Antiparasitic medications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antiparasitic medications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
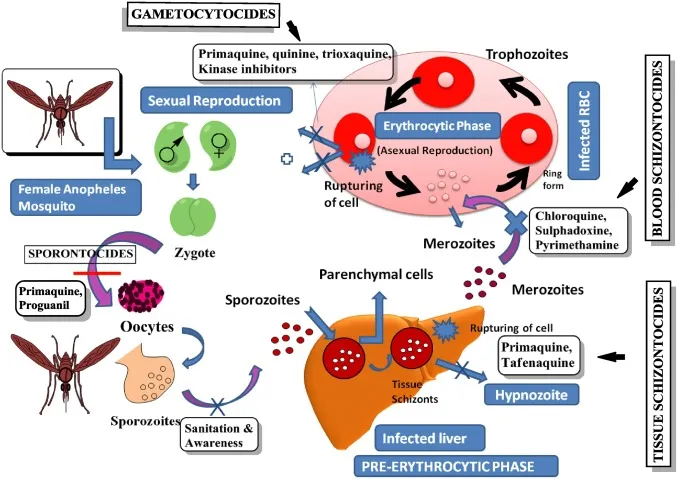
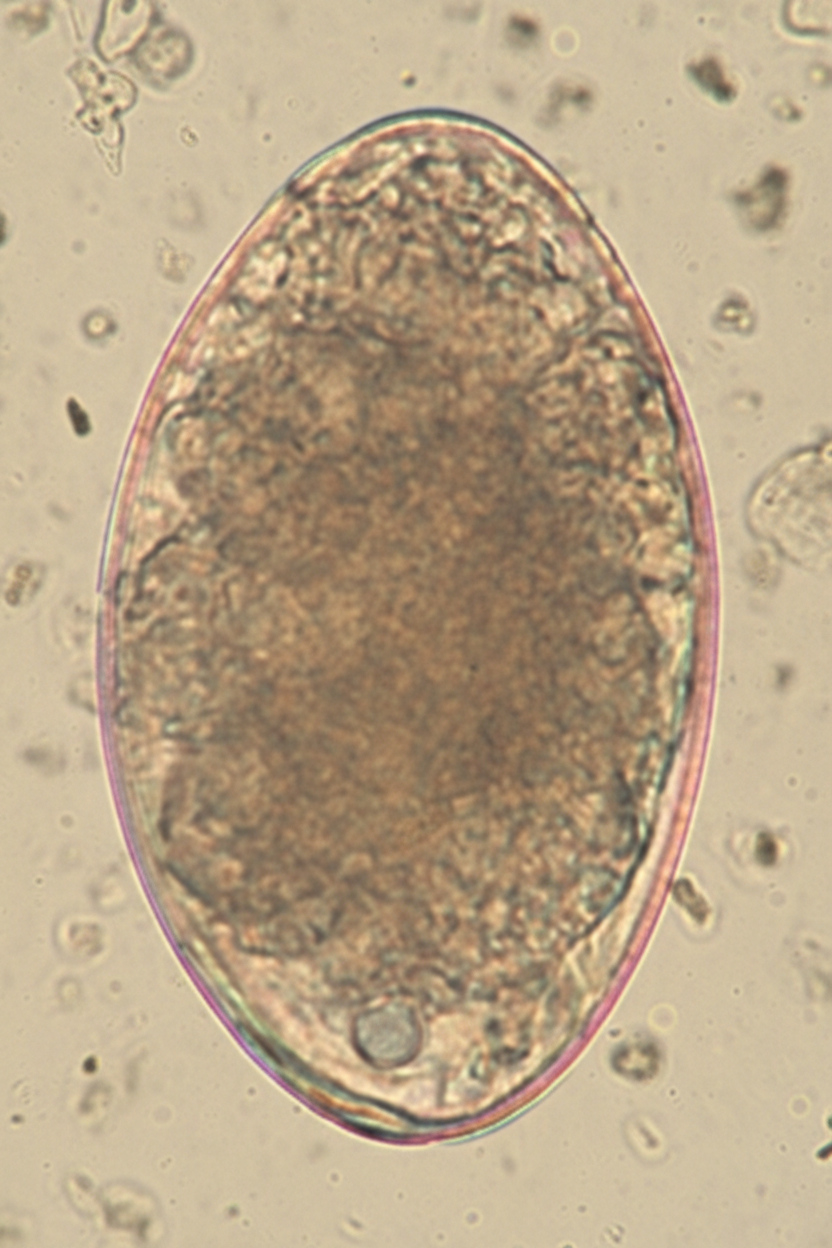
Antiparasitic medications US Medical PG Question 1: A 7-year-old girl is brought to the physician by her mother because of a 4-week history of irritability, diarrhea, and a 2.2-kg (5-lb) weight loss that was preceded by a dry cough. The family returned from a vacation to Indonesia 2 months ago. Her vital signs are within normal limits. Abdominal examination shows mild tenderness with no guarding or rebound and increased bowel sounds. Her leukocyte count is 9,200/mm3 with 20% eosinophils. A photomicrograph of a wet stool mount is shown. Which of the following is the most appropriate pharmacotherapy?
- A. Diethylcarbamazine
- B. Metronidazole
- C. Albendazole (Correct Answer)
- D. Praziquantel
- E. Doxycycline
Antiparasitic medications Explanation: ***Albendazole***
- The image shows a **hookworm egg**, characterized by its thin shell and developing larva inside; clinical features like **eosinophilia**, diarrhea, weight loss, and travel to an endemic area (Indonesia) are consistent with hookworm infection.
- **Albendazole** is the drug of choice for treating hookworm infections and other intestinal nematode infections.
*Diethylcarbamazine*
- This drug is primarily used for treating **lymphatic filariasis** (e.g., Wuchereria bancrofti, Brugia malayi) and **Loiasis** (African eye worm).
- It is not effective against hookworm infections.
*Metronidazole*
- **Metronidazole** is an antimicrobial agent effective against certain parasitic infections like **Giardia**, **Entamoeba histolytica**, and bacterial vaginosis.
- It is not indicated for the treatment of hookworm infections.
*Praziquantel*
- **Praziquantel** is an anthelminthic drug primarily used to treat infections caused by **flukes** (e.g., Schistosoma species) and **tapeworms** (e.g., Taenia species).
- It is not effective against hookworm infections.
*Doxycycline*
- **Doxycycline** is a tetracycline antibiotic with broad-spectrum activity against various bacterial infections and is also used in the treatment of some parasitic infections like **malaria prophylaxis** and **filariasis** (due to activity against Wolbachia endosymbionts).
- It is not a primary treatment for hookworm infections.
Antiparasitic medications US Medical PG Question 2: A 21-year-old male presents after several days of flatulence and greasy, foul-smelling diarrhea. The patient reports symptoms of nausea and abdominal cramps followed by sudden diarrhea. He says that his symptoms started after he came back from a camping trip. When asked about his camping activities, he reports that his friend collected water from a stream, but he did not boil or chemically treat the water. His temperature is 98.6°F (37°C), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Stool is sent for microscopy which returns positive for motile protozoans. Which of the following antibiotics should be started in this patient?
- A. Vancomycin
- B. Erythromycin
- C. Cephalexin
- D. Ciprofloxacin
- E. Metronidazole (Correct Answer)
Antiparasitic medications Explanation: ***Metronidazole***
- This patient's symptoms (greasy, foul-smelling diarrhea, flatulence) after consuming untreated stream water are highly suggestive of **Giardiasis**, caused by *Giardia lamblia*.
- **Metronidazole** is the first-line antibiotic for treating Giardiasis due to its efficacy against anaerobic parasites and protozoa.
*Vancomycin*
- **Vancomycin** is primarily used for serious gram-positive bacterial infections, particularly **methicillin-resistant *Staphylococcus aureus* (MRSA)** and *Clostridioides difficile* colitis.
- It has no activity against protozoal infections like Giardiasis.
*Erythromycin*
- **Erythromycin** is a macrolide antibiotic effective against a range of bacterial infections, including atypical pneumonia and certain sexually transmitted infections.
- It is not effective against protozoal parasites.
*Cephalexin*
- **Cephalexin** is a first-generation cephalosporin antibiotic used to treat bacterial infections such as skin and soft tissue infections, strep throat, and urinary tract infections.
- It does not have activity against protozoans.
*Ciprofloxacin*
- **Ciprofloxacin** is a fluoroquinolone antibiotic used for various bacterial infections, including urinary tract infections, gastrointestinal infections (e.g., traveler's diarrhea caused by bacteria), and respiratory tract infections.
- While effective against many bacteria, it is not the primary treatment for protozoal infections like Giardiasis.
Antiparasitic medications US Medical PG Question 3: Three days after starting a new drug for malaria prophylaxis, a 19-year-old college student comes to the physician because of dark-colored urine and fatigue. He has not had any fever, dysuria, or abdominal pain. He has no history of serious illness. Physical examination shows scleral icterus. Laboratory studies show a hemoglobin of 9.7 g/dL and serum lactate dehydrogenase of 234 U/L. Peripheral blood smear shows poikilocytes with bite-shaped irregularities. Which of the following drugs has the patient most likely been taking?
- A. Dapsone
- B. Doxycycline
- C. Primaquine (Correct Answer)
- D. Ivermectin
- E. Pyrimethamine
Antiparasitic medications Explanation: ***Primaquine***
- The patient's symptoms, including **dark urine**, **fatigue**, **scleral icterus**, **anemia** (hemoglobin 9.7 g/dL), elevated **LDH**, and **bite cells** on peripheral smear, are classic signs of **acute hemolytic anemia**.
- **Primaquine** is an antimalarial drug known to cause oxidative stress, leading to hemolysis in individuals with **glucose-6-phosphate dehydrogenase (G6PD) deficiency**. The "bite cells" are a hallmark of G6PD deficiency, as they result from the spleen removing Heinz bodies (oxidized hemoglobin).
*Dapsone*
- While **dapsone** can also cause **hemolytic anemia** in G6PD-deficient patients due to its oxidative properties, it is **not used for malaria prophylaxis**.
- Dapsone is primarily used for conditions like leprosy, dermatitis herpetiformis, and Pneumocystis pneumonia prophylaxis, making it an unlikely choice in this clinical scenario.
*Doxycycline*
- **Doxycycline** is a tetracycline antibiotic commonly used for malaria prophylaxis.
- Its common side effects include **photosensitivity**, **gastrointestinal upset**, and **esophageal irritation**, but it does not typically cause hemolytic anemia or bite cells.
*Ivermectin*
- **Ivermectin** is an antiparasitic drug used for conditions like onchocerciasis, strongyloidiasis, and scabies, but **not for malaria prophylaxis**.
- Side effects usually involve **neurological symptoms**, **skin reactions**, and **gastrointestinal disturbances**, but not hemolytic anemia.
*Pyrimethamine*
- **Pyrimethamine** is an antifolate drug used in combination with other drugs for malaria treatment and prophylaxis.
- Its primary adverse effects relate to **bone marrow suppression** (e.g., megaloblastic anemia, leukopenia), not hemolytic anemia or bite cells.
Antiparasitic medications US Medical PG Question 4: A 30-year-old man presents to the physician after he discovered a raised, red, string-shaped lesion beneath the skin on his right foot. The lesion seems to move from one location to another over the dorsum of his foot from day to day. He says that the lesion is extremely itchy and has not responded to over the counter topical treatment. He and his wife recently returned from a honeymoon in southern Thailand, where they frequented the tropical beaches. The physician diagnoses him with a parasitic infection and prescribes albendazole for the patient. With which of the following organisms is the patient most likely infected?
- A. Ancylostoma braziliense (Correct Answer)
- B. Dracunculus medinensis
- C. Necator americanus
- D. Strongyloides stercoralis
- E. Wuchereria bancrofti
Antiparasitic medications Explanation: ***Ancylostoma braziliense***
- This clinical presentation of a **pruritic, migratory, serpiginous rash** on the foot after exposure to contaminated sand (tropical beach in Thailand) is classic for **cutaneous larva migrans**, caused by hookworm larvae, predominantly *Ancylostoma braziliense*.
- The larvae penetrate the skin but cannot complete their life cycle in humans, instead migrating subcutaneously, causing the characteristic **"creeping eruption"**.
*Dracunculus medinensis*
- This parasite causes **dracunculiasis**, where the adult female worm migrates to the skin, creating a painful blister, often on the lower limbs, from which it emerges.
- It is acquired by ingesting **copepods** (water fleas) containing larvae, not by direct contact with contaminated sand, and the lesion typically ulcerates rather than migrating repeatedly.
*Necator americanus*
- This is a human hookworm that causes **iron deficiency anemia** and can lead to **cutaneous larva currens** from larval penetration, which is a rapidly advancing linear lesion, but it typically progresses to systemic infection where the worms reside in the small intestine.
- While it can cause an itchy rash at the site of penetration (ground itch), it does not cause the **chronic, migratory, serpiginous eruption** characteristic of cutaneous larva migrans.
*Strongyloides stercoralis*
- This parasite can cause **larva currens** (a rapidly moving linear skin eruption) and systemic complications, particularly in immunocompromised individuals.
- While it can cause skin lesions, the typical description is of a much faster-moving lesion that usually spreads from the anus and is less serpiginous and persistent in one area compared to the classic presentation of cutaneous larva migrans.
*Wuchereria bancrofti*
- This nematode causes **lymphatic filariasis** (elephantiasis), characterized by lymphedema, hydrocele, and chyluria, and is transmitted by **mosquito bites**.
- It does not cause cutaneous migratory lesions on the foot; its pathology relates to chronic lymphatic obstruction by adult worms.
Antiparasitic medications US Medical PG Question 5: A 24-year-old woman comes to the emergency department because of a 4-hour history of headaches, nausea, and vomiting. During this time, she has also had recurrent dizziness and palpitations. The symptoms started while she was at a friend's birthday party, where she had one beer. One week ago, the patient was diagnosed with a genitourinary infection and started on antimicrobial therapy. She has no history of major medical illness. Her pulse is 106/min and blood pressure is 102/73 mm Hg. Physical examination shows facial flushing and profuse sweating. The patient is most likely experiencing adverse effects caused by treatment for an infection with which of the following pathogens?
- A. Candida albicans
- B. Chlamydia trachomatis
- C. Neisseria gonorrhoeae
- D. Herpes simplex virus
- E. Trichomonas vaginalis (Correct Answer)
Antiparasitic medications Explanation: ***Trichomonas vaginalis***
- The patient's symptoms (headache, nausea, vomiting, dizziness, palpitations, facial flushing, sweating) after consuming alcohol while on antimicrobial therapy for a genitourinary infection are characteristic of a **disulfiram-like reaction**.
- **Metronidazole**, a common treatment for *Trichomonas vaginalis* infection, is known to cause a disulfiram-like reaction when combined with alcohol, due to inhibition of **acetaldehyde dehydrogenase**.
*Candida albicans*
- Genitourinary infections with *Candida albicans* (e.g., vulvovaginal candidiasis) are typically treated with **antifungal medications** like fluconazole, which do not cause disulfiram-like reactions with alcohol.
- While symptoms like headache can occur with some antifungals, the constellation of flushing, palpitations, and nausea after a single beer strongly points away from this pathogen.
*Chlamydia trachomatis*
- *Chlamydia trachomatis* is commonly treated with **azithromycin** or **doxycycline**, neither of which are associated with disulfiram-like reactions to alcohol.
- The patient's symptoms are specific to alcohol interaction with certain antimicrobials, not typical side effects of these antibiotics.
*Neisseria gonorrhoeae*
- Infections with *Neisseria gonorrhoeae* are usually treated with **ceftriaxone** (often with azithromycin), which also do not cause disulfiram-like reactions.
- The clinical presentation after alcohol consumption is inconsistent with the typical adverse effects of these treatments.
*Herpes simplex virus*
- Genitourinary infections caused by herpes simplex virus are treated with **antiviral medications** such as acyclovir or valacyclovir.
- These antiviral drugs do not cause disulfiram-like reactions when ingested with alcohol.
Antiparasitic medications US Medical PG Question 6: A 16-year-old boy is brought to the physician by his host parents for evaluation of a progressively pruritic rash over his shoulders and buttocks for the past 6 months. He recently came to the United States from Nigeria to attend a year of high school. He reports that it has been increasingly difficult for him to read the whiteboard during classes. Physical examination shows symmetrically distributed papules 4–8 mm in diameter, excoriation marks, and patchy hyperpigmentation over his shoulders, waist, and buttocks. There is nontender inguinal lymphadenopathy and several firm, nontender subcutaneous nodules along the right iliac crest. Six skin snip biopsies are taken from the pelvic girdle, buttocks, and thigh, and are then incubated in saline. After 24 hours, microscopic examination shows motile microfilariae. Which of the following is the most likely diagnosis?
- A. Cysticercosis
- B. Onchocerciasis (Correct Answer)
- C. Lymphatic filariasis
- D. Cutaneous larva migrans
- E. Trichuriasis
Antiparasitic medications Explanation: ***Onchocerciasis***
- The presentation of **pruritic rash with papules**, **subcutaneous nodules** (onchocercomas), and **visual difficulties** (river blindness) in an individual from an endemic area (Nigeria) is classic for **onchocerciasis**.
- The presence of **motile microfilariae in skin snips** after saline incubation is a diagnostic hallmark of this condition, caused by *Onchocerca volvulus*.
*Cysticercosis*
- This condition is caused by the larval stage of *Taenia solium* and typically presents with **calcified lesions** in the muscle and brain (neurocysticercosis), which can lead to seizures.
- It does not typically cause the generalized pruritic rash, subcutaneous nodules, or ocular symptoms described, nor would **motile microfilariae** be found in skin snips.
*Lymphatic filariasis*
- Caused by *Wuchereria bancrofti* or *Brugia malayi*, this disease is characterized by **lymphedema** and **hydrocele**, eventually leading to **elephantiasis**.
- While it involves filarial worms and can cause lymphadenopathy, it does not typically manifest with the described rash, vision problems, or **subcutaneous nodules** (onchocercomas).
*Cutaneous larva migrans*
- This condition, caused by hookworm larvae (e.g., *Ancylostoma braziliense*), presents as a **serpiginous, intensely pruritic eruption** where the larvae migrate under the skin.
- It does not cause subcutaneous nodules, generalized papular rash, or ocular involvement, and skin snips would not show **microfilariae**.
*Trichuriasis*
- Caused by the **whipworm** (*Trichuris trichiura*), this is an intestinal nematode infection that can lead to **abdominal pain**, **diarrhea**, **rectal prolapse**, and **anemia**.
- It does not present with skin lesions, subcutaneous nodules, or visual impairment, and diagnosis is typically made by finding **ova in stool samples**, not microfilariae in skin snips.
Antiparasitic medications US Medical PG Question 7: A 46-year-old man comes to the physician because of a 1-week history of headache, muscle pain, and recurrent fever spikes that occur without a noticeable rhythm. Two weeks ago, he returned from a 5-week-long world trip during which he climbed several mountains in India, Africa, and Appalachia. Chemoprophylaxis with chloroquine was initiated one week prior to the trip. Physical examination shows jaundice. The spleen is palpated 2 cm below the left costal margin. His hemoglobin concentration is 10 g/dL. A photomicrograph of a peripheral blood smear is shown. Which of the following agents is the most likely cause of this patient's findings?
- A. Chikungunya virus
- B. Trypanosoma cruzi
- C. Leishmania donovani
- D. Plasmodium falciparum (Correct Answer)
- E. Trypanosoma brucei
Antiparasitic medications Explanation: **Plasmodium falciparum**
- The image shows **multiple ring forms** and **applique forms** within red blood cells, which are characteristic of *Plasmodium falciparum* malaria. The clinical presentation of **headache, muscle pain, recurrent fever spikes without a noticeable rhythm, jaundice, splenomegaly, and anemia (Hb 10 g/dL)** in a traveler returning from India and Africa is highly consistent with malaria, especially given the chloroquine chemoprophylaxis which is often ineffective against chloroquine-resistant strains of *P. falciparum*.
- *P. falciparum* can cause severe disease, including **anemia** due to red blood cell destruction and **jaundice** due to hemolysis and liver involvement, and is notorious for its **irregular fever patterns** early in the infection cycle.
*Chikungunya virus*
- Chikungunya typically presents with **high fever, severe polyarthralgia**, and rash, but does not cause the parasitemia or specific red blood cell morphology seen in the image.
- While present in endemic regions like India and Africa, it does not lead to **anemia, splenomegaly, or jaundice** to the extent seen in this patient, nor does it appear on a blood smear as intracellular parasites.
*Trypanosoma cruzi*
- *Trypanosoma cruzi* causes **Chagas disease**, which is endemic to **Central and South America**, not India or Africa.
- While it can be found in blood smears during the acute phase (trypomastigotes), its morphology differs significantly from the ring forms seen, and the overall clinical picture of **fever, jaundice, and marked splenomegaly with characteristic RBC parasites** does not fit Chagas disease.
*Leishmania donovani*
- *Leishmania donovani* causes **visceral leishmaniasis (kala-azar)**, characterized by **prolonged fever, splenomegaly, hepatomegaly, pancytopenia**, and weight loss.
- While present in India and Africa, the parasites (**amastigotes**) are typically found within **macrophages** in bone marrow, spleen, or liver aspirates, not as ring forms within red blood cells on a peripheral blood smear.
*Trypanosoma brucei*
- *Trypanosoma brucei* causes **African sleeping sickness**, which involves **fever, headache, joint pain, neurological symptoms**, and lymphadenopathy (Winterbottom's sign).
- The parasites (trypomastigotes) are observed extracellularly in the blood, lymph, or CSF, and have a distinct **elongated, flagellated morphology** that is completely different from the intracellular ring forms seen in the provided image.
Antiparasitic medications US Medical PG Question 8: A 27-year-old previously healthy man presents to the clinic complaining of bloody diarrhea and abdominal pain. Sexual history reveals that he has sex with men and women and uses protection most of the time. He is febrile with all other vital signs within normal limits. Physical exam demonstrates tenderness to palpation of the right upper quadrant. Subsequent ultrasound shows a uniform cyst in the liver. In addition to draining the potential abscess and sending it for culture, appropriate medical therapy would involve which of the following?
- A. Supportive therapy
- B. Metronidazole and iodoquinol (Correct Answer)
- C. Sulfadiazine and pyrimethamine
- D. Nifurtimox
- E. Amphotericin
Antiparasitic medications Explanation: ***Metronidazole and iodoquinol***
- The patient's symptoms (bloody diarrhea, abdominal pain, fever, liver cyst) and risk factors (sexual activity with men and women) are highly suggestive of an **amoebic liver abscess** caused by *Entamoeba histolytica*.
- **Metronidazole** is the drug of choice for invasive amoebiasis (including liver abscess), while **iodoquinol** (or paromomycin) treats the intestinal luminal cysts to prevent recurrence and transmission.
*Supportive therapy*
- While supportive care is important for managing symptoms like fever and dehydration, it does not address the underlying **amoebic infection** or the liver abscess.
- Delaying specific antimicrobial therapy can lead to worsening of the abscess, potential rupture, and increased morbidity.
*Sulfadiazine and pyrimethamine*
- This combination is the standard treatment for **toxoplasmosis**, a protozoal infection that typically affects immunocompromised individuals and can cause encephalitis or disseminated disease.
- It is not effective against *Entamoeba histolytica* and would not resolve an amoebic liver abscess.
*Nifurtimox*
- **Nifurtimox** is an antiparasitic medication specifically used to treat **Chagas disease**, caused by *Trypanosoma cruzi*.
- Chagas disease presents with different clinical manifestations and is transmitted by blood-sucking triatomine bugs, which does not fit the patient's presentation.
*Amphotericin*
- **Amphotericin B** is a broad-spectrum **antifungal agent** used to treat severe systemic fungal infections.
- It has no activity against *Entamoeba histolytica* or other protozoal infections causing similar symptoms.
Antiparasitic medications US Medical PG Question 9: A 37-year-old man makes an appointment with his primary care physician because he has been feeling tired and is no longer able to play on a recreational soccer team. He also says his coworkers have commented that he appears pale though he has not noticed any changes himself. He says that he has been generally healthy and that the only notable event that happened in the last year is that he went backpacking all over the world. Based on clinical suspicion, a series of blood tests are performed with partial results presented below:
Hemoglobin: 9.8 g/dL
Platelet count: 174,000/mm^3
Mean corpuscular volume: 72 µm^3 (normal: 80-100 µm^3)
Iron: 22 µg/dL (normal: 50-170 µg/dL)
Ferritin: 8 ng/mL (normal: 15-200 ng/mL)
Lactate dehydrogenase: 57 U/L (normal: 45-90 U/L)
Urine hemoglobin: absent
Infection with which of the following types of organisms could lead to this pattern of findings?
- A. Nematode (Correct Answer)
- B. Mosquito-borne protozoa
- C. Double-stranded virus
- D. Single-stranded virus
- E. Tick-borne protozoa
Antiparasitic medications Explanation: ***Nematode***
- The patient's symptoms (fatigue, pallor) and lab results (**microcytic anemia** with **low hemoglobin**, **low MCV**, **low iron**, and **low ferritin**) are highly suggestive of **iron deficiency anemia**. The history of backpacking worldwide increases the suspicion of **hookworm infection**, which is a nematode that causes chronic gastrointestinal blood loss leading to iron deficiency.
- **Hookworms** (e.g., *Ancylostoma duodenale*, *Necator americanus*) attach to the intestinal wall, causing persistent blood loss as they feed, which depletes iron stores over time.
*Mosquito-borne protozoa*
- **Mosquito-borne protozoa** primarily refers to *Plasmodium* species which cause malaria. While malaria can cause anemia, it typically presents with **hemolytic anemia** (elevated LDH, jaundice), intermittent fevers, and splenomegaly, not the profound iron deficiency seen here.
- The anemia in malaria is usually **normocytic or macrocytic** due to increased erythropoiesis, and profound iron deficiency is not the primary mechanism.
*Double-stranded virus*
- **Double-stranded viruses** (e.g., adenoviruses, herpesviruses, some papillomaviruses) typically cause acute infections, and while some can lead to anemia through bone marrow suppression or chronic inflammation, they do not directly cause **iron deficiency anemia** with this specific lab profile.
- The clinical picture of chronic fatigue and iron depletion after travel is not characteristic of common viral infections caused by double-stranded viruses.
*Single-stranded virus*
- **Single-stranded viruses** (e.g., influenza, measles, HIV, dengue, enteroviruses) cause a wide range of illnesses. While some can lead to anemia, often through **bone marrow suppression** or chronic inflammation, they are not typically associated with the profound **iron deficiency** and microcytic anemia seen in this patient.
- Travel history can be relevant for some single-stranded viral infections (e.g., HIV, dengue), but the specific laboratory findings point away from a primary viral etiology for the anemia.
*Tick-borne protozoa*
- **Tick-borne protozoa** most commonly refers to *Babesia* species, which cause babesiosis. This disease primarily leads to **hemolytic anemia** (intravascular hemolysis, elevated LDH), fever, chills, and fatigue, which is distinct from the **iron deficiency anemia** presented in the case.
- **Babesiosis** would typically present with signs of hemolysis, such as elevated LDH and sometimes hemoglobinuria, which are absent in this patient.
Antiparasitic medications US Medical PG Question 10: A 27-year-old male who works on an organic farm is diagnosed with infection by N. americanus, a helminthic parasite. Eosinophils require which antibody isotype to destroy these parasites via antibody-dependent cellular cytotoxicity?
- A. IgE (Correct Answer)
- B. IgA
- C. IgG
- D. IgM
- E. IgD
Antiparasitic medications Explanation: ***IgE***
- **IgE** antibodies are crucial in the immune response against helminthic parasites, including *N. americanus*, by sensitizing **mast cells** and **eosinophils**.
- When **IgE** binds to the surface of parasites, the **Fc receptor** on eosinophils recognizes the Fc portion of IgE, leading to the release of cytotoxic granules that destroy the parasite (antibody-dependent cellular cytotoxicity).
*IgA*
- **IgA** is primarily found in **mucosal secretions** and plays a role in defending against pathogens at mucosal surfaces, but it is not the primary isotype involved in eosinophil-mediated **ADCC** against helminths.
- While IgA can bind to some immune cells, its main function is to **neutralize toxins** and prevent microbial adhesion at mucosal sites.
*IgG*
- **IgG** is the most abundant antibody in serum and is involved in various immune functions, including **opsonization**, **neutralization**, and **complement activation**.
- Although IgG can mediate ADCC by **NK cells** and **macrophages**, it is not the primary isotype for eosinophil-mediated killing of helminths, which is dominated by IgE.
*IgM*
- **IgM** is typically the first antibody produced during a primary immune response and is very effective at **activating the complement system**.
- Its large pentameric structure also limits its diffusion into tissues, and it does not play a direct role in eosinophil-mediated ADCC against helminthic parasites.
*IgD*
- **IgD** primarily functions as a **B cell receptor** on naive B lymphocytes, signaling for their activation and differentiation.
- It is present in very low concentrations in serum and its role in host defense against parasites or in ADCC is negligible.
More Antiparasitic medications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.