Blood and tissue parasites US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Blood and tissue parasites. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Blood and tissue parasites US Medical PG Question 1: A 42-year-old woman comes to the physician because of episodic abdominal pain and fullness for 1 month. She works as an assistant at an animal shelter and helps to feed and bathe the animals. Physical examination shows hepatomegaly. Abdominal ultrasound shows a 4-cm calcified cyst with several daughter cysts in the liver. She undergoes CT-guided percutaneous aspiration under general anesthesia. Several minutes into the procedure, one liver cyst spills, and the patient's oxygen saturation decreases from 95% to 64%. Her pulse is 136/min, and blood pressure is 86/58 mm Hg. Which of the following is the most likely causal organism of this patient's condition?
- A. Clonorchis sinensis
- B. Trichinella spiralis
- C. Echinococcus granulosus (Correct Answer)
- D. Strongyloides stercoralis
- E. Schistosoma mansoni
Blood and tissue parasites Explanation: ***Echinococcus granulosus***
- The presentation of a **calcified liver cyst** with **daughter cysts** in a patient with animal exposure (**animal shelter worker**) is highly suggestive of **hydatid disease** caused by *Echinococcus granulosus*.
- The **anaphylactic-like reaction** (decreased oxygen saturation, hypotension, tachycardia) upon cyst spillage during aspiration is a classic and dangerous complication, indicating a severe allergic response to the **hydatid fluid**.
*Clonorchis sinensis*
- This parasite causes **cholangitis** and **cholangiocarcinoma**, and typically presents with symptoms related to biliary obstruction, rather than large calcified cysts with daughter cysts.
- It is acquired by eating **undercooked freshwater fish** and is endemic in East Asia, which doesn't align with the patient's exposure history or cyst morphology.
*Trichinella spiralis*
- This parasite is acquired by consuming **undercooked pork** and causes **trichinosis**, characterized by muscle pain, periorbital edema, and eosinophilia, and does not typically form liver cysts.
- Liver involvement with *Trichinella* is rare and does not manifest as calcified cysts with daughter cysts.
*Strongyloides stercoralis*
- This nematode causes **strongyloidiasis**, often manifesting as gastrointestinal symptoms, skin rash (**larva currens**), and pulmonary symptoms in cases of autoinfection.
- It does not form macroscopic liver cysts, and liver involvement is generally non-cystic.
*Schistosoma mansoni*
- Causes **schistosomiasis**, which can lead to **hepatic fibrosis** (**pipestem fibrosis**) and **portal hypertension**, but does not typically cause large, calcified hydatid-like cysts with daughter cysts.
- Infection is acquired through contact with **freshwater contaminated with snails** carrying the parasitic larvae.
Blood and tissue parasites US Medical PG Question 2: A 30-year-old forest landscape specialist is brought to the emergency department with hematemesis and confusion. One week ago, she was diagnosed with influenza when she had fevers, severe headaches, myalgias, hip and shoulder pain, and a maculopapular rash. After a day of relative remission, she developed abdominal pain, vomiting, and diarrhea. A single episode of hematemesis occurred prior to admission. Two weeks ago she visited rainforests and caves in western Africa where she had direct contact with animals, including apes. She has no history of serious illnesses or use of medications. She is restless and her temperature is 38.0°C (100.4°F); pulse, 95/min; respirations, 20/min; and supine and upright blood pressure, 130/70 mm Hg and 100/65 mm Hg, respectively. Conjunctival suffusion is seen. Ecchymoses are observed on the lower extremities. She is bleeding from one of her intravenous lines. The peripheral blood smear is negative for organisms. The laboratory studies show the following:
Hemoglobin 10 g/dL
Leukocyte count 1,000/mm3
Segmented neutrophils 65%
Lymphocytes 20%
Platelet count 50,000/mm3
Partial thromboplastin time (activated) 60 seconds
Prothrombin time 25 seconds
Fibrin split products positive
Serum
Alanine aminotransferase (ALT) 85 U/L
Aspartate aminotransferase (AST) 120 U/L
γ-Glutamyltransferase (GGT) 83 U/L (N = 5–50 U/L)
Creatinine 2 mg/dL
Which of the following is the most likely causal pathogen?
- A. Zika virus
- B. Plasmodium falciparum
- C. Yersinia pestis
- D. Babesia microti
- E. Ebola virus (Correct Answer)
Blood and tissue parasites Explanation: ***Ebola virus***
- The patient's presentation with **fever, myalgias, headache, maculopapular rash, gastrointestinal symptoms (vomiting, diarrhea, hematemesis), confusion, bleeding diathesis (ecchymoses, IV site bleeding, prolonged PT/aPTT, positive fibrin split products)**, and recent travel to **rainforests and caves in western Africa with ape contact** is highly consistent with Ebola virus disease.
- Laboratory findings of **leukopenia, thrombocytopenia, elevated liver enzymes (ALT, AST, GGT), and acute kidney injury (creatinine 2 mg/dL)** further support this diagnosis, as Ebola can cause widespread organ damage and disseminated intravascular coagulation (DIC).
*Zika virus*
- While Zika can cause **fever, rash, and arthralgia**, it typically presents as a milder illness and does not characteristically lead to severe **hemorrhagic manifestations, confusion, or significant organ dysfunction** like the patient's presentation.
- The patient's severe gastrointestinal symptoms, profound coagulopathy, and significant organ involvement are not typical features of Zika virus infection.
*Plasmodium falciparum*
- **Malaria** caused by *Plasmodium falciparum* can lead to **fever, headache, myalgias, and confusion**, and severe malaria can cause **anemia and thrombocytopenia**.
- However, the prominent **maculopapular rash, severe hemorrhagic diathesis with multi-site bleeding, prolonged PT/aPTT, and significant leukopenia** are not characteristic features of *P. falciparum* malaria, and the peripheral blood smear was negative for organisms.
*Yersinia pestis*
- **Bubonic plague** (caused by *Yersinia pestis*) can cause **fever, headache, and severe illness**, often with characteristic **lymphadenopathy (buboes)**, and can progress to pneumonic or septicemic forms.
- The absence of prominent buboes and the specific constellation of hemorrhagic fever symptoms, rash, and liver/kidney involvement point away from *Yersinia pestis* and more towards a viral hemorrhagic fever.
*Babesia microti*
- **Babesiosis** is a tick-borne illness causing **fever, fatigue, myalgias, and hemolytic anemia**, primarily seen in immunocompromised individuals or those with splenectomy, and does not typically involve **maculopapular rash, severe hemorrhagic phenomena, or significant leukopenia**.
- While it can cause some anemia and thrombocytopenia, the overall clinical picture, especially the prominent bleeding and multi-organ failure, is inconsistent with babesiosis.
Blood and tissue parasites US Medical PG Question 3: A 28-year-old female in the 2nd trimester of pregnancy is diagnosed with primary Toxoplasma gondii infection. Her physician fears that the fetus may be infected in utero. Which of the following are associated with T. gondii infection in neonates?
- A. Hutchinson’s teeth, saddle nose, short maxilla
- B. Deafness, seizures, petechial rash
- C. Hydrocephalus, chorioretinitis, intracranial calcifications (Correct Answer)
- D. Patent ductus arteriosus, cataracts, deafness
- E. Temporal encephalitis, vesicular lesions
Blood and tissue parasites Explanation: ***Hydrocephalus, chorioretinitis, intracranial calcifications***
- These are the classic triad of symptoms (known as the **Sabin triad**) often associated with **congenital toxoplasmosis**.
- **Hydrocephalus** results from obstruction of cerebrospinal fluid flow, **chorioretinitis** can lead to vision loss, and **intracranial calcifications** are a hallmark of the infection's impact on the brain.
*Hutchinson’s teeth, saddle nose, short maxilla*
- These are characteristic features of **congenital syphilis**, not *Toxoplasma gondii* infection.
- **Hutchinson's triad** includes Hutchinson's teeth, interstitial keratitis, and sensorineural hearing loss in congenital syphilis.
*Deafness, seizures, petechial rash*
- While seizures can occur with severe congenital infections, this combination is more suggestive of **cytomegalovirus (CMV)** infection or **rubella**, which can cause petechial rash (blueberry muffin baby) and profound sensorineural deafness.
- *Toxoplasma gondii* does not typically cause a petechial rash as a primary symptom.
*Patent ductus arteriosus, cataracts, deafness*
- This constellation of symptoms is highly characteristic of **congenital rubella syndrome**.
- **Cardiac defects** (like patent ductus arteriosus), **ocular abnormalities** (cataracts), and **sensorineural deafness** are classical signs of rubella.
*Temporal encephalitis, vesicular lesions*
- **Temporal encephalitis** with vesicular lesions, particularly in a neonatal context, is a classic presentation of **congenital herpes simplex virus (HSV) infection**.
- *Toxoplasma gondii* can cause encephalitis, but not typically with vesicular lesions or a primary predilection for the temporal lobe in this specific clinical presentation.
Blood and tissue parasites US Medical PG Question 4: A 78-year-old woman living in New Jersey is brought to the emergency department in July with a fever for 5 days. Lethargy is present. She has had bloody urine over the last 48 hours but denies any nausea, vomiting, or abdominal pain. She has no history of serious illness and takes no medications. She has not traveled anywhere outside her city for the past several years. She appears ill. The temperature is 40.8℃ (105.4℉), the pulse is 108/min, the respiration rate is 20/min, and the blood pressure is 105/50 mm Hg. The abdominal exam reveals hepatosplenomegaly. Lymphadenopathy is absent. Petechiae are seen on the lower extremities. Laboratory studies show the following:
Laboratory test
Hemoglobin 8 g/dL
Mean corpuscular volume (MCV) 98 µm3
Leukocyte count 4,200/mm3
Segmented neutrophils 32%
Lymphocytes 58%
Platelet count 108,000/mm3
Bilirubin, total 5.0 mg/dL
Direct 0.7 mg/dL
Aspartate aminotransferase (AST) 51 U/L
Alanine aminotransferase (ALT) 56 U/L
Alkaline phosphatase 180 U/L
Lactate dehydrogenase (LDH) 640 U/L (N = 140–280 U/L)
Haptoglobin 20 mg/dL (N = 30–200 mg/dL)
Urine
Hemoglobin +
Urobilinogen +
Protein +
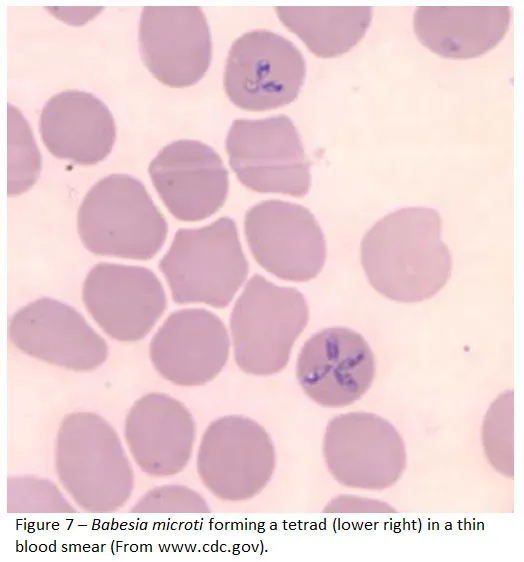
A peripheral blood smear is shown (see image). Which of the following is the most likely diagnosis?
- A. Babesiosis (Correct Answer)
- B. Leishmaniasis
- C. Lyme disease
- D. Malaria
- E. Plague
Blood and tissue parasites Explanation: ***Babesiosis***
- The patient's presentation with **fever, lethargy, hemolytic anemia** (low hemoglobin, elevated LDH, low haptoglobin, bilirubinemia, hemoglobinuria), **thrombocytopenia**, and **hepatosplenomegaly** is highly suggestive of babesiosis. The **peripheral blood smear showing intraerythrocytic parasites** (often described as ring forms or tetrads, "Maltese cross") is diagnostic. Living in **New Jersey** in **July** increases the likelihood of tick exposure, which transmits *Babesia microti*.
- Her age (78 years old) is a risk factor for severe babesiosis, and the **anemia and thrombocytopenia** are classic findings, with the elevated total bilirubin indicating significant hemolysis.
*Leishmaniasis*
- While leishmaniasis (specifically visceral leishmaniasis) can cause fever, hepatosplenomegaly, anemia, and thrombocytopenia, it is endemic to different regions (e.g., Mediterranean basin, South America, Asia, Africa) and is **not typically acquired in New Jersey**.
- Diagnosis is usually made by identifying **amastigotes in bone marrow, spleen, or lymph node aspirates**, not intraerythrocytic parasites on a peripheral smear.
*Lyme disease*
- Lyme disease, also transmitted by *Ixodes* ticks in New Jersey, typically presents with an **erythema chronicum migrans rash**, flu-like symptoms, and can lead to arthritis or cardiac/neurological manifestations.
- It **does not cause intraerythrocytic parasites or severe hemolytic anemia** with the lab findings described (elevated LDH, low haptoglobin, bilirubinemia, hemoglobinuria).
*Malaria*
- Malaria presents with fever, chills, anemia, and hepatosplenomegaly and is diagnosed by **intraerythrocytic parasites on a peripheral blood smear**. However, the patient has **not traveled to malaria-endemic regions** and has remained in her city for several years.
- While both *Babesia* and *Plasmodium* can appear as ring forms, the specific morphology (e.g., "Maltese cross" in *Babesia*) and geographic context strongly favor babesiosis in this case.
*Plague*
- Plague (caused by *Yersinia pestis*) typically presents as bubonic, septicemic, or pneumonic forms. **Bubonic plague** involves painful, swollen lymph nodes (buboes), which are absent in this patient.
- Although it can cause fever and systemic illness, it does not lead to **intraerythrocytic parasites or significant hemolytic anemia** as seen in this patient's lab results.
Blood and tissue parasites US Medical PG Question 5: A 50-year-old HIV-positive male presents to the ER with a two-day history of fever and hemoptysis. Chest radiograph shows a fibrocavitary lesion in the right middle lobe. Biopsy of the afflicted area demonstrates septate hyphae that branch at acute angles. Which of the following is the most likely causal organism?
- A. Mycobacterium tuberculosis
- B. Pneumocystis jirovecii
- C. Aspergillus fumigatus (Correct Answer)
- D. Candida albicans
- E. Mucor species
Blood and tissue parasites Explanation: ***Aspergillus fumigatus***
- The combination of **fever**, **hemoptysis**, a **fibrocavitary lesion** in an **HIV-positive** patient, and the presence of **septate hyphae branching at acute angles** on biopsy are classic findings for invasive **aspergillosis**.
- **Aspergillus** specifically targets individuals with compromised immune systems, and the pathological description of the hyphae is highly characteristic of this fungus.
*Mycobacterium tuberculosis*
- While **Mycobacterium tuberculosis** can cause **fever**, **hemoptysis**, and **cavitary lesions** in HIV-positive patients, the microscopic description of **septate hyphae branching at acute angles** is not consistent with bacterial infection.
- Tuberculosis is characterized by **acid-fast bacilli** and granulomatous inflammation, not fungal hyphae.
*Mucor species*
- **Mucor** (along with Rhizopus) causes **mucormycosis**, an invasive fungal infection that can affect immunocompromised patients and present with pulmonary involvement and cavitary lesions.
- However, mucormycosis is characterized by **non-septate (aseptate) hyphae branching at right (90-degree) angles**, not septate hyphae at acute angles, making it distinguishable from Aspergillus.
*Pneumocystis jirovecii*
- **Pneumocystis jirovecii** is a common cause of pneumonia in HIV-positive patients, typically presenting as **diffuse interstitial infiltrates** rather than cavitary lesions.
- Microscopic examination would reveal **cysts** and **trophozoites**, not septate hyphae, making it inconsistent with the biopsy findings.
*Candida albicans*
- While **Candida albicans** can cause infections in immunocompromised individuals, it typically presents as **oral thrush**, esophagitis, or disseminated candidiasis.
- Pulmonary involvement is less common and usually manifests as **pneumonitis** rather than cavitary lesions, and its hyphae are typically **pseudohyphae** or budding yeasts, not septate hyphae branching at acute angles.
Blood and tissue parasites US Medical PG Question 6: A 31-year-old male traveler in Thailand experiences fever, headache, and excessive sweating every 48 hours. Peripheral blood smear shows trophozoites and schizonts indicative of Plasmodia infection. The patient is given chloroquine and primaquine. Primaquine targets which of the following Plasmodia forms:
- A. Schizont
- B. Hypnozoite (Correct Answer)
- C. Trophozoite
- D. Merozoite
- E. Sporozoite
Blood and tissue parasites Explanation: ***Hypnozoite***
- **Primaquine** is a **radical cure** for malaria caused by *Plasmodium vivax* and *Plasmodium ovale* because it targets the dormant **hypnozoite** forms in the liver.
- The presence of **hypnozoites** leads to relapses, as they can reactivate and re-initiate the erythrocytic cycle.
*Schizont*
- **Schizonts** are merozoite-producing forms in red blood cells (**erythrocytic schizonts**) or liver cells (**hepatic schizonts**).
- While chloroquine targets **erythrocytic schizonts**, primaquine's primary unique action is against the dormant liver stages.
*Trophozoite*
- **Trophozoites** are the feeding and growing stages of the parasite within red blood cells, which mature into schizonts.
- **Chloroquine** is highly effective against **erythrocytic trophozoites** and schizonts, resolving acute malarial symptoms.
*Merozoite*
- **Merozoites** are released from ruptured schizonts and infect new red blood cells during the erythrocytic cycle.
- No specific antimalarial drug solely targets **merozoites** as a primary form; they are an infective stage for red blood cells.
*Sporozoite*
- **Sporozoites** are the forms injected by infected mosquitoes, which then travel to the liver and infect hepatocytes.
- While some drugs like atovaquone have activity against sporozoites, primaquine is specifically indicated for destroying the **hypnozoite** stage, preventing relapses.
Blood and tissue parasites US Medical PG Question 7: A 27-year-old female presents to her primary care physician because she is concerned about lighter colored patches on her skin. She recently went sunbathing and noticed that these areas also did not tan. Her doctor explains that she has a fungal infection of the skin that damages melanocytes by producing acids. She is prescribed selenium sulfide and told to follow-up in one month. Which of the following describes the appearance of the most likely infectious organism under microscopy?
- A. Broad based budding yeast
- B. "Captain's wheel" yeast
- C. Germ tube forming fungus
- D. Branching septate hyphae
- E. "Spaghetti and meatballs" fungus (Correct Answer)
Blood and tissue parasites Explanation: ***"Spaghetti and meatballs" fungus***
- The "spaghetti and meatballs" appearance on microscopy, referring to a mixture of short, septate hyphae and spherical yeast forms, is characteristic of **Malassezia globosa** or other *Malassezia* species, which cause **tinea versicolor**.
- **Tinea versicolor** presents as hypopigmented patches, especially after sun exposure, because the fungus produces **azelaic acid** that inhibits melanin synthesis.
*Broad based budding yeast*
- This description is characteristic of **Blastomyces dermatitidis**, which causes **blastomycosis**, a deep fungal infection.
- Blastomycosis typically manifests as pulmonary disease or disseminated lesions, not superficial hypopigmented skin patches.
*"Captain's wheel" yeast*
- The "captain's wheel" or multi-budding yeast appearance is characteristic of **Paracoccidioides brasiliensis**, the causative agent of **paracoccidioidomycosis**.
- This is a systemic mycosis primarily affecting the lungs and mucocutaneous areas, not a superficial skin infection like tinea versicolor.
*Germ tube forming fungus*
- The formation of **germ tubes** when incubated in serum at 37°C is a characteristic feature used to identify **Candida albicans**.
- *Candida* most commonly causes mucocutaneous candidiasis (e.g., thrush, vaginitis) or invasive infections, not hypopigmented skin patches that fail to tan.
*Branching septate hyphae*
- **Branching septate hyphae** are a general microscopic feature seen in many filamentous fungi, including dermatophytes like *Trichophyton* and *Microsporum*, which cause **tinea corporis** or **tinea pedis**.
- While dermatophytes cause skin infections, they typically result in erythematous, scaly, and often pruritic lesions and do not usually present as hypopigmented patches that fail to tan due to melanin inhibition, as seen in tinea versicolor.
Blood and tissue parasites US Medical PG Question 8: A 45-year-old man presents to the emergency department with abdominal distension. The patient states he has had gradually worsening abdominal distension with undulating pain, nausea, and vomiting for the past several months. The patient does not see a physician typically and has no known past medical history. He works as a farmer and interacts with livestock and also breeds dogs. His temperature is 98.7°F (37.1°C), blood pressure is 159/90 mmHg, pulse is 88/min, respirations are 15/min, and oxygen saturation is 99% on room air. Physical exam is notable for mild abdominal distension and discomfort to palpation of the upper abdominal quadrants. Laboratory values are ordered and are notable for a mild eosinophilia. A CT scan of the abdomen demonstrates multiple small eggshell calcifications within the right lobe of the liver. Which of the following is the most likely etiology of this patient's symptoms?
- A. Echinococcus granulosus (Correct Answer)
- B. Enterobius vermicularis
- C. Necator americanus
- D. Taenia solium
- E. Taenia saginata
Blood and tissue parasites Explanation: ***Echinococcus granulosus***
- The patient's history of working with **livestock** and dogs, combined with **abdominal pain**, **eosinophilia**, and characteristic **eggshell calcifications** in the liver on CT, is highly suggestive of **hydatid disease** caused by *Echinococcus granulosus*.
- This parasite's larval stage forms **hydatid cysts** primarily affecting the liver and lungs, which can grow slowly and cause symptoms as they expand.
*Enterobius vermicularis*
- This parasite causes **pinworm infection**, primarily manifesting as **perianal itching**, especially at night.
- It does not typically cause abdominal distension, liver cysts, or eosinophilia to this extent, and is diagnosed via the **scotch tape test**.
*Necator americanus*
- This is a type of **hookworm** that primarily causes **iron deficiency anemia** due to chronic blood loss in the GI tract.
- Symptoms include fatigue, weakness, and pallor, but not liver cysts with eggshell calcifications or significant abdominal distension as described.
*Taenia solium*
- **Pork tapeworm** infection can cause **cysticercosis** if humans ingest the eggs, leading to cysts in muscles, subcutaneous tissue, and the brain (neurocysticercosis).
- While it can cause cysts, the classic "eggshell calcifications" in the liver are not typical for *Taenia solium* infection, and the symptoms described fit *Echinococcus* better.
*Taenia saginata*
- This is the **beef tapeworm**, which causes relatively mild symptoms in humans, often limited to mild abdominal discomfort or passage of proglottids in stool.
- It does not cause tissue cysts like those seen in cysticercosis from *T. solium* or hydatid cysts from *Echinococcus*.
Blood and tissue parasites US Medical PG Question 9: A 26-year-old male with no significant past medical history goes camping with several friends in Virginia. Several days after returning, he begins to experience fevers, headaches, myalgias, and malaise. He also notices a rash on his wrists and ankles (Figure A). Which of following should be initiated for treatment of his condition?
- A. Azithromycin
- B. Doxycycline (Correct Answer)
- C. Pyrazinamide
- D. Vancomycin
- E. Praziquantel
Blood and tissue parasites Explanation: ***Doxycycline***
- The patient's symptoms (fever, headache, myalgias, rash on wrists and ankles after camping in Virginia) are highly suggestive of **Rocky Mountain spotted fever (RMSF)**, a tick-borne illness.
- **Doxycycline** is the first-line and most effective treatment for RMSF, regardless of age or rash presentation.
*Azithromycin*
- While effective for some bacterial infections, **azithromycin** is not the recommended treatment for RMSF and has shown poor efficacy against *Rickettsia rickettsii*.
- It is typically used for atypical pneumonia, chlamydial infections, and certain strep infections.
*Pyrazinamide*
- **Pyrazinamide** is an antitubercular drug used in combination therapy for **tuberculosis**.
- It has no role in the treatment of tick-borne rickettsial infections like RMSF.
*Vancomycin*
- **Vancomycin** is a glycopeptide antibiotic primarily used for serious **Gram-positive bacterial infections**, especially those resistant to other antibiotics (e.g., MRSA, *C. difficile*).
- It is not effective against rickettsial organisms.
*Praziquantel*
- **Praziquantel** is an anthelmintic medication used to treat **parasitic worm infections**, such as schistosomiasis and tapeworm infections.
- It has no activity against bacterial infections like RMSF.
Blood and tissue parasites US Medical PG Question 10: A 41-year-old male with a history of Pneumocystis jirovecii pneumonia is found to have multiple ring-enhancing lesions on brain CT. Which of the following is most likely responsible for this patient's abnormal scan?
- A. Protozoa (Correct Answer)
- B. Virus
- C. Neoplasm
- D. Bacteria
- E. Prion
Blood and tissue parasites Explanation: ***Protozoa***
- The patient's history of **Pneumocystis jirovecii pneumonia** (PJP) suggests an **immunocompromised state**, likely due to HIV/AIDS.
- In such patients, **ring-enhancing brain lesions** are highly characteristic of **cerebral toxoplasmosis**, an opportunistic infection caused by the protozoan *Toxoplasma gondii*.
*Virus*
- While viruses like **CMV** or **JC virus** (causing PML) can affect the brain in immunocompromised patients, they typically present with different imaging features (e.g., non-enhancing lesions in PML) and are less likely to cause multiple ring-enhancing lesions.
- Though HIV can cause **HIV encephalopathy**, it typically involves **diffuse atrophy** and **white matter changes**, rather than distinct ring-enhancing lesions.
*Neoplasm*
- **Primary central nervous system lymphoma (PCNSL)** can present with ring-enhancing lesions, especially in HIV-positive individuals.
- However, given the association with PJP, **infectious etiologies** like toxoplasmosis are generally more common as the initial diagnosis for multiple ring-enhancing lesions in this patient population.
*Bacteria*
- **Bacterial brain abscesses** can cause ring-enhancing lesions but are less common in disseminated opportunistic infections in HIV/AIDS compared to protozoal or fungal infections.
- They also typically present with a more **acute inflammatory picture** and may be preceded by a source of bacterial infection (e.g., endocarditis, sinusitis) not mentioned here.
*Prion*
- **Prion diseases** (e.g., Creutzfeldt-Jakob disease) cause rapidly progressive dementia and characteristic EEG and MRI findings (e.g., cortical ribboning, basal ganglia hyperintensity) that do not typically include multiple ring-enhancing lesions.
- They are also not associated with the immunocompromised state indicated by PJP.
More Blood and tissue parasites US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.