Leishmania species US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Leishmania species. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
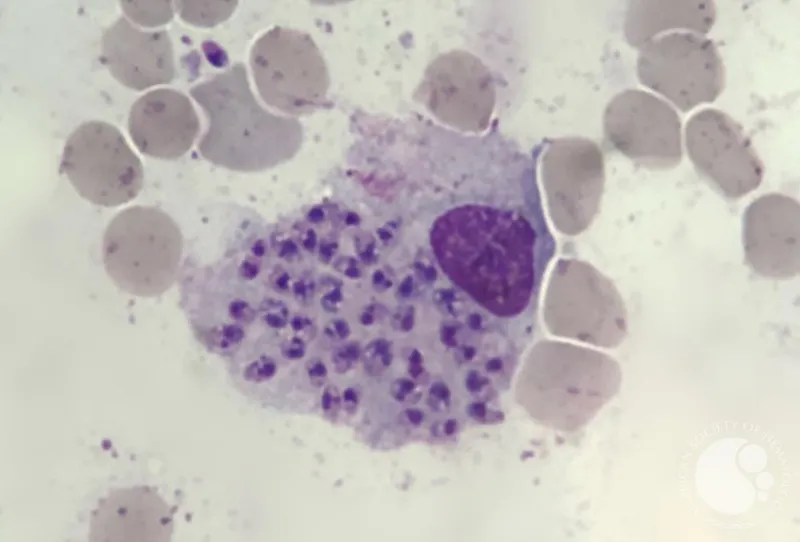
Leishmania species US Medical PG Question 1: A 34-year-old man comes to the physician for a 2-month history of an itchy rash on his forearm. He feels well otherwise and has not had any fever or chills. He returned from an archaeological expedition to Guatemala 4 months ago. Skin examination shows a solitary, round, pink-colored plaque with central ulceration on the right wrist. There is right axillary lymphadenopathy. A photomicrograph of a biopsy specimen from the lesion is shown. Which of the following is the most likely causal organism?
- A. Treponema pallidum
- B. Borrelia burgdorferi
- C. Trypanosoma brucei
- D. Ancylostoma duodenale
- E. Leishmania braziliensis (Correct Answer)
Leishmania species Explanation: ***Leishmania braziliensis***
- The patient's history of travel to **Guatemala**, a region endemic for **cutaneous leishmaniasis**, along with the characteristic skin lesion (**solitary, round, pink plaque with central ulceration**) and **axillary lymphadenopathy**, is highly suggestive of infection with *Leishmania braziliensis*.
- The microscopic image would typically show **amastigotes** within **macrophages**, which are pathognomonic for leishmaniasis.
*Treponema pallidum*
- This bacterium causes **syphilis**, which can present with a **chancre** (painless ulcer) in its primary stage.
- However, the chancre is typically firm, solitary, and non-itchy, and the patient's travel history and specific lesion morphology are more consistent with leishmaniasis.
*Borrelia burgdorferi*
- This spirochete causes **Lyme disease**, characterized by **erythema migrans** (a migrating rash with central clearing) in its early stage.
- The rash seen in this case does not resemble erythema migrans, and regional lymphadenopathy is less prominent compared to leishmaniasis.
*Trypanosoma brucei*
- This protozoan causes **African sleeping sickness**, which is endemic to **sub-Saharan Africa**, not Central America.
- Initial symptoms may include a **trypanosomal chancre** at the bite site, followed by systemic symptoms and neurological involvement, which are not described here.
*Ancylostoma duodenale*
- This is a type of **hookworm** that causes parasitic infection, primarily affecting the **gastrointestinal tract**, leading to **anemia**.
- Skin manifestations are typically **pruritic larvae currens** (creeping eruption) due to larval migration, which is different from the described ulcerated plaque.
Leishmania species US Medical PG Question 2: A 32-year-old woman presents to your office with abdominal pain and bloating over the last month. She also complains of intermittent, copious, non-bloody diarrhea over the same time. Last month, she had a cough that has since improved but has not completely resolved. She has no sick contacts and has not left the country recently. She denies any myalgias, itching, or rashes. Physical and laboratory evaluations are unremarkable. Examination of her stool reveals the causative organism. This organism is most likely transmitted to the human host through which of the following routes?
- A. Insect bite
- B. Penetration of skin (Correct Answer)
- C. Sexual contact
- D. Inhalation
- E. Animal bite
Leishmania species Explanation: ***Penetration of skin***
- The symptoms of **abdominal pain**, **bloating**, **intermittent copious non-bloody diarrhea**, and a recent **cough** are highly suggestive of a **hookworm infection**.
- Hookworm larvae (filariform larvae) primarily penetrate the skin, usually through bare feet, as their mode of entry into the human host.
*Insect bite*
- Although some parasitic infections are transmitted by insect bites (e.g., malaria, Chagas disease), hookworms are not transmitted this way.
- **Insect-borne diseases** typically present with different clinical manifestations or geographical associations.
*Sexual contact*
- **Sexually transmitted infections** involve direct contact of mucous membranes or body fluids during sexual activity.
- Hookworm infection transmission through sexual contact is not a recognized route.
*Inhalation*
- **Inhalation** is a route of transmission for respiratory pathogens (e.g., influenza, tuberculosis) or certain fungal infections, but not for hookworms.
- While hookworm larvae migrate through the lungs, the initial infection pathway is not via inhalation.
*Animal bite*
- **Animal bites** transmit diseases like rabies or certain bacterial infections, but not parasitic hookworms.
- Hookworm infection does not result from direct contact with an animal's saliva or puncture wound.
Leishmania species US Medical PG Question 3: A 48-year-old man comes to the physician because of a hypopigmented skin lesion on his finger. He first noticed it 4 weeks ago after cutting his finger with a knife while preparing food. He did not feel the cut. For the past week, he has also had fever, fatigue, and malaise. He has not traveled outside the country since he immigrated from India to join his family in the United States 2 years ago. His temperature is 38.7°C (101.7°F). Physical examination shows a small, healing laceration on the dorsal aspect of the left index finger and an overlying well-defined, hypopigmented macule with raised borders. Sensation to pinprick and light touch is decreased over this area. Which of the following is the most likely causal pathogen of this patient's condition?
- A. Epidermophyton floccosum
- B. Mycobacterium leprae (Correct Answer)
- C. Malassezia furfur
- D. Pseudomonas aeruginosa
- E. Leishmania donovani
Leishmania species Explanation: ***Mycobacterium leprae***
- The patient's history of immigration from **India**, a country endemic for leprosy, coupled with the **hypopigmented, anesthetic skin lesion** with raised borders, is classic for **leprosy** (Hansen's disease).
- The diminished sensation to pinprick and light touch in the affected area points to **nerve involvement**, a hallmark of *Mycobacterium leprae* infection.
*Epidermophyton floccosum*
- This fungus primarily causes **tinea infections** (ringworm), such as athlete's foot and jock itch.
- While it can cause skin lesions, they are typically **erythematous** and scaly, not hypopigmented with sensory loss.
*Malassezia furfur*
- This yeast is responsible for **tinea versicolor**, characterized by **hypopigmented or hyperpigmented patches** that typically scale.
- However, it does not cause **nerve damage** or accompanying sensory loss, and systemic symptoms like fever and malaise are not typical.
*Pseudomonas aeruginosa*
- This bacterium can cause various opportunistic infections, including skin infections like **ecthyma gangrenosum** or **folliculitis** in immunocompromised patients.
- *Pseudomonas* infections are usually painful, often associated with a characteristic **grape-like odor**, and do not typically present with chronic, anesthetic, hypopigmented lesions.
*Leishmania donovani*
- This parasite causes **visceral leishmaniasis** (kala-azar), which presents with fever, weight loss, hepatosplenomegaly, and **hyperpigmentation of the skin** (darkening), not hypopigmentation.
- It does not cause localized anesthetic skin lesions like those described in the patient.
Leishmania species US Medical PG Question 4: A 28-year-old woman comes to the emergency department for a rash that began 3 days ago. She has low-grade fever and muscle aches. She has no history of serious illness and takes no medications. She has had 5 male sexual partners over the past year and uses condoms inconsistently. Her temperature is 38.1°C (100.6° F), pulse is 85/min, and blood pressure is 126/89 mm Hg. Examination shows a diffuse maculopapular rash that includes the palms and soles. The remainder of the examination shows no abnormalities. A venereal disease research laboratory (VDRL) test is positive. Which of the following is the next appropriate step in management?
- A. Intravenous penicillin G
- B. Dark field microscopy
- C. Treponemal culture
- D. Oral doxycycline
- E. Fluorescent treponemal antibody absorption test (Correct Answer)
Leishmania species Explanation: ***Fluorescent treponemal antibody absorption test***
- A positive **VDRL** (a non-treponemal test) should be confirmed with a **treponemal-specific test** like the **fluorescent treponemal antibody absorption (FTA-ABS)** test or **Treponema pallidum particle agglutination (TPPA)** assay to definitively diagnose syphilis.
- This confirmatory step helps differentiate true syphilis from false-positive VDRL results, which can occur in autoimmune diseases (SLE, antiphospholipid syndrome), other infections (malaria, mononucleosis), pregnancy, or recent vaccination.
- While this patient's presentation is highly suggestive of **secondary syphilis** (diffuse maculopapular rash involving palms and soles, fever, myalgias, positive VDRL), confirmatory testing is the standard next step before initiating treatment.
- Note: In some clinical settings with classic secondary syphilis, immediate treatment may be initiated, but confirmatory testing remains the most appropriate next diagnostic step.
*Intravenous penicillin G*
- IV aqueous penicillin G is the treatment for **neurosyphilis**, not uncomplicated secondary syphilis.
- **Secondary syphilis** is treated with **intramuscular benzathine penicillin G 2.4 million units** as a single dose.
- Treatment should follow confirmed diagnosis with treponemal-specific testing.
*Dark field microscopy*
- This technique visualizes spirochetes directly from **primary lesions** (chancres) or moist secondary lesions (condyloma lata, mucous patches).
- It is not practical for this patient who has a diffuse maculopapular rash without obvious mucosal or genital lesions.
- Dark-field microscopy requires specialized equipment and expertise not readily available in most emergency departments.
*Treponemal culture*
- **Treponema pallidum** cannot be cultured on artificial media because it is an **obligate pathogen** that requires living host cells.
- Culture is not a diagnostic option for syphilis.
*Oral doxycycline*
- **Doxycycline 100 mg twice daily for 14 days** is an alternative treatment for early syphilis in **penicillin-allergic patients**.
- Treatment should only be initiated after diagnosis is confirmed with treponemal-specific testing.
- This is not the next appropriate step; confirmatory testing comes first.
Leishmania species US Medical PG Question 5: During a humanitarian medical mission in rural Vietnam, a medical resident encounters a 50-year-old man with a year-long history of a pruritic rash on his upper body and face, along with numbness and tingling sensation of both of his palms. He mostly works on his family’s rice farm, where he also takes care of livestock. A physical examination revealed multiple erythematous macules and papules on the face, arms, chest, and back, as well as thinning of the eyebrows and loss of some eyelashes. Additional findings include hypopigmented macules around the elbows, which are insensitive to light touch, temperature, and pinprick. The grip strength is slightly diminished bilaterally with the conservation of both bicipital reflexes. What is the most likely diagnosis?
- A. Leprosy (Correct Answer)
- B. Sporotrichosis
- C. Tinea corporis
- D. Scrofula
- E. Cutaneous leishmaniasis
Leishmania species Explanation: ***Leprosy***
- The combination of a **chronic pruritic rash**, **sensory loss** (numbness, tingling, insensitivity to touch/temperature/pinprick) in hypopigmented macules, **thinning eyebrows**, and **loss of eyelashes (madarosis)** points strongly to leprosy.
- The patient's long-term exposure in a rural, livestock-intensive environment in Vietnam is consistent with areas where **leprosy (Hansen's disease)** is endemic.
- **Peripheral neuropathy** with motor involvement (diminished grip strength) and preserved reflexes is characteristic.
*Sporotrichosis*
- Typically presents as **subcutaneous nodules** or ulcers, often in a **lymphocutaneous pattern**, following a puncture wound.
- While it can occur in agricultural workers, it doesn't usually cause widespread pruritic macules/papules, nerve involvement, or loss of eyebrows/eyelashes.
*Tinea corporis*
- Characterized by **annular, scaly, erythematous patches** with central clearing, often itchy.
- It does not cause sensory deficits, thinning of eyebrows/eyelashes, or hypopigmented, anesthetic lesions.
*Scrofula*
- This refers to **tuberculosis lymphadenitis**, primarily affecting the cervical lymph nodes, causing chronic swelling and sometimes draining sinuses.
- It does not present with a widespread pruritic rash, sensory neuropathy, or characteristic skin lesions like those described in the patient.
*Cutaneous leishmaniasis*
- Causes persistent **skin lesions (papules, nodules, ulcers)**, often with a raised border, typically following a bite from a sandfly.
- While it can be chronic and occur in endemic areas, it generally does not cause sensory nerve damage, eyebrow/eyelash loss, or widespread hypopigmented anesthetic macules.
Leishmania species US Medical PG Question 6: An investigator is studying human genetics and cell division. A molecule is used to inhibit the exchange of genetic material between homologous chromosomes. Which of the following phases of the cell cycle does the molecule target?
- A. Prophase II
- B. Prophase I (Correct Answer)
- C. Metaphase II
- D. Telophase I
- E. Anaphase I
Leishmania species Explanation: ***Prophase I***
- **Crossing over** (genetic recombination) occurs specifically during **Prophase I** of meiosis, particularly during the pachytene stage
- During this phase, homologous chromosomes pair up (synapsis) and exchange genetic material through recombination
- Inhibiting this exchange means targeting the phase where this critical genetic recombination takes place
*Prophase II*
- Prophase II is a stage in meiosis II where chromosomes condense again after a brief interkinesis
- **Crossing over does not occur** in Prophase II - genetic recombination has already been completed in Prophase I
- Homologous chromosomes are no longer paired at this stage
*Metaphase II*
- During Metaphase II, individual chromosomes (not homologous pairs) align along the metaphase plate
- There is **no exchange of genetic material** between homologous chromosomes at this stage
- This phase prepares for the separation of sister chromatids
*Telophase I*
- Telophase I involves decondensation of chromosomes and reformation of nuclear envelopes around the separated homologous chromosomes
- This marks the end of meiosis I, **after** genetic exchange has already occurred in Prophase I
- No crossing over occurs during this phase
*Anaphase I*
- In Anaphase I, **homologous chromosomes separate** and move to opposite poles of the cell
- This phase is characterized by segregation of chromosomes, **not genetic exchange**
- Crossing over has already been completed by this stage
Leishmania species US Medical PG Question 7: A 54-year-old gardener with diabetes mellitus from the Northeast Jilin Province in China acquired a small scratch from a thorn while working in his flower garden. After 3 weeks, he noticed a small pink, painless bump at the site of a scratch. He was not concerned by the bump; however, additional linearly-distributed bumps that resembled boils began to appear 1 week later that were quite painful. When the changes took on the appearance of open sores that drained clear fluid without any evidence of healing (as shown on the image), he finally visited his physician. The physician referred to the gardener for a skin biopsy to confirm his working diagnosis and to start treatment as soon as possible. Which of the following is the most likely diagnosis for this patient?
- A. Cat scratch disease
- B. Leishmaniasis
- C. Sporotrichosis (Correct Answer)
- D. Paracoccidioidomycosis
- E. Blastomycosis
Leishmania species Explanation: ***Sporotrichosis***
- The patient's history of a **thorn scratch** in a garden, followed by a **painless pink bump** that progressed to **linearly-distributed painful nodules** resembling boils and eventually **non-healing ulcers** with clear fluid drainage, is highly characteristic of **sporotrichosis** (also known as "rose gardener's disease"). This pattern is called **lymphocutaneous sporotrichosis**.
- **Sporotrichosis** is caused by the fungus *Sporothrix schenckii*, which is commonly found in soil and on plants, explaining the gardener's exposure.
*Cat scratch disease*
- This disease is caused by *Bartonella henselae* and is typically transmitted by the scratch or bite of a cat, not a thorn.
- It usually presents with a papule or pustule at the inoculum site followed by **lymphadenopathy** in the regional lymph nodes, which is distinct from the linear spread observed here.
*Leishmaniasis*
- Leishmaniasis is a parasitic disease transmitted by the bite of infected **sandflies**.
- While it can cause skin lesions ranging from papules to ulcers, the mode of transmission and the characteristic linear spread of nodules following a thorn injury do not fit this diagnosis.
*Paracoccidioidomycosis*
- This is a systemic fungal infection endemic to Central and South America, not typically seen in China's Jillin Province.
- It primarily affects the lungs, skin, and mucous membranes, with skin lesions often appearing as chronic, progressive ulcers but without the specific linear nodular pattern described.
*Blastomycosis*
- **Blastomycosis** is a fungal infection typically acquired by inhaling spores, primarily affecting the lungs, but it can disseminate to the skin, bones, and other organs.
- Cutaneous lesions are usually sharply demarcated, crusted plaques or verrucous lesions, but they do not typically present with the linear, nodular, and ulcerative progression seen in this case.
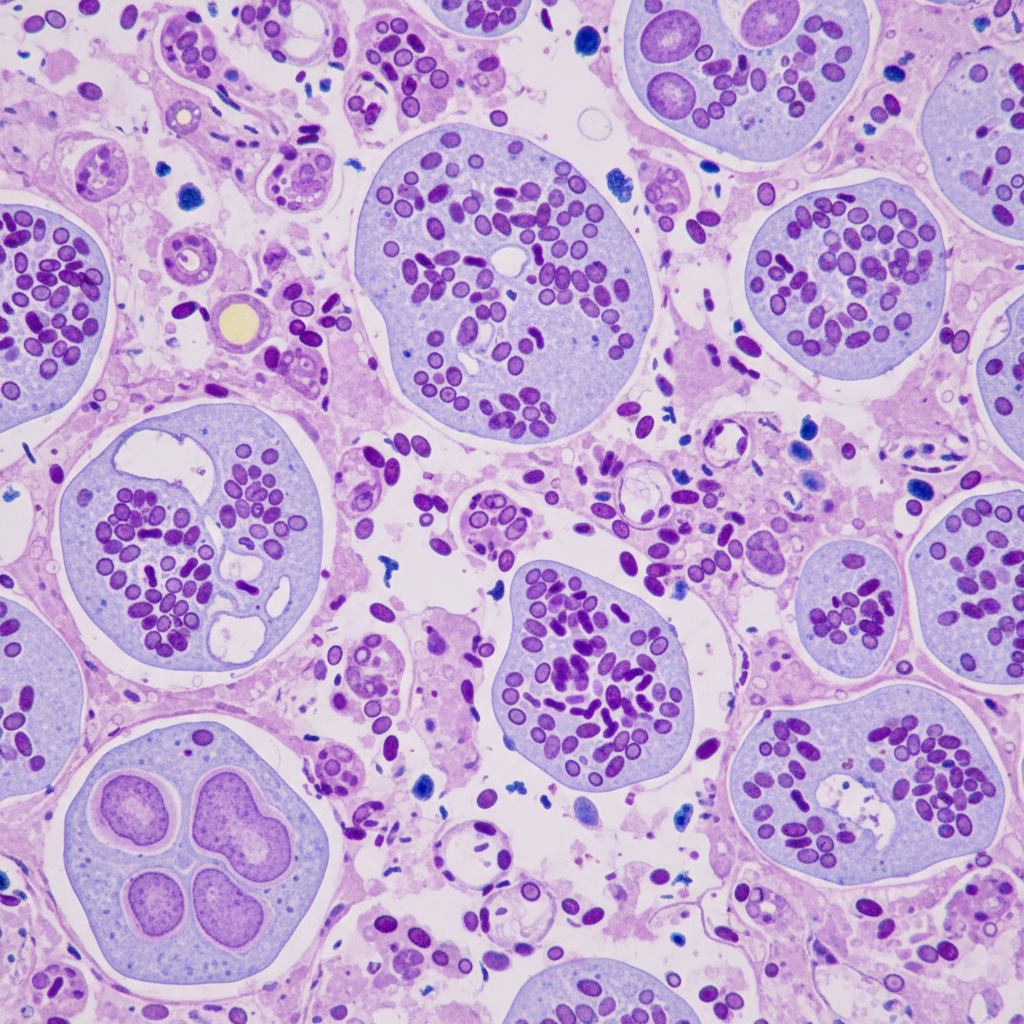
Leishmania species US Medical PG Question 8: A 47-year-old woman comes to the physician because of a 3-day history of fever, fatigue, loss of appetite, cough, and chest pain. Physical examination shows diffuse inspiratory crackles over the left lung field. An x-ray of the chest shows hilar lymphadenopathy and well-defined nodules with central calcifications. Urine studies show the presence of a polysaccharide antigen. A biopsy specimen of the lung shows cells with basophilic, crescent-shaped nuclei and pericellular halos located within macrophages. This patient's history is most likely to show which of the following?
- A. Visit to Arizona desert
- B. Recent trip to Brazil
- C. Previous mycobacterial infection
- D. Exposure to bat droppings (Correct Answer)
- E. Treatment with inhaled glucocorticoids
Leishmania species Explanation: ***Exposure to bat droppings***
- The clinical presentation, including fever, cough, chest pain, **hilar lymphadenopathy**, **nodules with central calcifications**, and **intracellular encapsulated yeasts** in macrophages, is classic for **histoplasmosis**.
- **Histoplasma capsulatum** is endemic to the Ohio and Mississippi River valleys and is transmitted through inhalation of spores from soil contaminated with **bat or bird droppings**.
*Visit to Arizona desert*
- Exposure in the **Arizona desert** is associated with **coccidioidomycosis** (Valley Fever), which presents with similar pulmonary symptoms but is caused by Coccidioides immitis/posadasii, characterized by **spherules** containing endospores.
- While it can cause hilar lymphadenopathy and nodules, the characteristic intracellular budding yeasts within macrophages and the polysaccharide antigen in urine point away from coccidioidomycosis.
*Recent trip to Brazil*
- A trip to **Brazil** might suggest diseases like **Paracoccidioidomycosis**, which presents with chronic mucocutaneous or disseminated lesions, or various tropical infections, but is not typically characterized by the specific pulmonary and microscopic findings described here.
- The histopathological findings of **intracellular yeasts with pericellular halos** (consistent with Histoplasma) would not be the primary finding for paracoccidioidomycosis, which generally shows characteristic **"pilot wheel"** or multiple budding yeasts.
*Previous mycobacterial infection*
- A previous **mycobacterial infection** would lead to tuberculosis, characterized by **acid-fast bacilli** and granulomas with **caseating necrosis**, which is different from the described intracellular yeasts and polysaccharide antigen.
- While tuberculosis can cause hilar lymphadenopathy and pulmonary nodules, the given microscopic description of cells with basophilic nuclei and pericellular halos within macrophages does not fit Mycobacterium tuberculosis.
*Treatment with inhaled glucocorticoids*
- Inhaled glucocorticoids are used to treat conditions like asthma or COPD and, while prolonged use can rarely predispose to **opportunistic fungal infections** (e.g., aspergillosis, candidiasis), they are not a cause of this specific clinical presentation or the microbiological findings of histoplasmosis.
- The use of inhaled steroids would not explain the geographic exposure, hilar lymphadenopathy, or the specific appearance of the fungal elements within macrophages described.
Leishmania species US Medical PG Question 9: A 30-year-old woman who is 24-weeks pregnant presents to the emergency department with fever, painful urination, and headache. The patient's blood pressure is 111/67 mm Hg, the pulse is 95/min, the respiratory rate is 16/min, and the temperature is 38.3°C (101.1°F). Physical examination reveals bilateral tender inguinal lymphadenopathy and painful genital lesions. On closer inspection, the patient’s genital lesions contain clear fluid and measure 5–6 mm in diameter. What is the appropriate description of these lesions?
- A. Pustule
- B. Ulcer
- C. Papule
- D. Bulla
- E. Vesicle (Correct Answer)
Leishmania species Explanation: ***Vesicle***
- A **vesicle** is defined as a **circumscribed, elevated lesion** (macule/papule) containing **clear fluid** and measuring less than 1 cm in diameter.
- The patient's lesions, which are 5-6 mm in diameter and contain clear fluid, perfectly fit the description of vesicles, characteristic of **herpes simplex virus (HSV)** infection.
*Pustule*
- A **pustule** is a small, elevated lesion similar to a vesicle but filled with **pus**, not clear fluid.
- Examples include acne or folliculitis, which are typically opaque and yellowish, unlike the described lesions.
*Ulcer*
- An **ulcer** is a defect or excavation of the skin past the **epidermis**, resulting in the loss of tissue.
- The patient's lesions are described as fluid-filled and elevated, not as an open wound with tissue loss.
*Papule*
- A **papule** is a **solid, elevated lesion** measuring less than 1 cm in diameter.
- While elevated and small, a papule does **not contain fluid**, which is a key characteristic of the described lesions.
*Bulla*
- A **bulla** is a **fluid-filled lesion** that is **larger than 1 cm** in diameter.
- The lesions described are 5-6 mm, making them smaller than the definition of a bulla.
Leishmania species US Medical PG Question 10: A 24-year-old female comes to the physician because of flu-like symptoms and a new rash for 2 days. She denies contacts with sick individuals or recent travel abroad, but recently went camping in Vermont. Vital signs are within normal limits. Examination of the lateral right thigh shows a circular red ring with central clearing. Which of the following is the natural reservoir of the pathogen responsible for this patient's symptoms?
- A. Rat
- B. Rabbit
- C. Tick
- D. Mouse (Correct Answer)
- E. Flea
Leishmania species Explanation: ***Mouse***
- The patient's symptoms, including **flu-like illness** and a **circular red rash with central clearing** (erythema migrans) after camping in Vermont, are classic for **Lyme disease**.
- The causative agent, *Borrelia burgdorferi*, is primarily maintained in **white-footed mice** (genus *Peromyscus*) in its natural reservoir during its larval and nymphal stages.
*Rat*
- While **rats** can carry and transmit various diseases, they are not the primary natural reservoir for *Borrelia burgdorferi*, the pathogen responsible for Lyme disease.
- Diseases associated with rats often include **leptospirosis** and **plague**, which present with different clinical pictures.
*Rabbit*
- **Rabbits** are known reservoirs for diseases like **tularemia** (*Francisella tularensis*), which can cause fever, skin lesions, and lymphadenopathy, but typically not the characteristic **erythema migrans** rash.
- They are not a significant natural reservoir for *Borrelia burgdorferi*.
*Tick*
- The **tick** (specifically *Ixodes scapularis* or **deer tick**) is the **vector** that transmits *Borrelia burgdorferi* to humans, not the natural reservoir.
- The tick acquires the bacteria from infected animal hosts such as mice and deer.
*Flea*
- **Fleas** are vectors for diseases such as **bubonic plague** (*Yersinia pestis*) and **endemic typhus** (*Rickettsia typhi*), which do not manifest with erythema migrans.
- They are not involved in the transmission or natural history of **Lyme disease**.
More Leishmania species US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.