Schistosomiasis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Schistosomiasis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Schistosomiasis US Medical PG Question 1: A 34-year-old man comes to the physician because of progressive swelling of the left lower leg for 4 months. One year ago, he had an episode of intermittent fever and tender lymphadenopathy that occurred shortly after he returned from a trip to India and resolved spontaneously. Physical examination shows 4+ nonpitting edema of the left lower leg. His leukocyte count is 8,000/mm3 with 25% eosinophils. A blood smear obtained at night confirms the diagnosis. Treatment with diethylcarbamazine is initiated. Which of the following is the most likely route of transmission of the causal pathogen?
- A. Penetration of the skin by hookworms in feces
- B. Penetration of the skin by cercariae from contaminated fresh water
- C. Deposition of larvae into the skin by a female black fly
- D. Ingestion of encysted larvae in undercooked pork
- E. Deposition of thread-like larvae into the skin by a female mosquito (Correct Answer)
Schistosomiasis Explanation: ***Deposition of thread-like larvae into the skin by a female mosquito***
- The symptoms described, including progressive **nonpitting edema** (lymphedema), a history of **fever** and **lymphadenopathy** after travel to an endemic area (India), and significant **eosinophilia**, are classic for **lymphatic filariasis**.
- Lymphatic filariasis, caused by filarial worms like *Wuchereria bancrofti* or *Brugia malayi*, is transmitted by **mosquitoes** that deposit infectious larvae onto the skin during a blood meal.
*Penetration of the skin by hookworms in feces*
- This describes the transmission of **hookworm infection**, which causes **iron deficiency anemia** and gastrointestinal symptoms, not lymphedema or high eosinophilia with nocturnal microfilaremia.
- While hookworms can cause eosinophilia, the clinical presentation of chronic lymphedema and the need for a nocturnal blood smear point away from hookworm infection.
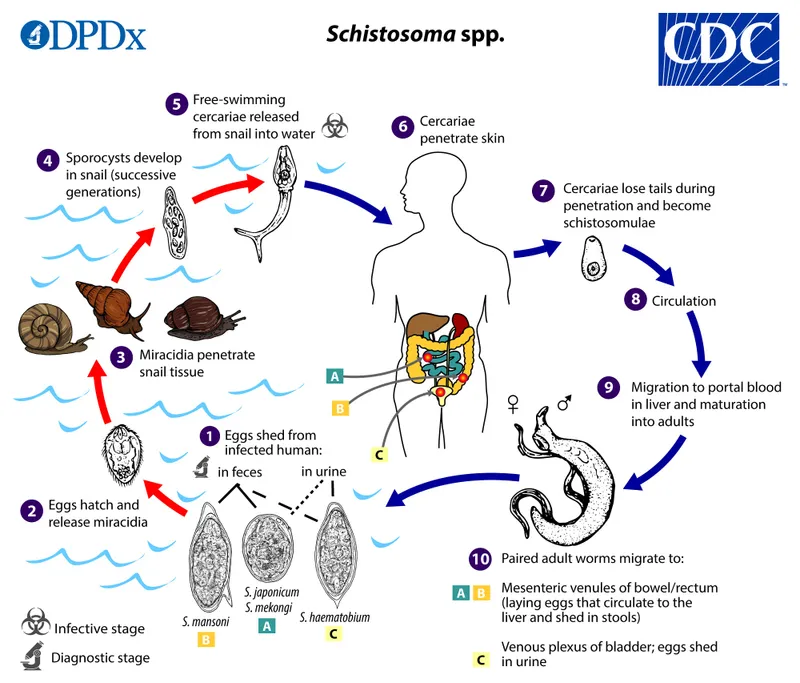
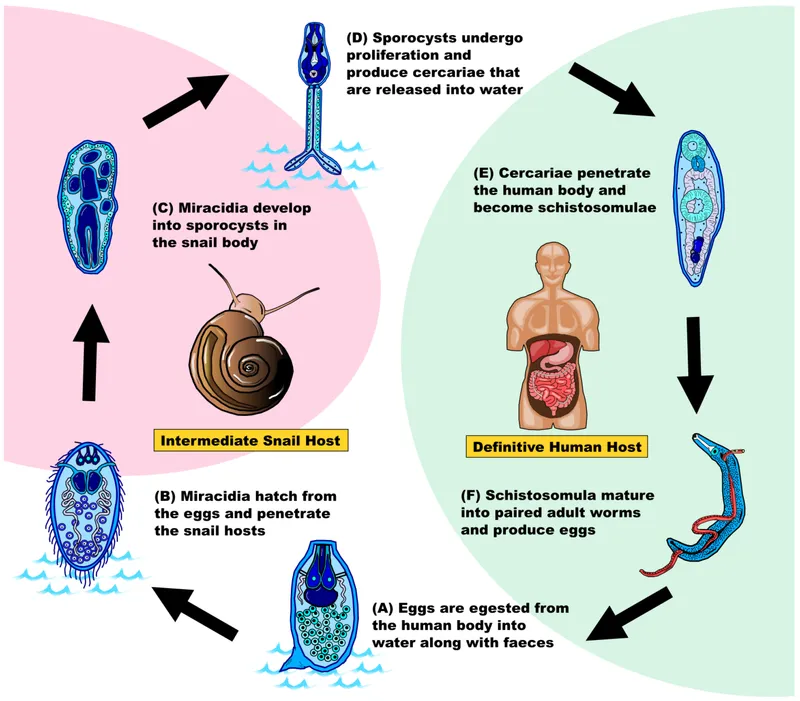
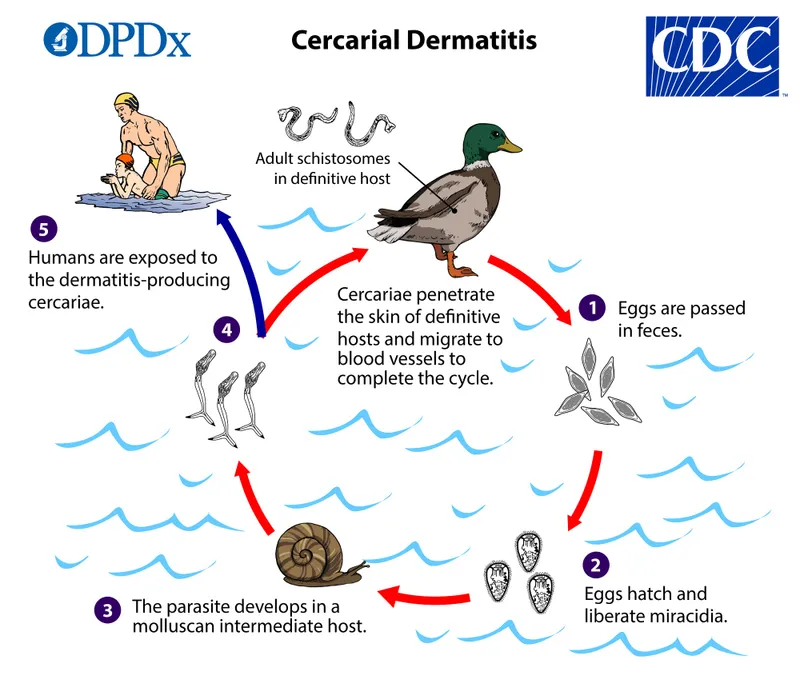
*Penetration of the skin by cercariae from contaminated fresh water*
- This is the transmission method for **schistosomiasis**, which can cause symptoms depending on the species and affected organs, such as **urinary tract disease**, **hepatic fibrosis**, or **intestinal inflammation**.
- Schistosomiasis does not typically present with the progressive lymphedema and episodic lymphadenitis characteristic of filariasis.
*Deposition of larvae into the skin by a female black fly*
- This describes the transmission of **onchocerciasis** (river blindness), caused by *Onchocerca volvulus*.
- Onchocerciasis primarily causes skin disease (intense **pruritus**, dermatitis) and **ocular lesions** leading to blindness, not extensive lymphedema of the limbs.
*Ingestion of encysted larvae in undercooked pork*
- This is the route of transmission for **trichinellosis**, caused by *Trichinella spiralis*.
- Trichinellosis involves **muscle pain**, fever, and periorbital edema, but not chronic lymphedema of the extremities or the specific nocturnal periodicity for diagnosis.
Schistosomiasis US Medical PG Question 2: A 19-year-old woman presents to the emergency department with chronic diarrhea, fatigue, and weakness. She also had mild lower extremity edema. On examination, she was noted to be pale. Blood testing revealed peripheral eosinophilia (60%) and a Hb concentration of 8 g/dL. The stool examination revealed Fasciolopsis buski eggs. Which of the following drugs would most likely be effective?
- A. Albendazole
- B. Oxamniquine
- C. Niclosamide
- D. Praziquantel (Correct Answer)
- E. Bithionol
Schistosomiasis Explanation: ***Praziquantel***
- **Praziquantel** is the **drug of choice** for treating trematode infections, including those caused by **Fasciolopsis buski**.
- Its mechanism of action involves increasing the permeability of the parasite's cell membrane to calcium, leading to paralysis and death of the fluke.
- It is highly effective, well-tolerated, and the standard first-line treatment.
*Albendazole*
- **Albendazole** is primarily used for various **nematode (roundworm)** infections, such as ascariasis, hookworm, and trichuriasis.
- While it has some activity against certain cestodes, it is not the first-line treatment for **Fasciolopsis buski**, a **trematode (fluke)**.
*Oxamniquine*
- **Oxamniquine** is an anthelmintic specifically used for the treatment of **schistosomiasis**, particularly against *Schistosoma mansoni*.
- It works by damaging the adult worms' teguments, but it is not effective against **Fasciolopsis buski**.
*Niclosamide*
- **Niclosamide** is an effective treatment for **cestode (tapeworm)** infections, such as *Taenia saginata* and *Hymenolepis nana*.
- Its mechanism involves inhibiting parasitic mitochondrial oxidative phosphorylation, but it is not active against **fluke** infections like **Fasciolopsis buski**.
*Bithionol*
- **Bithionol** is used primarily for treating **Fasciola hepatica** (the common liver fluke) and **Paragonimus westermani** (lung fluke) infections.
- While it has trematocidal activity, it is **not the drug of choice** for **Fasciolopsis buski**—**praziquantel** is preferred due to its superior efficacy, broader spectrum against intestinal flukes, better safety profile, and widespread availability.
Schistosomiasis US Medical PG Question 3: A 30-year-old man presents to the physician after he discovered a raised, red, string-shaped lesion beneath the skin on his right foot. The lesion seems to move from one location to another over the dorsum of his foot from day to day. He says that the lesion is extremely itchy and has not responded to over the counter topical treatment. He and his wife recently returned from a honeymoon in southern Thailand, where they frequented the tropical beaches. The physician diagnoses him with a parasitic infection and prescribes albendazole for the patient. With which of the following organisms is the patient most likely infected?
- A. Ancylostoma braziliense (Correct Answer)
- B. Dracunculus medinensis
- C. Necator americanus
- D. Strongyloides stercoralis
- E. Wuchereria bancrofti
Schistosomiasis Explanation: ***Ancylostoma braziliense***
- This clinical presentation of a **pruritic, migratory, serpiginous rash** on the foot after exposure to contaminated sand (tropical beach in Thailand) is classic for **cutaneous larva migrans**, caused by hookworm larvae, predominantly *Ancylostoma braziliense*.
- The larvae penetrate the skin but cannot complete their life cycle in humans, instead migrating subcutaneously, causing the characteristic **"creeping eruption"**.
*Dracunculus medinensis*
- This parasite causes **dracunculiasis**, where the adult female worm migrates to the skin, creating a painful blister, often on the lower limbs, from which it emerges.
- It is acquired by ingesting **copepods** (water fleas) containing larvae, not by direct contact with contaminated sand, and the lesion typically ulcerates rather than migrating repeatedly.
*Necator americanus*
- This is a human hookworm that causes **iron deficiency anemia** and can lead to **cutaneous larva currens** from larval penetration, which is a rapidly advancing linear lesion, but it typically progresses to systemic infection where the worms reside in the small intestine.
- While it can cause an itchy rash at the site of penetration (ground itch), it does not cause the **chronic, migratory, serpiginous eruption** characteristic of cutaneous larva migrans.
*Strongyloides stercoralis*
- This parasite can cause **larva currens** (a rapidly moving linear skin eruption) and systemic complications, particularly in immunocompromised individuals.
- While it can cause skin lesions, the typical description is of a much faster-moving lesion that usually spreads from the anus and is less serpiginous and persistent in one area compared to the classic presentation of cutaneous larva migrans.
*Wuchereria bancrofti*
- This nematode causes **lymphatic filariasis** (elephantiasis), characterized by lymphedema, hydrocele, and chyluria, and is transmitted by **mosquito bites**.
- It does not cause cutaneous migratory lesions on the foot; its pathology relates to chronic lymphatic obstruction by adult worms.
Schistosomiasis US Medical PG Question 4: A 32-year-old man presents to the physician with a history of fever, malaise, and arthralgia in the large joints for the last 2 months. He also mentions that his appetite has been significantly decreased during this period, and he has lost considerable weight. He also informs the physician that he often experiences tingling and numbness in his right upper limb, and his urine is also dark in color. The past medical records show that he was diagnosed with an infection 7 months before and recovered well. On physical examination, the temperature is 37.7°C (99.8°F), the pulse rate is 86/min, the respiratory rate is 14/min, and the blood pressure is 130/94 mm Hg. Which of the following infections has most likely caused the condition the patient is suffering from?
- A. Mycoplasma pneumoniae
- B. Epstein-Barr virus infection
- C. Yersinia enterocolitica
- D. Hepatitis B virus (Correct Answer)
- E. Chlamydophila pneumoniae
Schistosomiasis Explanation: ***Hepatitis B virus***
- The patient's symptoms of **fever**, **malaise**, **arthralgia** in large joints, **dark urine**, and **weight loss** are classic signs of **hepatitis B virus (HBV)** infection with **extrahepatic manifestations**.
- **Dark urine** indicates **bilirubinuria** from hepatic involvement, confirming liver pathology.
- **Arthralgia in large joints** is a well-recognized extrahepatic manifestation of HBV caused by **immune complex deposition** (Type III hypersensitivity).
- The **neurological symptoms** (tingling and numbness) strongly suggest **polyarteritis nodosa (PAN)**, a necrotizing vasculitis associated with HBV that commonly causes **mononeuritis multiplex** and peripheral neuropathy.
- The history of infection **7 months ago** with ongoing symptoms suggests progression to **chronic HBV infection** with systemic complications.
*Mycoplasma pneumoniae*
- This infection primarily causes **respiratory symptoms**, such as **atypical pneumonia** ("walking pneumonia"), and is less likely to lead to persistent arthralgia, significant weight loss, or dark urine.
- While post-infectious arthralgia can rarely occur, it is not a prominent feature and does not explain the hepatic (dark urine) or neurological manifestations.
*Epstein-Barr virus infection*
- **Epstein-Barr virus (EBV)** typically causes **infectious mononucleosis**, characterized by **fever**, **fatigue**, **pharyngitis**, **lymphadenopathy**, and **splenomegaly**.
- While mild arthralgia can occur, it is not a dominant feature, and **dark urine** (bilirubinuria), **significant weight loss**, and **peripheral neuropathy** are not characteristic of EBV infection.
*Yersinia enterocolitica*
- Infections with **Yersinia enterocolitica** typically cause **acute gastroenteritis** with **diarrhea**, **abdominal pain**, and sometimes **reactive arthritis** (Reiter syndrome).
- **Reactive arthritis** more commonly affects **lower extremity joints** in an **asymmetric pattern** and occurs post-infection, not during active infection.
- The **dark urine**, **neuropathy**, and **chronic constitutional symptoms** are not characteristic of Yersinia infection.
*Chlamydophila pneumoniae*
- This pathogen primarily causes **respiratory tract infections**, similar to Mycoplasma pneumoniae, leading to **atypical pneumonia** or **bronchitis**.
- It is not typically associated with chronic arthralgia, significant weight loss, dark urine (hepatic involvement), or neurological symptoms as described in this case.
Schistosomiasis US Medical PG Question 5: A 40-year-old man presents to the office with complaints of epigastric discomfort for the past 6 months. He adds that the discomfort is not that bothersome as it does not interfere with his daily activities. He does not have any other complaints at the moment. The past medical history is insignificant. He is a non-smoker and does not consume alcohol. He recently came back from a trip to South America where he visited a relative who owned a sheep farm. On physical examination, he has a poorly palpable epigastric non-tender mass with no organomegaly. The hepatitis B and C serology are negative. The liver CT scan and MRI are shown. What is the most likely diagnosis?
- A. Echinococcosis (Correct Answer)
- B. Liver abscess
- C. Hepatocellular carcinoma
- D. Tuberculosis
- E. Hemangioma
Schistosomiasis Explanation: ***Echinococcosis (Correct Answer)***
- The patient's history of travel to **South America** and contact with a **sheep farm** is highly suggestive of exposure to *Echinococcus granulosus*, the causative agent of hydatid disease.
- The **CT scan image** shows a large, well-defined cyst with a **calcified wall** and internal septations, consistent with the characteristic appearance of a **hydatid cyst** in the liver.
- This presentation is classic for **hepatic echinococcosis**: chronic indolent course, epidemiological exposure, and pathognomonic imaging findings.
*Liver abscess (Incorrect)*
- Liver abscesses typically present with more acute symptoms such as **fever, chills, and significant pain**, which are absent in this case.
- Imaging usually reveals a **hypo-dense lesion** with a rim of enhancement, possibly gas formation, and less commonly a calcified wall.
*Hepatocellular carcinoma (Incorrect)*
- This patient lacks typical risk factors for HCC, such as **chronic hepatitis B or C infection** (serology is negative) or cirrhosis.
- HCC imaging typically shows an **enhancing mass** that washes out on delayed phases, without the calcified, multi-loculated appearance seen here.
*Tuberculosis (Incorrect)*
- Hepatic tuberculosis typically presents with fever, weight loss, and multiple **small, hypo-dense lesions** on imaging, often with an associated pulmonary or extra-pulmonary focus.
- The single, large, calcified cystic lesion seen on imaging is not characteristic of hepatic tuberculosis.
*Hemangioma (Incorrect)*
- Hepatic hemangiomas are benign vascular tumors that often present as **incidental findings** and are typically asymptomatic.
- On CT scans, they show characteristic **peripheral nodular enhancement** that fills in centripetally on delayed phases, which is different from the calcified cyst observed.
Schistosomiasis US Medical PG Question 6: A 31-year-old man comes to the physician because of a 2-day history of nausea, abdominal discomfort, and yellow discoloration of the eyes. Six weeks ago, he had an episode of fever, joint pain, swollen lymph nodes, and an itchy rash on his trunk and extremities that persisted for 1 to 2 days. He returned from a backpacking trip to Colombia two months ago. His temperature is 39°C (101.8°F). Physical examination shows scleral icterus. Infection with which of the following agents is the most likely cause of this patient's findings?
- A. Enterotoxigenic E. coli
- B. Hepatitis B (Correct Answer)
- C. Borrelia burgdorferi
- D. Campylobacter jejuni
- E. Hepatitis A
Schistosomiasis Explanation: ***Hepatitis B***
- This patient's presentation is **classic for acute hepatitis B infection**. The key diagnostic feature is the **serum sickness-like prodrome** that occurred 6 weeks ago, characterized by **fever, arthralgia, lymphadenopathy, and urticarial rash**.
- This prodromal syndrome results from **circulating immune complexes** (HBsAg-antibody complexes) and is a **hallmark of Hepatitis B**, occurring in 10-20% of acute HBV cases during the pre-icteric phase.
- The timeline fits perfectly: **exposure 2 months ago** (travel to Colombia) → **prodrome at 6 weeks** (4-10 weeks post-exposure is typical) → **icteric phase now** (jaundice with scleral icterus).
- Hepatitis B can be transmitted through **sexual contact, needlestick injuries, or exposure to contaminated instruments** during travel, making it highly relevant in this travel context.
*Hepatitis A*
- While hepatitis A is common in travelers to endemic areas and causes acute hepatitis, it **does NOT typically present with the serum sickness-like prodrome** described here.
- HAV prodrome is usually **nonspecific** (malaise, anorexia, nausea) and does **not include arthralgia, lymphadenopathy, or urticarial rash**.
- The described prodromal syndrome with rash and joint pain is **pathognomonic for HBV**, not HAV.
*Borrelia burgdorferi*
- This bacterium causes **Lyme disease**, characterized by **erythema migrans** (expanding target lesion), not an urticarial rash.
- Lyme disease does not cause **acute hepatitis with jaundice** or the icteric presentation seen here.
- Not consistent with the clinical timeline or hepatic involvement.
*Enterotoxigenic E. coli*
- ETEC causes **traveler's diarrhea** with watery stools, cramping, and nausea, typically within days of exposure.
- Does **not cause hepatitis**, jaundice, or a prodromal syndrome with rash and arthralgia.
- Symptoms resolve within 3-5 days without hepatic involvement.
*Campylobacter jejuni*
- Causes **bacterial gastroenteritis** with bloody diarrhea, fever, and abdominal pain.
- Does **not cause acute hepatitis** with jaundice or the serum sickness-like prodrome described.
- While travel-associated, it does not explain the hepatic and systemic findings.
Schistosomiasis US Medical PG Question 7: A 45-year-old man presents to the emergency department with abdominal distension. The patient states he has had gradually worsening abdominal distension with undulating pain, nausea, and vomiting for the past several months. The patient does not see a physician typically and has no known past medical history. He works as a farmer and interacts with livestock and also breeds dogs. His temperature is 98.7°F (37.1°C), blood pressure is 159/90 mmHg, pulse is 88/min, respirations are 15/min, and oxygen saturation is 99% on room air. Physical exam is notable for mild abdominal distension and discomfort to palpation of the upper abdominal quadrants. Laboratory values are ordered and are notable for a mild eosinophilia. A CT scan of the abdomen demonstrates multiple small eggshell calcifications within the right lobe of the liver. Which of the following is the most likely etiology of this patient's symptoms?
- A. Echinococcus granulosus (Correct Answer)
- B. Enterobius vermicularis
- C. Necator americanus
- D. Taenia solium
- E. Taenia saginata
Schistosomiasis Explanation: ***Echinococcus granulosus***
- The patient's history of working with **livestock** and dogs, combined with **abdominal pain**, **eosinophilia**, and characteristic **eggshell calcifications** in the liver on CT, is highly suggestive of **hydatid disease** caused by *Echinococcus granulosus*.
- This parasite's larval stage forms **hydatid cysts** primarily affecting the liver and lungs, which can grow slowly and cause symptoms as they expand.
*Enterobius vermicularis*
- This parasite causes **pinworm infection**, primarily manifesting as **perianal itching**, especially at night.
- It does not typically cause abdominal distension, liver cysts, or eosinophilia to this extent, and is diagnosed via the **scotch tape test**.
*Necator americanus*
- This is a type of **hookworm** that primarily causes **iron deficiency anemia** due to chronic blood loss in the GI tract.
- Symptoms include fatigue, weakness, and pallor, but not liver cysts with eggshell calcifications or significant abdominal distension as described.
*Taenia solium*
- **Pork tapeworm** infection can cause **cysticercosis** if humans ingest the eggs, leading to cysts in muscles, subcutaneous tissue, and the brain (neurocysticercosis).
- While it can cause cysts, the classic "eggshell calcifications" in the liver are not typical for *Taenia solium* infection, and the symptoms described fit *Echinococcus* better.
*Taenia saginata*
- This is the **beef tapeworm**, which causes relatively mild symptoms in humans, often limited to mild abdominal discomfort or passage of proglottids in stool.
- It does not cause tissue cysts like those seen in cysticercosis from *T. solium* or hydatid cysts from *Echinococcus*.
Schistosomiasis US Medical PG Question 8: A 29-year-old internal medicine resident presents to the emergency department with complaints of fevers, diarrhea, abdominal pain, and skin rash for 2 days. He feels fatigued and has lost his appetite. On further questioning, he says that he returned from his missionary trip to Brazil last week. He is excited as he talks about his trip. Besides a worthy clinical experience, he also enjoyed local outdoor activities, like swimming and rafting. His past medical history is insignificant. The blood pressure is 120/70 mm Hg, the pulse is 100/min, and the temperature is 38.3°C (100.9°F). On examination, there is a rash on the legs. The rest of the examination is normal. Which of the following organisms is most likely responsible for this patient’s condition?
- A. Schistosoma mansoni (Correct Answer)
- B. Schistosoma haematobium
- C. Vibrio cholerae
- D. Onchocerca volvulus
- E. Schistosoma japonicum
Schistosomiasis Explanation: ***Schistosoma mansoni***
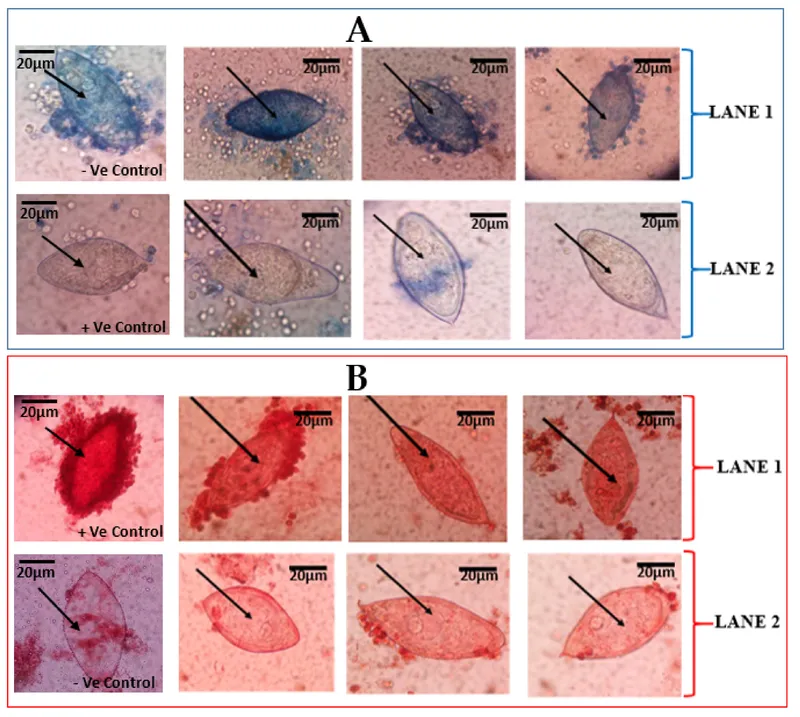
- The patient's symptoms (fevers, diarrhea, abdominal pain, rash, fatigue) after swimming and rafting in Brazil are classic for **acute schistosomiasis (Katayama fever)**, and *Schistosoma mansoni* is endemic to South America, including Brazil, affecting the **gastrointestinal tract**.
- The rash on the legs is consistent with the entry points of **cercariae** through the skin, and the systemic symptoms develop as the adult worms mature and lay eggs.
*Schistosoma haematobium*
- This species primarily causes **urinary schistosomiasis**, with symptoms like **hematuria**, dysuria, and bladder wall calcification.
- It is prevalent in Africa and the Middle East, not typically associated with Brazil.
*Vibrio cholerae*
- *Vibrio cholerae* causes severe, watery **diarrhea** (rice-water stools) and rapid **dehydration**, usually without a prominent rash or prolonged systemic symptoms like fatigue and fever as the primary presentation.
- While diarrhea is present, the array of other symptoms and the exposure history do not align with cholera.
*Onchocerca volvulus*
- This parasite causes **onchocerciasis (river blindness)**, transmitted by blackflies, and primarily manifests as **dermatitis**, subcutaneous nodules, and significant eye disease leading to blindness.
- It does not typically cause acute febrile illness with prominent gastrointestinal symptoms like those described.
*Schistosoma japonicum*
- *Schistosoma japonicum* is found in East Asia (e.g., China, Philippines), not South America, and primarily affects the **gastrointestinal tract** and liver, similar to *S. mansoni*.
- The geographical exposure to Brazil makes *S. mansoni* the most likely cause, despite similar clinical features to *S. japonicum*.
Schistosomiasis US Medical PG Question 9: A 27-year-old woman comes to the physician for a 1-week-history of painful urination and urinary frequency. She has no history of serious illness and takes no medications. She is sexually active with her boyfriend. Her temperature is 36.7°C (98.1°F). There is no costovertebral angle tenderness. Urine dipstick shows leukocyte esterase. A Gram stain does not show any organisms. Which of the following is the most likely causal pathogen?
- A. Escherichia coli
- B. Chlamydia trachomatis (Correct Answer)
- C. Gardnerella vaginalis
- D. Neisseria gonorrhoeae
- E. Trichomonas vaginalis
Schistosomiasis Explanation: ***Chlamydia trachomatis***
- This patient presents with symptoms of **dysuria** and **urinary frequency**, consistent with a **urethritis**. The absence of bacteria on Gram stain points towards an **atypical pathogen**.
- **Chlamydia trachomatis** is a common cause of **non-gonococcal urethritis** and is a sexually transmitted infection, which fits with the sexually active history.
*Escherichia coli*
- **E. coli** is the most common cause of **bacterial urinary tract infections (UTIs)**, but a Gram stain in this case would typically reveal Gram-negative rods.
- While it causes dysuria and frequency, the **negative Gram stain** makes it less likely than an atypical pathogen.
*Gardnerella vaginalis*
- **Gardnerella vaginalis** is associated with **bacterial vaginosis**, causing a characteristic **fishy odor** and **vaginal discharge**, which are not reported here.
- It does not typically cause urethritis leading to painful urination and urinary frequency.
*Neisseria gonorrhoeae*
- **Neisseria gonorrhoeae** can cause **urethritis** with symptoms similar to those presented, and it is a sexually transmitted infection.
- However, Gram stain would typically show **Gram-negative diplococci** (intracellularly), which were not observed in this case.
*Trichomonas vaginalis*
- **Trichomonas vaginalis** is a **protozoan parasite** causing **trichomoniasis**, which commonly presents with **vaginitis** (frothy, green-yellow discharge, itching) or sometimes urethritis.
- While it is a **sexually transmitted infection**, this organism is not detected by Gram stain (which only stains bacteria); it would require **wet mount microscopy** for visualization. The primary presentation is usually vaginal, and it's less likely to be the sole cause of these urinary symptoms without other signs of vaginitis.
Schistosomiasis US Medical PG Question 10: A 46-year-old woman comes to the physician for a 6-month history of worsening bronchial asthma control. Before this issue began, she only used her salbutamol inhaler once a day. Now, she has to use it multiple times daily and also reports frequent nighttime awakening. Seven months ago, she moved to an apartment that is damp and has mold on some of the walls. The physician injects 0.1 mL of Candida albicans extract on the mid-volar surface of the right arm intradermally. After 48 hours there is a palpable induration of 17 mm. This reaction is most likely a result of release of which of the following substances?
- A. Interleukin-10
- B. Superoxide anion
- C. Tryptase
- D. Interferon-γ (Correct Answer)
- E. Lysozyme
Schistosomiasis Explanation: ***Interferon-γ***
- The patient's worsened asthma, fungal exposure, and positive delayed-type hypersensitivity (DTH) skin test to *Candida albicans* suggest a **Th1-mediated immune response**.
- **Interferon-γ (IFN-γ)** is a key cytokine produced by Th1 cells, crucial for activating macrophages and cell-mediated immunity, which drives the induration observed in DTH reactions.
*Interleukin-10*
- **Interleukin-10 (IL-10)** is primarily an **anti-inflammatory cytokine** that suppresses immune responses, particularly Th1 and Th2 activity.
- Its release is associated with downregulating, rather than mediating, the robust inflammatory reaction seen in a positive DTH test.
*Superoxide anion*
- **Superoxide anion** is a reactive oxygen species produced by phagocytes (e.g., neutrophils, macrophages) as part of the **respiratory burst** to kill ingested pathogens.
- While important for host defense, it is not the primary mediator responsible for the induration and cellular infiltration characteristic of a *Candida* DTH skin test.
*Tryptase*
- **Tryptase** is an enzyme released by **mast cells** upon activation, typically during **immediate hypersensitivity reactions (Type I)**.
- Its presence is indicative of allergic reactions mediated by IgE, which manifest as wheal and flare, not the delayed induration seen in this case.
*Lysozyme*
- **Lysozyme** is an enzyme found in secretions (e.g., tears, saliva) and phagocytes, which degrades bacterial cell walls.
- It plays a role in innate immunity against bacteria but is not directly involved in the mediation of a delayed-type hypersensitivity reaction to fungal antigens.
More Schistosomiasis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.