acute malarial symptoms.
*Merozoite*
- **Merozoites** are released from ruptured schizonts and infect new red blood cells during the erythrocytic cycle.
- No specific antimalarial drug solely targets **merozoites** as a primary form; they are an infective stage for red blood cells.
*Sporozoite*
- **Sporozoites** are the forms injected by infected mosquitoes, which then travel to the liver and infect hepatocytes.
- While some drugs like atovaquone have activity against sporozoites, primaquine is specifically indicated for destroying the **hypnozoite** stage, preventing relapses.
Malaria parasites and life cycle US Medical PG Question 4: An 8-year-old boy is brought to the physician because of a 1-day history of severe left hand pain. He has had similar painful episodes in the past that required hospitalization. Physical examination shows pale conjunctivae. There is tenderness on palpation of the wrist and the small joints of the left hand. Peripheral blood smear shows crescent-shaped erythrocytes. He is started on a pharmacologic agent that is known to cause macrocytosis. This drug causes an arrest in which of the following cell cycle phases?
- A. S phase (Correct Answer)
- B. G0 phase
- C. G2 phase
- D. M phase
- E. G1 phase
Malaria parasites and life cycle Explanation: ***S phase***
- This patient presents with **sickle cell disease** given the history of recurrent severe pain episodes, pale conjunctivae (suggesting anemia), and **crescent-shaped erythrocytes** on peripheral blood smear.
- The pharmacologic agent that causes **macrocytosis** and is used in sickle cell disease is **hydroxyurea** through increasing **fetal hemoglobin**; it primarily works by inhibiting **ribonucleotide reductase**, an enzyme essential for **DNA synthesis**, thereby arresting cells in the **S phase**.
*G0 phase*
- The **G0 phase** is a resting phase where cells are not actively dividing or preparing to divide.
- Hydroxyurea targets rapidly dividing cells by interfering with DNA replication, so it does not primarily arrest cells in the inactive G0 phase.
*G2 phase*
- The **G2 phase** is the growth phase where the cell checks its DNA and prepares for mitosis.
- While hydroxyurea can indirectly affect the G2/M checkpoint, its direct mechanism of action is primarily in the S phase by preventing proper DNA synthesis.
*M phase*
- The **M phase** is the stage of cell division, including mitosis and cytokinesis.
- Drugs that block the M phase typically interfere with **microtubule formation** (e.g., vinca alkaloids, taxanes), which is not the primary mechanism of hydroxyurea.
*G1 phase*
- The **G1 phase** is the initial growth phase where the cell grows and synthesizes proteins.
- While cells must pass through G1 before entering S phase, hydroxyurea's direct DNA synthesis inhibition occurs during the S phase rather than preventing entry into S from G1.
Malaria parasites and life cycle US Medical PG Question 5: A 42-year-old man comes to his physician with a history of fever, non-bloody diarrhea, and headache for 10 days. He also complains of anorexia and abdominal pain. He returned from a trip to India 3 weeks ago. His temperature is 40.0°C (104.0°F), pulse is 65/min, respirations are 15/min, and blood pressure is 135/80 mm Hg. He has developed a blanchable rash on his chest and trunk. A photograph of the rash is shown. Examination of the heart, lungs, and abdomen show no abnormalities. Laboratory studies show:
Hemoglobin 15 g/dL
Mean corpuscular volume 95 μm3
White blood cell count 3400/mm3
Percent segmented neutrophils 40%
Which of the following is the most likely diagnosis?
- A. Leptospirosis
- B. Enteric fever (Correct Answer)
- C. Dengue fever
- D. Malaria
- E. Nontyphoidal salmonellosis
Malaria parasites and life cycle Explanation: ***Enteric fever***
- The constellation of **fever**, **non-bloody diarrhea**, **bradycardia** (pulse 65/min with 40°C fever), **leukopenia** (WBC 3400/mm³), **rose spots** (blanchable rash on chest/trunk), and recent travel to **India** (endemic area) is highly characteristic of enteric fever caused by *Salmonella Typhi* or *Paratyphi*.
- Abdominal pain, anorexia, and headache are also common symptoms, and the relatively low **neutrophil percentage** (40%) further supports the diagnosis of a bacterial infection with atypical white blood cell response.
*Leptospirosis*
- While leptospirosis can cause **fever** and **headache** and is found in tropical regions, it typically presents with **conjunctival suffusion**, **muscle pain**, and sometimes **jaundice** or **renal involvement**, none of which are detailed here.
- Exposure usually involves contact with contaminated water or soil, and **diarrhea** is less common than in enteric fever.
*Dengue fever*
- Dengue fever is characterized by **high fever**, severe **myalgia** and **arthralgia** ("breakbone fever"), and often a **maculopapular rash**, but **bradycardia** and **leukopenia** with low neutrophils are not typical features.
- **Hemorrhagic manifestations** are also a concern in severe dengue, which are not described.
*Malaria*
- Malaria presents with cyclical **fever** (often paroxysmal), **chills**, **sweats**, and frequently causes **anemia** and **thrombocytopenia**.
- While **leukopenia** can occur, the presence of **rose spots** and sustained fever with relative **bradycardia** point away from malaria as the primary diagnosis.
*Nontyphoidal salmonellosis*
- This typically causes **gastroenteritis** with **diarrhea**, **vomiting**, and **fever**, which is usually self-limiting.
- It would not typically present with **rose spots**, pronounced **bradycardia**, or a prolonged course with systemic symptoms suggestive of enteric fever.
Malaria parasites and life cycle US Medical PG Question 6: A 32-year-old man is brought to the emergency department with fever, dyspnea, and impaired consciousness. His wife reports that he has also had an episode of dark urine today. Two weeks ago, he returned from a trip to the Republic of Congo. His temperature is 39.4°C (103°F), pulse is 114/min, and blood pressure is 82/51 mm Hg. Physical examination shows scleral icterus. Decreased breath sounds and expiratory crackles are heard on auscultation of the lungs bilaterally. His hemoglobin concentration is 6.3 g/dL. A blood smear shows red blood cells with normal morphology and ring-shaped inclusions. Further laboratory testing shows normal rates of NADPH production. Which of the following is the most appropriate pharmacotherapy for this patient?
- A. Proguanil
- B. Dapsone
- C. Chloroquine
- D. Artesunate (Correct Answer)
- E. Atovaquone
Malaria parasites and life cycle Explanation: ***Artesunate***
- This patient presents with **severe malaria**, indicated by fever, impaired consciousness, hypotension, dyspnea, dark urine (hemoglobinuria), scleral icterus (hemolysis), and anemia, following travel to an endemic area (Republic of Congo). The blood smear finding of **ring-shaped inclusions** with normal red cell morphology is characteristic of **Plasmodium falciparum** infection.
- **Artesunate** is the drug of choice for **severe malaria** due to its rapid parasitic clearance and superior efficacy compared to other antimalarials, especially in regions with high chloroquine resistance, as is typical in the Republic of Congo for *P. falciparum*.
*Proguanil*
- Proguanil is primarily used in **malaria prophylaxis** or in combination with other drugs (e.g., atovaquone-proguanil) for uncomplicated malaria.
- It is not indicated as monotherapy for **severe *P. falciparum* malaria**, nor is it suitable for emergency treatment of life-threatening infections.
*Dapsone*
- Dapsone is an **antibiotic** primarily used in the treatment of **leprosy** and prevention of *Pneumocystis jirovecii* pneumonia or toxoplasmosis in immunocompromised patients.
- It has **no significant role** in the treatment of malaria, especially severe *P. falciparum* infection.
*Chloroquine*
- Chloroquine was historically a first-line treatment for malaria but is largely ineffective against **chloroquine-resistant *P. falciparum***, which is widely prevalent in the Republic of Congo and contributes to severe disease.
- Administering chloroquine in this context would likely lead to **treatment failure** and worsening of the patient's severe condition.
*Atovaquone*
- Atovaquone, usually combined with proguanil (Malarone), is effective for **uncomplicated malaria** and prophylaxis.
- However, it is **not the preferred agent for severe malaria** due to slower action and lack of intravenous formulation for initial critical management.
Malaria parasites and life cycle US Medical PG Question 7: A 7-year-old boy is brought to the emergency department by his parents with a 2-day history of severe fatigue. His parents say that he has no past medical history, but caught an illness that was going around his school 1 week ago. While ill, he had several days of abdominal pain and bloody diarrhea. His family history is significant for several family members who required blood transfusions, and he lives in an old house. Physical exam reveals conjunctival pallor and mild jaundice. Which of the following would most likely be seen on peripheral blood smear in this patient?
- A. Schistocytes (Correct Answer)
- B. Degmacytes
- C. Spherocytes
- D. Codocytes
- E. Echinocytes
Malaria parasites and life cycle Explanation: ***Schistocytes***
- This patient's presentation with recent **bloody diarrhea**, **fatigue**, **conjunctival pallor**, and **mild jaundice** is highly suggestive of **hemolytic uremic syndrome (HUS)**, often triggered by Shiga toxin-producing E. coli (STEC) infection.
- **Schistocytes**, or fragmented red blood cells, are a hallmark of **microangiopathic hemolytic anemia (MAHA)**, which is central to HUS pathogenesis due to damage to red blood cells as they pass through obstructed microvessels.
*Degmacytes*
- **Degmacytes**, also known as **bite cells**, are seen in conditions involving **oxidative stress** leading to Heinz body formation, such as **G6PD deficiency** or unstable hemoglobin variants.
- While hemolysis is present in this patient, the clinical context of prior diarrheal illness and the specific findings point away from primary oxidative damage.
*Spherocytes*
- **Spherocytes** are typically associated with **hereditary spherocytosis** or **autoimmune hemolytic anemia (AIHA)**.
- These conditions cause red blood cells to lose their biconcave shape and become spherical, leading to premature destruction, but they do not typically follow a diarrheal illness in this manner.
*Codocytes*
- **Codocytes**, or **target cells**, are characteristic of **thalassemias**, **liver disease**, and **iron deficiency anemia**.
- They indicate an increase in surface area to volume ratio of the red blood cell and are not typically seen with the acute hemolytic picture presented here.
*Echinocytes*
- **Echinocytes**, or **burr cells**, are often associated with **uremia**, **pyruvate kinase deficiency**, and sometimes occur as an artifact of blood smear preparation.
- While HUS can lead to kidney injury, echinocytes are not the primary and most characteristic finding in the acute hemolytic phase of HUS.
Malaria parasites and life cycle US Medical PG Question 8: A 46-year-old man comes to the physician because of a 1-week history of headache, muscle pain, and recurrent fever spikes that occur without a noticeable rhythm. Two weeks ago, he returned from a 5-week-long world trip during which he climbed several mountains in India, Africa, and Appalachia. Chemoprophylaxis with chloroquine was initiated one week prior to the trip. Physical examination shows jaundice. The spleen is palpated 2 cm below the left costal margin. His hemoglobin concentration is 10 g/dL. A photomicrograph of a peripheral blood smear is shown. Which of the following agents is the most likely cause of this patient's findings?
- A. Chikungunya virus
- B. Trypanosoma cruzi
- C. Leishmania donovani
- D. Plasmodium falciparum (Correct Answer)
- E. Trypanosoma brucei
Malaria parasites and life cycle Explanation: **Plasmodium falciparum**
- The image shows **multiple ring forms** and **applique forms** within red blood cells, which are characteristic of *Plasmodium falciparum* malaria. The clinical presentation of **headache, muscle pain, recurrent fever spikes without a noticeable rhythm, jaundice, splenomegaly, and anemia (Hb 10 g/dL)** in a traveler returning from India and Africa is highly consistent with malaria, especially given the chloroquine chemoprophylaxis which is often ineffective against chloroquine-resistant strains of *P. falciparum*.
- *P. falciparum* can cause severe disease, including **anemia** due to red blood cell destruction and **jaundice** due to hemolysis and liver involvement, and is notorious for its **irregular fever patterns** early in the infection cycle.
*Chikungunya virus*
- Chikungunya typically presents with **high fever, severe polyarthralgia**, and rash, but does not cause the parasitemia or specific red blood cell morphology seen in the image.
- While present in endemic regions like India and Africa, it does not lead to **anemia, splenomegaly, or jaundice** to the extent seen in this patient, nor does it appear on a blood smear as intracellular parasites.
*Trypanosoma cruzi*
- *Trypanosoma cruzi* causes **Chagas disease**, which is endemic to **Central and South America**, not India or Africa.
- While it can be found in blood smears during the acute phase (trypomastigotes), its morphology differs significantly from the ring forms seen, and the overall clinical picture of **fever, jaundice, and marked splenomegaly with characteristic RBC parasites** does not fit Chagas disease.
*Leishmania donovani*
- *Leishmania donovani* causes **visceral leishmaniasis (kala-azar)**, characterized by **prolonged fever, splenomegaly, hepatomegaly, pancytopenia**, and weight loss.
- While present in India and Africa, the parasites (**amastigotes**) are typically found within **macrophages** in bone marrow, spleen, or liver aspirates, not as ring forms within red blood cells on a peripheral blood smear.
*Trypanosoma brucei*
- *Trypanosoma brucei* causes **African sleeping sickness**, which involves **fever, headache, joint pain, neurological symptoms**, and lymphadenopathy (Winterbottom's sign).
- The parasites (trypomastigotes) are observed extracellularly in the blood, lymph, or CSF, and have a distinct **elongated, flagellated morphology** that is completely different from the intracellular ring forms seen in the provided image.
Malaria parasites and life cycle US Medical PG Question 9: A 37-year-old man makes an appointment with his primary care physician because he has been feeling tired and is no longer able to play on a recreational soccer team. He also says his coworkers have commented that he appears pale though he has not noticed any changes himself. He says that he has been generally healthy and that the only notable event that happened in the last year is that he went backpacking all over the world. Based on clinical suspicion, a series of blood tests are performed with partial results presented below:
Hemoglobin: 9.8 g/dL
Platelet count: 174,000/mm^3
Mean corpuscular volume: 72 µm^3 (normal: 80-100 µm^3)
Iron: 22 µg/dL (normal: 50-170 µg/dL)
Ferritin: 8 ng/mL (normal: 15-200 ng/mL)
Lactate dehydrogenase: 57 U/L (normal: 45-90 U/L)
Urine hemoglobin: absent
Infection with which of the following types of organisms could lead to this pattern of findings?
- A. Nematode (Correct Answer)
- B. Mosquito-borne protozoa
- C. Double-stranded virus
- D. Single-stranded virus
- E. Tick-borne protozoa
Malaria parasites and life cycle Explanation: ***Nematode***
- The patient's symptoms (fatigue, pallor) and lab results (**microcytic anemia** with **low hemoglobin**, **low MCV**, **low iron**, and **low ferritin**) are highly suggestive of **iron deficiency anemia**. The history of backpacking worldwide increases the suspicion of **hookworm infection**, which is a nematode that causes chronic gastrointestinal blood loss leading to iron deficiency.
- **Hookworms** (e.g., *Ancylostoma duodenale*, *Necator americanus*) attach to the intestinal wall, causing persistent blood loss as they feed, which depletes iron stores over time.
*Mosquito-borne protozoa*
- **Mosquito-borne protozoa** primarily refers to *Plasmodium* species which cause malaria. While malaria can cause anemia, it typically presents with **hemolytic anemia** (elevated LDH, jaundice), intermittent fevers, and splenomegaly, not the profound iron deficiency seen here.
- The anemia in malaria is usually **normocytic or macrocytic** due to increased erythropoiesis, and profound iron deficiency is not the primary mechanism.
*Double-stranded virus*
- **Double-stranded viruses** (e.g., adenoviruses, herpesviruses, some papillomaviruses) typically cause acute infections, and while some can lead to anemia through bone marrow suppression or chronic inflammation, they do not directly cause **iron deficiency anemia** with this specific lab profile.
- The clinical picture of chronic fatigue and iron depletion after travel is not characteristic of common viral infections caused by double-stranded viruses.
*Single-stranded virus*
- **Single-stranded viruses** (e.g., influenza, measles, HIV, dengue, enteroviruses) cause a wide range of illnesses. While some can lead to anemia, often through **bone marrow suppression** or chronic inflammation, they are not typically associated with the profound **iron deficiency** and microcytic anemia seen in this patient.
- Travel history can be relevant for some single-stranded viral infections (e.g., HIV, dengue), but the specific laboratory findings point away from a primary viral etiology for the anemia.
*Tick-borne protozoa*
- **Tick-borne protozoa** most commonly refers to *Babesia* species, which cause babesiosis. This disease primarily leads to **hemolytic anemia** (intravascular hemolysis, elevated LDH), fever, chills, and fatigue, which is distinct from the **iron deficiency anemia** presented in the case.
- **Babesiosis** would typically present with signs of hemolysis, such as elevated LDH and sometimes hemoglobinuria, which are absent in this patient.
Malaria parasites and life cycle US Medical PG Question 10: A 4-year-old girl presents with recurrent abdominal pain and a low-grade fever for the past 2 months. The patient’s mother says that she has lost her appetite which has caused some recent weight loss. She adds that the patient frequently plays outdoors with their pet dog. The patient is afebrile and vital signs are within normal limits. On physical examination, conjunctival pallor is present. Abdominal examination reveals a diffusely tender abdomen and significant hepatomegaly. There is also a solid mass palpable in the right upper quadrant measuring about 3 x 4 cm. Laboratory findings are significant for the following:
Hemoglobin (Hb%) 9.9 g/dL
Total count (WBC) 26,300/µL
Differential count
Neutrophils 36%
Lymphocytes 16%
Eosinophils 46%
Platelets 200,000/mm3
Erythrocyte sedimentation rate 56 mm/h
C-reactive protein 2 mg/L
Serum globulins 5 g/dL
Laparoscopic resection of the mass is performed, and a tissue sample is sent for histopathology. Which of the following is the organism most likely responsible for this patient’s condition?
- A. Ancylostoma braziliense
- B. Ascaris lumbricoides
- C. Toxocara canis (Correct Answer)
- D. Trichuris trichiura
- E. Toxocara cati
Malaria parasites and life cycle Explanation: ***Toxocara canis***
- The child's history of playing outdoors with a pet dog, **eosinophilia**, **hepatomegaly**, abdominal mass, and **elevated globulins** are highly suggestive of **visceral larva migrans (VLM)**, most commonly caused by *Toxocara canis*.
- *Toxocara canis* larvae migrate through human tissues, particularly the liver, causing granuloma formation that can present as palpable masses and systemic symptoms.
*Ancylostoma braziliense*
- This hookworm primarily causes **cutaneous larva migrans**, presenting as an intensely pruritic, serpiginous rash.
- It does not typically cause systemic symptoms like hepatomegaly, abdominal masses, or significant eosinophilia in the way described.
*Ascaris lumbricoides*
- *Ascaris lumbricoides* causes **ascariasis**, primarily manifesting as intestinal symptoms, malnutrition, or pulmonary symptoms during larval migration (Löffler syndrome)
- While it can cause eosinophilia, it rarely presents with solid hepatic masses or the specific constellation of symptoms seen here.
*Trichuris trichiura*
- *Trichuris trichiura* causes **trichuriasis** (whipworm infection), primarily leading to **gastrointestinal symptoms** such as abdominal pain, diarrhea, and rectal prolapse in heavy infections.
- It is not associated with migratory visceral larvae, hepatomegaly, or palpable liver masses.
*Toxocara cati*
- While *Toxocara cati* also causes visceral larva migrans, it is associated with **cats** rather than dogs. The patient's history specifically mentions a pet dog.
- The clinical presentation with hepatomegaly, abdominal mass, and eosinophilia would otherwise be consistent with *Toxocara* infection.
More Malaria parasites and life cycle US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.