Soil-transmitted helminths US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Soil-transmitted helminths. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Soil-transmitted helminths US Medical PG Question 1: A 4-year-old girl presents with recurrent abdominal pain and a low-grade fever for the past 2 months. The patient’s mother says that she has lost her appetite which has caused some recent weight loss. She adds that the patient frequently plays outdoors with their pet dog. The patient is afebrile and vital signs are within normal limits. On physical examination, conjunctival pallor is present. Abdominal examination reveals a diffusely tender abdomen and significant hepatomegaly. There is also a solid mass palpable in the right upper quadrant measuring about 3 x 4 cm. Laboratory findings are significant for the following:
Hemoglobin (Hb%) 9.9 g/dL
Total count (WBC) 26,300/µL
Differential count
Neutrophils 36%
Lymphocytes 16%
Eosinophils 46%
Platelets 200,000/mm3
Erythrocyte sedimentation rate 56 mm/h
C-reactive protein 2 mg/L
Serum globulins 5 g/dL
Laparoscopic resection of the mass is performed, and a tissue sample is sent for histopathology. Which of the following is the organism most likely responsible for this patient’s condition?
- A. Ancylostoma braziliense
- B. Ascaris lumbricoides
- C. Toxocara canis (Correct Answer)
- D. Trichuris trichiura
- E. Toxocara cati
Soil-transmitted helminths Explanation: ***Toxocara canis***
- The child's history of playing outdoors with a pet dog, **eosinophilia**, **hepatomegaly**, abdominal mass, and **elevated globulins** are highly suggestive of **visceral larva migrans (VLM)**, most commonly caused by *Toxocara canis*.
- *Toxocara canis* larvae migrate through human tissues, particularly the liver, causing granuloma formation that can present as palpable masses and systemic symptoms.
*Ancylostoma braziliense*
- This hookworm primarily causes **cutaneous larva migrans**, presenting as an intensely pruritic, serpiginous rash.
- It does not typically cause systemic symptoms like hepatomegaly, abdominal masses, or significant eosinophilia in the way described.
*Ascaris lumbricoides*
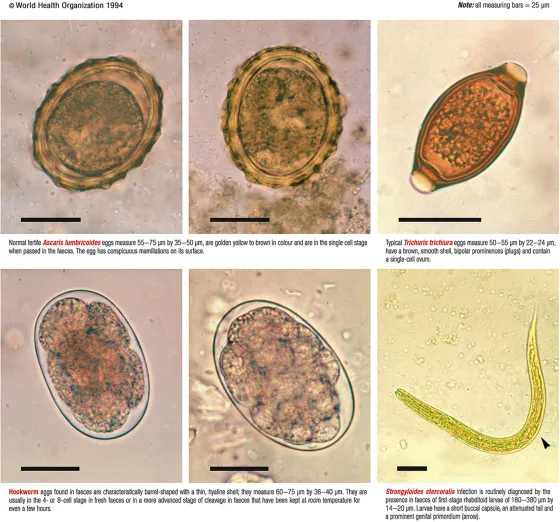
- *Ascaris lumbricoides* causes **ascariasis**, primarily manifesting as intestinal symptoms, malnutrition, or pulmonary symptoms during larval migration (Löffler syndrome)
- While it can cause eosinophilia, it rarely presents with solid hepatic masses or the specific constellation of symptoms seen here.
*Trichuris trichiura*
- *Trichuris trichiura* causes **trichuriasis** (whipworm infection), primarily leading to **gastrointestinal symptoms** such as abdominal pain, diarrhea, and rectal prolapse in heavy infections.
- It is not associated with migratory visceral larvae, hepatomegaly, or palpable liver masses.
*Toxocara cati*
- While *Toxocara cati* also causes visceral larva migrans, it is associated with **cats** rather than dogs. The patient's history specifically mentions a pet dog.
- The clinical presentation with hepatomegaly, abdominal mass, and eosinophilia would otherwise be consistent with *Toxocara* infection.
Soil-transmitted helminths US Medical PG Question 2: A 22-year-old man presents with abdominal cramps and diarrhea over the last few weeks. He notes that several of his bowel movements have a small amount of blood. Past medical history is significant for an intermittent cough that has been persistent since returning from Mexico last month. The patient takes no current medications. On physical examination, there is diffuse tenderness to palpation. Which of the following medications is indicated for this patient’s condition?
- A. Pyrantel
- B. Praziquantel
- C. Albendazole
- D. Mebendazole
- E. Ivermectin (Correct Answer)
Soil-transmitted helminths Explanation: ***Ivermectin***
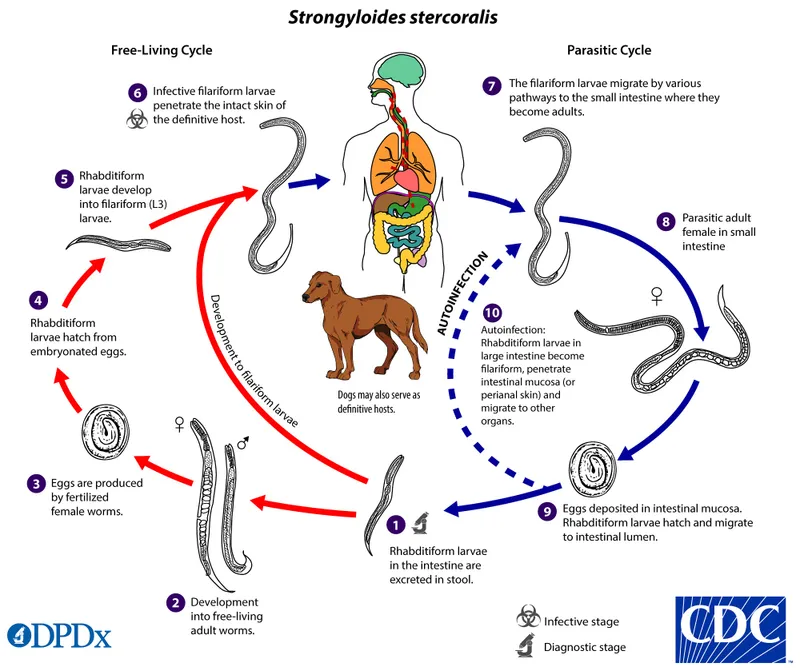
- This patient's symptoms (abdominal cramps, bloody diarrhea, persistent cough, recent travel to Mexico) are highly suggestive of **Strongyloidiasis**. **Ivermectin** is the drug of choice for this parasitic infection.
- Strongyloidiasis larvae can cause a **transient cough** as they migrate through the lungs, and adult worms in the intestines lead to gastrointestinal symptoms like **diarrhea** and abdominal pain.
*Pyrantel*
- **Pyrantel** is primarily effective against **pinworms**, **roundworms**, and **hookworms**, but not Strongyloides.
- It works by neuromuscular blockade, causing paralysis and expulsion of the worms.
*Praziquantel*
- **Praziquantel** is the drug of choice for treating **tapeworm** infections (e.g., Taenia species) and **schistosomiasis**.
- It acts by increasing the permeability of the worm's cells to calcium, leading to paralysis and death.
*Albendazole*
- **Albendazole** is a broad-spectrum anthelmintic effective against many intestinal nematodes, including **hookworm**, **roundworm**, and **whipworm**, and some tissue nematodes.
- While it has some activity against Strongyloides, **Ivermectin is generally preferred** due to higher efficacy and fewer side effects in many cases of strongyloidiasis.
*Mebendazole*
- **Mebendazole** is effective against various intestinal worms such as **pinworms**, **roundworms**, and **hookworms**.
- Its mechanism of action involves inhibiting microtubule synthesis, thereby impairing glucose uptake by the worms.
Soil-transmitted helminths US Medical PG Question 3: A 32-year-old woman presents to your office with abdominal pain and bloating over the last month. She also complains of intermittent, copious, non-bloody diarrhea over the same time. Last month, she had a cough that has since improved but has not completely resolved. She has no sick contacts and has not left the country recently. She denies any myalgias, itching, or rashes. Physical and laboratory evaluations are unremarkable. Examination of her stool reveals the causative organism. This organism is most likely transmitted to the human host through which of the following routes?
- A. Insect bite
- B. Penetration of skin (Correct Answer)
- C. Sexual contact
- D. Inhalation
- E. Animal bite
Soil-transmitted helminths Explanation: ***Penetration of skin***
- The symptoms of **abdominal pain**, **bloating**, **intermittent copious non-bloody diarrhea**, and a recent **cough** are highly suggestive of a **hookworm infection**.
- Hookworm larvae (filariform larvae) primarily penetrate the skin, usually through bare feet, as their mode of entry into the human host.
*Insect bite*
- Although some parasitic infections are transmitted by insect bites (e.g., malaria, Chagas disease), hookworms are not transmitted this way.
- **Insect-borne diseases** typically present with different clinical manifestations or geographical associations.
*Sexual contact*
- **Sexually transmitted infections** involve direct contact of mucous membranes or body fluids during sexual activity.
- Hookworm infection transmission through sexual contact is not a recognized route.
*Inhalation*
- **Inhalation** is a route of transmission for respiratory pathogens (e.g., influenza, tuberculosis) or certain fungal infections, but not for hookworms.
- While hookworm larvae migrate through the lungs, the initial infection pathway is not via inhalation.
*Animal bite*
- **Animal bites** transmit diseases like rabies or certain bacterial infections, but not parasitic hookworms.
- Hookworm infection does not result from direct contact with an animal's saliva or puncture wound.
Soil-transmitted helminths US Medical PG Question 4: A 17-year-old girl comes to the physician because of a 1-week history of severe itching in the area of her genitals. She reports that the itching is most severe at night. She has been sexually active with three partners over the past year; she uses condoms for contraception. Her current sexual partner is experiencing similar symptoms. Pelvic examination shows vulvar excoriations. A photomicrograph of an epilated pubic hair is shown. Which of the following is the most likely causal organism?
- A. Pediculus humanus
- B. Epidermophyton floccosum
- C. Phthirus pubis (Correct Answer)
- D. Enterobius vermicularis
- E. Sarcoptes scabiei
Soil-transmitted helminths Explanation: ***Phthirus pubis***
- The symptoms of **pruritus**, especially **worse at night**, and the involvement of the **genital area** are classic for **pubic lice** (P. pubis or "crabs").
- The photomicrograph of an **epilated pubic hair with attached nits** (lice eggs) or an adult louse, along with her partner's similar symptoms, confirms the diagnosis.
*Pediculus humanus*
- This refers to **body lice** or **head lice**. While P. humanus capitis (head lice) can cause pruritus, it typically affects the scalp and is less common in the pubic area.
- **Body lice** usually inhabit clothing and only come to the skin to feed, causing generalized itching rather than specific genital pruritus with visible organisms on pubic hair.
*Epidermophyton floccosum*
- This is a **dermatophyte fungus** that causes **tinea cruris** (jock itch), which presents as an itchy, red, scaly rash, often with a raised border.
- It would not show up as organisms on pubic hair or cause excoriations specifically due to discrete insect bites.
*Enterobius vermicularis*
- This is a **pinworm** that causes **perianal pruritus**, especially at night, as the female worms migrate to lay eggs.
- While it causes itching in a similar area and is worse at night, it primarily affects the perianal region and is diagnosed by finding eggs via a **tape test**, not by visual inspection of pubic hair for organisms.
*Sarcoptes scabiei*
- This mite causes **scabies**, characterized by intense pruritus (worse at night) and a **papular rash**, often with **burrows**.
- While it can affect the genital area, the characteristic finding would be burrows or a widespread rash, not visible lice or nits attached to pubic hair as the primary finding.
Soil-transmitted helminths US Medical PG Question 5: A 26-year-old male with no significant past medical history goes camping with several friends in Virginia. Several days after returning, he begins to experience fevers, headaches, myalgias, and malaise. He also notices a rash on his wrists and ankles (Figure A). Which of following should be initiated for treatment of his condition?
- A. Azithromycin
- B. Doxycycline (Correct Answer)
- C. Pyrazinamide
- D. Vancomycin
- E. Praziquantel
Soil-transmitted helminths Explanation: ***Doxycycline***
- The patient's symptoms (fever, headache, myalgias, rash on wrists and ankles after camping in Virginia) are highly suggestive of **Rocky Mountain spotted fever (RMSF)**, a tick-borne illness.
- **Doxycycline** is the first-line and most effective treatment for RMSF, regardless of age or rash presentation.
*Azithromycin*
- While effective for some bacterial infections, **azithromycin** is not the recommended treatment for RMSF and has shown poor efficacy against *Rickettsia rickettsii*.
- It is typically used for atypical pneumonia, chlamydial infections, and certain strep infections.
*Pyrazinamide*
- **Pyrazinamide** is an antitubercular drug used in combination therapy for **tuberculosis**.
- It has no role in the treatment of tick-borne rickettsial infections like RMSF.
*Vancomycin*
- **Vancomycin** is a glycopeptide antibiotic primarily used for serious **Gram-positive bacterial infections**, especially those resistant to other antibiotics (e.g., MRSA, *C. difficile*).
- It is not effective against rickettsial organisms.
*Praziquantel*
- **Praziquantel** is an anthelmintic medication used to treat **parasitic worm infections**, such as schistosomiasis and tapeworm infections.
- It has no activity against bacterial infections like RMSF.
Soil-transmitted helminths US Medical PG Question 6: A previously healthy 48-year-old man comes to the physician because of a 2-week history of a nonpruritic rash on his right forearm. The rash began as pustules and progressed to form nodules and ulcers. He works as a gardener. Physical examination shows right axillary lymphadenopathy and the findings in the photograph. Which of the following is the most likely causal organism?
- A. Bartonella henselae
- B. Sporothrix schenckii (Correct Answer)
- C. Pasteurella multocida
- D. Blastomyces dermatitidis
- E. Pseudomonas aeruginosa
Soil-transmitted helminths Explanation: ***Sporothrix schenckii***
- The patient's occupation as a **gardener** and the description of a rash progressing from **pustules to nodules and ulcers**, associated with **axillary lymphadenopathy** along a lymphatic chain, are classic findings of **sporotrichosis** (rose gardener's disease), caused by *Sporothrix schenckii*.
- This fungus is found in soil and on plants, and infection typically occurs via **traumatic inoculation** (e.g., thorn prick).
*Bartonella henselae*
- This bacterium causes **cat-scratch disease**, characterized by a papule or pustule at the inoculation site and regional lymphadenopathy.
- While it causes lymphadenopathy, the skin lesions typically do not progress to the chronic **ulcerative and nodular pattern along lymphatic drainage** seen here, and there's no history of cat exposure.
*Pasteurella multocida*
- *Pasteurella multocida* is a common cause of **wound infections after animal bites or scratches**, particularly from cats and dogs.
- Infections typically manifest as rapid onset of **erythema, swelling, and pain** at the bite site, often with cellulitis, rather than the described pustular-to-nodular-to-ulcerative progression along lymphatic channels.
*Blastomyces dermatitidis*
- *Blastomyces dermatitidis* causes **blastomycosis**, a systemic fungal infection that can present with cutaneous lesions, often **papules, pustules, or ulcers**, but these are typically associated with **pulmonary involvement** and occur after inhalation of spores, not directly from skin inoculation with lymphatic spread in a gardener.
- The skin lesions of blastomycosis are often described as **verrucous** with sharply demarcated borders.
*Pseudomonas aeruginosa*
- *Pseudomonas aeruginosa* can cause various skin infections, especially in immunocompromised individuals, those with burns, or associated with water exposure (e.g., **"hot tub folliculitis"**).
- While it can cause pustules, it does not typically produce the **lymphocutaneous spread** of nodules and ulcers observed in this patient's presentation.
Soil-transmitted helminths US Medical PG Question 7: A 38-year-old man comes to the physician because of a 2-week history of abdominal pain and an itchy rash on his buttocks. He also has fever, nausea, and diarrhea with mucoid stools. One week ago, the patient returned from Indonesia, where he went for vacation. Physical examination shows erythematous, serpiginous lesions located in the perianal region and the posterior thighs. His leukocyte count is 9,000/mm3 with 25% eosinophils. Further evaluation is most likely to show which of the following findings?
- A. Rhabditiform larvae on stool microscopy (Correct Answer)
- B. Entamoeba histolytica antibodies on stool immunoassay
- C. Branching septate hyphae on KOH preparation
- D. Oocysts on acid-fast stool stain
- E. Giardia lamblia antibodies on stool immunoassay
Soil-transmitted helminths Explanation: ***Rhabditiform larvae on stool microscopy***
- The patient's symptoms, including **abdominal pain**, **diarrhea with mucoid stools**, **itchy rash (larva currens)**, and **eosinophilia** after traveling to Indonesia, are highly suggestive of **Strongyloidiasis**.
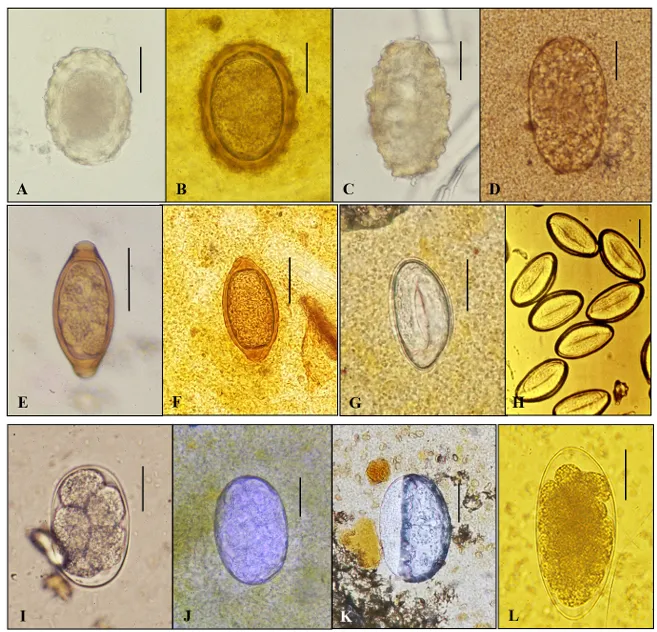
- **Rhabditiform larvae** are typically found in stool samples during the diagnostic phase of strongyloidiasis, as adult worms live in the small intestine and release these larvae.
*Entamoeba histolytica antibodies on stool immunoassay*
- While *Entamoeba histolytica* can cause **dysentery**, **abdominal pain**, and fever, it does not cause an **itchy migratory rash** or significant **eosinophilia**.
- Diagnosis typically involves detecting **trophozoites or cysts** in stool or specific **antigen detection**, not usually antibodies in stool.
*Branching septate hyphae on KOH preparation*
- **Branching, septate hyphae** are characteristic of **fungal infections**, such as dermatophytosis, which primarily affect the skin.
- This finding would not explain the systemic symptoms like **abdominal pain**, **diarrhea**, **fever**, and eosinophilia described in the patient.
*Oocysts on acid-fast stool stain*
- **Oocysts detected by acid-fast stain** are indicative of parasitic infections like **Cryptosporidiosis** or **Cyclosporiasis**, which cause **watery diarrhea** and abdominal cramps.
- These infections do not typically present with the **pruritic serpiginous rash** (larva currens) or the high level of **eosinophilia** seen in this patient.
*Giardia lamblia antibodies on stool immunoassay*
- *Giardia lamblia* causes **giardiasis**, characterized by **diarrhea**, **abdominal cramps**, **bloating**, and **malabsorption**.
- However, giardiasis typically does not cause **eosinophilia** or an **itchy migratory rash**, which are key features in this case.
Soil-transmitted helminths US Medical PG Question 8: A 22-year-old man comes to the physician because of abdominal pain, diarrhea, and weight loss that started after a recent backpacking trip in Southeast Asia. He does not smoke or drink alcohol. His leukocyte count is 7,500/mm3 (61% segmented neutrophils, 13% eosinophils, and 26% lymphocytes). Stool microscopy shows rhabditiform larvae. This patient is most likely to develop which of the following?
- A. Perianal serpiginous rash (Correct Answer)
- B. Hematuria
- C. Rectal prolapse
- D. Peripheral lymphedema
- E. Muscle tenderness
Soil-transmitted helminths Explanation: ***Perianal serpiginous rash***
- The patient's symptoms (abdominal pain, diarrhea, weight loss, recent travel to Southeast Asia, eosinophilia, and rhabditiform larvae in stool) are highly suggestive of **Strongyloidiasis**.
- The **rhabditiform larvae** of **Strongyloides stercoralis** can autoinfect the host, migrating through the skin from the perianal area, causing a characteristic **larva currens** or **perianal serpiginous rash**.
*Hematuria*
- **Hematuria** is typically associated with **Schistosomiasis** (especially *Schistosoma haematobium*), which involves the genitourinary tract.
- While schistosomiasis is prevalent in some parts of Southeast Asia, the patient's presentation with **rhabditiform larvae** and **eosinophilia** points away from it.
*Rectal prolapse*
- **Rectal prolapse** can occur with chronic straining due to severe diarrhea or constipation, or in conditions like **Trichuriasis (whipworm infection)**.
- While diarrhea is present, the specific finding of **rhabditiform larvae** and the high eosinophil count are not characteristic of conditions directly leading to rectal prolapse.
*Peripheral lymphedema*
- **Peripheral lymphedema** is a hallmark symptom of **Filariasis**, caused by parasitic worms like *Wuchereria bancrofti* or *Brugia malayi*, transmitted by mosquitoes.
- The patient's presentation, particularly the **rhabditiform larvae in stool**, does not support a diagnosis of filariasis.
*Muscle tenderness*
- **Muscle tenderness** and myalgia can be associated with several parasitic infections, most notably **Trichinellosis**, caused by *Trichinella spiralis*.
- However, the finding of **rhabditiform larvae in stool** and the absence of specific symptoms like periorbital edema or splinter hemorrhages make trichinellosis less likely than strongyloidiasis.
Soil-transmitted helminths US Medical PG Question 9: A 37-year-old man makes an appointment with his primary care physician because he has been feeling tired and is no longer able to play on a recreational soccer team. He also says his coworkers have commented that he appears pale though he has not noticed any changes himself. He says that he has been generally healthy and that the only notable event that happened in the last year is that he went backpacking all over the world. Based on clinical suspicion, a series of blood tests are performed with partial results presented below:
Hemoglobin: 9.8 g/dL
Platelet count: 174,000/mm^3
Mean corpuscular volume: 72 µm^3 (normal: 80-100 µm^3)
Iron: 22 µg/dL (normal: 50-170 µg/dL)
Ferritin: 8 ng/mL (normal: 15-200 ng/mL)
Lactate dehydrogenase: 57 U/L (normal: 45-90 U/L)
Urine hemoglobin: absent
Infection with which of the following types of organisms could lead to this pattern of findings?
- A. Nematode (Correct Answer)
- B. Mosquito-borne protozoa
- C. Double-stranded virus
- D. Single-stranded virus
- E. Tick-borne protozoa
Soil-transmitted helminths Explanation: ***Nematode***
- The patient's symptoms (fatigue, pallor) and lab results (**microcytic anemia** with **low hemoglobin**, **low MCV**, **low iron**, and **low ferritin**) are highly suggestive of **iron deficiency anemia**. The history of backpacking worldwide increases the suspicion of **hookworm infection**, which is a nematode that causes chronic gastrointestinal blood loss leading to iron deficiency.
- **Hookworms** (e.g., *Ancylostoma duodenale*, *Necator americanus*) attach to the intestinal wall, causing persistent blood loss as they feed, which depletes iron stores over time.
*Mosquito-borne protozoa*
- **Mosquito-borne protozoa** primarily refers to *Plasmodium* species which cause malaria. While malaria can cause anemia, it typically presents with **hemolytic anemia** (elevated LDH, jaundice), intermittent fevers, and splenomegaly, not the profound iron deficiency seen here.
- The anemia in malaria is usually **normocytic or macrocytic** due to increased erythropoiesis, and profound iron deficiency is not the primary mechanism.
*Double-stranded virus*
- **Double-stranded viruses** (e.g., adenoviruses, herpesviruses, some papillomaviruses) typically cause acute infections, and while some can lead to anemia through bone marrow suppression or chronic inflammation, they do not directly cause **iron deficiency anemia** with this specific lab profile.
- The clinical picture of chronic fatigue and iron depletion after travel is not characteristic of common viral infections caused by double-stranded viruses.
*Single-stranded virus*
- **Single-stranded viruses** (e.g., influenza, measles, HIV, dengue, enteroviruses) cause a wide range of illnesses. While some can lead to anemia, often through **bone marrow suppression** or chronic inflammation, they are not typically associated with the profound **iron deficiency** and microcytic anemia seen in this patient.
- Travel history can be relevant for some single-stranded viral infections (e.g., HIV, dengue), but the specific laboratory findings point away from a primary viral etiology for the anemia.
*Tick-borne protozoa*
- **Tick-borne protozoa** most commonly refers to *Babesia* species, which cause babesiosis. This disease primarily leads to **hemolytic anemia** (intravascular hemolysis, elevated LDH), fever, chills, and fatigue, which is distinct from the **iron deficiency anemia** presented in the case.
- **Babesiosis** would typically present with signs of hemolysis, such as elevated LDH and sometimes hemoglobinuria, which are absent in this patient.
Soil-transmitted helminths US Medical PG Question 10: A 16-year-old boy is brought to the physician by his host parents for evaluation of a progressively pruritic rash over his shoulders and buttocks for the past 6 months. He recently came to the United States from Nigeria to attend a year of high school. He reports that it has been increasingly difficult for him to read the whiteboard during classes. Physical examination shows symmetrically distributed papules 4–8 mm in diameter, excoriation marks, and patchy hyperpigmentation over his shoulders, waist, and buttocks. There is nontender inguinal lymphadenopathy and several firm, nontender subcutaneous nodules along the right iliac crest. Six skin snip biopsies are taken from the pelvic girdle, buttocks, and thigh, and are then incubated in saline. After 24 hours, microscopic examination shows motile microfilariae. Which of the following is the most likely diagnosis?
- A. Cysticercosis
- B. Onchocerciasis (Correct Answer)
- C. Lymphatic filariasis
- D. Cutaneous larva migrans
- E. Trichuriasis
Soil-transmitted helminths Explanation: ***Onchocerciasis***
- The presentation of **pruritic rash with papules**, **subcutaneous nodules** (onchocercomas), and **visual difficulties** (river blindness) in an individual from an endemic area (Nigeria) is classic for **onchocerciasis**.
- The presence of **motile microfilariae in skin snips** after saline incubation is a diagnostic hallmark of this condition, caused by *Onchocerca volvulus*.
*Cysticercosis*
- This condition is caused by the larval stage of *Taenia solium* and typically presents with **calcified lesions** in the muscle and brain (neurocysticercosis), which can lead to seizures.
- It does not typically cause the generalized pruritic rash, subcutaneous nodules, or ocular symptoms described, nor would **motile microfilariae** be found in skin snips.
*Lymphatic filariasis*
- Caused by *Wuchereria bancrofti* or *Brugia malayi*, this disease is characterized by **lymphedema** and **hydrocele**, eventually leading to **elephantiasis**.
- While it involves filarial worms and can cause lymphadenopathy, it does not typically manifest with the described rash, vision problems, or **subcutaneous nodules** (onchocercomas).
*Cutaneous larva migrans*
- This condition, caused by hookworm larvae (e.g., *Ancylostoma braziliense*), presents as a **serpiginous, intensely pruritic eruption** where the larvae migrate under the skin.
- It does not cause subcutaneous nodules, generalized papular rash, or ocular involvement, and skin snips would not show **microfilariae**.
*Trichuriasis*
- Caused by the **whipworm** (*Trichuris trichiura*), this is an intestinal nematode infection that can lead to **abdominal pain**, **diarrhea**, **rectal prolapse**, and **anemia**.
- It does not present with skin lesions, subcutaneous nodules, or visual impairment, and diagnosis is typically made by finding **ova in stool samples**, not microfilariae in skin snips.
More Soil-transmitted helminths US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.